Abstract
Upper eyelid blepharoplasty is one of the most common procedures performed worldwide for both functional and cosmetic indications. There is a high rate of patient satisfaction; however, in this era of social media, patient expectations are higher than ever. Today's digitally savvy patients expect perfect outcomes with no complications and rapid recovery. To achieve optimal results, a careful preoperative evaluation and sound surgical technique is essential for minimizing complications. Here the authors review their approach to the management of the blepharoplasty patient.
Keywords: blepharoplasty, upper eyelid, cosmetic surgery, functional surgery, eyelid ptosis, dry eye, complications
Upper eyelid blepharoplasty is a common procedure that should be in the armamentarium of the aesthetic and reconstructive surgeon. This procedure can transform a person's life through improvement in appearance and visual function. Upper eyelid blepharoplasty should not be considered in isolation, but rather in the context of rejuvenation of the upper third of the face. Functional indications for surgery include significant upper eyelid dermatochalasis encroaching on the visual axis and impeding peripheral vision, associated upper eyelid entropion or lash ptosis causing ocular surface irritation, and severe blepharitis and excessive dermatochalasis affecting prosthetic function in the anophthalmic socket. Cosmetic indications include aesthetically displeasing dermatochalasis and upper eyelid fullness.
The foundation of successful blepharoplasty begins with a complete preoperative evaluation, a discussion of expectations, the selection of the appropriate surgical technique, and a discussion of potential complications. Preoperative and postoperative photographs are essential for the documentation of functional and cosmetic patients.
Preoperative Evaluation
The preoperative evaluation begins with a careful history to elicit patient's concerns, expectations, and motivations for blepharoplasty. Establishing a strong physician–patient relationship will ensure both parties are satisfied during all phases of care. For functional patients, documentation of impaired visual symptoms, visual field testing showing improvement with eyelid lifting, and photographic documentation showing the degree of skin redundancy are required for many third-party payers. Cosmetic patients should show their areas of concern by using a mirror in their discussion with the physician. Photographs in the frontal, three-quarter profile, and side profiles should be obtained.
Surgeons should pay particular attention to a history of previous facial surgery, trauma, neuromodulators and soft tissue fillers, medication allergies, anticoagulants, and over-the-counter supplements. Patients with a history of multiple cosmetic surgeries by different surgeons with minimally evident complaints are concerning for body dysmorphic syndrome, and surgery should be avoided at all costs. Ocular symptoms such as dry eye and a history of refractive surgery should be elicited to minimize postoperative ocular surface complications.
The surgeon should have intimate knowledge of the anatomical relationships of the seven layers of the upper eyelid (Fig. 1). Within the upper eyelid, there are two fat pads. The nasal and the central/preaponeurotic fat pads have distinctive appearances because of the differential content of carotenoids (Fig. 2).1 The fullness of the specific upper eyelid fat pads should be noted and addressed during blepharoplasty. With aging, there is a selective loss of the central/preaponeurotic fat pad with relative preservation of the nasal fat pad.1 The degree of dermatochalasis is documented, and the height and shape of the eyelid crease is measured and recorded. Upper eyelid ptosis may be coexistent; this can also be addressed at the time of surgery (Fig. 3).2 In Asian patients, the patient's preference for a crease is critical and needs to be discussed prior to surgery (this aspect is beyond the scope of this discussion).3 Lateral fullness may be due to the prolapse of the lacrimal gland (Fig. 2). This can be addressed with the repositioning of the lacrimal gland during blepharoplasty rather than excision of the prolapsed gland, as this will lead to dry eye. Asymmetric or atypical fullness of the lacrimal gland warrants biopsy to rule out malignancy.
Fig. 1.
