Abstract
Aging changes to the lower eyelids and midface include pseudoherniated orbital fat, tear trough deformity, lid laxity, and dermatochalasis. Surgical repair often aims at treating redundant skin or orbital fat malposition with a lower eyelid blepharoplasty. Either a transcutaneous or transconjunctival approach may be used, though recent trends have favored the transconjunctival technique if procedures require more than simple skin excision. In manipulating the inferior orbital fat pads, a surgeon has many options including excision, repositioning, or augmentation with synthetic dermal filler, autologous fat grafts, or acellular dermal allografts. The authors review and detail indications, preoperative evaluation, techniques, and complications of lower lid blepharoplasty.
Keywords: lower lid blepharoplasty, infraorbital fat, tear trough deformity
Lower eyelid and midface changes are frequently the first aesthetic complaints of an aging patient. A youthful eyelid–cheek complex is classically defined as a single convex line seen on profile view.1 As people age, the globe may descend within the orbit, leading to a pseudoherniation of orbital fat and subsequent double-convex lower eyelid contour. The midface may likewise descend, leading to inferiorly displaced cheek fat and a tear trough deformity. Common complaints are bags or circles under the eyes or a chronically tired look. Many techniques and approaches exist to address these concerns, including both noninvasive (e.g., filler, lasers, or chemical resurfacing) and invasive (e.g., blepharoplasty or midface lift) procedures. The exact surgical approach remains controversial and is largely dependent upon surgeon preference and a patient's stated cosmetic desire. Given the meteoric rise in cosmetic procedures in the United States,2 an increasing elderly population, and emerging less-invasive surgical techniques for cosmetic correction of the lower eyelid, these procedures can only be expected to grow in frequency. Here we review the indications, preoperative considerations, operative techniques, and complications of lower lid blepharoplasty.
Indications
The most common reasons for lower lid blepharoplasty consultation are aging changes, such as excessive skin, lower lid laxity, laxity or hypertrophy of the orbicularis, herniated orbital fat, malar festoons, nasojugal folds, or tear trough deformities.3 4 5 Zoumalan et al detailed an algorithm to determine whether a patient was a candidate for lower lid blepharoplasty based on seven criteria, including the presence and extent of herniated orbital fat, the presence of infraorbital rim hollowing, amount of excess skin, appearance of midface volume loss, Fitzpatrick score, eyelid–cheek vector, and lid tone.6 It is important to note when one might pursue nonsurgical options. Patients without herniated fat pads or excess skin may benefit from more conservative treatment with dermal fillers, or in patients with Fitzpatrick skin type III or less—chemical peeling and laser resurfacing.3 Alternatively, these modalities may be combined as an adjuvant to surgery.7
Preoperative Evaluation
A careful medical history and evaluation of the periorbital region are essential to a successful lower lid blepharoplasty. A thorough past medical and past ocular history should be obtained. Chronic medical conditions including hypertension, diabetes mellitus, cardiac events, bleeding or clotting disorders, thyroid abnormalities, and previous surgical history should be noted, as well as current medication use. Anticoagulants should be withheld for at least 2 weeks prior to surgery. A detailed ocular history and careful ophthalmic exam including visual acuity as well as the presence of ocular surface disease or conditions that may predispose to an ocular surface disease. Unrecognized dry eye syndrome may be associated with long-term morbidity in these patients if appropriate measures are not taken.8 9 10 Particular note should be given to previous refractive procedures (e.g., laser epithelial keratomileusis or photorefractive keratectomy); blepharoplasty should be delayed at least 6 months following refractive surgery.8 11 Smoking is another common, yet often overlooked pre-existing condition that may predispose patients to tear film abnormalities and subsequent ocular surface disease.12 Preoperative smoking-cessation counseling is warranted in these patients. Finally, medications such as niacin, echinacea, and kava should be held as they may predispose the patient to ocular surface disease.3 8
A detailed examination of the relevant anatomy is essential for an optimal outcome. The lower eyelid margin should rest at the inferior corneal limbus with its lowest point slightly temporal to the pupil center. The lid crease should be 2 mm below the lash line medially and 5 mm laterally.13 The lower eyelid is conventionally divided into three lamellae: an anterior lamella consisting of skin and orbicularis oculi muscle, a middle lamella consisting of the orbital septum, and a posterior lamella consisting of the tarsal plate, eyelid retractors, and palpebral conjunctiva. The lower lid retractors include the capsulopalpebral fascia, a web-like band of connective tissue that transmits forces from the inferior rectus to the lower lid, and the inferior tarsal muscle. Both the capsulopalpebral fascia and the inferior tarsal muscle insert onto the tarsal plate. Of particular consideration in lower lid blepharoplasty are postseptal infraorbital fat pads, of which there are three: the medial, central, and lateral. Note that the inferior oblique muscle separates the medial and central fat pads and aggressive dissection in this area may lead to postoperative damage and strabismus.
