Abstract
Orbital fractures are very common after facial trauma. The assessment of a patient with a suspected orbital wall injury includes a detailed oculofacial examination as well as radiologic imaging. Surgical repair with or without an implant may be indicated for diplopia, enophthalmos, or both. Cicatricial eyelid malposition is an iatrogenic complication commonly due to poor orbitotomy technique. Optimal repair involves direct exposure of the perimeter of the fractures' site through surgical planes that minimally scar the eyelids. A wide variety of implant options exist; however, thin, pliable, nonadherent materials such as nylon foil may offer several advantages. The authors describe the evaluation and management of orbital wall fractures.
Keywords: orbit fracture, orbital floor, medial orbital wall, orbit implant, blow-out, enophthalmos, entrapment
Fractures to the orbital walls commonly result after blunt trauma to the midface. Although great force is generally required for breaks in the superior or lateral walls, the thin bones of the medial wall and orbital floor easily fracture with mild-to-moderate trauma. Disruption of one or more of these walls can expand orbital volume, confine orbital soft tissue, or both. The ophthalmologic manifestations include enophthalmos and impaired extraocular motility. The repair of orbital fractures involves fracture site exposure, freeing tissue prolapsed into the fracture site, and reapproximating the orbital wall support, usually with an implant. Surgical reconstruction should account for the complex curvatures of each wall that combine to form a conoid shape with its apex in the superomedial posterior orbit. Here we review the evaluation and repair of the most common orbital fractures of the orbital floor, medial wall, and a combination of the two.
Evaluation of Orbital Fractures
Clinical Evaluation
A complete ophthalmic examination is essential for any patient presenting with periocular or ocular trauma. A detailed eye exam is necessary to rule out globe trauma prior to further manipulation, especially orbital or facial fracture repair. The surgical repair of orbital or facial fractures may place pressure on the globe, aggravate ophthalmologic injuries, and seriously compromise the potential for vision recovery (Fig. 1).
Fig. 1.
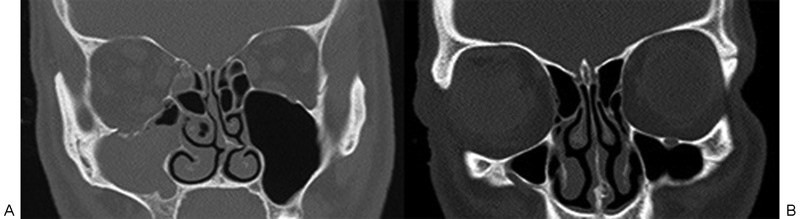
Coronal computed tomography images of the obits showing a left inferior orbital wall fracture (A) and irregularity of the nasal globe contour of the left eye (B) suggesting a globe rupture.
There are several common clinical exam findings, regardless of the etiology of the fractures, suggestive of an orbital fracture (Table 1). Varying degrees of periorbital ecchymosis and edema are typical after trauma. Crepitus may be noted if air from the sinuses has tracked into the subcutaneous tissues after nose blowing or sneezing. Point tenderness or step-offs along the orbital rim may be noted in the location of a possible fracture involving the orbital rim. Restricted extraocular muscle movements may be present due to multiple mechanisms. Orbital tissue edema and muscle entrapment are common etiologies as is the loss of wall support (Table 2; Figs. 2, 3). Posttraumatic dysmotility may also ensue from direct muscle damage or edema and nerve damage. Although radiographic imaging can be used to evaluate for muscle involvement, muscle entrapment is a clinical diagnosis. Once the globe is deemed intact and stable, some advocate forced duction testing in the assessment of eye movement problems. Forced duction testing, however, may be misleading in the acute post trauma setting due to hemorrhage and edema. Additionally, forced ductions are extremely uncomfortable with a patient who is awake. We advocate forced duction testing only on a limited basis, under anesthesia if possible, and only if the findings will significantly change clinical or surgical management. In cases of entrapped orbital tissue, a surgeon should rely on direct visualization of the fracture site and not forced duction testing as evidence of release of tissue incarceration.
Table 1. Clinical examination findings indicating possible orbital fractures.
| Periorbital ecchymosis or edema |
| Step-offs along orbital rim |
| Point tenderness along the orbital rim Restricted extraocular movements |
| Numbness along distribution of the inferior orbital nerve |
| Asymmetry of globe position |
| Enophthalmos on exophthalmometry |
Table 2. Clinical examination findings indicating entrapment of extraocular muscle.
| Restricted extraocular movements |
| Restricted eye movements with forced duction testing |
| Nausea |
| Vomiting |
| Bradycardia from oculocardiac reflex |
Fig. 2.

Photographs of a patient with a left inferior orbital wall fracture showing restriction of both upgaze (A) and downgaze (B).
Fig. 3.
Coronal computed tomography image of the patient from Fig. 2 showing a left inferior orbital wall fracture and displacement of the inferior rectus muscle, which is also shown to be caught along the medial edge of the fracture site.
