Abstract
Tissue adhesives are being used in medical and cosmetic industries and first aid for a long time. But their everyday usage has not been widespread. Only case report information is available about their usage. Despite good and meaningful results after they were used, there is lack of standard information that gives idea of about in which cases they could be helpful. Nowadays, cyanoacrylates are used in the surgery more frequently. In this review, we wanted to oversee the biochemical properties and the urological utilisation areas of cyanoacrylates.
Keywords: Biochemical features, cyanoacrylate, glue, urologic diseases
Introduction
Tissue glues are classified as natural protein based, biomimetic, synthetic, and hybrid tissue adhesives (Table 1).[1] Cyanoacrylic (CA) glues are synthetic, and hybrid tissue sealants, belonging to a chemical group which demonstrates strong, and rapidly acting adhesive properties, and used prevalently in industry, medicine, and household activities. CA family is termed based on cyano, and ethylene groups, and variable alkyl groups, and consists of methyl-2-cyanoacrylate (2-MCA), ethyl-2-cyanoacrylate (2-ECA), n-butyl-cyanoacrilate (nBCA), isobutyl cyanoacrilate, octyl cyanoacrylate (OCA), and 2-octyl cyanoacrylate (2-OCA) (Figure 1). The 2-OCA is used in medicine, veterinery medicine, and emergency first aid. OCAs have been developed to alleviate toxicity concerns, and minimize skin irritation, and allergic response. Firstly, OCA spray form was used to decrease blood loss in soldiers till they gained access into medical facilities. BCA was used till 1970, however USA Food and Drug Administration did not permit its further use.[2] nBCA demonstrated irritative effects, however nowadays different cyanoacrylate variants formed with the addition of compounds to CAs have been easily used in medicine.
Table 1.
Tissue adhesives[1]
| Natural protein based tissue adhesives | Biomimetic tissue adhesives | Synthetic and hybrid tissue adhesives |
|---|---|---|
|
Fibrin Selants (Raplixa, Artiss, Evarrest, Tisseel, FloSeal, Proceed, CoStasis) -They contain mixture of fibrinogen, and thrombin -Effect: Coagulation |
- Adhesives secreted by small sea organisms (Mussel, Worm, Tube worms): Binding to amine, and thiol groups on the tissue surface -Red, and brown-colored algae secrete phenol compounds - Binding to hydrophobic, and hydrophilic surfaces |
Cyanoacrylate glues -Monomers; they polymerize in water, weak bases, cell membrane, and tissue |
|
Gelatine adhesives (Gelatine-mTG: Coagulation; Peptide-based polymer hydrogels : Cross-linkage with tissue transaminases; Gelatine-resorcinol-formaldehyde (GFR) and Gelatine-resorcinol-formaldehyde-glutaraldehyde (GRFG): Covalent binding to amine groups in the tissue ) |
-Adhesives secreted by lizards |
Cross-linking adhesive agents -Chondroitine-PEG adhesives Hidrogels(CS-PEG, CS-NHS, PEG-(NH2)6) -Human serum albumin (HSA)+Trisuccinimidyl citrate, disuccinimidyl tartrate (DST), disuccinimidly maleate -Isocyanate functional adhesives: 2,4-toluene diisocyanate (TDI), 4,40-methylene-bis(phenyl isocyanate)(MDI) -1,2-ethylene glycol bis-(dilactic acid)+hexamethylene diisocyanate (HDI) -Chitosan: It is a linear aminopolysaccharides synthetized with deacetylation of chitin. Chitin is abundantly found in exoskeleton of shellfish and it is the second most frequently detected natural polymer in the earth after cellulose. |
|
Albumin adhesives (BioGlue: Albumin and Glutaraldehyde) |
-Adhesives secreted by Australian frogs |
Sealants activated by light -Focal Seal: Hydrophilic polyethylene glycol (PEG) and glicolide or lactide, trimethylene carbonate and acrylic acid – It is activated by light, and adheres to tissue -Sebacic acid ve glyserol temelinde acrylate – They are polymerized by light -Chitosan derivatives – They are activated by UV -dityrosine –it is synthetized from insects, and mussels– They are activated by light |
|
Heat-activated adhesives -Lactide-ɛ-caprolactone -Trimethylolpropane-lactide- ɛ-caprolactone |
Nu: nucleophil, charged proton
Figure 1.
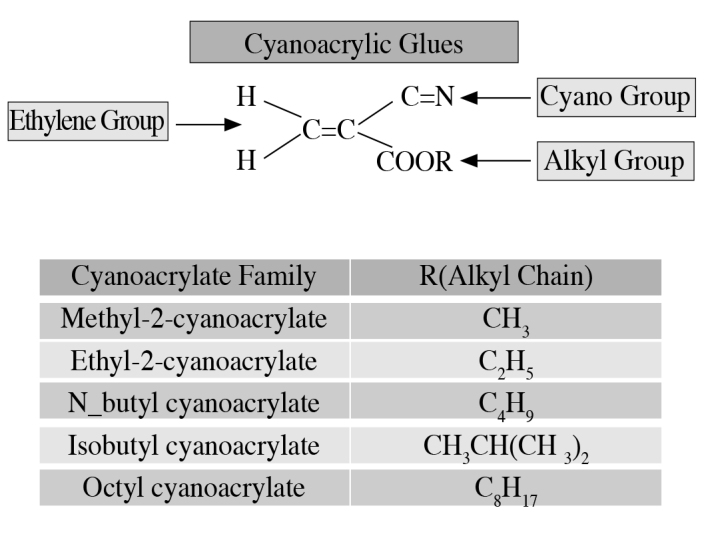
Cyanoacrylate family
Studies have approved their higher safety profiles, and improved functionalities in wound closure when compared with suturing.[3] As observed in many studies closure of wounds with time have led to favourable results as decrease in the incidence of infection, and achievement of cosmetic healing.[3–5] It has been reported that CAs were used to prevent seeding of tumor cells during surgery with favourable outcomes.[6] The shelf-life of CA tubes kept close is one year, it is one month if the tubes are opened for application. Polimerization stops at −18°C, and this issue should be kept in mind while storage conditions are ensured.[7] As review of Cochrane database has revealed that CAs have been used prevalently from the year 2004 up to now.[7] In surgery it is widespreadly used as an alternative to suture materials for the prevention of infection, and leakage. CAs exert their effects through a mechanism resembling to granulation process occurring during various stages of wound healing.[3–5,8]
Biochemical Characteristics of CAs (Table 2)
Table 2.