One should also make note of atypical anatomy, including excessive skin, lid laxity, fat prolapse, orbital vector, tear trough deformity, or malar festoons. If dermatochalasis is present, assess patients with their mouth open or while looking up to stretch the skin and help estimate the amount that may be safely removed. Lid laxity may be evaluated with the snap-back and distraction tests. The snap-back test is performed by pulling the lower lid inferiorly and away from the globe and noting the time it takes for the lid to return to its normal position once released without the patient blinking. A normal lid snaps back to its native position immediately, whereas an abnormal lid may take a few seconds to return to the native position if at all. The distraction test is performed by pulling the lid away from the globe and measuring the distance to which the lid is pliable. Distraction > 6 mm is considered a positive test. Specific laxity of the medial and lateral canthal tendons should also be assessed. Medial canthal tendon laxity is measured by the punctual excursion distant on lateral distraction of the lower lid. Lateral canthal tendon laxity is measured by distracting the lid medially and noting the movement of the lateral commissure; movement > 2 mm is considered abnormal. Fat prolapse is often fairly evident. Subtle changes to the lower lid fat pads may be made more prominent in downgaze and masked in upgaze. The term negative vector describes a posterior displacement of the orbital rim in relation to the lower lid (i.e., a prominent globe relative to the maxilla) and is another involutional change seen in aging. Malar anatomy should be carefully evaluated for periorbital hollows, which may represent bony tear trough deformities or prominent nasojugal folds due to muscle displacement. The lateral canthal fold normally sits 2 mm superior to the medial canthal fold. Abnormalities in this position may be referred to as canthal tilt, and may be classified as positive, negative, or neutral.
Operative Technique
The approach to lower lid blepharoplasty may be either transcutaneous or transconjunctival; each of which has advantages and disadvantages. Apart from a surgeon's familiarity with each procedure, the need for skin resection has traditionally been the deciding factor between the two. Both approaches allow the surgeon to address herniated orbital fat as well as midface volume loss. Fat removal, fat repositioning, and augmentation with dermal filler or autologous fat grafting have become popular ways to address these concerns.
Transcutaneous Approach
The two principal methods of transcutaneous lower lid blepharoplasty are the skin flap and skin–muscle flap methods. The skin flap method is performed with a subciliary incision with the skin elevated off of the orbicularis with forceps to the level of the infraorbital rim. As originally described by Castanares,14 this incision is made 2 mm inferior to the lash line of the lower lid. Recently, McCollough et al have popularized a technique involving a subciliary incision 4 mm inferior to the lash line,15 typically at the most superior horizontal rhytid of the lower lid,16 to protect the integrity of the tarsofacial hammock. Once the incision has been made, the surgeon dissects the subcutaneous plane between the lower eyelid skin and the orbicularis muscle. The advantage of the skin flap method is the conservative removal of excess skin without disruption to the underlying orbicularis. In contrast, the skin–muscle flap method is a more aggressive procedure often used in younger patients with orbicularis oculi hypertrophy and excess lower eyelid skin. This procedure uses the dissection plane between the orbicularis and the orbital septum. As originally described,17 the excess pretarasal orbicularis muscle is trimmed. Today many surgeons prefer to trim the preseptal orbicularis muscle as it is functionally less important.18 The dissection is continued along the orbital septum with periorbital fat being accessed through small incisions in the septum. In addition to skin excision, one may also access and elevate the suborbicularis oculi fat with attachment to the external lateral orbital rim. Alternatively, one may also redrape fat, particularly if a lid swinging technique is used. Finally, with the transcutaneous approach one may also perform a simultaneous midface lift. One should be careful in the skin–muscle flap not to damage branches of the zygomatic nerve, which may lead to orbicularis hypotony and lower lid malposition.