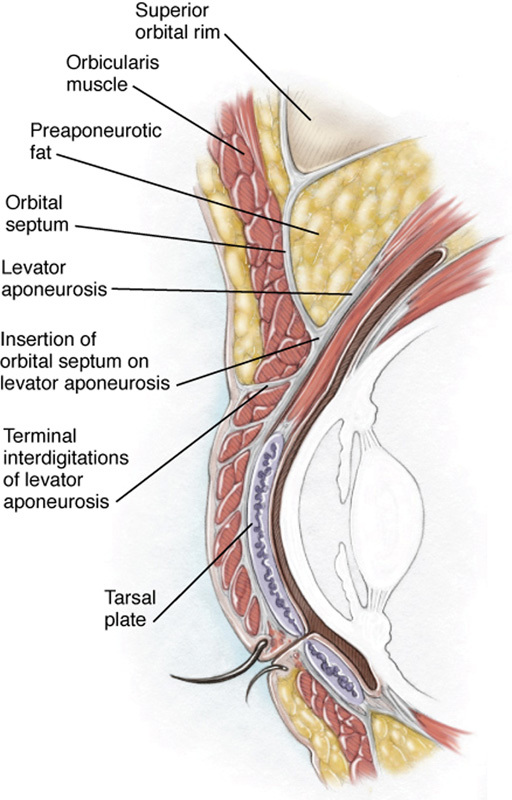
Cross-sectional anatomy of the upper eyelid.
Fig. 2.
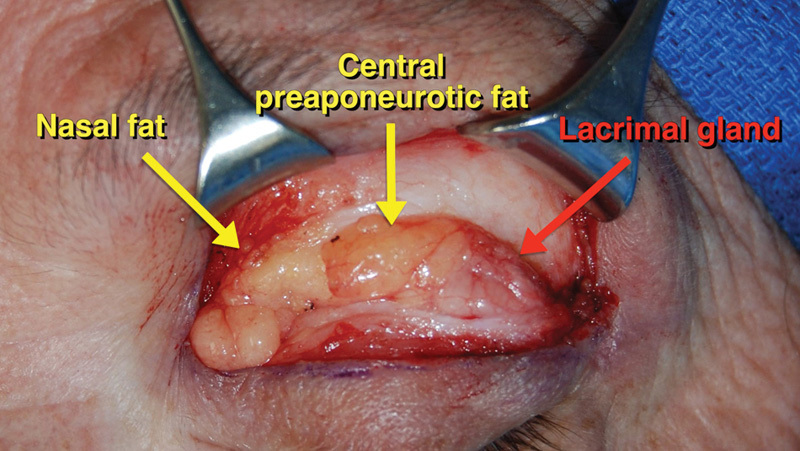
Exposure of the upper eyelid fat pads and lacrimal gland. The nasal fat pad has a paler color compared with the orange-colored central preaponeurotic fat pad. Care is taken to avoid damage to the lacrimal gland during blepharoplasty.
Fig. 3.
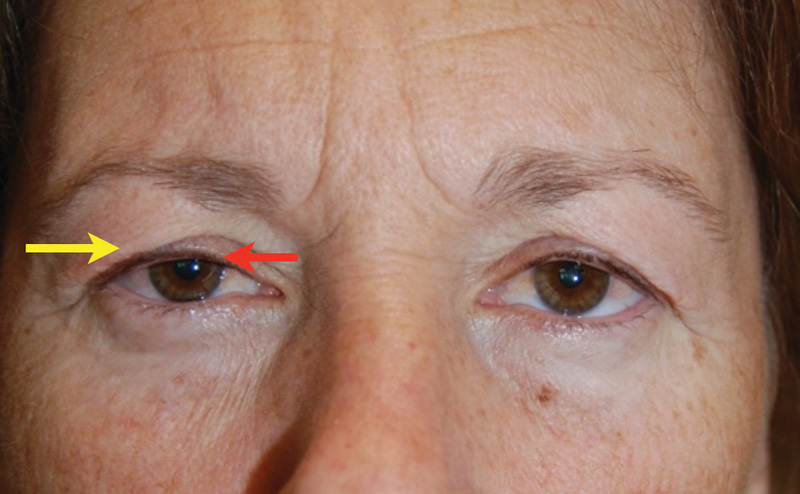
Concurrent upper eyelid dermatochalasis (yellow arrow) and blepharoptosis (red arrow).
Examination of the eyebrows is essential in any blepharoplasty patient. The position and shape of the brow should be documented. In general, females have a higher and more arched brow compared with the lower and flatter configuration of the male brow (Fig. 4). Brow ptosis is generally defined as descent below the superior orbital rim. In patients with significant upper eyelid dermatochalasis, compensatory brow elevation may be present. Postoperatively, brow descent may occur after upper eyelid blepharoplasty as there is loss of brow recruitment after the visual axis has been cleared by the surgery. Careful documentation and discussion with the patient will minimize unexpected outcomes. Brow ptosis and rejuvenation techniques, though not discussed here, may be performed concurrently with upper blepharoplasty.