Cyanoacrylate glues, and characteristic features
| Cyanoacrylate glues (Acrylic resin) |
Biochemical and physiologic characteristics | |
|---|---|---|
|
Methyl-2-cyanoacrylate (2-MCA) (short-chain) |
-Formaldehyde is liberated -Toxic |
-Bacteriostatic activity |
|
Ethyl-2-cyanoacrylate (2-ECA) (short-chain) |
-Formaldehyde is liberated -Toxic |
-Significantly decreases APTT -Bacteriostatic activity |
|
N-butyl cyanoacrylate (nBCA) (long-chain) |
-Slow degradation -Minimal toxic effects -Strong, solid-rigid bonding |
-High tensile force -Strong bonding -Decreases APTT significantly -Bacteriostatic activity |
| Isobutyl cyanoacrylate | -Slow degradation -Minimal toxic effects -Strong, solid-rigid bonding |
-Bacteriostatic activity |
|
Octyl cyanoacrylate (OCA) (long-chain) |
-Slow degradation -Minimal toxic effects -Weaker bonding |
-Bacteriostatic activity |
Cyanoacrylates are acrylic resins which adhere, and bind to the surface within 5–6 seconds in the presence of water, and especially with hydroxide ions, and finally undergo exothermic polymerization within 60 seconds (Figure 2). It perfectly binds to the tissue, and exerts bacteriostatic effects. Dependent on the quality of adhesives, and tissue types, their duration of activity may show variations, while film layer formed by the glue may be eliminated by hydrolytic resolution. OCA, and nBCA have been widely used in medical, and veterinary applications, and generally they do not induce pain. Butyl esther forms ensure strong, solid, and rigid bonding, while octyl esther forms show weak affinity to tissues, and due to their long-chain components they degrade more slowly. nBCAs have been used from 1970 up to now as a medical sealant, hemostatic, and embolic agent for wound repair, for skin closure in pediatric surgery, and obliteration of processus vaginalis during repair of congenital inguinal hernias, as a hemostatic agent to control bleeding of parenchymal organs, in aortic, and thoracic surgery, in the management of arteriovenous malformations, and bleeding gastric varices, in applications for vascular neuroradiology, and interventional radiology.[9–12] If basic principles are obeyed safe use of nBCA for external, and internal applications has been demonstrated both in preclinical, and clinical studies.[13]
Figure 2.
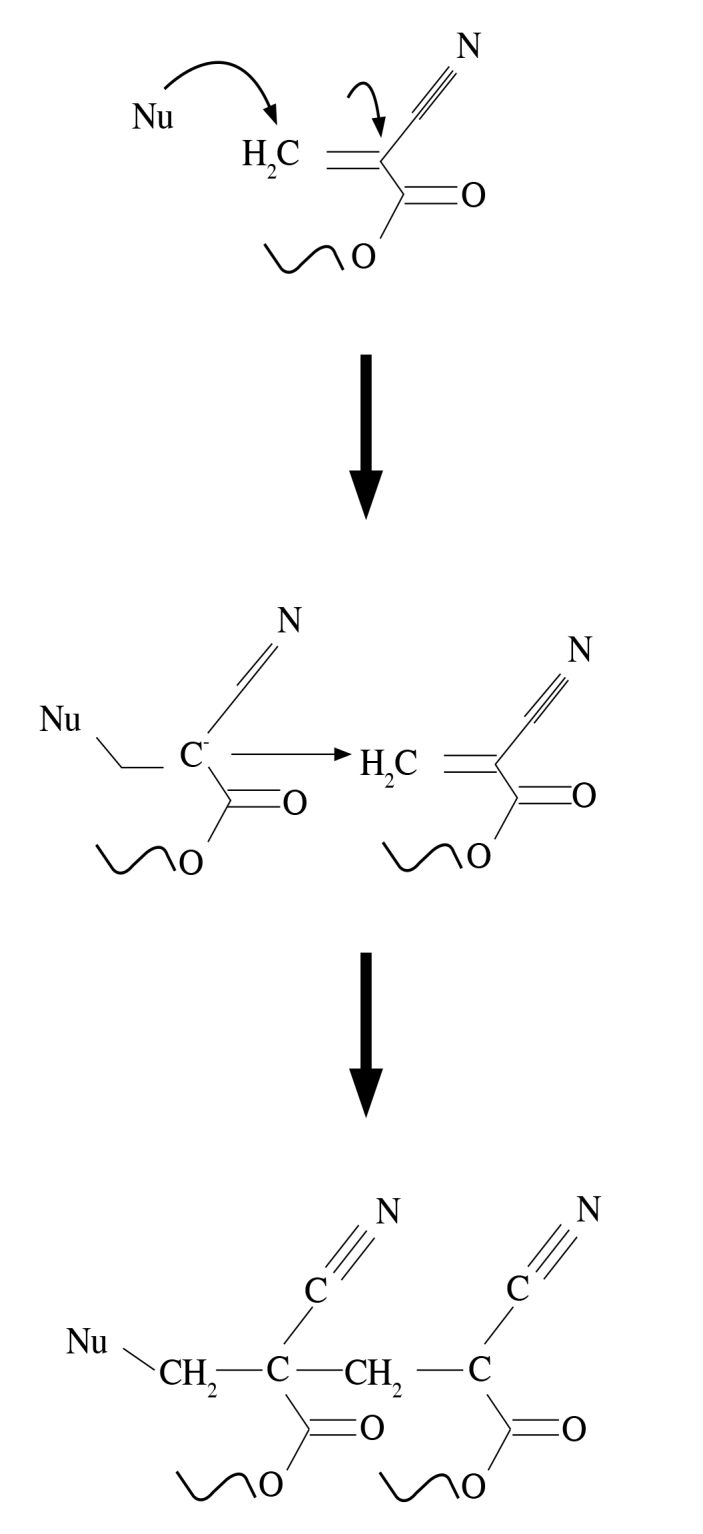
Polymerization of cyanoacrylate glues
Cyanoacrylic glues ensure high degree, and strong bonding to biologic tissues when compared with other adhesives. CAs have short (methyl-2 or ethyl-2), and long-chain (n-butyl-2, and n-octyl-2) forms. Thanks to polymerization mechanism, when they get contact with blood or water contained in the tissue they form a very tight cover. Short-chain forms are rarely used. Because they are very rapidly degrade, and subsequent formation of formaldehyde is very toxic. However long-chain forms degrade slowly, and have minimal toxic effects. They can be easily used in topical applications for closure of the skin defects. A paramount increase in the use of long-chain CAs has been reported.[14]
In recent years Glubran® (General Enterprise Marketing, Viareggio, Lucca, Italy) which was developed to minimize toxic effect of CA glues contains ethyl-2-cyanoacrylate, butyl acrylate, and methacryloxysulphalan, while Glubran-2® (General Enterprise Marketing, Viareggio, Lucca, Italy) comprise combination of n-butyl cyanoacrylate, and methacryloxysulpholen monomers.[15–17] In a study by Kull et al.[18] it has been proved in all tests that Glubran-2® creates a high tensile strength between biologic tissues, and polymerized film layer with resultant increased bonding capability. In tension tests higher breaking strength of polymerized adhesive has been acceptedly emphasized.