Asymmetry of globe positioning may be noted both initially and subsequently after orbital swelling has improved. Inferior displacement of the globe may be seen after a large inferior orbital wall fracture. Exophthalmometry measurements may show enophthalmos on the side of the fracture with large orbital wall fractures increasing the orbital volume (Fig. 4). Often, enophthalmos is not present in the acute setting due to edema, hemorrhage, or both, and exophthalmometry may even show exophthalmos. Dysmotility and globe displacement can lead to diplopia in different directions of gaze. Anesthesia in the distribution of the infraorbital nerve (including the lower eyelid, cheek, upper lip, and gums on the affected side) is common because most inferior orbital wall fractures are adjacent to the infraorbital neovascular bundle. Canthal dystopia may be seen at the lateral commissure in zygomatic fractures and at the medial commissure in nasoethmoidal fractures. Nasoethmoidal fractures can also cause damage to the lacrimal system and predispose patients to epiphora. An afferent pupillary defect may be seen in patients with fractures that extend into the optic canal or in cases of traumatic optic neuropathy or other types of eye trauma. Frontal bone trauma at the brow may rarely transmit forces directly to the optic nerve without obvious fractures. Ophthalmic examination can reveal many common signs of ocular trauma, including subconjunctival hemorrhage, hyphema, traumatic mydriasis, traumatic cataract, vitreous hemorrhage, retinae commotio, retinal detachment, retinal hemorrhage, and other traumatic posterior segment findings.
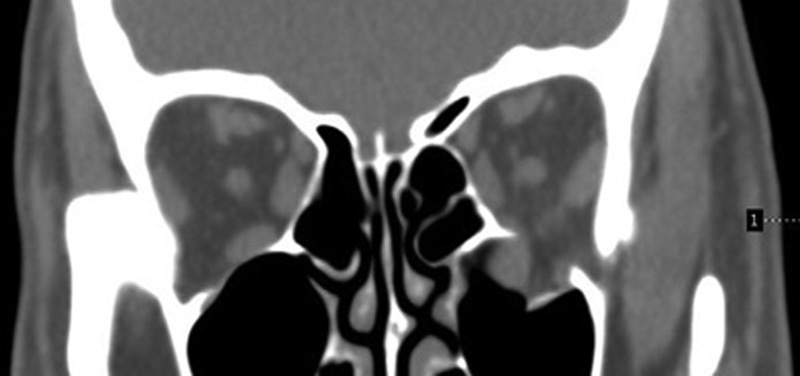
Fig. 4.
Photograph (A) showing evidence of enophthalmos on the left that is suggested clinically by the smaller palpebral fissure and deepened superior sulcus. Coronal computed tomography image (B) showing an inferior orbital wall fracture and an increase in the orbital volume compared with the noninjured right orbit.
Radiographic Evaluation
Computed tomography (CT) is ideal in the trauma setting to not only assess the orbit, but to evaluate for cranial or other extraorbital injury. A CT can also identify intraocular (Fig. 5) or intraorbital foreign bodies (Fig. 6), especially metallic foreign bodies. Magnetic resonance imaging is contraindicated when a metallic foreign body is suspected due to the possibility of magnet-induced metal displacement and further injury during imaging.1 2
Fig. 5.
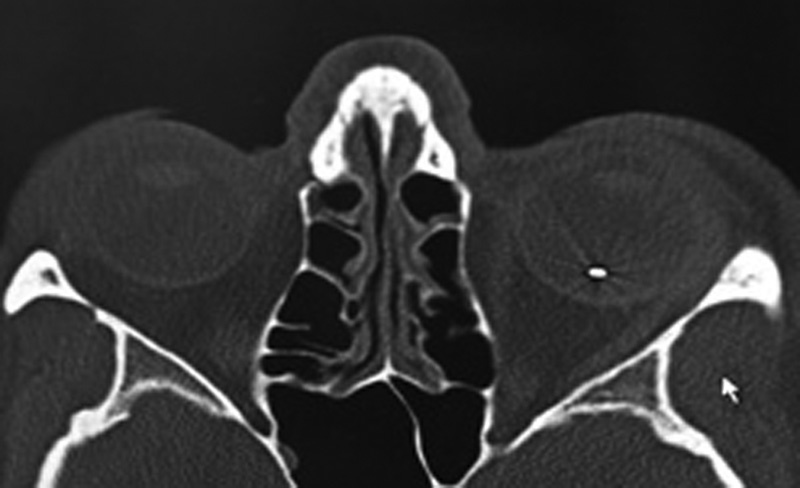
Axial computed tomography image showing an intraocular foreign body of the left eye in the setting of an open globe injury from a ceiling fan falling.
Fig. 6.

Coronal computed tomography image showing an intraorbital foreign body of the right orbit adjacent to the globe. The patient had been hammering a nail.
