Abstract
Background
Anhedonia is a cardinal feature of major depression and is hypothesized to be driven by low motivation, in particular blunted reward sensitivity. It has been suggested to be a marker that represents a genetic predisposition to this disorder. However, little is known about the mechanisms underlying this heightened risk in unaffected first-degree relatives of patients with major depression. We previously demonstrated abnormal reward biases in acutely depressed patients. The present study aimed to examine the development of reward bias in first-degree relatives of patients with major depression.
Methods
Forty-seven first-degree relatives of patients with major depression (26 females, age 18-52) and 60 healthy controls with no family history of depression (34 females, age 21-48) were recruited. A probabilistically rewarded difficult visual discrimination task, in which participants were instructed about the contingencies, was used to assess blunted reward sensitivity. A response bias towards the more frequently rewarded stimulus (termed “reward bias”) was the primary outcome variable in this study. Participants also completed self-reported measures of anhedonia and depressive symptoms.
Results
Compared with the control group, relatives of patients with major depression with sub-clinical depressive symptoms displayed a blunted reward bias. Relatives without symptoms displayed largely intact motivational processing on both self-report and experimental measures. The degree of anhedonia was associated with attenuated reward bias in first-degree relatives of patients with major depression, especially in those with sub-clinical symptoms.
Limitations
The study did not include a depressed patient group, which restricted our ability to interpret the observed group differences.
Conclusions
Blunted reward sensitivity may be largely manifested in a subgroup of relatives with high levels of depressive symptoms.
Keywords: Depression, Reward, Anhedonia, Risk factors
1. Introduction
Individuals closely related to patients with major depressive disorder (MDD) are at a nearly three-fold greater risk of developing depression than the general population (Weissman et al., 2006). Studying unaffected individuals with a family history of MDD may provide clues to the mechanisms underlying risk for MDD (Lisiecka et al., 2013). Several studies have shown that, compared with individuals without a family history of psychiatric disorders, unaffected first-degree relatives of MDD patients are characterized by elevated neuroticism and depressive cognitive styles, and that these traits are stable over time (Lauer et al., 1998). Relatives of MDD patients also display a range of neurobiological abnormalities similar to those observed in patients with MDD (Baare et al., 2010; Frokjaer et al., 2009; Lisiecka et al., 2012; Mannie et al., 2011), suggesting a possible genetic basis for these traits.
Among the various clinical features of patients with MDD, decreased hedonic and motivational capacity, or anhedonia, has been proposed as a potential risk factor (Hasler et al., 2004). Anhedonia is often prodromal to major depression (Dryman and Eaton, 1991), can be relatively stable across episodes (Oquendo et al., 2004), commonly occurs in depression and other psychiatric syndromes (Fawcett et al., 1983; Loas et al., 1999), and has important implications for understanding the efficacy of antidepressant therapy and development of depression (Martinotti et al., 2012; Miller, 2007). A large body of research has confirmed that depression is characterized by deficits in motivational processing and dysregulation of the brain's reward system (Eshel and Roiser, 2010). Behavioural studies have revealed that individuals with depression exhibit deficits in establishing a reward bias (Liu et al., 2011; Pizzagalli et al., 2009b), and in reward-related decision-making (Forbes et al., 2007). Disrupted reward processing also predicts the future development of depressive symptoms (Forbes et al., 2007; Pizzagalli et al., 2005; Vrieze et al., 2013). In addition, neuroimaging studies have consistently shown that anhedonic symptoms, but not depressive symptoms per se, are negatively correlated with ventral striatal activation in patients with MDD (Dowd and Barch, 2010; Epstein et al., 2006; Harvey et al., 2010; Keedwell et al., 2005; Wacker et al., 2009), with a similar pattern observed in non-clinical samples (Chentsova-Dutton and Hanley, 2010; Harvey et al., 2007).
Preliminary evidence suggests that individuals at genetic risk of depression may also experience motivational disturbance, consistent with the hypothesis that it may be a trait marker for this disorder. TREK1 genotype is associated with higher levels of anhedonic symptoms (Dillon et al., 2010), and results from a twin study (Bogdan and Pizzagalli, 2009) support the notion that anhedonia is heritable and a predisposing vulnerability factor for depression (Loas, 1996). Familial risk for depression is also associated with altered neural responses during reward and punishment processing (Foti et al., 2011; Gotlib et al., 2010; Luking et al., 2015; McCabe et al., 2012). However, it is also clear that dysfunctional reward processing is also observed in other psychiatric disorders, including schizophrenia (Barch et al., 2014; Wang et al., 2015) and bipolar disorder (Di Nicola et al., 2013; Pizzagalli et al., 2008b). Indeed, anhedonia has been reported to be a stable clinical feature in schizophrenic illness (Herbener and Harrow, 2002) and a trait-like feature in bipolar disorder, occurring across euthymic and depressive illness states (Di Nicola et al., 2013); although the similarities in motivational symptoms could conceivably be driven by different pathological mechanisms in different disorders (Whitton et al., 2015). More research is needed to understand how specific components of motivational dysfunction relate to specific neural and cognitive systems in depression (e.g., the positive valence systems construct proposed to underlie anhedonia) (Insel et al., 2010), and to familial risk for MDD (Luking et al., 2015).
In the clinical definition provided by the DSM-IV (APA, 1994), anhedonia, namely the loss of interest (i.e. motivation) or pleasure (i.e. hedonic response) in previously enjoyable activities, is not a unitary construct. Theoretical models dating back to the work of Donald Klein have posited that deficits in hedonic capacity in depression encompass both anticipatory and consummatory processing (Klein, 1984). Whether deficits in reward processing are driven primarily by low anticipatory “wanting” or reduced consummatory “liking” is currently unclear (Berridge and Robinson, 1998; Berridge et al., 2009), but recent research probing motivation, reinforcement learning and reward-based decision-making suggests that anhedonia is most closely linked to abnormalities in reward anticipation rather than consummation (Whitton et al., 2015). A study in a student population suggested a link between anhedonia and low levels of reward anticipation (Chentsova-Dutton and Hanley, 2010) and patients with MDD showed unwillingness to exert effort to obtain rewards, suggestive of impairments in motivation and reward-based decision-making (Treadway et al., 2012). However, a neuroimaging study in MDD using a monetary task that dissociates the anticipatory and consummatory phases of reward processing found reduced striatal activation to reward gains mainly during the consummatory phase of reward processing (Pizzagalli et al., 2009a); although notably reward-related speeding, often interpreted as reflecting motivation, was also attenuated in MDD in this study.
To further examine the role of reward processing as a potential vulnerability factor in depression, it is necessary to establish disrupted reward processing in unaffected first-degree relatives of depression (Hasler et al., 2004), which can be achieved by using specific clinical anhedonia measures in combination with behavioural tasks that tap motivational processing. Similar to our previous study (Liu et al., 2011), reward sensitivity was assessed here by participants' ability to modulate their responses to reward (i.e. generate a response bias) on a rewarded signal detection task with known reinforcement contingencies. We measured two components of trait anhedonia (anticipatory and consummatory anhedonia) using the Temporal Experience of Pleasure Scale (TEPS) (Gard et al., 2006), and current anhedonia using the Snaith-Hamilton Pleasure Scale (SHAPS) (Snaith et al., 1995).