Biocompatibility of Glubran® and Glubran-2®, their cytotoxicity, their compatibility with blood, and their antimicrobial activities have been tested In in vitro biochemical studies performed using ‘neutral red uptake test’, any toxic effect of Glubran® and Glubran-2® extracts was not observed when they were applied at 1:10 dilution on L929 cells incubated on culture media. Both adhesives decrease partial thromboplastin time (APTT) significantly. Therefore desired hemostasis is achieved. Decrease in APTT exerts a hemostatic effect, and therefore it contributes to tissue adhesion induced by adhesives. On the other hand, any negative effect on the activity of prothrombin, fibrinogen levels, platelet, total and subgroup leucocyte counts has not been reported. Therefore they don’t have hemolytic effects. Glubran®, and Glubran-2® exert similar effects on blood parametres.[15,19] Montanaro et al.[15] reported that when used at high concentrations, adhesives may have cytotoxic effects, however when they are diluted they may lead to adverse effects at an acceptable level. On the other hand they confirmed that when used intensively, adhesives have acceptable levels of tissue compatibility.[15,19]
Toxicity
Cyanoacrylates interact with tissue. Smokes appearing after reaction of CAs with tissue, are caused by vaporization of CA monomers, and they irritate sensitive membranes of eyes, nose, and throat. They polymerize, and lose their toxic effects instantaneously when they get contact with moisture in the membranes. In order to minimize these risks aeration should be very well ensured when CA is used. In nearly 5% of those who are exposed continuously to the effects of CA, sensitivity to CA can develop which lead to flu-like symptoms. It may irritate skin, and lead to allergic cutaneous reactions. Rarely it may trigger asthmatic crisis.[20] Association Advancing Occupational and Environmental Health (ACGIH) has determined its exposure limit as 200 per one billion particles. For all CA glues only one criterion of toxicity does not exist. Presence of very different CA formulas lead to formulation of multiple number of glues. As indicated by ‘United States National Toxicology Programme’ and ‘United Kingdom Health ve Safety Executive’ though ECAs have short-chain structures, when complied with instructions for use, their application is safe, therefore conduction of additional study is not required.[20] Since 2-OCA compounds has a longer organic skeleton, they dissolve very slowly, and can not reach tissue toxicity threshold levels (Table 2).
Their use in Urologic Diseases
Cyanoacrylates are glues have a single component. They rapidly dry up (within 2–50 seconds) and do not contain any solvent. They have a higher thermal resistance. Besides they ensure adhesion even with a little amount of glue, and penetrate into even very small gaps. In urologic practice, ethyl, and n-butyl versions of Glubran® and Glubran-2® are used. Firstly, they were developed, and used during World War II.[17] As soon as they get contact with air, blood, and tissues, they react rapidly with these media, and start to be polymerized. Within 60–90 seconds they form a resistant film layer with a higher tensile strength.[15–17] They are highly adhesive synthetic lucent fluids with hemostatic properties. On wet places, and moist environments they form a tension-resistant film layer with antibacterial properties which does not allow passage of fluid.[21] Owing to their hemostatic, embolic, and adhesive properties their use in urology conveys importance, and butyl, and esther forms are frequently employed.[17,22] Optimal polymerization temperature of CA glue is 45°C, and it has antiseptic properties.[23] In 1998 FDA approved use of 2-octyl-cyanoacrylate for the closure of external wounds, and surgical incisions.[17]
Experimental Studies
Testes
In an experiment performed on rats by Ayyıldız et al.[24] the authors applied Glubran-2® on testicular tissue, and tunica albuginea, and demonstrated that Glubran-2® had exerted adverse effects on testicular tissue, seminiferous tubuli, impaired spermatogenesis, tunica albuginea, and caused testicular calcification. They indicated necessity of exercising utmost care during testicular applications.[24]
Penile tissue
Akgül et al.[25] examined effectiveness of Glubran 2® in cavernosal surgery in the management of experimental penile fracture, and reported its favourable effect on healing thanks to its hemostatic, adhesive, and anti-inflammatory properties. It decreases development of fibrosis. The development of reaction to foreign substance was reported at a lesser frequency.[25,26] Excellent results had been obtained from pathological analysis performed during acute phase. Its long-term penile tissue reactions should be evaluated, and mating of rats should be observed.[25] Its long-term effects on erection should be overseen.
Urethra and spongiosal tissue
In the same study, Ayyıldız et al.[24] applied Glubran 2® on urethra, and spongiosal tissue of injury-induced rats, and demonstrated that healing of tissues had been excellently, and favourably effected. Their study has substatiated easy applicability of Glubran 2® mainly in hypospadias, then all urethral surgeries, and penile tissues.[24]
Renal artery occlusion
In an experimental animal study, Cylwik et al.[27] embolized renal arteries with CA glue delivered through catheterization, and histopathological evaluation performed 3 months later revealed that adhesive was not resorbed at all. Seven days later they observed degeneration of collagen, elastic fibers, and reticulin, and development of tumefaction. While 24 hours later inflammatory process had started, and 2–3 months later secondary collagenation, and hyalinization were observed. Inflammation forms at the perivascular area. Two-three months later progressive atrophy of nephrons, and parenchymal fibrosis develop without occurrence of renal infarction.[27]
Applications on Patients (Table 3)
Table 3.