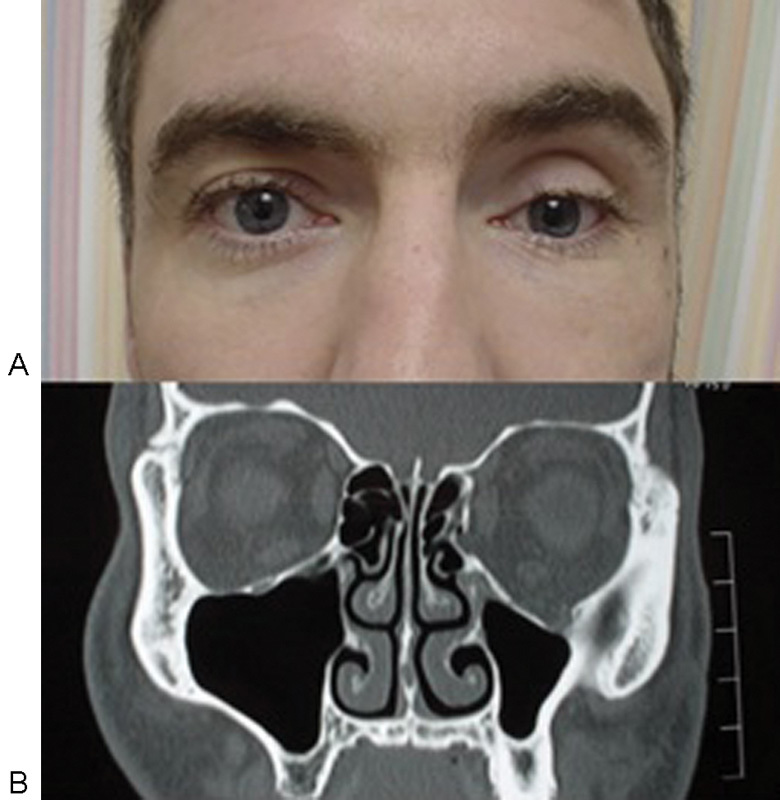
Computed tomography without contrast is also the imaging option of choice for the evaluation of orbital and facial fractures.3 A CT of the orbits and face with thin cuts (1.5–2 mm) is recommended to provide sufficient detail. Coronal views can often show details of orbital floor fractures best (Fig. 7).4 Changes in the shape of rectus muscles on coronal views are useful to assess for traction on periorbital soft tissues and muscle. For instance, with an inferior entrapment, the normal round or horizontal axis oval appearance of the inferior rectus may appear elongated into a vertical oval on cross section. Axial and sagittal views are also helpful in the evaluation of fractures and in tracking extraocular muscles along their orbital course (Fig. 8). Three-dimensional reconstruction can help demonstrate spatial relationships of larger facial fractures, but have limited usefulness for orbital wall fractures. The displacement of orbital bones is best assessed in the bone window, whereas orbital soft tissue herniation and muscle entrapment can be best assessed in the soft tissue window. The extent of bone displacement seen on imaging can be helpful in determining if surgical repair is necessary, as a larger orbital floor fracture with greater displacement of orbital tissues will more likely result in enophthalmos and require surgical repair. A careful evaluation of the images for associated facial fractures, involving the frontal, zygomatic, maxillary, nasal, and mandibular bones and orbital buttresses, is also important. Other findings on imaging in the setting of an orbital floor fracture may include opacification of the maxillary sinuses and displacement of the globe (Fig. 9).
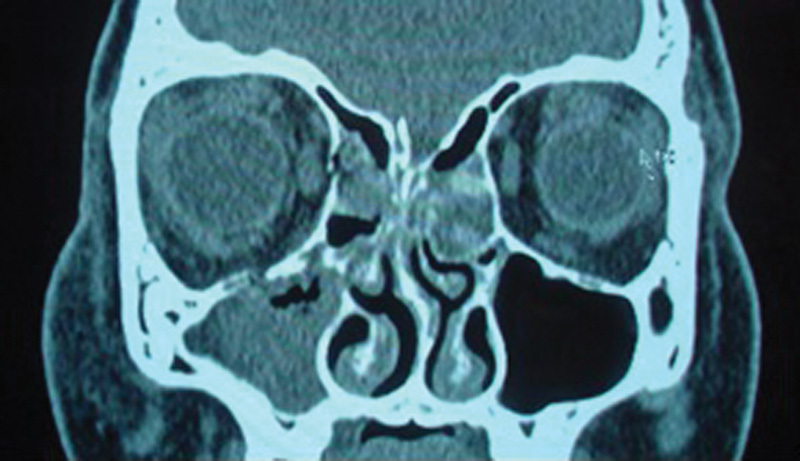
Fig. 7.

Coronal computed tomography image showing an inferior orbital wall fracture on the left.
Fig. 8.
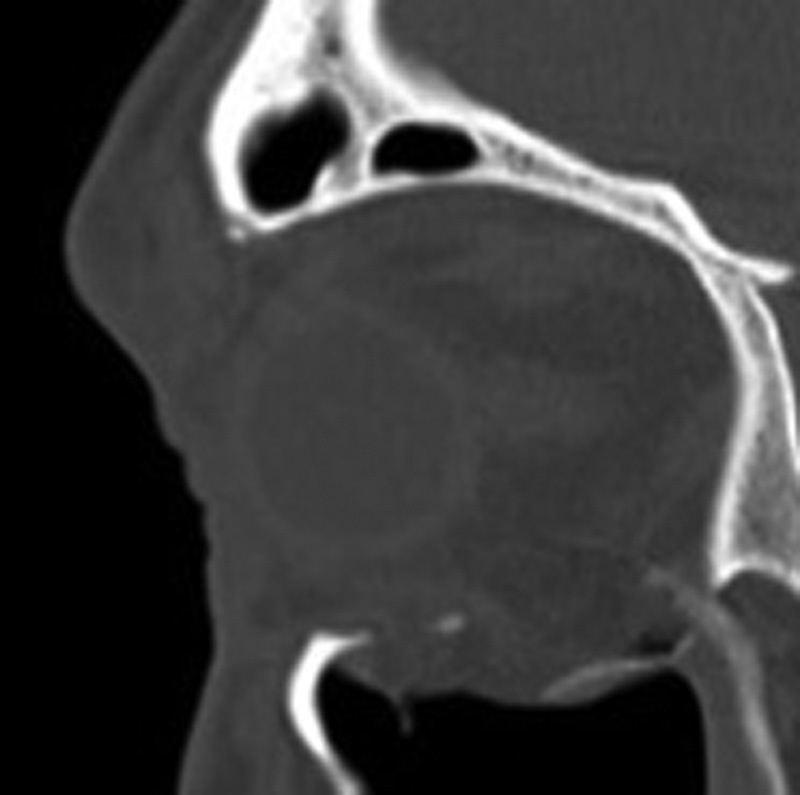
Sagittal computed tomography image showing the inferior rectus herniating in the location of the inferior orbital wall fracture.