The goals of the present investigation were: (i) to test whether deficits in establishing a reward bias occur in first-degree relatives of patients with MDD; and (ii) to investigate whether such blunted reward sensitivity is associated with anhedonia in these individuals. Importantly, individuals at high risk for MDD often show subclinical levels of depressive symptoms, which may confer risk for future illness (Angold et al., 1987), and anhedonic symptoms are more likely to be reported in participants with depressive symptoms. Therefore we examined reward sensitivity in relatives with subclinical depressive symptoms, relatives without depressive symptoms and healthy controls at low risk for depression, which facilitated a more precise characterization of risk. Based on our hypothesis that the mechanisms driving anhedonia are heritable, and prior findings of anticipatory reward processing abnormalities in depressed individuals, we hypothesized that first-degree relatives of depressed individuals would show a blunted reward bias. We further hypothesized that first-degree relatives with fewer depressive symptoms would display blunted reward bias and anhedonia to a lesser extent than first-degree relatives with more depressive symptoms. Finally, we hypothesized that clinical measures of anhedonia, especially anticipatory anhedonia, would be associated with blunted reward bias in this sample, over and above associations with general depressive symptoms.
2. Methods and Materials
2.1. Participants
Forty-seven unaffected relatives of patients with MDD (26 females, age 18-52) were recruited when they accompanied their depressed relative to attend a doctor's appointment in a psychiatric hospital (Guangzhou Psychiatric Hospital, China). All relatives and depressed patients were interviewed by their attending psychiatrists (LZW, YHZ). All depressed patients met the diagnostic criteria for MDD according to the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition: DSM-IV) (APA, 1994), without any other concurrent Axis I disorders (excepting anxiety), current or past psychotic features or manic episodes. Sixty healthy controls (34 females, age 21-48) were recruited from the local community by advertisement. All participants were further screened to exclude any medical or neurological disorders, current or past history of any mental disorder and substance abuse/dependence, or the use of psychotropic medications. Healthy controls who reported any psychiatric disorders in a first degree relative were also excluded. The Wechsler Abbreviated Scale of Intelligence (WAIS) (Gong, 1992) was used to estimate intelligence quotient (IQ).
All participants completed the Chinese Beck Depression Inventory (BDI; (Beck et al., 1961; Wang et al., 1999), which is a reliable self-report measure of depression severity and has been validated in the Chinese population (Wang et al., 1999). As a screening tool in a non-clinical population, the standard BDI cut-off score is 10 (Beck et al., 1988), indicating at least mild depression. Healthy volunteers who scored 10 or above on the BDI were therefore excluded from the control group. Some relatives had a score of 10 or above on the BDI, but had never met the threshold for MDD. We used a categorical analysis, creating two subgroups of relatives based on high (BDI score 10 or above: N=26) and low (BDI score below 10: N=21) levels of depression. The study was approved by the Ethics Committee of the Guangzhou Psychiatric Hospital. Written informed consent was obtained from all participants.
2.2. Mood and anhedonia assessments
Participants completed questionnaire assessments in a quiet room in the hospital. The Snaith-Hamilton Pleasure Scale (SHAPS) was used to measure current anhedonia (Snaith et al., 1995). The Chinese version used for the present study includes 14 items and has been shown to possess adequate reliability (Liu et al., 2012). Higher scores indicate more anhedonic symptoms. The Cronbach's alpha in this sample was 0.85.
The Revised Temporal Experience of Pleasure Scale (TEPS) - Chinese Version was used to evaluate trait anticipatory (TEPS-ANT) and consummatory anhedonia (TEPS-CON) (Chan et al., 2010). The scale has been validated in clinical and non-clinical samples (Chan et al., 2012; Gard et al., 2006). The Chinese version includes 20 items and a lower total score indicates a higher level of anhedonia. The scale had acceptable internal validity in this sample, with Cronbach's alphas of 0.75 for the TEPS-ANT and 0.76 for the TEPS-CON.
The BDI is widely used to assess the severity of depressive symptoms (Beck et al., 1961). The Cronbach's alpha in the present sample was 0.94.
2.3. Probabilistic reward task
After completing the questionnaires, participants performed a probabilistic reward task. The task was developed based on signal-detection theory (Pizzagalli et al., 2005) and used an asymmetrical reward schedule design, in which one of two difficult-to-distinguish stimuli (based on features of cartoon faces) was presented and the participants were asked to respond by indicating which of the two stimuli they had seen. Stimuli were presented on a Dell 520 latitude laptop computer (with a 15 inch screen) using stimulus presentation software (E-prime 2, Psychology Software Tools, Inc.). Participants viewed the stimuli at a distance of about 50 cm.
One stimulus type was rewarded for correct responses three times more often than the other type. Creating this asymmetric reward schedule between the two types of stimuli reliably produces a systematic preference (response bias) for the more frequently rewarded stimulus.(Pizzagalli et al., 2005) This reward response bias has previously been suggested to provide a behavioural measure of “hedonic capacity” or reward sensitivity (Bogdan and Pizzagalli, 2006; Pizzagalli et al., 2005), although in those studies participants had to learn which stimulus was rewarded more frequently, which may complicate the interpretation of the results (Huys et al., 2013). Therefore in the present task, participants were instructed about the reward asymmetry explicitly, meaning that any differences observed were unlikely to be related to learning ability.
Rewards were scheduled according to a pseudo-randomized sequence, with correct responses being rewarded on 60% of the trials for the more frequently rewarded (‘rich’) stimulus and on 20% of the trials for the less frequently rewarded (‘lean’) stimulus. Faces with long mouths or short noses were more frequently rewarded, while those with short mouths or long noses were less frequently rewarded. In each block, the first 10 trials presented one facial feature (e.g., mouth) and the second 10 trials presented another facial feature (e.g., nose), and so on alternately. The stimulus lengths for the long and short mouth were 11 mm and 10 mm, respectively, and the lengths for the long and short nose were 5.5 mm and 5 mm, respectively. These stimulus lengths had been demonstrated to be effective in ensuring adequate task difficulty in our previous study (Liu et al., 2011).
Participants were instructed that they should try to win as much money as possible but were also informed that rewards would not be provided for correct responses on every trial. They were also instructed regarding the contingencies. On each trial, after a central fixation point (1000 ms), a mouth-less cartoon face was presented (500 ms). Then, a cartoon face with either a long or short mouth (or nose) was displayed briefly in the middle of monitor (100 ms) and then disappeared, leaving the mouth-less face on the screen (1500 ms). During this period, participants were asked to identify whether a cartoon face with a long or short mouth (or nose) had been shown by pressing the “1” or the “4” key, respectively. When a response was correct on a rewarded trial, the participant received a 1500 ms feedback display (“Congratulations!! You've got 20 cents (RMB)!”), which was followed by a blank screen for 250 ms. If no accurate response was given or the response was accurate but no reward was scheduled, a blank screen was presented for 1750 ms. The task included three blocks of 80 trials and lasted approximately 20 minutes.
After completing the reward task, the participants were debriefed and were given their “winnings” for performing the task (although the same amount (50 Chinese Yuan, about 8 USD) was given to each participant).
2.4. Data analysis
Trials with reaction times more than 3 SD away from the mean, or premature/no response trials, were excluded (3.59%). Reward response bias (or simply reward bias, Log b) and discriminability (Log d) were computed using the method described in previous studies (Bogdan and Pizzagalli, 2006; Pizzagalli et al., 2005). Reward bias (towards the ‘rich’, i.e. more frequently rewarded, stimulus) was our main behavioural outcome measure, while discriminability acted as a control measure for overall task performance. Reward bias and discriminability were computed as:
As shown in the formula, a high reward bias (Log b) emerges with (i) large numbers of correct identifications of the frequently rewarded stimulus and misses for the infrequently rewarded stimulus, and (ii) small numbers of misses for the frequently rewarded stimulus and correct identifications of the infrequently rewarded stimulus. Therefore a straightforward interpretation of a positive score on this measure is a systematic preference for the response paired with the more frequent reward. Discriminability (Log d) is calculated from the log transformed difference between the proportion of hits (correct identifications of the frequently rewarded and infrequently rewarded stimulus) and misses (incorrect identifications of the frequently rewarded and infrequently rewarded stimulus). Therefore a straightforward interpretation of a positive score on this measure is the ability to distinguish between the two stimuli. This can be used to rule out group differences in the ability to perform the visual discrimination. In cases where any of the scores entering these equations had a value of zero, these formulas were adjusted to add 0.5 to every value prior to calculation of the bias and discriminability scores (Pizzagalli et al., 2007).