Indications of use for cyanoacrylate glues in urology
| Indications of use for cyanoacrylate glues in urology |
|---|
| Indications |
| Circumcision |
| Urinary fistulas |
| Enteric fistulas |
| Lymphocele |
| Endoscopic procedures |
| Laparoscopy |
| Bladder tumor excision –bleeding |
| Urethrocutaneous fistulas |
| Partial nephrectomy |
| Tumor rupture |
| Varicocele |
| Arterio-venous fistulas |
| Hypospadias |
| Priapism |
| Skin closure |
| Pediatric urology |
| Mesh fixation |
Circumcision
In recent years, tissue adhesives have been more prevalently used because of their easy applicability, their ability to shorten procedures, and excellent cosmetic outcomes relative to standard suturing techniques.[28–30] Especially their antimicrobial effects on gram-positive bacteria are very important for wound care.[31] Decrease in the incidence of sinus formation, and tissue granulation is another important advantage of these adhesives.[32] The above-mentioned problems developing during circumcision using laser, have been overcomed by additional use of tissue adhesives. On the other hand they prevent the risk of development of hematoma, and suture-related adhesions.[33] Kelly et al.[32] used CA glues in 502 cases whom they performed suturless circumcision operations, and couldn’t encounter postoperative complications as hematoma, and bleeding. Görgülü et al.[33] used CA after circumcisions they performed using laser, and reported complications only at a minimum level. They reported incredibly low rates of hematoma, and bleeding (0%) with combination therapy, while in standard treatment incidence rates of hematoma, and bleeding were reported as 1.4, and 2.2%, respectively. In the combination group in 0.8% cases of dehiscence of circumcision site was seen.[33]
Urinary fistulas
Bardari et al.[21] used Glubran® in 3 cases, and published their results. The first patient had undergone suprapubic prostatectomy for BPH. This patient had previously undergone abdominoperineal resection for rectum carcinoma, and a fistula had developed between prostate loge, and perineum. A ureteral catheter with two open ends was placed in the fistula, and fistula was closed with CA glue when the bladder was empty without any complication. The other two cases had undergone radical cystoprostatectomy. One of them developed a fistula between neobladder and urethra, and urine leakage at the site of anastomosis between neobladder, and urethra had been detected. Since fistulas had stemmed from neobladder, the application was performed when the neobladder was fully distended Warm physiologic saline was used during application of the adhesive glue to achieve rapid polymerization. In all three cases 2 mL Glubran® achieved adequate healing. Urethral catheters were left dwelling for 2–7 days, and uneventful healing was achieved.[21] During an average follow-up period of 21 months, in none of the patients urinary leakage, fistula, stone formation, and any other side effect were seen.[21]
Muto et al.[34] used CA glues via endoscopic, percutaneous, and endovaginal routes for urinary fistulas developed due to different etiologies. They treated 13 patients with iatrogenic, and inflammatory urinary fistulas using 1–3 mL Glubran®. They also emphasized that they had achieved complete success for long fistulas narrower than 1 cm, while in 2 cases with larger, and short fistulas this treatment had failed. During average follow-up period of 35 months, any recurrence was not seen in successful cases. The authors stressed that CA glues are safe, and provide minimally invasive occlusive treatment which can be applied via endoscopic, percutaneous, and endovaginal. They also underlined that these adhesives should be considered as a first option in the treatment of urinary fistulas.[34]
It was demonstrated that vesicocutaneous fistula (2 cases) occurring following surgery performed to correct bladder extrophy was closed with deepitelization after use of adhesive glue. Safe use of Glubran 2® in pediatric cases has been also emphasized.[35]
Incidence of anastomotic leakage following radical prostatectomy has been reportedly range between 3.5, and 23 percent.[36] Lim et al.[37] presented 10 (0.5%) patients whose vesicourethral anastomotic leakage developed after radical prostatectomy (total n=1828) was successfully treated under local anesthesia using nBCA (Histoacryl®), and fibrin adhesive applied with the aid of cystoscopy (Figure 3). They indicated that before application of Histoacryl, they had instilled 5% dextrose through catheter to refrain from premature polymerization of CA, and freezing of nBCA which facilitated realization of this application. The authors observed development of a bladder stone because of migration of the adhesive into bladder.[37] Formation of bladder stone had been associated with the use of fibrin adhesives. Still authors recommend that every possibility should be checked to discard potential migration of Histoacryl® into bladder lumen.[37] Besides, use of lipiodol together with CA glues offers the advantage of radiographic visualization.[37]
Figure 3.
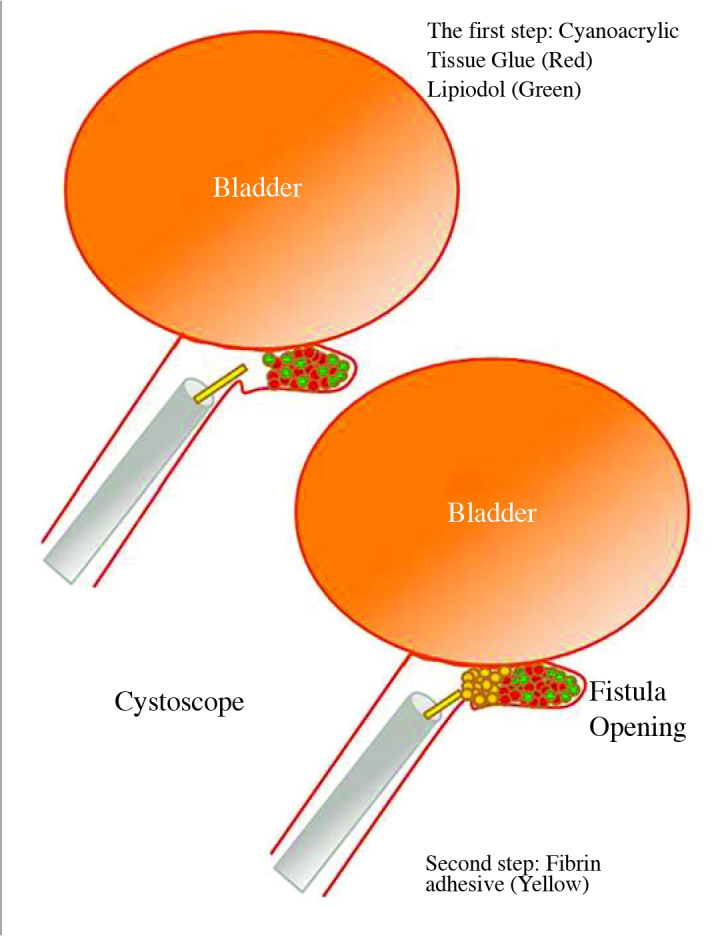
Application for urethroperineal fistula[37]
Enteric fistulas
Generally, they occur after any surgical treatment of gastrointestinal system. It is one of the serious complications of abdominal surgery. Reoperation increases both morbidity, and mortality rates.[38,39] Besides, they delay patients’return to their social activities, and prolong hospital stay. If second operation also fails, then the risk of morbidity, and mortality will also tremendously increase. Therefore CA glues were used to shorten closure time of the fistula, and also prevent a second operation.[38–40] Previously, foams, and fibrin adhesives had been used to close enteric fistulas temporarily. These agents do not provide tensile, and bonding strength as achieved with CA glues.[15,16] Mauri et al.[40] analyzed three cases that developed enteric fistulas after gastrointestinal cancer surgery in consideration of chemical, and physical characteristics of Glubran 2®. Treatment was successful immediately after treatment in two, and in the long-term in one case. The authors indicated CA glues as the most ideal agents for the closure of this kind of fistulas.[40] They also stated that for optimal utilization of CA substrates, and ensure their adhesion to neighbouring tissues, before embolization, and application, collections of fluid or abscess should be completely drained. The auathors added a few drops of lipiodol on the adhesive to ensure visualization. Even though this procedure was applied on scarce number of patients, they performed this procedure under radiographic visualization. They demonstrated that this technique will potentially help to shorten healing process of postoperative enteric fistulas, and decrease the number of reoperations.[40]
Lymphocele
Efficacy of CAs for the treatment of lymphorrhea, and lymphocele developed after pelvic, and retroperitoneal lymphadenectomy, and also for the hemostatic control of hematomas developed following pelvic surgery has been also indicated.[21]
Endoscopic application
Polymerization is accomplished more rapidly in full bladder, and wet environment. This condition facilitates realization of polimerization suitable for endoscopic use. Placement of adhesive glue does not constitute a risk in cases with full bladder.[21]
Laparoscopy
In a comprehensive study where 1347 cases from 26 centers who had undergone laparoscopic partial nephrectomy were evaluated, LPN was emphasized as a relatively challenging technique which carries risk of important complications as bleeding requiring transfusion, and urine leakage, and also concerns about need for ablation, and reconstruction exist.[41] When these cases are analyzed in detail, we see that Glubran® has been used singly or in combination with fibrin adhesives in series with 15, 34, and 36 cases. In recent years, studies have investigated the role of newly introduced tissue adhesives, and proved that when they were used for hemostasis, and repair of the collecting system, they increased success rates, and decreased complication rates in addition to their safe use in LPN.[42] In their series of 23 cases who had undergone LPN, Košina et al.[43] reported that Glubran 2® was a safe, and effective adhesive, and during long-term follow-up, they didn’t encounter tumor recurrence without any additional serious financial burden on treatment expenditures.