Fig. 9.
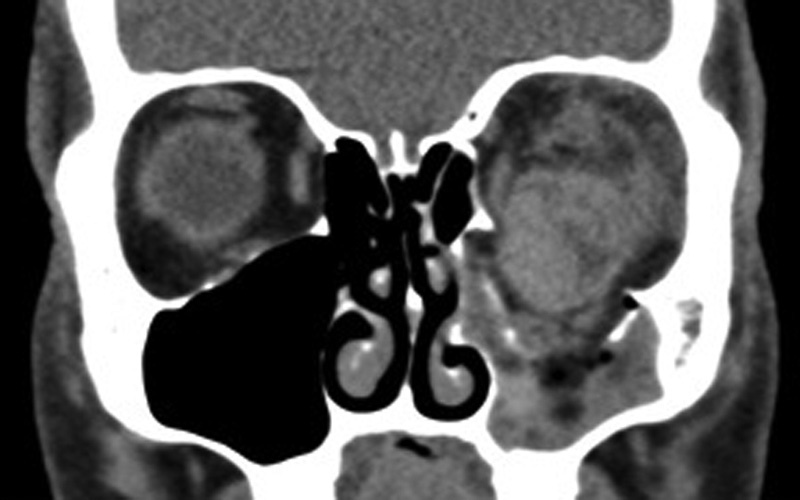
Coronal computed tomography image showing significant left globe displacement inferiorly through the inferior orbital wall fracture and into the maxillary sinus.
Inferior Wall Fractures
Orbital floor fractures are caused by either hydraulic mechanisms, in which an increase in orbital pressure is transmitted by the orbital soft tissues to the orbital walls causing a “blowout” fracture, or by buckling mechanisms, as a result of deformation of the orbital rim transmitting force to the thinner orbital floor bones posteriorly, or a combination of the two mechanisms.5
Anatomy
The normal orbital volume is ∼30 mL.6 7 The orbital floor is composed of the maxillary, zygomatic, and palatine bones and is the shortest of all of the orbital walls measuring 35 to 40 mm. It terminates at the posterior edge of the maxillary sinus. The infraorbital groove, canal, and foramen traverse the length of the inferior orbital floor and tunnel through the maxilla encasing the infraorbital neurovascular bundle. The infraorbital nerve exits through the infraorbital foramen and provides sensory innervations to the lower eyelid, midface, upper lip, and gums. The orbital floor is also in close proximity to the inferior rectus and inferior oblique muscles. The inferior oblique muscle arises from the orbital surface of the maxilla just lateral to the lacrimal grove, then passes laterally, posteriorly, and superiorly (inferior to the inferior rectus muscle) to insert on the sclera just underneath the lateral rectus muscle.
The anatomical landmarks of most fractures correlate with the bony anatomy. Floor fractures often extend up the infraorbital groove and/or the canal. The infraorbital nerve can commonly be contused in orbital floor fractures causing hypoesthesia in the V2 distribution. Posteriorly, the orbital floor is usually intact because it is part of the strong palatine bone.
Clinical Evaluation for Inferior Orbital Wall Fractures
Several clinical exam findings may be suggestive of an inferior orbital wall fracture. There may be a step-off along the inferior orbital rim if the fracture extends anteriorly. Restriction of upgaze may be seen if there is entrapment of the inferior rectus muscle in the fracture site. If the infraorbital neovascular bundle has been injured (if the fracture involves the infraorbital groove or is located adjacent to it), hypesthesia may be present in the area supplied by the infraorbital nerve. Hypoglobus or enophthalmos may be noted if there is a large inferior orbital wall fracture with significant loss of support. Blood in the maxillary sinus can also be a helpful clue to the possible presence of an orbital floor fracture.
White-Eyed Blowout Fractures
Children may show a different constellation of symptoms and signs than adults in the setting of an orbital blowout fracture. Children may present with a “white eye” with a very minimal amount of periorbital edema, subconjunctival hemorrhage, or injection.8 Extraocular movement examination may show restricted movement if a muscle is entrapped, most commonly during upgaze when the inferior rectus is trapped in an inferior orbital wall fracture, which can improve significantly after repair (Fig. 10). This restricted gaze may be seen in combination with nausea, vomiting, increased pain, and bradycardia from an oculocardiac reflex. A CT of the orbit may show minimal disruption of the orbital floor and a fracture (Fig. 11).8 These fractures may be difficult to detect on imaging because pediatric orbital bones are significantly more elastic and may snap back into their original position following the initial outfracture. Importantly, one should not rely on CT to diagnose extraocular muscle entrapment. Restricted eye movements with a high clinical suspicion for muscle entrapment should prompt urgent surgical intervention. Esmaeli et al reviewed 20 patients who presented with white-eyed blowout fractures. Restrictive strabismus resolved much more rapidly in patients who underwent surgery within days (2–4 days) compared with the patients who were repaired in weeks (2–4 weeks)—these patients also had a slower recovery and several were noted to have permanent restrictive changes.8
Fig. 10.

Photographs of a patient with a white-eyed blowout fracture on the right, showing restriction in upgaze on the right prior to surgical repair (A) and improvement in upgaze after surgical repair (B).
Fig. 11.
Coronal computed tomography image showing the inferior orbital wall fracture on the right with minimal bone displacement.