Fig. 4.

Configuration of the male (A) versus female brow (B). The male brow has a flatter shape compared with the more curved, arching brow in females. Brow ptosis can be concurrently treated during upper eyelid blepharoplasty.
The ocular examination should include evaluation of the tear film and tear lake, corneal evaluation for dryness and the presence of scars, and an assessment for lagophthalmos with gentle eyelid closure. Patients with a history of refractive surgery, such as laser in situ keratomileusis (LASIK), are particularly prone to dry eye syndrome after blepharoplasty and quantitative tear measurements such as Schirmer's testing should be performed.4 Management of any dry eye symptoms should be optimized prior to blepharoplasty with artificial tears and immune modulators such as topical cyclosporine and punctal occlusion.
Informed consent, postoperative care, a discussion of complications, and the possible need for revision surgery should be addressed during the preoperative evaluation. Determining and setting realistic goals and expectations should be established prior to surgery. As discussed earlier, screening for complicated patients, such as those with body dysmorphic syndrome or other psychopathology, is essential as surgery will not cure these conditions and psychiatric consultation may be warranted.
Skin Marking
Accurate skin marking of the upper eyelids is an essential step for successful upper eyelid blepharoplasty. Typically, the native eyelid crease is utilized. In non-Asians, the central eyelid crease height is typically 6 to 9 mm in males and 8 to 11 mm in females. In Asians, the eyelid crease is often much closer to the lid margin, averaging 4 to 6 mm in males and 6 to 8 mm in females. This is a result of the position where the levator aponeurosis fuses with the orbital septum, which is much higher in the occidental eye. If the upper eyelid crease is unusually high or asymmetric, levator dehiscence-related blepharoptosis should be suspected and the crease should be marked at the native crease position, not the crease position resulting from the levator dehiscence. The nasal aspect of the upper eyelid crease marking should be tapered slightly upward and not extend past the punctum to avoid medial upper eyelid webbing. Laterally, the marking is extended beyond the lateral canthus if hooding is present.
Next, two toothless forceps are used to pinch redundant skin for excision. The inferior arm of the forceps will pinch the previously marked lid crease, and the upper arm will pinch the upper limits of excision. No lagophthalmos should be induced with the forceps; at most, a minimal eversion of the lashes may be noted. Initial markings are made centrally, medially, and laterally, and then connected in a curvilinear fashion to trace out a natural appearing curve of the skin crease incision. In marking the area of skin excision, care must be taken to ensure that 20 mm of skin remains between the upper eyelid margin and the lower border of the eyebrow to avoid anterior lamellar deficiency. Fig. 5 shows a typical upper eyelid blepharoplasty marking in a patient with significant lateral hooding. If general anesthesia is not used, the patient is asked to open and close his or her eyelids; one should aim to have an overlap of the upper and lower markings of the upper eyelid skin. Excess ink on the skin should be blotted with gauze to minimize diffusion of the mark.
Fig. 5.

(A) The pinch technique is used to identify excess upper eyelid dermatochalasis. (B) A typical upper eyelid blepharoplasty showing extension of the mark beyond the lateral canthus to address hooding.
Blepharoplasty is routinely performed in an outpatient setting under local anesthesia without monitored anesthesia care. General anesthesia may be used, but this is often reserved for combined cases involving the forehead and lower face. We use a local anesthetic mixture containing 1% lidocaine, 0.25% bupivacaine, and 1:200,000 epinephrine. To minimize discomfort, the mixture can be buffered with sodium bicarbonate. The bicarbonate should be mixed freshly as the higher pH can result in precipitation of the anesthetic and decreased efficacy. The anesthetic mixture is given subcutaneously, with the needle directed away from the globe. Additional anesthetic is given in the superonasal quadrant to reduce discomfort when sculpting the nasal fat pad. Prior to sterile preparation with 5% povidone iodine, a topical anesthetic is given to minimize corneal and conjunctival discomfort.