Reaction times and response rates were recorded for every trial type. We also report reaction times for correct responses, the proportion of ‘rich’ hits (correct responses on ‘rich’ stimulus trials) and the proportion of ‘rich’ false alarms (incorrect responses on ‘lean’ stimulus trials).
Statistical analysis was performed using SPSS 15.0 software (SPSS Inc., Chicago, IL, USA). Repeated measures analysis of variance (ANOVA) with Group (controls, relatives with low depression-rating scores, relatives with high depression-rating scores) as a between-subject factor and Block (1, 2, 3) as a within-subject factor was performed for all outcome measures. Greenhouse-Geisser correction was used where appropriate and Bonferroni corrected post-hoc contrasts were used to identify differences between groups when significant main effects or interactions were identified. For accuracy (percent correct) and reaction time, ANOVAs included Stimulus Type (frequently rewarded – ‘rich’, infrequently rewarded – ‘lean’) as an additional within-subject factor.
Pearson correlation coefficients were calculated to examine the relationship between behavioural measures and questionnaires. To test a possible specific link between anhedonia and reward bias, further hierarchical regression analysis was conducted to determine if one type of anhedonia component (measured by the SHAPS and TEPS) uniquely predicted the overall reward bias during the task after controlling for overall depression severity (BDI score: entered in the first step), both in the complete sample and within each group separately.
3. Results
3.1. Group characteristics
Table 1 summarizes demographic information and ratings on the questionnaire measures. There were no significant differences between the three groups on measures of gender, education, and estimated IQ. Since the relatives groups were older than the healthy controls, we repeated all analyses including age as covariate, but this did not alter the results. Relatives with high BDI scores had higher state anhedonia (measured by the SHAPS) than relatives with low BDI scores and healthy controls (all ps<0.001). Relatives with high BDI scores also had higher trait anhedonia (measured by the TEPS and the TEPS-ANT subscale) than healthy controls (all ps<0.05). Relatives with low BDI scores were similar to healthy controls on all symptom scales.
Table 1. Demographic characteristics and self-reported measures of symptoms.
| Relatives with high depression-rating scores (N=21) | Relatives with Low depression-rating scores (N=26) | Healthy control group (N=60) | Analysis | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Gender (M/F) | 9/12 | 12/14 | 26/34 | χ2 = 1.94,df=2,p >0.05 |
| Age (years) | 36.1±11.8 | 34.7 ±12.2 | 30.3±6.4 | F(2,106)=4.63,p<0.05 |
| Education (years) | 12.9±3.1 | 13.3± 3.2 | 13.6±2.9 | F(2,106)=1.14,p=0.32 |
| Estimated IQ | 102.5±9.3 | 108.6±11.5 | 106.1±14.6 | F(2,106)=1.25,p=0.29 |
| Self-reported experience of symptoms | ||||
| BDI (0-63) | 15.5±4.8 | 2.5±2.5 | 2.8±2.4 | F(2,106)=156.27, p<0.001*† |
| SHAPS (14-56) | 27.2±4.9 | 21.0±5.5 | 22.0±5.5 | F(2,106)=8.97,p <0.001*† |
| TEPS-ANT (11-66) | 38.2±9.1 | 43.7±8.6 | 44.7±7.7 | F(2,106)=4.93,p<0.01† |
| TEPS-CON (9-54) | 32.3±8.6 | 36.5±8.2 | 36.1±7.2 | F(2,106)=2.17,p>0.05 |
| TEPS total score | 70.9±16.1 | 80.1±14.7 | 80.8±12.9 | F(2,106)=4.43,p<0.05† |
Data are presented as n or mean ± SD.
Notes: BDI: Beck Depression Inventory; SHAPS: Snaith-Hamilton Pleasure Scale;
TEPS-ANT: Temporal Experience of Pleasure Scale – Anticipatory Pleasure Subscale;
TEPS-CON: Temporal Experience of Pleasure Scale – Consummatory Pleasure Subscale.
Post-hoc tests revealed differences between the relatives with high depression-rating scores and the relatives with low depression-rating scores.
Post-hoc tests revealed differences between the relatives with high depression-rating scores and the healthy controls.
3.2. Behavioural analysis: reward bias
There was no main effect of Group on reward bias (F(1,104)=1.68, p=0.19, partial η2=0.03), but the main effect of Block on reward bias was significant (F(2,208)=13.80, p<0.001, partial η2=0.12), which was qualified by a significant Block × Group interaction (F(4,208)=2.91, p=0.024, partial η2=0.05). Relatives with high BDI scores had a blunted reward bias, which was similar across all three blocks (simple main effect of block: F(2,40)=2.06, p=0.14, partial η2=0.09). Healthy controls and relatives with low BDI scores both showed decreased reward bias over blocks (simple main effect of block in the relatives with low BDI scores: F(2,50)=8.93, p<0.005, partial η2=0.26 in healthy controls: F(2,118)=8.55, p<0.001, partial η2=0.13). In comparison with relatives with low BDI scores and healthy controls, relatives with high BDI scores had a lower reward bias in block 1 (all ps<0.05) (see Figure 1). ANCOVA including age as covariate on reward bias showed a similar significant Block × Group interaction (F(4,206)=2.92, p=0.02, partial η2=0.05), indicating that these results were not influenced by the age difference between groups.
Figure 1.
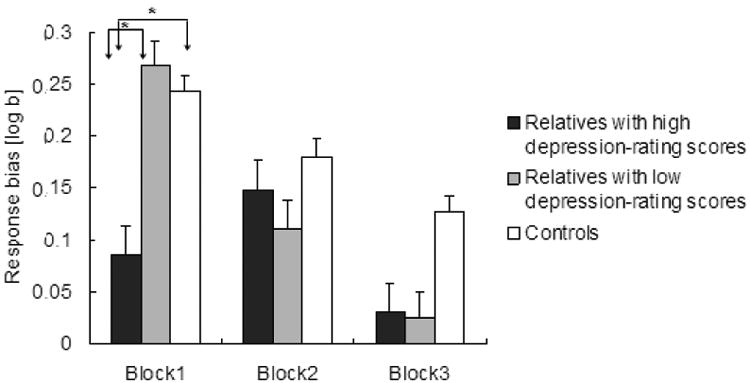
Response bias in the relatives with high depression-rating scores, relatives with low depression-rating scores and healthy controls from block 1 to block 3. Error bars represent standard errors of the mean. The solid lines and asterisks indicate significant differences between groups (Bonferroni corrected p<0.05).
We conducted an additional exploratory repeated-measures ANOVA, with all relatives constituting a single high-risk group compared with healthy controls, to test whether blunted reward bias was a general feature in relatives of depressed patients. There was a similar main effect of Block on reward bias (F(2,210)=15.61, p<0.001, partial η2=0.13) and a trend towards a main effect of Group (F(1,105)=2.83, p=0.096, partial η2=0.03), with relatives having a relatively reduced reward bias (mean±SEM: 0.11±0.03) compared with healthy controls (0.18±0.03). There was no Block × Group interaction (F(2,210)<0.56, p>0.57, partial η2<0.01).
3.3. Relationship between reward bias and self-report measures
Across the whole sample, SHAPS score was negatively associated with a lower reward bias overall (r=-0.25, p<0.01), in block 1 (r=-0.31, p<0.001) and in block 3 (r=-0.25, p<0.01). Total TEPS and TEPS-ANT scores (note that lower values indicate greater anhedonia) were associated with a higher reward bias in block 3 (TEPS: r=0.24, p<0.05; TEPS-ANT: r=0.20, p<0.05). TEPS-CON was associated with a higher reward bias overall (r=0.20, p<0.05), in block 1 (r=0.22, p<0.05) and in block 3 (r=0.24, p<0.05). Higher BDI score was associated with a lower reward bias in block 1 (r=-0.24, p<0.05) (see Table 3).