Endoscopic Resection of Bladder Tumor
Carmignani et al.[44] performed nephroureterectomy in a 81-year-old patient with a grade 3, stage pT3N0M0 transitional cell carcinoma (TCC) of the bladder who were using heparin because of varices of his lower extremities. During TUR-M performed for TCC recurrence, arterial bleeding occurred which couldn’t be terminated with endoscopic techniques. Subsequently based on previous experiences 3 mL Glubran-2® was injected 3 mm deep around bleeding area which completely stopped bleeding. The authors indicated that they experienced similar cases before, and obtained favourable results. They emphasized that if bleedings occurring during cystoscopic procedures can not be controlled by using any means, the first alternative should be CA glues. They also demonstrated that during this application bladder should be full, and distended for 90 seconds so as to allow the adhesive to stick to the bladder wall, and form a film layer.[44]
Ureterocutaneous fistula
Ureterocutaneous fistula is a rarely seen complication of renal surgery. For the treatment of fistula developed in a 33-year-old female patient, 2 mL CA glue was delivered through urethral lumen via retrograde endoscopic approach into the fistula tract. The authors demonstrated closure of fistula one week later, and also complete symptomatic relief was observed during 5 months of follow-up. They reported that this is a suitable, and effective approach in the management of ureterocutaneous fistulas.[45]
Open partial nephrectomy
Košina et al.[43] used CA glues to prevent bleeding, and urine leakage in patients who were switched from laparoscopic to open partial nephrectomy. They reported that outcomes were comparable to those obtained with laparoscopic surgery without any occurrence of bleeding, and urine leakage during postoperative period, and tumor recurrence within 3 years of follow-up.
Embolization of varicocele
Favard et al.[46] retrospectively compared three CA glues including Glubran 2®’ used for the embolization of varicocele, and reported minimum pain on 1., 7., and 30. days after embolization in all cases with shorter scopy times. Recurrence rates of varicoceles at 25. months of the follow-up period were statistically significantly lower in patients for whom Glubran 2® was used relative to other adhesive glues. Glubran 2® induces a local inflammatory reaction characterized by sclerosis, and thrombosis which does not cause more severe pain when compared with other embolic agents. Glubran 2® cyanoacrylate glue provides rapid, and practical application in the embolization of varicoceles in addition, it exposes patients to lower doses of radiation, and leads to decreased recurrence rates.[46]
Arteriovenous Malformations
Transcatheter embolization was performed using Glubran-2® for a young patient with diagnosis of pelvic arteriovenous malformation who had described recurrent episodes of hematuria. All vascular branches involved in pelvic arteriovenous malformation were successfully occluded, symptoms of the patients regressed, and at the end of 6 months of follow-up, permanent occlusion of ÁV malformation was ensured.[47]
Hypospadias
Based on their clinical experience on a scarce number of cases Ayyıldız et al.[24] used Glubran 2® as an adjunct during primary repair of hypospadias, and indicated lack of any contraindication for its use with this indication (unpublished data). On the contrary, Hosseini et al.[35] reported skin necrosis due to overuse of the adhesive in two cases with hypospadias.
Priapism
Gandini et al.[48] performed embolization of fistula using Glubran-2® with the aid of a catheter for the management of arteriovenous fistulas in 2 cases who developed posttraumatic priapism. Cases with priapism were treated successfully 24 hours later. Sexual activity of the patients was regained 30 days later, and they demonstrated permanent closure of arteriovenous fistulas during 12 months of follow-up period.[48]
Skin closure
Recently, 2-octylcyanoacrylate tissue adhesives (2-OCA; Dermabond®, Ethicon, Inc., Sommerville, New Jersey, USA) have being used for the closure of minor lacerations, and minor surgical incisions. Shimizu et al.[49] reported their use of adhesives for the closure of post-radical prostatectomy wounds from the year 2006 on, while before that date they were using staplers. They retrospectively compared the patients for whom they had used staplers (n=133), and 2*OCA (n=101) from the perspective of economic burden. Wound site infection developed in 3 cases for whom they had used adhesives, and 3 patients for whom they used staplers had contracted infections. In one case in the tissue adhesive group wound dehiscence was seen. Use of staplers instead of synthetic adhesives decreases treatment costs considerably with acceptable side effects.[49]
Applications in Pediatric Urology
Prestipino et al.[50], used CA adhesives for hypospadias surgery, and indicated that they could be used as an alternative to suturing with excellent outcomes in that they form extra film layers, and demonstrate strong tissue bonding capabilities. Adhesives form impermeable watertight barriers for body fluids as urine and blood. It is a perfect barrier against feces, and other infectious agents. They reinforce healthy tissue repair, and prevent development of edema, and hematoma. Despite these positive effects, they have found a limited use in pediatric applications. Their applications include closure of surgical incision, circumcision, and closure of urethrocutaneous fistulas developed following hypospadias surgery.[50]
Cyanoacrylates are favourable alternatives for closure of post-circumcision wounds relative to conventional techniques. In addition to their easy applicability, they considerably shorten operative times, and duration of postoperative pain, ensure eventless safe healing, and provide better cosmetic results.[24] Other indication for their use is closure of urethrocutaneous fistula developing after hypospadias surgery.[24,51]
Owing to their tensile strength CAs get contact with all corners of the fistula, healing process with perfect outcomes have been observed. This non-surgical application is really encouraging, and allows closure of fistulas without surgical intervention. This healing process occurs in both short-, and long-standing fistulas. This treatment alleviates anxiety of families, and they can be easily applied without the need for general anesthesia.[22,50]
Besides, their use for the obliteration of processus vaginalis during hydrocelectomy has been also reported.[9–12]
Their use with mesh
In an experimental trial, Kukleta et al.[13] performed mesh fixation in rabbits with CA glue – nBCA (Histoacryl®), and did not observe a reaction in muscle tissue during the acute phase. They reported fibroblastic tissue reaction characterized by mildly or moderately inflammatory cells. Evaluation made 360 days later, had demonstrated a mild increase in fibrotic tissue, and mononuclear cell counts, together with higher number of multinuclear giant cells in certain foci. They revealed disappearance of adhesive in the tissue after ninety days. They used Histoacryl® CA glue in the fixation of meshes during the laparoscopic repair of hernias. For the fixation of meshes 6–8 drops of tissue adhesive had been used instead of suturing in 1336 cases, and favourable results had been obtained, and minimal tissue reaction was reported. Any difference could not be found between tissue adhesives, suturing, and use of staplers. Their study demonstrated suitability of using tissue adhesives as the first alternative based on comparative assessments of benefit, and economic burden.[13]
Application of cyanoacrylate tissue adhesives
Devices are available for superficial, vesical, intraureteral, intraurethral, tissue, intravascular, and laparoscopic applications. Figure 4 shows shows application devices. Besides, ureteral catheters which are frequently used in urology, and needles used for endoscopic treatment of vesicoureteral reflux have been also utilized. The advantages of CA tissue adhesives are shown in Figure 5.