Surgical Technique
Multiple modalities may be used for the surgical incision including a surgical blade, CO2 laser, and radiofrequency needle. Regardless of the instrument, a corneal shield should be placed prior to incision to protect the eye. We prefer making all skin incisions with a standard no.15 blade. Next, the skin is removed with Westcott scissors or cutting cautery. The orbicularis oculi is typically preserved to minimize problems with eyelid closure postoperatively. A caveat to this suggestion is in the Asian eyelid: trimming of a thin 1.0- to 2.0-mm cuff of orbicularis oculi muscle along the incision will facilitate a more natural, flattening contour of the newly formed upper eyelid crease. Hemostasis is achieved with the light application of a bipolar cautery.
If selective orbital fat is to be removed, the orbital septum is opened medially to identify the nasal fat. Care should be taken to avoid excessive manipulation in the superomedial orbit as the trochlea and superior oblique muscle are located in this region. The nasal fat pad can be distinguished from the central fat pad as the former is lighter yellow in color. The amount of nasal fat pad to be removed can be estimated by applying slight pressure on the globe to assess the degree of nasal fat prolapse. After fat sculpting, careful hemostasis is achieved. If the lacrimal gland is prolapsed, it can be resuspended by 5–0 Prolene suture fixation to the periosteum along the inner aspect of the superolateral orbital rim. Upper eyelid ptosis repair can be performed through an anterior or posterior approach when appropriate.
Layered closure is achieved with interrupted 7–0 Vicryl sutures for the reapproximation of the orbicularis oculi muscle. Skin closure is performed with a running 6–0 fast absorbing gut suture or a 6–0 Prolene suture. The latter is removed at the 1-week postoperative visit. Tissue glues have been described, but we feel this is unnecessary and may have a higher rate of postoperative wound dehiscence. Final postoperative photographs are documented at the 3-month visit (Fig. 6).
Fig. 6.
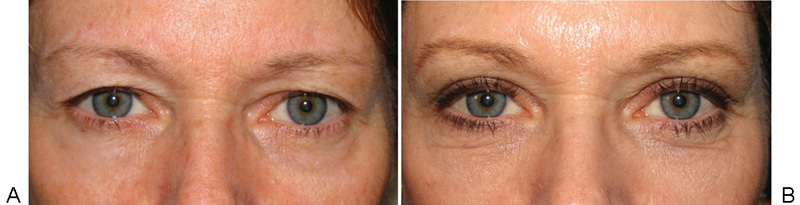
Before (A) and after (B) upper eyelid blepharoplasty with nasal fat removal and orbicularis oculi preservation at 3 months postoperatively.
Postoperative Care
Patients are instructed to use a combination antibiotic and steroid ophthalmic ointment twice daily on the incisions. Ice packs are applied at 30-minute intervals for the first 3 days and the patient is instructed to sleep with the head of the bed elevated to approximately 30 degrees. The first postoperative visit is at 1 week after surgery.
Complications
As with any procedure, complications may occur despite careful planning and meticulous surgical technique. Prior to discharge, warnings signs of bleeding, vision loss, compartment syndrome, and infection are reviewed. Patients should be given appropriate discharge paperwork with instructions and contact information during and after office hours to mitigate postoperative complications. In this section, we review several potential complications of blepharoplasty and how to minimize them.
Asymmetry
Asymmetry may be one of the most common complaints after upper eyelid blepharoplasty surgery. The adage, “measure twice, cut once” should be followed. Also, the surgeon should assess for blepharoptosis and eyelid malposition preoperatively, and address these as well to achieve symmetrical results. Asymmetry may also be a result of globe prominence that may not have been detected preoperatively. Therefore, careful measurements as well as preoperative photos from multiple angles must be performed. Residual skin is not considered a complication per se and patients should be counseled that revision surgery may be performed postoperatively.
Lagophthalmos
Lagophthalmos and resultant dry eyes are a complication of upper eyelid blepharoplasty. Early temporary lagophthalmos can occur due to edema from the surgery or orbicularis paresis from anesthesia or surgical trauma. To prevent such complications, the surgeon should utilize conservative skin markings to retain at least 20 mm of upper eyelid skin, measured centrally from the lower margin of the brow to the lid margin. Also, the surgeon should minimize removal of the orbicularis oculi muscle, as removal may result in poor closure of the eyelids.5 Treatment involves the supplementation of the anterior lamella from a suitable donor site (Fig. 7). Despite full-thickness skin grafting, insufficient orbicularis may be present, which leads to continued lagophthalmos. In such cases, upper eyelid loading with a weight may be necessary.