Table 3. Pearson correlations between questionnaire measures and response bias across all participants (N=107).
| Overall RB | RB in block1 | RB in block 2 | RB in block 3 | |
|---|---|---|---|---|
| SHAPS | -0.25**\ p=0.009 | -0.31**\ p<0.001 | -0.07 | -0.25**\ p=0.009 |
| TEPS | 0.14 | 0.14 | -0.02 | 0.24*\ p=0.01 |
| TEPS_ANT | 0.06 | 0.04 | -0.06 | 0.20*\ p=0.04 |
| TEPS_CON | 0.20* p=0.04 | 0.22* p=0.02 | 0.03 | 0.23* p=0.02 |
| BDI | -0.15 | -0.24* p=0.01 | -0.03 | -0.11 |
Notes:
Indicates p<0.05;
Indicates p<0.01; RB: Response Bias.
Regression analysis showed that only the SHAPS measure of anhedonia predicted overall reward bias in the whole sample after controlling for BDI score (ΔR2=0.07, ΔF(2,106)=3.67, p<0.05).
Exploratory ANCOVAs were performed on reward bias scores with questionnaire measurements entered as covariates to examine whether the above associations with anhedonia differed between the groups. Significant interactions with Group were identified for all anhedonia measurements (SHAPS, TEPS, TEPS-ANT and TEPS-CON: all Fs>2.28, all ps<0.05). Thus, we further explored the association between reward reward bias and anhedonia in each group separately.
For healthy controls and relatives with low BDI scores, no significant association was found.
For relatives with high BDI scores, anhedonia measured by the SHAPS (r=-0.53, p<0.05) and trait consummatory anhedonia measured by the TEPS-CON (r=0.43, p=0.05) were associated with a lower overall reward bias (see Figure 2). In addition, there were significant associations between anhedonia and low reward bias for SHAPS in block 2 (r=-0.48, p<0.05) and block 3 (r=-0.47, p<0.05), for TEPS in block 3 (r=0.52, p<0.05), and for TEPS-CON in block 3 (r=0.58, p<0.01).
Figure 2.
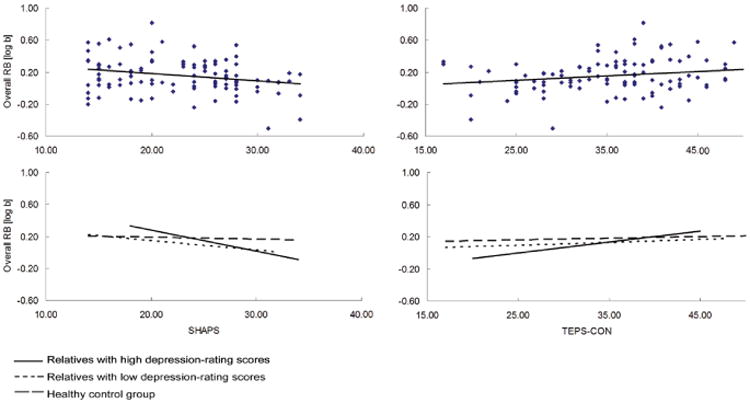
Top: Scatterplot depicting the relationship between overall response bias (RB) and anhedonia questionnaire measurements in the whole sample. Bottom: Regression lines depicting the relationship separately for the healthy controls, relatives with low depression-rating scores and relatives with high depression-rating scores. Higher anhedonia (SHAPS) and trait consummatory anhedonia (TEPS-CON) were associated with a lower overall response bias in the whole sample and in the relatives with high depression-rating scores (all ps<0.05).
Regression analysis showed that only the SHAPS measure of anhedonia predicted overall reward bias in relatives with high BDI scores after controlling for BDI score (ΔR2=0.31, ΔF(2,20)=4.07, p<0.05).
In summary, we found that the association between anhedonia and attenuated reward bias was mainly driven by the group of relatives with high BDI scores, and that there was a specific association between low reward bias and anhedonia over and above sub-clinical depressive symptoms.
3.4. Control analyses: discriminability and other measures
Other behavioural data (discriminability, accuracy, reaction time for correct responses, hits and false alarms for the more frequently rewarded stimulus) are reported in Table 2. For the sake of brevity, only statistical details for effects involving Group are reported.
Table 2. Behavioural data.
| Behavioral measures | Relatives with high depression-rating scores (N=21) | Relatives with low depression-rating scores (N=26) | Healthy control group (N=60) |
|---|---|---|---|
| Block 1 | |||
| Discrimination (log d) | 0.4±0.4 | 0.5±0.3 | 0.5±0.3 |
| Accuracy for frequently rewarded stimulus (%) | 0.7±0.2 | 0.8±0.2 | 0.8±0.1 |
| Accuracy for infrequently rewarded stimulus (%) | 0.6±0.2 | 0.6±0.2 | 0.6±0.2 |
| Reaction time for correct responses (ms) | 517.1±179.5 | 504.5±147.9 | 473.1±125.8 |
| Hits (%) | 69.7±20.9 | 80.1±16.9 | 80.9±11.6 |
| False alarms (%) | 38.8±20.4 | 39.0±15.9 | 38.1±16.5 |
| Block 2 | |||
| Discrimination (log d) | 0.5±0.5 | 0.6±0.3 | 0.6±0.3 |
| Accuracy for frequently rewarded stimulus (%) | 0.7±0.2 | 0.8±0.2 | 0.8±0.1 |
| Accuracy for infrequently rewarded stimulus (%) | 0.6±0.2 | 0.7±0.2 | 0.7±0.2 |
| Reaction time for correct | 474.0±159.6 | 472.3±115.6 | 447.8±111.1 |
| responses (ms) | |||
| Hits (%) | 75.1±22.1 | 78.1±15.7 | 82.1±11.6 |
| False alarms (%) | 34.2±19.3 | 30.1±17.1 | 31.6±14.8 |
| Block 3 | |||
| Discrimination (log d) | 0.5±0.4 | 0.6±0.3 | 0.5±0.3 |
| Accuracy for frequently rewarded stimulus (%) | 0.7±0.2 | 0.8±0.1 | 0.8±0.1 |
| Accuracy for infrequently rewarded stimulus (%) | 0.7±0.2 | 0.7±0.2 | 0.7±0.2 |
| Reaction time for correct responses (ms) | 456.2±151.9 | 474.2±103.7 | 445.3±120.4 |
| Hits (%) | 71.3±19.2 | 78.2±13.5 | 79.5±12.0 |
| False alarms (%) | 30.8±16.4 | 25.3±17.3 | 31.0±16.0 |
| Data are presented as mean ± SD. | |||
Discriminability
No effects involving Group were identified (all Fs<1.26, all ps>0.28). The results were similar when age was included as a covariate (all ps>0.34).
Accuracy
A pattern consistent with that for reward bias was observed. The Stimulus Type × Group interaction showed trend towards significance (F(2,104)=2.87, p=0.06, partial η2 =0.05), with lower accuracy for the more frequently rewarded stimulus in relatives with high BDI scores compared with healthy controls (p=0.02). No other effects involving Group were identified (all Fs<1.26, all ps >0.28).
Reaction time for correct responses: No effects involving Group was identified (all Fs<1.06, all ps>0.37).