Figure 4.

Application apparatus
Figure 5.
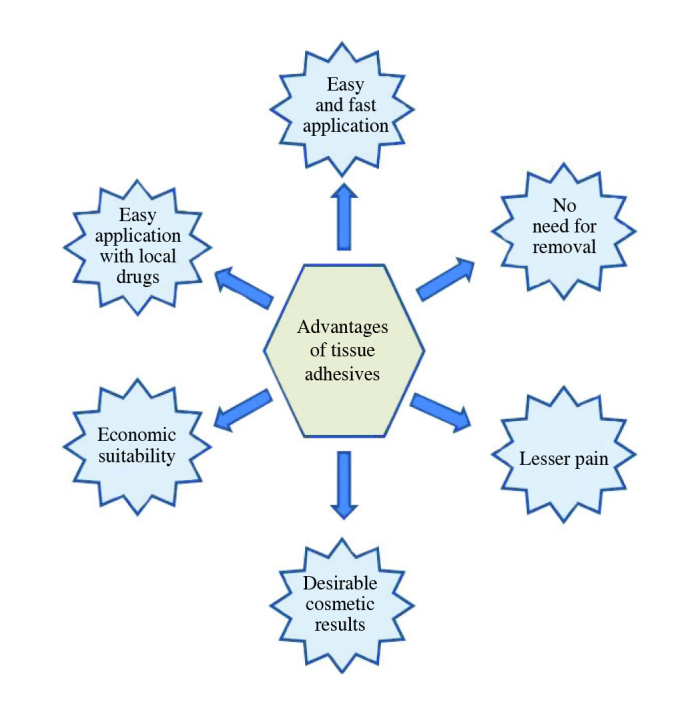
Advantages of CA tissue adhesives
In conclusion, based on the information obtained from studies cited in the literature, their use has been mostly indicated in case reports, and despite favourable, and significant outcomes, standard information on their indications of use in urology is lacking. However as a matter of fact application of newly designed CAs (Glubran®) does not exert harmful effects on tissues. With this fact under consideration, their indications should be investigated based on risk-benefit ratio. Tissue adhesives should be routinely used for the prevention of postoperative bleeding, and implantation of tumor cells when tumoral integrity is disrupted, and also in cases of urine leakage. Prioritization of their use in iatrogenic urethrocutaneous fistulas developed after hypospadias repair decreases morbidity, and mortality. However their use in these indications should not be considered as an alternative to surgery. Thanks to new formulations of both short-, and long-chain CA tissue adhesives, minimal toxic effects have been indicated. When their biochemical characteristics, rapid adhesions to tissues, antiseptic, and hemostatic effects taken into account, their use in daily practice does not appear to be contraindicated. However generally all tissue adhesives do not handle all potential problems. Of course, a good surgical technique is needed. Besides use of radiopaque substances as lipiodol together with CA glues confers an advantage for better visualization of the application site. In addition, it should not be forgotten that for the management of the fistulas with narrow, and long tracts, trial of CA tissue adhesives will offer an important alternative.
Footnotes
Peer-review: This manuscript was prepared by the invitation of the Editorial Board and its scientific evaluation was carried out by the Editorial Board.
Author Contributions: Concept - S.N.A.; Design - S.N.A; Supervision - A.A.; Resources - S.N.A., A.A.; Materials - S.N.A.; Data Collection and/or Processing - S.N.A.; Analysis and/or Interpretation - S.N.A., A.A.; Literature Search - S.N.A., A.A.; Writing Manuscript - S.N.A.; Critical Review - A.A.; Other - S.N.A., A.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Bochynska AI, Hannink D, Grijpma DW, Buma P. Tissue adhesives for meniscus tear repair: an overview of current advances and prospects for future clinical solutions. J Mater Sci. 2016;27:85–102. doi: 10.1007/s10856-016-5694-5. https://doi.org/10.1007/s10856-016-5694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer AJ, McClain SA, Katz A. A porcine epistaxis model: hemostatic effects of octylcyanoacrylate. Otolaryngol Head Neck Surg. 2004;130:553–7. doi: 10.1016/j.otohns.2003.09.035. https://doi.org/10.1016/j.otohns.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 3.Dalvi AA, Faria MM, Pinto AA. Non-suture closure of wound using cyanoacrylate. J Postgrad Med. 1986;32:97–100. [PubMed] [Google Scholar]
- 4.Fischl RA. An adhesive for primary closure of skin incisions: a preliminary report. Plast Reconstr Surg Transplant Bull. 1962;30:607–10. doi: 10.1097/00006534-196211000-00009. https://doi.org/10.1097/00006534-196211000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Rothnie NG, Taylor GW. Sutureless Skin Closure. BMJ. 1963;2:1027–30. doi: 10.1136/bmj.2.5364.1027. https://doi.org/10.1136/bmj.2.5364.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zoccali C, Covello R, Di Francesco A, Zoccali G. A cyanoacrylate and silastic patch to reduce the risk of opening of the tumor: technical note. Eur J Surg Oncol. 2013;39:44–5. doi: 10.1016/j.ejso.2012.08.025. https://doi.org/10.1016/j.ejso.2012.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Available at: https://en.wikipedia.org/wiki/Cyanoacrylate
- 8.Coulthard P, Worthington H, Esposito M, Elst M, Waes OJ. Tissue adhesives for closure of surgical incisions. Cochrane Database Syst Rev. 2004;2:CD004287. doi: 10.1002/14651858.CD004287.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Amiel GE, Sukhotnik I, Kawar B, Siplovich L. Use of N-butyl-2-cyanoacrylate in elective surgical incisions-long term outcomes. J Am Coll Surg. 1999;189:21–5. doi: 10.1016/s1072-7515(99)00068-x. https://doi.org/10.1016/S1072-7515(99)00068-X. [DOI] [PubMed] [Google Scholar]
- 10.Esposito C, Damiano R, Settimi A, De Marco M, Maglio P, Centonze A. Experience with the use of tissue adhesives in pediatric endoscopic surgery. Surg Endosc. 2004;18:290–2. doi: 10.1007/s00464-003-9032-x. https://doi.org/10.1007/s00464-003-9032-x. [DOI] [PubMed] [Google Scholar]
- 11.Miyano G, Yamataka A, Kato Y, Tei E, Lane GJ, Kobayashi H, et al. Laparoscopic injection of dermabond tissue adhesive for the repair of inguinal hernia: short- and long-term follow-up. J Pediatr Surg. 2004;39:1867–70. doi: 10.1016/j.jpedsurg.2004.08.018. https://doi.org/10.1016/j.jpedsurg.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Seewald S, Seitz U, Yang AM, Soehendra N. Variceal bleeding and portal hypertension: still a therapeutic challenge? Endoscopy. 2001;33:126–39. doi: 10.1055/s-2001-11666. [DOI] [PubMed] [Google Scholar]