Indications for Repair
Isolated inferior orbital wall fractures do not require emergent surgical intervention unless there is concern for extraocular muscle entrapment. If restrictive strabismus or significant globe malposition is present, then surgical intervention is indicated (Table 3). Patients with orbital floor fractures are often observed for 1 to 2 weeks to allow for the spontaneous resolution of orbital edema and presenting symptoms.9 Indications for repair within this 2-week period include
Table 3. Clinical examination findings indicating entrapment of extraocular muscle.
| Restricted extraocular movements |
| Restricted eye movements with forced duction testing |
| Nausea |
| Vomiting |
| Bradycardia from oculocardiac reflex |
Persistent diplopia, especially in primary or downgaze, or concern for orbital restriction
Enophthalmos > 2 mm
Malposition of the globe, either posterior or inferior displacement
A large orbital floor fracture (greater than 50% of orbital floor) or significant increase in orbital volume in which enophthalmos is predicted
Associated rim or facial fractures causing disfigurement or other facial pathophysiology (e.g., oral malocclusion in low maxillofacial fracture, trismus with zygomaticomaxillary complex fracture)
Surgical Approach
Anesthesia: Orbital fracture repair is usually performed under general anesthesia. We use 1% lidocaine with 1:100,000 epinephrine combined with 0.5% bupivacaine and bicarbonate injected subconjuntivally in the inferior fornix and at the lateral canthus.
Forced ductions under anesthesia: A forced duction test may be helpful to evaluate for globe restriction due to entrapment. Some surgeons repeat this test after completion of the surgery to assess for release of the restriction; however, we advocate direct visualization of soft tissue release from the perimeter of the fracture site as the primary measure.
Incision: We favor a lateral canthotomy and inferior cantholysis (swinging eyelid) inferior fornix transconjunctival incision, a well-described approach to orbital floor fractures (Fig. 12).10 11 12 13 14 15 A lateral canthotomy incision is fashioned using a No. 15 blade. This is continued using straight scissors, then the inferior ramus of the lateral canthal tendon is severed. Conjunctiva and lower eyelid retractors are incised at the inferior one-quarter and superior three-quarters line between the inferior fornix and inferior aspect of the tarsus.12 14 Dissection is continued down the infraorbital rim in the septal plane, where the periosteum is elevated (Fig. 13). Dissection is then initiated in the preseptal plane, avoiding the orbicularis muscle anteriorly and orbital fat posteriorly, to expose the periosteum along the inferior orbital rim. External subciliary or direct rim incisions have also been described, but are not preferred due to the risks of cicatricial eyelid malposition and the visibility of the scar.16 Transnasal and transantral endoscopic management of orbital floor fractures are also alternate, less-direct approaches.17 18
Fig. 12.
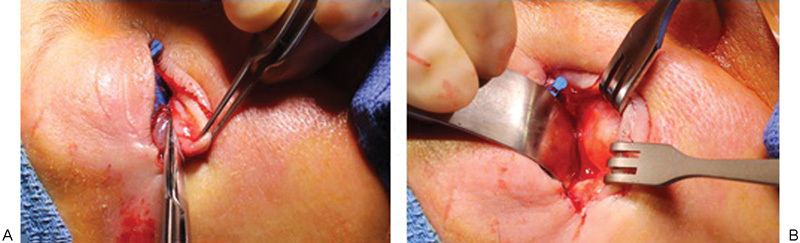
(A) The lower eyelid is distracted inferiorly after canthotomy/cantholysis and a conjunctiva/retractor band incision is created. (B) With blunt manipulation, a malleable distracts orbit tissue posteriorly, while Senn retractors keep anterior lamella tissues out of the way of the subsequent periosteal incision.
Fig. 13.
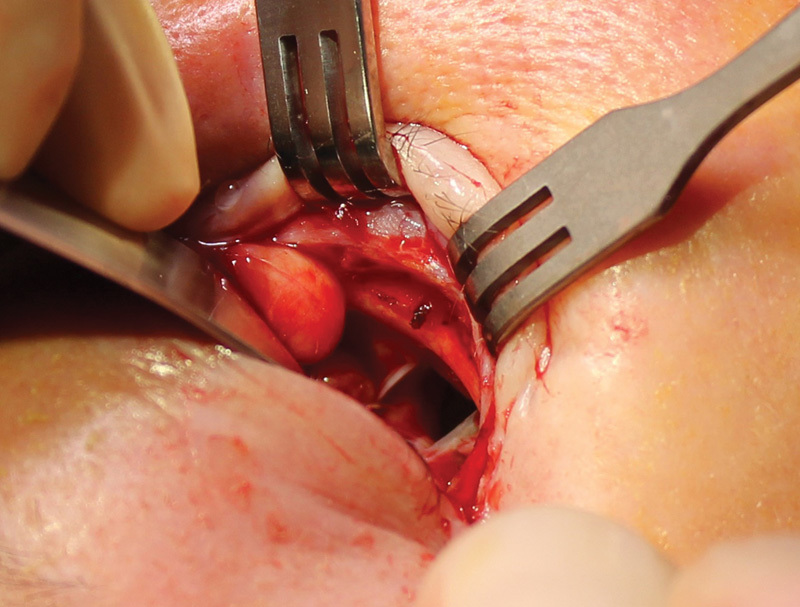
Lifting the periosteum exposes the inferior wall fracture.