Fig. 7.

(A) Anterior lamellar deficiency and lagophthalmos resulting from the excessive removal of upper eyelid skin and orbicularis muscle. (B) Placement of a full-thickness skin graft from the retroauricular area with improvement in eyelid closure.
Lacrimal Gland Injury
The lacrimal gland may be damaged iatrogenically during blepharoplasty, resulting in diminished tear production. The surgeon should not mistake the lacrimal gland as redundant preaponeurotic fat. In addition to the lateral position, the lacrimal gland has a more pale appearance than the preaponeurotic fat and attempted removal with sharp dissection or cutting cautery often results in more patient discomfort owing to its richer sensory innervation. If prolapsed, the gland can be reposited along the periosteum.
Canthal Webbing
Postoperative canthal webbing is aesthetically displeasing and may be noticed by the patient and/or surgeon. An effective preventive measure is to taper the nasal incision markings superiorly and to avoid extending the marking medially to the punctum. Medial canthal webbing can be revised with a Z-plasty. Similarly, the upper and lower incision markings should not be tapered down sharply; this may result in lateral canthal webbing.
Postoperative Hemorrhage
Hemorrhage is a possible complication of any surgical procedure. Preseptal hematomas can be managed conservatively with ice, rest, and elevation of the head of the bed. Retrobulbar hemorrhages are the most concerning, as they may result in an orbital compartment syndrome and loss of vision.6 Patients must be educated on the warning of signs and symptoms of vision-threatening hemorrhage and to seek emergent medical attention. The first step in the management of this condition is to open the blepharoplasty incision (Fig. 8). If this does not adequately reduce orbital pressure, then an emergent lateral canthotomy and cantholysis are performed. Meticulous hemostasis during the procedure, the use of tapered rather than cutting needles for skin closure, the application of ice packs postoperatively, and the cessation of anticoagulants before surgery will minimize the risk of postoperative hemorrhage.
Fig. 8.

Postoperative retrobulbar hemorrhage treated by evacuation through the upper eyelid blepharoplasty incision. If necessary, a lateral canthotomy and cantholysis may be performed to further relieve an orbital compartment syndrome.
Blepharoptosis
Blepharoptosis may be apparent after upper eyelid blepharoplasty. As mentioned above, the surgeon must assess for ptosis preoperatively and should consider treating the condition concurrently.2 Furthermore, to prevent iatrogenically induced blepharoptosis, the surgeon should be cognizant of the levator that is located posterior to the preaponeurotic fat pad, and avoid excessive pretarsal dissection. Additionally, the surgeon should avoid excessive downward traction of the upper eyelid during surgery, as this may result in iatrogenic dehiscence or damage to the levator palpebrae.
Corneal Abrasion
Corneal abrasions can easily occur if preventative precautions are not taken. The surgeon should use corneal shields with lubricating ointment during surgery to prevent this complication.7 Any corneal abrasion should be treated postoperatively by an eye-care specialist, as these may develop into corneal ulcers. Most mechanical abrasions heal within 24 to 72 hours with proper treatment and monitoring. When using CO2 laser or radiofrequency ablation, inadvertent corneal scarring and perforation may occur and the use of a metallic corneal shield is warranted.
Wound Dehiscence
Postoperative wound dehiscence can occur and requires repair if it is large in size or involves prolapsed deep tissues. Smaller dehiscences may be observed (Fig. 9). To minimize this complication, the patient should be advised to avoid eye rubbing and to use ice packs to minimize hemorrhage and itching. In addition, the patient should use protective eye shields while sleeping, and should not perform any heavy lifting. They should also avoid wearing contact lenses for the first 2 weeks postoperatively.
Fig. 9.