4. Discussion
We explored behavioural responsiveness to reward in first-degree relatives of patients with MDD and healthy controls, and investigated the relationship between reward response bias and anhedonic symptoms in these participants. We observed two distinct patterns in the relatives, according to whether they reported high or low (sub-clinical) levels of depressive symptoms. Relatives with low BDI scores could successfully establish a reward bias, and were statistically indistinguishable from controls. However, they showed a marked decrease in reward bias over blocks, exhibiting substantial attenuation by block 3. In contrast, relatives with high BDI scores, who also exhibited significantly higher anhedonia than healthy controls, had significantly lower reward bias scores from the very first block. Finally, low reward bias was associated with questionnaire-measured anhedonia across all participants, and specifically in the relatives with high BDI scores, over and above the severity of subclinical depressive symptoms.
This study demonstrated a deficit in establishing a reward bias only in relatives with high BDI scores, but not in relatives with low BDI scores. The finding cannot be explained by difficulty in performing the task, because no group differences in discriminability and reaction time were observed. Possibly, relatives with low depression-rating scores have the ability to seek out reward actively like individuals without depressed relatives, since they possess a largely intact motivational system (according to our questionnaire and behavioural measures). Current evidence for reward processing abnormalities in individuals with elevated MDD risk mainly comes from neuroimaging studies with small sample sizes (Gotlib et al., 2010; McCabe et al., 2012; Olino et al., 2014). Findings from a small number of behavioural studies with high-risk samples have reported that individual differences in depression-related symptoms are related to reward responsiveness. For example, blunted gain approach was reported to be associated with elevated negative mood in children at high risk of depression (Luking et al., 2015). Rawal et al (2013) reported that diminished reward seeking on a value-based choice task can predict the onset of depression in adolescents with a family history of MDD. Moreover, the severity of parental depression was associated with alterations in reward processing in two high-risk samples (Luking et al., 2015; Rawal et al., 2014). Interestingly, only high-risk adolescents with a current depressive disorder displayed less reward seeking behaviour (Rawal et al., 2013).
These prior findings and those from the present study raise the possibility that disrupted reward processing may be a consequence of more severe depressive symptoms, as opposed to reflecting a trait marker. Another possibility is that because the participants were explicitly informed about the reward probabilities, relatives with low BDI scores might be able to use this information intentionally as a compensatory strategy to improve their behavioural performance. Due to habituation during this quite repetitive task, healthy controls may show a decreasing reward bias towards the end of the task. Indeed, this was reported in a previous study (Pizzagalli et al., 2009b), and may explain why a significant difference between healthy controls and relatives with high BDI scores was only observed at the beginning of task. Notably, relatives with low BDI scores showed a numerically greater reduction in response bias over the course of the task than healthy controls (with no significant bias in this group in the final block), which suggests that they might be unable to maintain this adaptive behaviour over time. However, we note that this effect did not achieve statistical significance and therefore needs to be interpreted with caution.
Consistent with our hypothesis, we detected anhedonic features and blunted reward bias in relatives with elevated depressive symptoms. Although a genetic predisposition to hedonic deficits might leave individuals vulnerable to the development of depression, other factors such as exposure to stressful life events (Bogdan et al., 2013) also likely contribute substantially to individual variation in reward-related behaviour. Anhedonia is more common in clinically severe depression (Pelizza and Ferrari, 2009): Only about 37% of individuals diagnosed with depression experience clinically significant anhedonia (Pelizza and Ferrari, 2009), and less than 25% of patients with remitted unipolar depression are considered to have a significant reduction in hedonic capacity (Di Nicola et al., 2013). While it would be interesting to compare anhedonic and non-anhedonic participants directly, if we had split the relatives and healthy controls into high and low hedonic groups according to the SHAPS clinical cut-off (Snaith et al., 1995), only nine relatives and three healthy controls would be characterized as experiencing “clinically significant” anhedonia, which would preclude meaningful statistical analysis.
In this study, relatives with high BDI scores also had high levels of trait anhedonia, possibly constituting a trait abnormality. However, we cannot exclude the possibility that the relatives with high BDI scores recruited in this study may represent a subsyndromally depressed sample, despite the negative DSM-IV diagnosis. Nonetheless, failing to establish a reward bias in relatives with high BDI scores might lead to difficulty in engaging in reward-related behaviour and might contribute to the development of diminished motivation, thereby increasing risk for depression. Similarly attenuated reward responses have been reported in clinically depressed individuals (Liu et al., 2011; Pechtel et al., 2013; Pizzagalli et al., 2009b), in particular those with marked anhedonia (Vrieze et al., 2013) and melancholic features (Fletcher et al., 2015). It would be of interest in future work to follow relatives with high BDI scores and test whether attenuated reward bias is associated with the subsequent development of MDD.
A weakness of our study is that the design of the task we employed may limit comparison with findings from previous work. Different constructs of reward, including ‘liking’ (hedonic impact), ‘wanting’ (valuation, or motivational salience), and learning (generating predictive associations), have both overlapping and distinct neurobiological substrates, and have been argued to be dissociable (Berridge, 2012; Berridge and Robinson, 1998; Berridge et al., 2009). A meta-analytic study using a computational approach to dissect reward-related cognitive processes in data from previous studies that used a similar signal-detection task (but without explicit instruction) (Bogdan and Pizzagalli, 2006; Pizzagalli et al., 2008a; Pizzagalli et al., 2008b; Pizzagalli et al., 2009b; Pizzagalli et al., 2005), reported that the response bias measured by the task reflects at least two separable components: one is the learning rate, i.e. the extent to which stimulus-reward associations change following feedback; the other is reward sensitivity, i.e. the value placed on the outcome by the participants (Huys et al., 2013). Importantly, this computational analysis demonstrated that anhedonia and MDD are predominantly associated with low reward sensitivity (i.e. value), not learning rate (Huys et al., 2013). To remove the potential confound of learning in the present study, the participants were informed of the reward asymmetry, which allowed us to focus on measuring reward sensitivity. However, this does preclude a direct comparison with findings from previous studies in which participants had to learn the probabilistic outcomes associated with stimuli by trial-and-error.
The correlations between anhedonia and dysfunctional reward processing in our study are noteworthy. Consistent with our hypothesis, we identified significant correlations between clinical measures of anhedonia and blunted reward bias across the whole sample. When each group was considered individually, there was no significant relationship between the level of anhedonia and reward response bias in relatives with low BDI scores and healthy controls. Instead, the association between anhedonia and attenuated reward bias was mainly driven by relatives with higher (but sub-clinical) depressive symptoms. Importantly, even after controlling for general depressive symptoms, anhedonia measured by the SHAPS still predicted reward bias, both in the whole sample and in the high BDI relatives group. The SHAPS evaluates hedonic experience or positive valence, which is a related, but conceptually distinct construct to depression (Franken et al., 2007; Franz et al., 1998; Leventhal et al., 2006; Liu et al., 2012; Nakonezny et al., 2015). This result suggests that altered behavioural responsiveness to reward may be specifically relevant to the positive valence system in relatives with high BDI scores, who are at high risk of developing depression.
There are controversies in the extant literature as to which component of anhedonia is most important in depression (Baskin-Sommers and Foti, 2015; Chen et al., 2015; Whitton et al., 2015). While some researchers emphasize that MDD is mainly characterized by an impaired anticipatory component in reward processing (‘wanting’), emerging evidence (including the present study) suggests a link between blunted reward sensitivity and consummatory anhedonia (‘liking’) (Bress and Hajcak, 2013; Liu et al., 2011; Liu et al., 2014), at least as assessed by the TEPS-CON. However, the SHAPS, which was the only measure of anhedonia that predicted reward bias after accounting for general depressive symptoms, is generally considered a unidimensional instrument (Liu et al., 2012; Nakonezny et al., 2010) that captures both recent hedonic tone and trait anhedonia (Di Nicola et al., 2013). In addition, it should be noted that TEPS-CON scores did not differ between the groups in the present study. Therefore more research is needed to disentangle the relationships between specific components of anhedonia and reward response bias.