Transconjunctival Approach
The transconjunctival approach was developed to reduce visible external scarring while simultaneously allowing access to orbital fat pads. It is a good option in patients with pseudoherniated infraorbital fat and little lid laxity, which may make the transcutaneous approach difficult.19 An incision is made in the lower conjunctiva inferior to the tarsus,4 20 21 allowing easy access to the inferior periorbital fat without violating the anterior lamella. There are two ways to access the infraorbital fat in the transconjunctival lower lid blepharoplasty: the pre- and postseptal approaches. The preseptal approach involves an incision 4 mm inferior to the tarsus, allowing the surgeon to stay anterior to the septum. Massry et al have described an incision 6 to 7.5 mm inferior to the tarsus, which allows for an entry posterior to the septum without disrupting septal integrity.22 Once accessed, fat may be manipulated as determined by the surgeon. Following fat manipulation, the septal reset technique prevents unpredictable postoperative fat migration. In this technique, orbital fat is fixated to preperiosteal fat.23 Briefly, a subciliary incision is used to release the orbital septum at the level of the arcus marginalis, a transcanthal canthopexy is performed to support the lid margin, and the septum is then fixated to the inferior orbital rim. Given that the transconjunctival approach typically avoids the orbital septum, it has a lower incidence of postoperative lid retraction.21 24
Once accessed by either the transcutaneous or transconjunctival approach, orbital fat may be excised, repositioned, or augmented with an autologous fat transplant, synthetic filler, or acellular dermal allograft. Fat excision is usually reserved for younger patients with infraorbital fat prominence and without facial degenerative changes.25 One must be judicious when removing fat as excessive removal may result in a more prominent tear trough or hollowed appearance of the lower eyelids. In addition, the periorbital fat also plays an important role in vertical globe position; removal of as little as 0.5 mL of fat may displace the globe 1 mm inferiorly and 2 mm posteriorly.19 In the older patient with volume loss in the midface, fat repositioning or redraping may be used to correct the descent of midface structures.26 27 28 29 When repositioning fat, either the supra- or subperiosteal planes are used; both have similar cosmetic results (Figs. 1 2 3 4).30
Fig. 1.
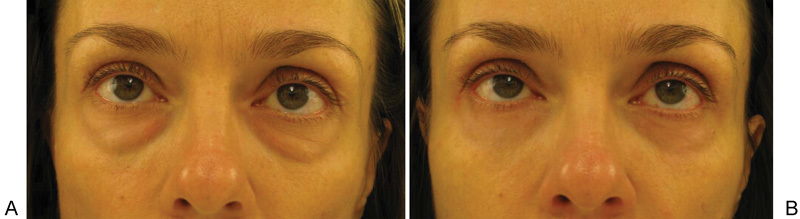
Bilateral lower eyelid fat transfer only. (A) Preoperative. (B) Postoperative.
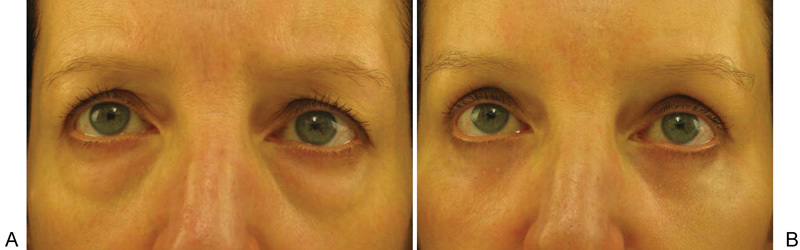
Fig. 2.

Improvement in tear trough without fat excision only. (A) Preoperative. (B) Postoperative.
Fig. 3.
Fat excision and fat transfer medially. The patient also had an upper blepharoplasty and temporal brow lift. (A) Preoperative. (B) Postoperative.
Fig. 4.

Upper and lower eyelid blepharoplasty with fat excision and festoon excision. (A) Preoperative. (B) Postoperative.
Regardless of either the transcutaneous or the transconjunctival approaches, lid laxity is commonly addressed with orbicularis and horizontal lid tightening. The lateral canthus can be elevated with suture canthopexy in the case of minimal (1–2 mm) lid laxity. For moderate (3–6 mm) laxity, lateral retinacular canthopexy may be more appropriate to elevate the lateral canthal tendon to the periosteum of the upper lateral rim.31 Severe lower lid laxity (> 6 mm) may necessitate lateral canthoplasty with lateral cantholysis for increased mobility.31 32 Alternatively, one may also consider a lateral tarsal strip.
Complications
Complications of a lower lid blepharoplasty are most commonly related to lid malpositioning, ectropion, and disruption of lamellar structures. A useful organizational tool developed by Lelli and Lisman categorizes these complications as early, intermediate, and late.33 Early complications include corneal abrasions, orbital hemorrhage, and infections. Corneal abrasions may be prevented with the use of corneal shields during surgery. Orbital hemorrhage is a rare, but potentially sight-threatening complication requiring emergent identification of the bleeding source and possibly a return to the operating room for release of the arcus marginalis and lateral canthus. These patients may require medical therapy with mannitol, acetazolamide, systemic, and topical steroids, and 95% oxygen with 5% carbon dioxide. Infections should be promptly treated with topical, and if necessary, systemic antibiotics.