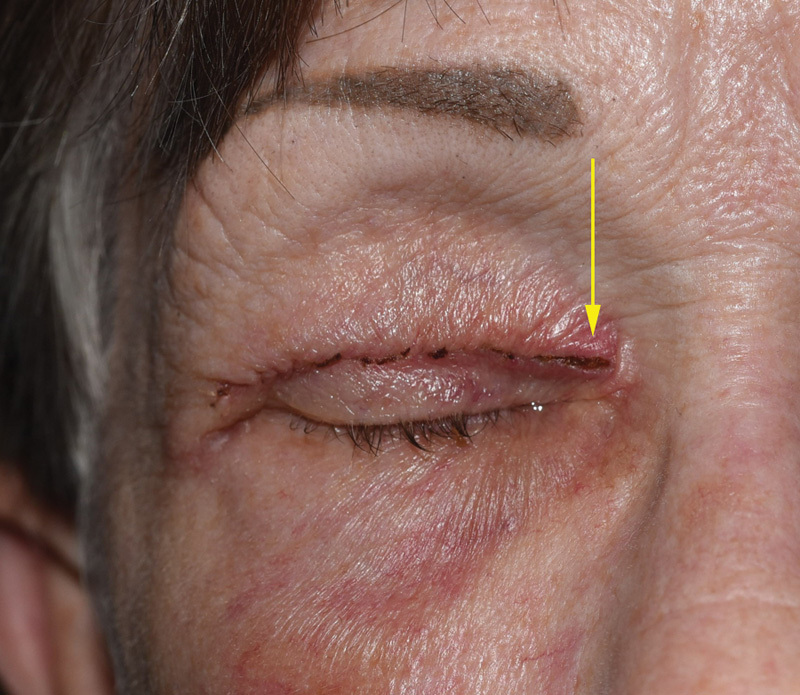
Dehiscence of the medial aspect of the blepharoplasty incision.
Suture Granulomas
Suture granulomas may occur from the use of delayed absorbable sutures such as polygalactin. The use of nonabsorbable sutures (such as polypropylene or nylon) can significantly reduce the risk of these reactions. Granulomas should be treated with early removal of the remaining absorbable suture. Additionally, the application of an antibiotic/steroid ointment or a steroid injection can be performed. If the suture granuloma persists, the surgeon can make a small linear “nick” skin incision and excise the granuloma in the office, allowing the minute skin incision to close by secondary intent. The clinician should have a high index of suspicion for atypical mycobacterial infections that can present as delayed hyperemic nodules along incision lines (Fig. 10). Its diagnosis requires long-term repeat cultures and chronic treatment with macrolide antibiotics.8
Fig. 10.

Delayed, hyperemic nodule along the blepharoplasty incision caused by an atypical mycobacterial infection.
Postoperative Infection
Infections after upper eyelid blepharoplasty are not common owing to the robust vascular supply of the periorbita. However, infections from methicillin-resistant staphylococcus aureus (MRSA) are increasing in frequency. Adherence to sterile surgical technique and a high index of suspicion for MRSA is essential for nonresolving infections. Orbital cellulitis should be considered in any patient with proptosis, pain, decreased vision, and extraocular motility dysfunction. Bacterial cultures, orbital imaging, intravenous antibiotics, and hospital admission may be necessary.
Postoperative Diplopia
Diplopia is uncommon, but should be differentiated between monocular or binocular. Monocular diplopia is likely caused by ocular surface changes from ointment, dry eye, or refractive changes after eyelid surgery. Binocular, vertical diplopia suggests damage to the trochlea and/or superior oblique (iatrogenic Brown's syndrome) from overzealous resection of the nasal fat.9 The surgeon must understand not only the anatomy of the eyelid, but the orbit as well.
Superior Sulcus Deformity
The superior sulcus deformity refers to a deep and hollow appearance of the superior sulcus. This complication can be minimized by preserving the preaponeurotic fat pad during blepharoplasty. The surgeon can differentiate the medial fat pad, which is a lighter yellow color, from the preaponeurotic central fat pad, which is darker yellow.10 With aging, the medial fat pad tends to prolapse, whereas the preaponeurotic central fat pad tends to involute with time. Furthermore, the surgeon must attempt to minimize damage to the levator palpebrae muscle during surgery, as damage to the levator may result in levator aponeurosis dehiscence from its normal attachment to the tarsal plate, resulting in the appearance of a high and deep superior sulcus.