Exposure of the orbital floor: A Freer or Cottle elevator is used to gently elevate the periosteum posteriorly into the orbit. A malleable reactor can be used to protect the globe and elevate the orbital tissues for improved visualization. Orbital soft tissues are carefully elevated from the fracture site in a hand-over-hand technique. The orbital floor fracture is often found in the inferomedial orbit. The orbital tissue that has herniated through the fracture site can be carefully elevated and retracted with a malleable retractor. Care must be taken to avoid damage to the infraorbital neovascular bundle. Out-fractured fragments of bone can be extracted with the aid of a muscle hook or forceps. The orbital floor fracture must be completely exposed, especially the posterior edge of the fracture to ensure that all herniated or entrapped tissue has been freed. The posterior wall of the maxillary sinus is a useful landmark, signifying the apex. Dissection superior to the sinus should not proceed further posteriorly than the depth of the posterior maxillary sinus wall owing to the risk of injury to the optic nerve. Often, adequate exposure of the posterior medial floor fracture requires exposure from a separate approach. We recommend opening the medial wall through a transcaruncular incision, if the posterior medial floor fracture ledge is not apparent or the implant will not seat easily, or both.
Placement of an orbital floor implant: There are a wide variety of orbital implants that are available for orbital floor fracture repair. We prefer nonporous alloplastic thin implants such as nylon. This type of implant has been used to repair orbital blowout fractures since two case reports in 1961 by Browning and Walker popularized its use.19 These implants are available in thicknesses that range from 0.05 to 2.0 mm; we prefer the Nylon foil implants of 0.35-mm thickness. This thickness is flexible enough to conform to orbital walls, yet rigid enough to provide adequate support of the orbital contents. It is also useful in combined fractures of the inferior and medial orbital walls due to its flexibility. Placement of too large of an implant can cause displacement of the globe or can affect the function of the extraocular muscles. The size and flexibility of the nylon foil implant allows for reconstruction of a similar shape and structure to the original orbital walls. We also prefer the nonporous aspect of this implant and do not fixate the implant within the orbit or encourage fibrovascular ingrowth into the implant, because this may also encourage cicatricial changes of the extraocular muscles directly adjacent to the implant and subsequent diplopia.14 It is important to have the fracture fully visualized. The implant is cut to fit the floor of the orbit with enough overlap over the fracture edges (Fig. 14). If further modification of the size is needed, the edges of the implant are trimmed until the ideal fit is achieved. The posterior aspect of the implant should rest on the orbital floor posterior to the most posterior aspect of the fracture site. The anterior aspect of the implant rests comfortably inside the orbital rim. Implants well seated across the perimeter of the fracture site with abundant overlap onto the nondisplaced bone do not require fixation and a tamponade effect of orbit soft tissues further hold them in place, as a scar capsule forms that further stabilizes the device.
Fig. 14.
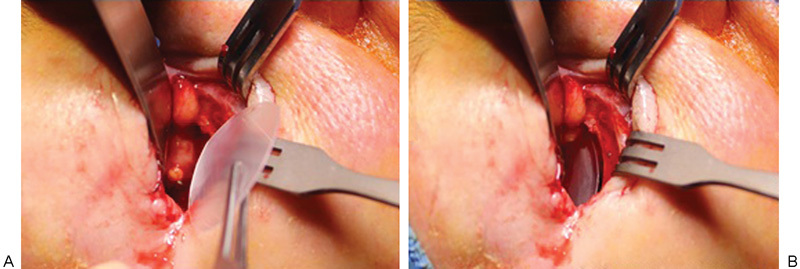
(A) A nylon foil implant is cut to approximate the size of the floor fracture. (B) The implant is place to cover the fracture with stable bone for peripheral support.
Closure: The conjunctiva and the lower eyelid retractors are then closed with interrupted 6–0 mild chromic or plain gut sutures (Fig. 15). Sutureless transconjunctival repair has also been described, but we recommend a few interrupted sutures reapproximating the retractor band to forestall reverse ptosis.20 Ophthalmic antibiotic ointment can be placed in the eye. No patch is placed to provide continued observation of the globe in the postoperative period. Orbital hemorrhage is the main concern in the more immediate postoperative period, so careful vision monitoring is important.
Fig. 15.
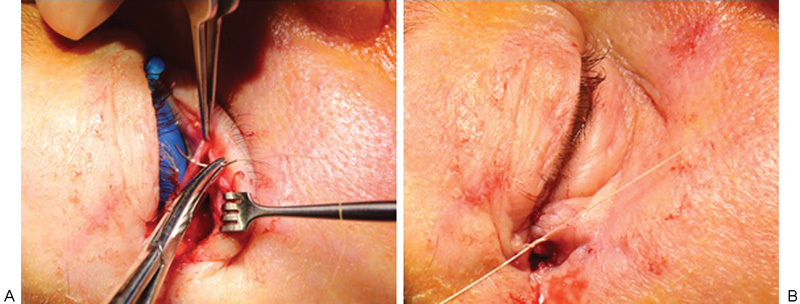
(A) The fornix incision is closed with a buried 6–0 chromic suture. (B) The lateral tarsus is secured to the lateral rim periosteum with a 4–0 Vicryl suture.
Alternate Options for Orbital Fracture Implants
There exist a wide variety of implant choices used in orbital wall repair.14 21 22 23 24 25 26 Alloplastic materials are now more commonly used than autogenous tissues due to their ease in availability and lack of harvesting procedure requirements (Table 4). We have a strong preference for thin (0.35 mm) nylon foil (SupraFOIL; Supramid) owing to its balance of pliability and rigidity, nonadherent surface, and ability to implant or explant through small incisions with implant folding. Other implants that have been described include silicone (Silastic; Dow Corning), hydroxyapatite (such as Biocoral), polytetrafluoroethylene (Teflon orbital implants), titanium mesh (such as that from KLS Martin, Stryker Craniomaxillofacial, and Synthes, Inc.), porous polyethylene (Medpor; Porex Surgical), and porous polyethylene with embedded titanium (Medor Titan; Porex Surgical).