- 13.Kukleta JF, Freytag C, Weber M. Efficiency and safety of mesh fixation in laparoscopic inguinal hernia repair using n-butyl cyanoacrylate: long-term biocompatibility in over 1,300 mesh fixations. Hernia. 2012;16:153–62. doi: 10.1007/s10029-011-0887-9. https://doi.org/10.1007/s10029-011-0887-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sinha S, Naik M, Wright V, Timmons J, Campbell AC. A single blind, prospective, randomized trial comparing n-butyl 2-cyanoacrylate tissue adhesive (Indermil) and sutures for skin closure in hand surgery. J Hand Surg Br. 2001;26:264–5. doi: 10.1054/jhsb.2000.0572. https://doi.org/10.1054/jhsb.2000.0572. [DOI] [PubMed] [Google Scholar]
- 15.Montanaro L, Arciola CR, Cenni E, Ciapetti G, Savioli F, Filippini F, et al. Cytotoxicity, blood compatibility and antimicrobial activity of two cyanoacrylate glues for surgical use. Biomaterials. 2001;22:59–66. doi: 10.1016/s0142-9612(00)00163-0. https://doi.org/10.1016/S0142-9612(00)00163-0. [DOI] [PubMed] [Google Scholar]
- 16.Loffroy R. Using Glubran 2 acrylic glue to maximize results of transcatheter arterial embolization for refractory upper gastrointestinal bleeding. Scand J Gastroenterol. 2015;50:1306–7. doi: 10.3109/00365521.2015.1040996. https://doi.org/10.3109/00365521.2015.1040996. [DOI] [PubMed] [Google Scholar]
- 17.Pursifulla NF, Moreyb AF. Tissue glues and nonsuturing techniques. Curr Opin Urol. 2007;17:396–401. doi: 10.1097/MOU.0b013e3282f0d683. https://doi.org/10.1097/MOU.0b013e3282f0d683. [DOI] [PubMed] [Google Scholar]
- 18.Kull S, Martinelli I, Briganti E, Losi P, Spiller D, Tonlorenzi S, et al. Glubran-2 surgical glue: in vitro evaluation of adhesive and mechanical properties. J Surg Res. 2009;157:e15–21. doi: 10.1016/j.jss.2009.01.034. [DOI] [PubMed] [Google Scholar]
- 19.Pascual G, Sotomayor S, Rodríguez M, Pérez-Köhler B, Kühnhardt A, Fernández-Gutiérrez M, et al. Cytotoxicity of cyanoacrylate-based tissue adhesives and short-term preclinical in vivo biocompatibility in abdominal hernia repair. PLoS One. 2016;11:e0157920. doi: 10.1371/journal.pone.0157920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Available at: http://www.ca-plus.com/faq.html
- 21.Bardari F, D’Urso L, Muto G. Conservative treatment of iatrogenic urinary fistulas: the value of cyanoacrylic glue. Urology. 2001;58:1046–8. doi: 10.1016/s0090-4295(01)01399-1. https://doi.org/10.1016/S0090-4295(01)01399-1. [DOI] [PubMed] [Google Scholar]
- 22.Lapointe SP, N-Fékété C, Lortat-Jacob S. Early closure of fistula after hypospadias surgery using N-butyl cyanoacrylate: preliminary results. J Urol. 2002;168:1751–3. doi: 10.1097/01.ju.0000028339.08334.d7. https://doi.org/10.1097/00005392-200210020-00024. [DOI] [PubMed] [Google Scholar]
- 23.Bady S, Wongworawat MD. Effectiveness of antimicrobial incise drapes versus cyanoacrylate barrier preparations for surgical sites. Clin Orthop Relat Res. 2009;467:1674–7. doi: 10.1007/s11999-009-0768-z. https://doi.org/10.1007/s11999-009-0768-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayyildiz A, Nuhoğlu B, Cebeci O, Caydere M, Ustün H, Germiyanoğlu C. The effect of cyanoacrylic glue on rat testis, urethra and spongiosal tissue: an experimental study. J Urol. 2006;175:1943–7. doi: 10.1016/S0022-5347(05)00921-3. https://doi.org/10.1016/S0022-5347(05)00921-3. [DOI] [PubMed] [Google Scholar]
- 25.Akgül T, Ayyildiz A, Cebeci O, Nuhoğlu B, Ozer E, Germiyanoğlu C, et al. Effect of cyanoacrylic glue on penile fracture: an experimental study. J Urol. 2008;180:749–52. doi: 10.1016/j.juro.2008.03.181. https://doi.org/10.1016/j.juro.2008.03.181. [DOI] [PubMed] [Google Scholar]
- 26.Zhu H, Yang XJ, Li XL, Zhang HX, Zheng FY. Non-suture technique for rabbit oviduct anastomosis with 2-octyl cyanoacrylate: a histopathologic and biomechanical analysis. J Obstet Gynaecol Res. 2013;39:685–91. doi: 10.1111/j.1447-0756.2012.02002.x. https://doi.org/10.1111/j.1447-0756.2012.02002.x. [DOI] [PubMed] [Google Scholar]
- 27.Cylwik B, Darewicz J, Karasewicz B. Morphometric and histological examinations of dog kidneys after embolization of the renal artery with the cyanoacrylic glue “Chirurcoll-Polfa”. Int Urol Nephrol. 1985;17:303–9. doi: 10.1007/BF02083498. https://doi.org/10.1007/BF02082479. [DOI] [PubMed] [Google Scholar]
- 28.Toriumi DM, O’Grady K, Desai D, Bagal A. Use of octyl-2-cyanoacrylate for skin closure in facial plastic surgery. Plast Reconstr Surg. 1998;102:2209–19. doi: 10.1097/00006534-199811000-00062. https://doi.org/10.1097/00006534-199811000-00062. [DOI] [PubMed] [Google Scholar]
- 29.Maw JL, Quinn JV, Wells GA, Ducic Y, Odell PF, Lamothe A, et al. A prospective comparison of octylcyanoacrylate tissue adhesive and suture for the closure of head and neck incisions. J Otolaryngol. 1997;26:26–30. [PubMed] [Google Scholar]
- 30.Bruns TB, Worthington JM. Using tissue adhesive for wound repair: a practical guide to dermabond. Am Fam Physician. 2000;61:1383–8. [PubMed] [Google Scholar]
- 31.Quinn JV, Osmond MH, Yurack JA, Moir PJ. N-2-butylcyanoacrylate: risk of bacterial contamination with an appraisal of its antimicrobial effects. J Emerg Med. 1995;13:581–5. doi: 10.1016/0736-4679(95)80025-5. https://doi.org/10.1016/0736-4679(95)80025-5. [DOI] [PubMed] [Google Scholar]
- 32.Kelly BD, Lundon DJ, Timlin ME, Sheikh M, Nusrat NB, D’Arcy FT, et al. Paediatric sutureless circumcision-an alternative to the standard technique. Pediatr Surg Int. 2012;28:305–8. doi: 10.1007/s00383-011-3015-0. https://doi.org/10.1007/s00383-011-3015-0. [DOI] [PubMed] [Google Scholar]