Researchers have recently begun to explore reward-related deficits in different subtypes of depression. One study, using a similar signal-detection approach to that employed here, showed that attenuated reward bias is primarily associated with melancholic depression, and not observed in non-melancholic patients (Fletcher et al., 2015). Another study using a multimodal neuroimaging approach to record neural responses to positive outcomes during a gambling task showed that feedback negativity (FN), an ERP component thought to index reward evaluation, and ventral striatal activation were blunted only in the MDD subgroup with impaired mood reactivity to positive events, independent of DSM-defined melancholic or atypical MDD subtypes (Foti et al., 2014). These findings indicate substantial heterogeneity in reward processing between individuals with MDD. Future studies should consider the multiple facets of anhedonia in depression, and specifically develop instruments to measure the different components of hedonic capacity, compare their dysregulation in different psychiatric disorders, and explore how these different facets might change as a function of having experienced a depressive episode.
Our study had several limitations. First, we were able to include only a relatively small sample and did not formally evaluate global cognitive function in our participants. Moreover, a depressed patient group was not included. Future studies should evaluate dysfunctional reward response between MDD patients and relatives in larger samples. Second, this sample recruited the first-degree relatives of depressed individuals, but we did not limit whether the first-degree relatives were parents, children or siblings of patients with depression. We also did not collect information on whether the relatives were living with the patients or whether they were their primary caregivers. How these factors may have affected hedonic capacity in the relatives is unclear in present study. Third, due to the limitations of our clinical interview, this study might have included some healthy controls who were related to people with a history of major depressive disorder but did not report it. Furthermore, some relatives were excluded because they met criteria for a DSM-IV diagnosis, which precludes generalization of our results to relatives with comorbid mental disorders, in particular anxiety. Finally, this study used a trial-average analysis within each block; as a result, we were unable to determine whether the observed behavioural differences were the result of processes that evolve in a trial-by-trial manner. An alternative approach, beyond the scope of the present report, would be to construct a computational model of performance in this reinforcement task to evaluate the temporal evolution of reward processing (Chase et al., 2010; Philiastides et al., 2010; Steele et al., 2007). Using such an analysis, it would be possible to simulate how latent variables such as reward value change over time and explore whether clinical symptoms influence model-estimated reward processing across participants.
Notwithstanding these limitations, our findings suggest that a subgroup of first-degree relatives of patients with MDD who experience subclinical depressive symptoms display blunted reward sensitivity, which is associated with clinical measures of anhedonia over and above general depressive symptoms. Blunted reward sensitivity may therefore constitute a risk marker for MDD. These data also support the notion that the existing clinical characterization of anhedonia in depression may represent an aggregation of several underlying cognitive constructs, and requires refinement.
References
- Angold A, Weissman MM, John K, Merikangas KR, Prusoff BA, Wickramaratne P, Gammon GD, Warner V. Parent and child reports of depressive symptoms in children at low and high risk of depression. J Child Psychol Psychiatry. 1987;28:901–915. doi: 10.1111/j.1469-7610.1987.tb00678.x. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Baare WF, Vinberg M, Knudsen GM, Paulson OB, Langkilde AR, Jernigan TL, Kessing LV. Hippocampal volume changes in healthy subjects at risk of unipolar depression. J Psychiatr Res. 2010;44:655–662. doi: 10.1016/j.jpsychires.2009.12.009. [DOI] [PubMed] [Google Scholar]
- Barch DM, Treadway MT, Schoen N. Effort, anhedonia, and function in schizophrenia: reduced effort allocation predicts amotivation and functional impairment. J Abnorm Psychol. 2014;123:387–397. doi: 10.1037/a0036299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskin-Sommers AR, Foti D. Abnormal reward functioning across substance use disorders and major depressive disorder: Considering reward as a transdiagnostic mechanism. Int J Psychophysiol. 2015 doi: 10.1016/j.ijpsycho.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Berridge KC. From prediction error to incentive salience: mesolimbic computation of reward motivation. Eur J Neurosci. 2012;35:1124–1143. doi: 10.1111/j.1460-9568.2012.07990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Rev. 1998;28:309–369. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- Berridge KC, Robinson TE, Aldridge JW. Dissecting components of reward: ‘liking’, ‘wanting’, and learning. Curr Opin Pharm. 2009;9:65–73. doi: 10.1016/j.coph.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdan R, Nikolova YS, Pizzagalli DA. Neurogenetics of depression: A focus on reward processing and stress sensitivity. Neurobiol Dis. 2013;52:12–23. doi: 10.1016/j.nbd.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdan R, Pizzagalli DA. Acute stress reduces reward responsiveness: implications for depression. Biol Psychiatry. 2006;60:1147–1154. doi: 10.1016/j.biopsych.2006.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdan R, Pizzagalli DA. The heritability of hedonic capacity and perceived stress: a twin study evaluation of candidate depressive phenotypes. Psychol Med. 2009;39:211–218. doi: 10.1017/S0033291708003619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bress JN, Hajcak G. Self-report and behavioral measures of reward sensitivity predict the feedback negativity. Psychophysiology. 2013;50:610–616. doi: 10.1111/psyp.12053. [DOI] [PubMed] [Google Scholar]
- Chan RC, Wang Y, Huang J, Shi Y, Hong X, Ma Z, Li Z, Lai MK, Kring AM. Anticipatory and consummatory components of the experience of pleasure in schizophrenia: Cross-cultural validation and extension. Psychiatry Res. 2010;175:181–183. doi: 10.1016/j.psychres.2009.01.020. [DOI] [PubMed] [Google Scholar]
- Chan RCK, Shi Y, Lai MK, Wang YN, Wang Y, Kring AM. The Temporal Experience of Pleasure Scale (TEPS): Exploration and Confirmation of Factor Structure in a Healthy Chinese Sample. PLoS One. 2012;7:e35352. doi: 10.1371/journal.pone.0035352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase HW, Frank MJ, Michael A, Bullmore ET, Sahakian BJ, Robbins TW. Approach and avoidance learning in patients with major depression and healthy controls: relation to anhedonia. Psychol Med. 2010;40:433–440. doi: 10.1017/S0033291709990468. [DOI] [PubMed] [Google Scholar]
- Chen C, Takahashi T, Nakagawa S, Inoue T, Kusumi I. Reinforcement learning in depression: A review of computational research. Neurosci Biobehav Rev. 2015;55:247–267. doi: 10.1016/j.neubiorev.2015.05.005. [DOI] [PubMed] [Google Scholar]
- Chentsova-Dutton Y, Hanley K. The effects of anhedonia and depression on hedonic responses. Psychiatry Res. 2010;179:176–180. doi: 10.1016/j.psychres.2009.06.013. [DOI] [PubMed] [Google Scholar]