Table 4. Orbital implant options.
| Alloplastic implants |
| Nonporous implants |
| Nylon (SupraFOIL) implant |
| Silicone (Silastic) |
| Polytetrafluoroethylene (Teflon) |
| Titanium |
| Porous implants |
| Porous polyethylene (Medpor) |
| Porous polyethylene with embedded titanium (Medpor Titan) |
| Autogenous tissues |
| Bone grafts–cranial bone, iliac crest, rib bone |
Medial Wall Fractures
Overview
Medial wall fractures can occur in isolation or in conjunction with an orbital floor fracture. The overall evaluation and indications for repair of a medial wall fracture are similar to that of an inferior wall fracture as expansion of volume can result in enophthalmos and tissue entrapment can result in diplopia. Entrapment of tissue of the medial orbit including the medial rectus muscle can occur with a medial wall fracture; therefore, the careful evaluation of horizontal gaze can help to identify restriction.
Anatomy
The medial wall is primarily composed of the thin lamina papyracea of the ethmoid bone and includes the lacrimal bone anteriorly, the maxillary bone inferiorly, and the lesser wing of the sphenoid posteriorly. The suture line at the superior border of the medial wall between the ethmoid bone and the frontal bone is readily identifiable by the anterior and posterior ethmoidal arteries. This border is an important landmark, as breaks superior to a suture communicate to the fovea ethmoidalis and can expose dura. The location of the ethmoidal arteries also aids in approximating orbital depth, as the anterior artery is 24 mm from the lacrimal crest and the posterior artery is an additional 12 mm of depth and just 6 mm from the orbital apex. The thin ethmoidal bone transitions to a thick strut of bone inferiorly, which provides significant support for the orbit and is often preserved in orbital fractures.
Surgical Approach
The medial wall can be exposed through either a transcutaneous incision or a transcaruncular incision. A skin incision allows for access to extraorbital facial injuries and the repair of naso-orbitoethmoid complex fractures, when present. The resultant scar is usually inconspicuous. A caruncular incision avoids a cutaneous wound altogether. Through either incision dissection, one should take care to preserve the lacrimal system and the medial canthal tendon. The periosteum is then incised and elevated and a periosteal elevator and malleable are used to expose the borders of the fracture and free herniated tissue from the fracture site. As with the inferior wall fracture, there are a variety of orbital implants available; our preference is for a thin (0.35 mm) nylon foil implant. After placement of the implant, its security on stable bone is confirmed and the wound is closed.
Combined Floor and Medial Wall Fractures
With combined fractures of the medial wall and the orbital floor, there may be a loss of the inferonasal support to the orbit, creating a challenging reconstruction of orbital volume. In this case, repair of the individual fracture sites may fail to approximate the inferonasal support of the strut. Access to both the floor and medial wall is complicated by the inferior medial origin of the inferior oblique muscle from the maxillary bone near the lacrimal fossa. Options for the re-creation of the transition from the inferior to medial wall include rigid implants fixed anteriorly, or larger implants seated high on the medial wall extending past the lateral floor defect such as nylon foil in a “wraparound” technique.14
Complications
Orbital fracture repair may be associated with significant morbidity for patients. Visual loss following fracture repair is generally the result of retrobulbar hemorrhage in the acute presentation that causes orbital compartment syndrome. In the case of an orbital compartment syndrome, the intraocular pressure is acutely elevated and can be relieved by a canthotomy and cantholysis procedure of the lower eyelid with or without the upper eyelid to control pressure.
Diplopia may result from extraocular muscle ischemia or scarring due to the trauma or from persistent entrapment of the muscle. Neurogenic causes from trauma present with diplopia and full ductions on exam, generally observation for a period of at least 3 months should be undertaken before any intervention, as neurogenic diplopia may resolve gradually without surgery. Adhesion to orbital implants can be considered in cases of late-onset diplopia and may require removal or revision of the implant.
Enophthalmos after orbital fracture can result in significant facial asymmetry. Failure to restore orbital volume after surgical correction, the shifting of an orbital implant, or atrophy of orbital contents after trauma can lead to persistent enophthalmos. Imaging may aid in the evaluation of persistent enophthalmos to guide possible revision of the fracture repair.
Infection after an orbital fracture is uncommon; there is no consensus on the use of antibiotics after an orbital fracture. Infection or significant surrounding inflammation of an orbital implant may require removal of the implant.
Eyelid malposition including lower eyelid retraction, entropion, or ectropion may occur after trauma as well as surgical exposure of the fracture site. Care must be taken with orbital access and wound closure so as to not cause adhesions or cicatricial changes to the eyelids and soft tissues.
Conclusion
Orbital fractures are commonly seen in the setting of trauma to the midface. Evaluation and management of orbital fractures requires a deep understanding of orbital anatomy and physiology. The goals of orbit repair are to restore orbital positioning and eye movement in a safe and effective manner.