Multiple Upper Eyelid Creases
It is possible to have multiple upper eyelid creases postoperatively; careful preoperative markings must be performed to avoid this complication. The surgeon should avoid excessive pretarsal dissection and resection of tissue and try to preserve the central fat pad. Multiple creases secondary to volume deflation may be treated with hyaluronic filler to volumize the area of multiple creases.11
Operating Room Fires
Operating room fires are a serious hazard during surgery. Cautery instrument tips should not contact cotton tip applicators, cotton sheets, paper drapes, and eyelashes. If supplemental oxygen is used, the oxygen cannula should be above the surgical drape to avoid an oxygen trap. Furthermore, oxygen exposure near the tips of the cut and cautery instruments should be avoided. Operating room fires can be a devastating complication of surgery; care must be taken to avoid such hazards.
Conclusion
The upper eyelid blepharoplasty procedure is a safe and effective procedure with an overall high patient-satisfaction rate. Taking the necessary precautions to prevent complications and recognizing and treating them promptly are important in achieving optimal postoperative outcomes. Preoperative assessment, understanding the patient's expectations and desired outcomes, meticulous measurements for skin markings, and proper surgical technique all play important roles in achieving the best surgical results.
Acknowledgment
This study was supported by a grant from the Research to Prevent Blindness organization.
References
- 1.Oh S R, Chokthaweesak W, Annunziata C C, Priel A, Korn B S, Kikkawa D O. Analysis of eyelid fat pad changes with aging. Ophthal Plast Reconstr Surg. 2011;27(5):348–351. doi: 10.1097/IOP.0b013e3182141c37. [DOI] [PubMed] [Google Scholar]
- 2.Neimkin M G, Couch S M, Holds J B, Bodnar Z M, Reggie S N. The role of surgeon technique in current practice patterns for combined ptosis and dermatochalasis. Ophthal Plast Reconstr Surg. 2016 doi: 10.1097/IOP.0000000000000668. [DOI] [PubMed] [Google Scholar]
- 3.Park D D. Aging Asian upper blepharoplasty and brow. Semin Plast Surg. 2015;29(3):188–200. doi: 10.1055/s-0035-1556853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korn B S, Kikkawa D O, Schanzlin D J. Blepharoplasty in the post-laser in situ keratomileusis patient: preoperative considerations to avoid dry eye syndrome. Plast Reconstr Surg. 2007;119(7):2232–2239. doi: 10.1097/01.prs.0000260750.15059.17. [DOI] [PubMed] [Google Scholar]
- 5.Rees T D. The “dry eye” complication after a blepharoplasty. Plast Reconstr Surg. 1975;56(4):375–380. doi: 10.1097/00006534-197510000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Teng C C, Reddy S, Wong J J, Lisman R D. Retrobulbar hemorrhage nine days after cosmetic blepharoplasty resulting in permanent visual loss. Ophthal Plast Reconstr Surg. 2006;22(5):388–389. doi: 10.1097/01.iop.0000235500.88819.c8. [DOI] [PubMed] [Google Scholar]
- 7.Parikh M, Kwon Y H. Vision loss after inadvertent corneal perforation during lid anesthesia. Ophthal Plast Reconstr Surg. 2011;27(5):e141–e142. doi: 10.1097/IOP.0b013e31822d5d6d. [DOI] [PubMed] [Google Scholar]
- 8.Mauriello J A Jr; Atypical Mycobacterial Study Group. Atypical mycobacterial infection of the periocular region after periocular and facial surgery Ophthal Plast Reconstr Surg 2003193182–188. [DOI] [PubMed] [Google Scholar]
- 9.Syniuta L A, Goldberg R A, Thacker N M, Rosenbaum A L. Acquired strabismus following cosmetic blepharoplasty. Plast Reconstr Surg. 2003;111(6):2053–2059. doi: 10.1097/01.PRS.0000056840.61348.35. [DOI] [PubMed] [Google Scholar]
- 10.Sires B S, Saari J C, Garwin G G, Hurst J S, van Kuijk F J. The color difference in orbital fat. Arch Ophthalmol. 2001;119(6):868–871. doi: 10.1001/archopht.119.6.868. [DOI] [PubMed] [Google Scholar]
- 11.Choi H S, Whipple K M, Oh S R. et al. Modifying the upper eyelid crease in Asian patients with hyaluronic acid fillers. Plast Reconstr Surg. 2011;127(2):844–849. doi: 10.1097/PRS.0b013e3181fed6cb. [DOI] [PubMed] [Google Scholar]