- Di Nicola M, De Risio L, Battaglia C, Camardese G, Tedeschi D, Mazza M, Martinotti G, Pozzi G, Niolu C, Di Giannantonio M, Siracusano A, Janiri L. Reduced hedonic capacity in euthymic bipolar subjects: a trait-like feature? J Affect Disord. 2013;147:446–450. doi: 10.1016/j.jad.2012.10.004. [DOI] [PubMed] [Google Scholar]
- Dillon DG, Bogdan R, Fagerness J, Holmes AJ, Perlis RH, Pizzagalli DA. Variation in TREK1 gene linked to depression-resistant phenotype is associated with potentiated neural responses to rewards in humans. Hum Brain Mapp. 2010;31:210–221. doi: 10.1002/hbm.20858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd EC, Barch DM. Anhedonia and emotional experience in schizophrenia: neural and behavioral indicators. Biol Psychiatry. 2010;67:902–911. doi: 10.1016/j.biopsych.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryman A, Eaton WW. Affective symptoms associated with the onset of major depression in the community: findings from the US National Institute of Mental Health Epidemiologic Catchment Area Program. Acta Psychiatr Scand. 1991;84:1–5. doi: 10.1111/j.1600-0447.1991.tb01410.x. [DOI] [PubMed] [Google Scholar]
- Epstein J, Pan H, Kocsis JH, Yang Y, Butler T, Chusid J, Hochberg H, Murrough J, Strohmayer E, Stern E, Silbersweig DA. Lack of ventral striatal response to positive stimuli in depressed versus normal subjects. The American Journal of Psychiatry. 2006;163:1784–1790. doi: 10.1176/ajp.2006.163.10.1784. [DOI] [PubMed] [Google Scholar]
- Eshel N, Roiser JP. Reward and punishment processing in depression. Biol Psychiatry. 2010;68:118–124. doi: 10.1016/j.biopsych.2010.01.027. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Clark DC, Scheftner WA, Gibbons RD. Assessing anhedonia in psychiatric patients. Arch Gen Psychiatry. 1983;40:79–84. doi: 10.1001/archpsyc.1983.01790010081010. [DOI] [PubMed] [Google Scholar]
- Fletcher K, Parker G, Paterson A, Fava M, Iosifescu D, Pizzagalli DA. Anhedonia in melancholic and non-melancholic depressive disorders. J Affect Disord. 2015;184:81–88. doi: 10.1016/j.jad.2015.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Shaw DS, Dahl RE. Alterations in reward-related decision making in boys with recent and future depression. Biol Psychiatry. 2007;61:633–639. doi: 10.1016/j.biopsych.2006.05.026. [DOI] [PubMed] [Google Scholar]
- Foti D, Carlson JM, Sauder CL, Proudfit GH. Reward dysfunction in major depression: multimodal neuroimaging evidence for refining the melancholic phenotype. Neuroimage. 2014;101:50–58. doi: 10.1016/j.neuroimage.2014.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foti D, Kotov R, Klein DN, Hajcak G. Abnormal Neural Sensitivity to Monetary Gains Versus Losses Among Adolescents at Risk for Depression. J Abnorm Child Psychol. 2011;39:913–924. doi: 10.1007/s10802-011-9503-9. [DOI] [PubMed] [Google Scholar]
- Franken IH, Rassin E, Muris P. The assessment of anhedonia in clinical and non-clinical populations: further validation of the Snaith-Hamilton Pleasure Scale (SHAPS) J Affect Disord. 2007;99:83–89. doi: 10.1016/j.jad.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Franz M, Lemke MR, Meyer T, Ulferts J, Puhl P, Snaith RP. German version of the Snaith-Hamilton-Pleasure Scale (SHAPS-D). Anhedonia in schizophrenic and depressive patients. Fortschr Neurol Psychiatr. 1998;66:407–413. doi: 10.1055/s-2007-995279. [DOI] [PubMed] [Google Scholar]
- Frokjaer VG, Vinberg M, Erritzoe D, Svarer C, Baare W, Budtz-Joergensen E, Madsen K, Madsen J, Kessing LV, Knudsen GM. High familial risk for mood disorder is associated with low dorsolateral prefrontal cortex serotonin transporter binding. Neuroimage. 2009;46:360–366. doi: 10.1016/j.neuroimage.2009.02.008. [DOI] [PubMed] [Google Scholar]
- Gard DE, Gard MG, Kring AM, John OP. Anticipatory and consummatory components of the experience of pleasure: A scale development study. Journal of research in personality. 2006;40:1086–1102. [Google Scholar]
- Gong YX. Manual of Wechsler Adult Intelligence Scale - Chinese version. Changsha: Chinese Map Press; 1992. [Google Scholar]
- Gotlib IH, Hamilton JP, Cooney RE, Singh MK, Henry ML, Joormann J. Neural processing of reward and loss in girls at risk for major depression. Arch Gen Psychiatry. 2010;67:380–387. doi: 10.1001/archgenpsychiatry.2010.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PO, Armony J, Malla A, Lepage M. Functional neural substrates of self-reported physical anhedonia in non-clinical individuals and in patients with schizophrenia. J Psychiatr Res. 2010;44:707–716. doi: 10.1016/j.jpsychires.2009.12.008. [DOI] [PubMed] [Google Scholar]
- Harvey PO, Pruessner J, Czechowska Y, Lepage M. Individual differences in trait anhedonia: a structural and functional magnetic resonance imaging study in non-clinical subjects. Mol Psychiatry. 2007;12703:767–775. doi: 10.1038/sj.mp.4002021. [DOI] [PubMed] [Google Scholar]
- Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacology. 2004;29:1765–1781. doi: 10.1038/sj.npp.1300506. [DOI] [PubMed] [Google Scholar]
- Herbener ES, Harrow M. The course of anhedonia during 10 years of schizophrenic illness. J Abnorm Psychol. 2002;111:237–248. [PubMed] [Google Scholar]
- Huys QJ, Pizzagalli DA, Bogdan R, Dayan P. Mapping anhedonia onto reinforcement learning: a behavioural meta-analysis. Biology of Mood and Anxiety Disorders. 2013;3:12. doi: 10.1186/2045-5380-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. A– J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Keedwell PA, Andrew C, Williams SC, Brammer MJ, Phillips ML. The neural correlates of anhedonia in major depressive disorder. Biol Psychiatry. 2005;58:843–853. doi: 10.1016/j.biopsych.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Klein D. Depression and anhedonia. In: Clark DC, Fawcett J, editors. Anhedonia and aVect deWcit states. New York: PMA Publishing; 1984. pp. 1–14. [Google Scholar]
- Lauer CJ, von Zerssen D, Schreiber W, Modell S, Holsboer F, Krieg JC. The pre-morbid psychometric profile is stable over time in subjects at high familial risk for affective disorders. J Affect Disord. 1998;51:45–53. doi: 10.1016/s0165-0327(98)00155-4. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Chasson GS, Tapia E, Miller EK, Pettit JW. Measuring hedonic capacity in depression: a psychometric analysis of three anhedonia scales. J Clin Psychol. 2006;62:1545–1558. doi: 10.1002/jclp.20327. [DOI] [PubMed] [Google Scholar]
- Lisiecka DM, Carballedo A, Fagan AJ, Connolly G, Meaney J, Frodl T. Altered inhibition of negative emotions in subjects at family risk of major depressive disorder. J Psychiatr Res. 2012;46:181–188. doi: 10.1016/j.jpsychires.2011.10.010. [DOI] [PubMed] [Google Scholar]
- Lisiecka DM, Carballedo A, Fagan AJ, Ferguson Y, Meaney J, Frodl T. Recruitment of the left hemispheric emotional attention neural network in risk for and protection from depression. J Psychiatry Neurosci. 2013;38:117–128. doi: 10.1503/jpn.110188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu WH, Chan RC, Wang LZ, Huang J, Cheung EF, Gong QY, Gollan JK. Deficits in sustaining reward responses in subsyndromal and syndromal major depression. Prog Neuropsychopharmacol B− ol Psychiatry. 2011;35:1045–1052. doi: 10.1016/j.pnpbp.2011.02.018. [DOI] [PubMed] [Google Scholar]
- Liu WH, Wang LZ, Shang HR, Shen Y, Li Z, Cheung EF, Chan RC. The influence of anhedonia on feedback negativity in major depressive disorder. Neuropsychologia. 2014;53:213–220. doi: 10.1016/j.neuropsychologia.2013.11.023. [DOI] [PubMed] [Google Scholar]