- 33.Gorgulu T, Olgun A, Torun M, Kargi E. A fast, easy circumcision procedure combining a CO2 laser and cyanoacrylate adhesive: a non-randomized comparative trial. IBJU. 2006;42:113–7. doi: 10.1590/S1677-5538.IBJU.2015.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muto G, D’Urso, Castelli E, Formiconi A, Bardari F. Cyanoacrylic glue: a minimally invasive nonsurgical first line approach for the treatment of some urinary fistulas. J Urol. 2005;174:2239–43. doi: 10.1097/01.ju.0000181809.51544.20. https://doi.org/10.1097/01.ju.0000181809.51544.20. [DOI] [PubMed] [Google Scholar]
- 35.Hosseini SM, Bahador A, Foroutan HR, Sabet B, Geramizadeh B, Zarenezhad M. The application of a new cyanoacrylate glue in pediatric surgery for fistula closure. Iran J Med Sci. 2011;36:54–6. [PMC free article] [PubMed] [Google Scholar]
- 36.Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P. Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol. 2012;62:1–15. doi: 10.1016/j.eururo.2012.02.029. https://doi.org/10.1016/j.eururo.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 37.Lim JH, You D, Jeong IG, Park HK, Ahn H, Kim CS. Cystoscopic injection of N-butyl-2-cyanoacrylate followed by fibrin glue for the treatment of persistent or massive vesicourethral anastomotic urine leak after radical prostatectomy. Int J Urol. 2013;20:980–5. doi: 10.1111/iju.12094. https://doi.org/10.1111/iju.12094. [DOI] [PubMed] [Google Scholar]
- 38.Falconi M, Pederzoli P. The relevance of gastrointestinal fistulae in clinical practice: a review. Gut. 2001;49(Suppl 4):2e10. doi: 10.1136/gut.49.suppl_4.iv2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schecter WP, Hirshberg A, Chang DS, Harris HW, Napolitano LM, Wexner SD, et al. Enteric fistulas: principles of management. J Am Coll Surg. 2009;209:484e91. doi: 10.1016/j.jamcollsurg.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 40.Mauri G, Sconfienza LM, Fiore B, Brambilla G, Pedicini V, Poretti D, et al. Post-surgical enteric fistula treatment with image-guided percutaneous injection of cyanoacrylic glue. Clinical Radiology. 2013;68:59e63. doi: 10.1016/j.crad.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 41.Gill IS, Matin SF, Desai MM, Kaouk JH, Steinberg A, Mascha E, et al. Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol. 2003;170:64–8. doi: 10.1097/01.ju.0000072272.02322.ff. https://doi.org/10.1097/01.ju.0000072272.02322.ff. [DOI] [PubMed] [Google Scholar]
- 42.Breda A, Stepanian SV, Lam JS, Liao JC, Gill IS, Colombo JR, et al. Use of Haemostatic Agents and Glues during Laparoscopic Partial Nephrectomy: A Multi-Institutional Survey from the United States and Europe of 1347 Cases. Eur Urol. 2007;52:798–803. doi: 10.1016/j.eururo.2007.02.035. https://doi.org/10.1016/j.eururo.2007.02.035. [DOI] [PubMed] [Google Scholar]
- 43.Košina J, Pacovský J, Hušek P, Holub L, Broďák M. Tissue cyanoacrylate glue in partial nephrectomy - our own experience and assessment. Rozhl Chir. 2016;95:79–82. [PubMed] [Google Scholar]
- 44.Carmignani L, Acquati P, Rocco F. Case report: Cystoscopic use of cyanoacrylate glue for bleeding during transurethral resection of bladder tumors. J Endourol. 2006;20:923–4. doi: 10.1089/end.2006.20.923. https://doi.org/10.1089/end.2006.20.923. [DOI] [PubMed] [Google Scholar]
- 45.Omar M, Abdulwahab-Ahmed A, El Mahdey Ael D. Endoscopic management of a chronic ureterocutaneous fistula using cyanoacrylic glue. Cent European J Urol. 2014;67:430–2. doi: 10.5173/ceju.2014.04.art25. https://doi.org/10.5173/ceju.2014.04.art25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Favard N, Moulin M, Fauque P, Bertaut A, Favelier S, Estivalet L, et al. Comparison of three different embolic materials for varicocele embolization: retrospective study of tolerance, radiation and recurrence rate. Quant Imaging Med Surg. 2015;5:806–14. doi: 10.3978/j.issn.2223-4292.2015.10.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gandini R, Angelopoulos G, Konda D, Messina M, Chiocchi M, Perretta T, et al. Transcatheter embolization of a large symptomatic pelvic arteriovenous malformation with Glubran 2 acrylic glue. Cardiovasc Intervent Radiol. 2008;31:1030–3. doi: 10.1007/s00270-007-9224-1. https://doi.org/10.1007/s00270-007-9224-1. [DOI] [PubMed] [Google Scholar]
- 48.Gandini R, Spinelli A, Konda D, Reale CA, Fabiano S, Pipitone V, et al. Superselective embolization in posttraumatic priapism with glubran 2 acrylic glue. Cardiovasc Intervent Radiol. 2004;27:544–8. doi: 10.1007/s00270-003-0210-y. https://doi.org/10.1007/s00270-003-0210-y. [DOI] [PubMed] [Google Scholar]
- 49.Shimizu T, Masumori N, Hirobe M, Hashimoto K, Maeda T, Fukuta F, et al. Use of 2-octylcyanoacrylate tissue glue for skin closure in radical retropubic prostatectomy. Hinyokika Kiyo. 2010;56:495–8. [PubMed] [Google Scholar]
- 50.Prestipino M, Bertozzi M, Nardi N, Appignani A. Outpatient department repair of urethrocutaneous fistulae using n-butylcyanoacrylate (NBCA): A single-centre experience. BJU Int. 2011;108:1514–7. doi: 10.1111/j.1464-410X.2010.10083.x. https://doi.org/10.1111/j.1464-410X.2010.10083.x. [DOI] [PubMed] [Google Scholar]
- 51.Elemen L, Seyidov TH, Tugay M. The advantages of cyanoacrylate wound closure in circumcision. Pediatr Surg Int. 2011;27:879–83. doi: 10.1007/s00383-010-2741-z. https://doi.org/10.1007/s00383-010-2741-z. [DOI] [PubMed] [Google Scholar]