References
- 1.Grove A S Jr New diagnostic techniques for the evaluation of orbital trauma Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol 197783(4 Pt 1):626–640. [PubMed] [Google Scholar]
- 2.Grove A S Jr. Orbital trauma and computed tomography. Ophthalmology. 1980;87(5):403–411. doi: 10.1016/s0161-6420(80)35219-6. [DOI] [PubMed] [Google Scholar]
- 3.Grove A S Jr. Computed tomography in the management of orbital trauma. Ophthalmology. 1982;89(5):433–440. doi: 10.1016/s0161-6420(82)34770-3. [DOI] [PubMed] [Google Scholar]
- 4.Grove A S Jr Tadmor R New P F momose K J Orbital fracture evaluation by coronal computed tomography Am J Ophthalmol 197885(5 Pt 1):679–685. [DOI] [PubMed] [Google Scholar]
- 5.Raflo G T. Blow-in and blow-out fractures of the orbit: clinical correlations and proposed mechanisms. Ophthalmic Surg. 1984;15(2):114–119. [PubMed] [Google Scholar]
- 6.Zide B M Jelks G W Surgical Anatomy of the Orbit 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1985 [Google Scholar]
- 7.Kahana A Lucarelli M J Burkat C N Dortzbach R K Diagnosis and management of orbital fracturesIn: Mallajosyula S, ed., Surgical Atlas of the Orbit Delhi, India: Jaypee Brothers; 2008 [Google Scholar]
- 8.Jordan D R, Allen L H, White J, Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthal Plast Reconstr Surg. 1998;14(6):379–390. doi: 10.1097/00002341-199811000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Hawes M J, Dortzbach R K. Surgery on orbital floor fractures. Influence of time of repair and fracture size. Ophthalmology. 1983;90(9):1066–1070. doi: 10.1016/s0161-6420(83)80049-9. [DOI] [PubMed] [Google Scholar]
- 10.Tenzel R R, Miller G R. Orbital blow-out fracture repair, conjunctival approach. Am J Ophthalmol. 1971;71(5):1141–1142. doi: 10.1016/0002-9394(71)90592-7. [DOI] [PubMed] [Google Scholar]
- 11.Tessier P. The conjunctival approach to the orbital floor and maxilla in congenital malformation and trauma. J Maxillofac Surg. 1973;1(1):3–8. doi: 10.1016/s0301-0503(73)80005-0. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg R A, Lessner A M, Shorr N, Baylis H I. The transconjunctival approach to the orbital floor and orbital fat. A prospective study. Ophthal Plast Reconstr Surg. 1990;6(4):241–246. doi: 10.1097/00002341-199012000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Kushner G M. Surgical approaches to the infraorbital rim and orbital floor: the case for the transconjunctival approach. J Oral Maxillofac Surg. 2006;64(1):108–110. doi: 10.1016/j.joms.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 14.Nunery W R, Tao J P, Johl S. Nylon foil “wraparound” repair of combined orbital floor and medial wall fractures. Ophthal Plast Reconstr Surg. 2008;24(4):271–275. doi: 10.1097/IOP.0b013e3181788de8. [DOI] [PubMed] [Google Scholar]
- 15.McCord C D Jr, Moses J L. Exposure of the inferior orbit with fornix incision and lateral canthotomy. Ophthalmic Surg. 1979;10(6):53–63. [PubMed] [Google Scholar]
- 16.Appling W D, Patrinely J R, Salzer T A. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg. 1993;119(9):1000–1007. doi: 10.1001/archotol.1993.01880210090012. [DOI] [PubMed] [Google Scholar]
- 17.Cheong E C, Chen C T, Chen Y R. Endoscopic management of orbital floor fractures. Facial Plast Surg. 2009;25(1):8–16. doi: 10.1055/s-0028-1112226. [DOI] [PubMed] [Google Scholar]
- 18.Strong E B, Kim K K, Diaz R C. Endoscopic approach to orbital blowout fracture repair. Otolaryngol Head Neck Surg. 2004;131(5):683–695. doi: 10.1016/j.otohns.2004.05.017. [DOI] [PubMed] [Google Scholar]
- 19.Browning C W, Walker R V. Polyethylene in posttraumatic orbital floor reconstruction. Am J Ophthalmol. 1961;52:672–677. doi: 10.1016/0002-9394(61)90152-0. [DOI] [PubMed] [Google Scholar]
- 20.Ho V H, Rowland J P Jr, Linder J S, Fleming J C. Sutureless transconjunctival repair of orbital blowout fractures. Ophthal Plast Reconstr Surg. 2004;20(6):458–460. doi: 10.1097/01.iop.0000143715.26518.4c. [DOI] [PubMed] [Google Scholar]
- 21.Rubin P A, Bilyk J R, Shore J W. Orbital reconstruction using porous polyethylene sheets. Ophthalmology. 1994;101(10):1697–1708. doi: 10.1016/s0161-6420(94)31113-4. [DOI] [PubMed] [Google Scholar]
- 22.Morrison A D, Sanderson R C, Moos K F. The use of silastic as an orbital implant for reconstruction of orbital wall defects: review of 311 cases treated over 20 years. J Oral Maxillofac Surg. 1995;53(4):412–417. doi: 10.1016/0278-2391(95)90714-9. [DOI] [PubMed] [Google Scholar]
- 23.Custer P L, Lind A, Trinkaus K M. Complications of supramid orbital implants. Ophthal Plast Reconstr Surg. 2003;19(1):62–67. doi: 10.1097/00002341-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Aronowitz J A, Freeman B S, Spira M. Long-term stability of Teflon orbital implants. Plast Reconstr Surg. 1986;78(2):166–173. doi: 10.1097/00006534-198608000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Polley J W, Ringler S L. The use of Teflon in orbital floor reconstruction following blunt facial trauma: a 20-year experience. Plast Reconstr Surg. 1987;79(1):39–43. [PubMed] [Google Scholar]
- 26.Park D J, Garibaldi D C, Iliff N T, Grant M P, Merbs S L. Smooth nylon foil (SupraFOIL) orbital implants in orbital fractures: a case series of 181 patients. Ophthal Plast Reconstr Surg. 2008;24(4):266–270. doi: 10.1097/IOP.0b013e31817e0fe0. [DOI] [PubMed] [Google Scholar]