- Liu WH, Wang LZ, Zhu YH, Li MH, Chan RC. Clinical utility of the Snaith-Hamilton-Pleasure scale in the Chinese settings. BMC Psychiatry. 2012;12:184. doi: 10.1186/1471-244X-12-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loas G. Vulnerability to depression: a model centered on anhedonia. J Affect Disord. 1996;41:39–53. doi: 10.1016/0165-0327(96)00065-1. [DOI] [PubMed] [Google Scholar]
- Loas G, Boyer P, Legrand A. Anhedonia in the deficit syndrome of schizophrenia. Psychopathology. 1999;32:207–219. doi: 10.1159/000029092. [DOI] [PubMed] [Google Scholar]
- Luking KR, Pagliaccio D, Luby JL, Barch DM. Child Gain Approach and Loss Avoidance Behavior: Relationships With Depression Risk, Negative Mood, and Anhedonia. J Am Acad Child Adolesc Psychiatry. 2015;54:643–651. doi: 10.1016/j.jaac.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannie ZN, Taylor MJ, Harmer CJ, Cowen PJ, Norbury R. Frontolimbic responses to emotional faces in young people at familial risk of depression. J Affect Disord. 2011;130:127–132. doi: 10.1016/j.jad.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Martinotti G, Sepede G, Gambi F, Di Iorio G, De Berardis D, Di Nicola M, Onofrj M, Janiri L, Di Giannantonio M. Agomelatine versus venlafaxine XR in the treatment of anhedonia in major depressive disorder: a pilot study. J Clin Psychopharmacol. 2012;32:487–491. doi: 10.1097/JCP.0b013e31825d6c25. [DOI] [PubMed] [Google Scholar]
- McCabe C, Woffindale C, Harmer CJ, Cowen PJ. Neural processing of reward and punishment in young people at increased familial risk of depression. Biol Psychiatry. 2012;72:588–594. doi: 10.1016/j.biopsych.2012.04.034. [DOI] [PubMed] [Google Scholar]
- Miller A. Social neuroscience of child and adolescent depression. Brain Cogn. 2007;65:47–68. doi: 10.1016/j.bandc.2006.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakonezny PA, Carmody TJ, Morris DW, Kurian BT, Trivedi MH. Psychometric evaluation of the Snaith-Hamilton pleasure scale in adult outpatients with major depressive disorder. Int Clin Psychopharmacol. 2010;25:328–333. doi: 10.1097/YIC.0b013e32833eb5ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakonezny PA, Morris DW, Greer TL, Byerly MJ, Carmody TJ, Grannemann BD, Bernstein IH, Trivedi MH. Evaluation of anhedonia with the Snaith-Hamilton Pleasure Scale (SHAPS) in adult outpatients with major depressive disorder. J Psychiatr Res. 2015;65:124–130. doi: 10.1016/j.jpsychires.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, McMakin DL, Morgan JK, Silk JS, Birmaher B, Axelson DA, Williamson DE, Dahl RE, Ryan ND, Forbes EE. Reduced reward anticipation in youth at high-risk for unipolar depression: a preliminary study. Dev Cogn Neurosci. 2014;8:55–64. doi: 10.1016/j.dcn.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Barrera A, Ellis SP, Li S, Burke AK, Grunebaum M, Endicott J, Mann JJ. Instability of symptoms in recurrent major depression: a prospective study. A− J Psychiatry. 2004;161:255–261. doi: 10.1176/appi.ajp.161.2.255. [DOI] [PubMed] [Google Scholar]
- Pechtel P, Dutra SJ, Goetz EL, Pizzagalli DA. Blunted reward responsiveness in remitted depression. J Psychiatr Res. 2013;47:1864–1869. doi: 10.1016/j.jpsychires.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelizza L, Ferrari A. Anhedonia in schizophrenia and major depression: state or trait? Ann Gen Psychiatry. 2009;8:22. doi: 10.1186/1744-859X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philiastides MG, Biele G, Vavatzanidis N, Kazzer P, Heekeren HR. Temporal dynamics of prediction error processing during reward-based decision making. Neuroimage. 2010;53:221–232. doi: 10.1016/j.neuroimage.2010.05.052. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA, Bogdan R, Ratner KG, Jahn AL. Increased perceived stress is associated with blunted hedonic capacity: potential implications for depression research. Behav Res Ther. 2007;45:2742–2753. doi: 10.1016/j.brat.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Evins AE, Schetter EC, Frank MJ, Pajtas PE, Santesso DL, Culhane M. Single dose of a dopamine agonist impairs reinforcement learning in humans: behavioral evidence from a laboratory-based measure of reward responsiveness. Psychopharmacology (Berl) 2008a;196:221–232. doi: 10.1007/s00213-007-0957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Goetz E, Ostacher M, Iosifescu DV, Perlis RH. Euthymic patients with bipolar disorder show decreased reward learning in a probabilistic reward task. Biol Psychiatry. 2008b;64:162–168. doi: 10.1016/j.biopsych.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R, Dougherty DD, Iosifescu DV, Rauch SL, Fava M. Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. A− J Psychiatry. 2009a;166:702–710. doi: 10.1176/appi.ajp.2008.08081201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Iosifescu D, Hallett LA, Ratner KG, Fava M. Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task. J Psychiatr Res. 2009b;43:76–87. doi: 10.1016/j.jpsychires.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Jahn AL, O'Shea JP. Toward an objective characterization of an anhedonic phenotype: a signal-detection approach. Biol Psychiatry. 2005;57:319–327. doi: 10.1016/j.biopsych.2004.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawal A, Collishaw S, Thapar A, Rice F. ‘The risks of playing it safe’: a prospective longitudinal study of response to reward in the adolescent offspring of depressed parents. Psychol Med. 2013;43:27–38. doi: 10.1017/S0033291712001158. [DOI] [PubMed] [Google Scholar]
- Rawal A, Riglin L, Ng-Knight T, Collishaw S, Thapar A, Rice F. A longitudinal high-risk study of adolescent anxiety, depression and parent-severity on the developmental course of risk-adjustment. J Child Psychol Psychiatry. 2014;55:1270–1278. doi: 10.1111/jcpp.12279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. The British Journal of Psychiatry. 1995;167:99–103. doi: 10.1192/bjp.167.1.99. [DOI] [PubMed] [Google Scholar]
- Steele JD, Kumar P, Ebmeier KP. Blunted response to feedback information in depressive illness. Brain. 2007;130:2367–2374. doi: 10.1093/brain/awm150. [DOI] [PubMed] [Google Scholar]
- Treadway MT, Bossaller NA, Shelton RC, Zald DH. Effort-based decision-making in major depressive disorder: a translational model of motivational anhedonia. J Abnorm Psychol. 2012;121:553–558. doi: 10.1037/a0028813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrieze E, Pizzagalli DA, Demyttenaere K, Hompes T, Sienaert P, de Boer P, Schmidt M, Claes S. Reduced reward learning predicts outcome in major depressive disorder. Biol Psychiatry. 2013;73:639–645. doi: 10.1016/j.biopsych.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker J, Dillon DG, Pizzagalli DA. The role of the nucleus accumbens and rostral anterior cingulate cortex in anhedonia: integration of resting EEG, fMRI, and volumetric techniques. Neuroimage. 2009;46:327–337. doi: 10.1016/j.neuroimage.2009.01.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Huang J, Yang XH, Lui SS, Cheung EF, Chan RC. Anhedonia in schizophrenia: Deficits in both motivation and hedonic capacity. Schizophr Res. 2015 doi: 10.1016/j.schres.2015.06.019. [DOI] [PubMed] [Google Scholar]
- Wang XD, Wang XL, Ma H. Rating scales for mental health. Chinese Mental Health Journal. 1999;12:841. [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. A− J Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Whitton AE, Treadway MT, Pizzagalli DA. Reward processing dysfunction in major depression, bipolar disorder and schizophrenia. Curr Opin Psychiatry. 2015;28:7–12. doi: 10.1097/YCO.0000000000000122. [DOI] [PMC free article] [PubMed] [Google Scholar]