Intermediate complications include eyelid malposition, strabismus, corneal exposure, and epiphora. Eyelid malpositions include lower lid retraction, lagophthalmos, and ectropion. Lower lid retraction is a common complication; it may result from damage to the anterior or middle lamella either from overzealous skin excision or disruption of the septum while trying to access orbital fat. Conservative treatment includes lid massage and Carraway exercises.6 34 35 Some authors have also suggested the injection of triamcinolone or 5-fluorouracil into the postsurgical wound as an off-label use to minimize scarring and prevent vertical lid shortening.6 33 36 If surgical revision is indicated, a full-thickness skin graft is used to correct anterior lamellar deformities and a hard-palate spacer graft or acellular dermal allograft is used to correct deformities of the middle lamella.34 Lagophthalmos may similarly result from excessive skin excision, or alternatively, damage to the zygomatic nerve leading to a reduced orbicularis tone. Exposure keratopathy and worsening of pre-existing ocular surface disease are common sequelae of lagophthalmos. Treatment in these cases involves aggressive lubrication and warm compresses; rarely, a return to the operating room may be necessary for lateral canthal repositioning. Ectropion similarly results from vertical lid shortening of the anterior lamella and may be prevented through the aforementioned lateral canthopexy to support the lower lid position in case of increasing vertical tension. Strabismus is commonly due to damage to the inferior oblique muscle, but is usually managed conservatively.
Late complications include changes in eyelid height and contour, hypertrophic scarring, and dermal pigmentation. Similar to the previously listed lid malpositions, changes in lid height and contour are often secondary to changes in the anterior and middle lamellae and require similar treatment. Visible scarring is most common after a transcutaneous approach, and may be minimized by careful preoperative consideration of incision placement.
Conclusion
To perform lower lid blepharoplasty effectively, a surgeon must be aware of the indications, alternative treatments, preoperative considerations, operative techniques, and associated complications and management. Further study is needed to clarify the advantages of the transcutaneous versus the transconjunctival surgical approaches, as well as fat repositioning and augmentation, and which populations may benefit most from these treatments.
References
- 1.Hamra S T. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg. 1995;96(2):354–362. doi: 10.1097/00006534-199508000-00014. [DOI] [PubMed] [Google Scholar]
- 2.The American Society for Aesthetic Plastic Surgery; Cosmetic surgery national databank statistics. Aesthet Surg J [serial online] Available at: http://www.surgery.org/sites/default/files/ASAPS-Stats2015.pdf. Accessed January 3, 2017
- 3.Naik M N, Honavar S G, Das S, Desai S, Dhepe N. Blepharoplasty: an overview. J Cutan Aesthet Surg. 2009;2(1):6–11. doi: 10.4103/0974-2077.53092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davison S P, Irio M, Oh C. Transconjunctival lower lid blepharoplasty with and without fat repositioning. Clin Plast Surg. 2015;42(1):51–56. doi: 10.1016/j.cps.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Pepper J P, Baker S R. Transcutaneous lower blepharoplasty with fat transposition. Clin Plast Surg. 2015;42(1):57–62. doi: 10.1016/j.cps.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Zoumalan C I, Roostaeian J. Simplifying blepharoplasty. Plast Reconstr Surg. 2016;137(1):196e–213e. doi: 10.1097/PRS.0000000000001906. [DOI] [PubMed] [Google Scholar]
- 7.Smith C B, Waite P D. Lower transcutaneous blepharoplasty. Atlas Oral Maxillofac Surg Clin North Am. 2016;24(2):135–145. doi: 10.1016/j.cxom.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Jindal K, Sarcia M, Codner M A. Functional considerations in aesthetic eyelid surgery. Plast Reconstr Surg. 2014;134(6):1154–1170. doi: 10.1097/PRS.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 9.Moss S E, Klein R, Klein B E. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118(9):1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 10.Prischmann J, Sufyan A, Ting J Y, Ruffin C, Perkins S W. Dry eye symptoms and chemosis following blepharoplasty: a 10-year retrospective review of 892 cases in a single-surgeon series. JAMA Facial Plast Surg. 2013;15(1):39–46. doi: 10.1001/2013.jamafacial.1. [DOI] [PubMed] [Google Scholar]
- 11.McKinney P Byun M The value of tear film breakup and Schirmer's tests in preoperative blepharoplasty evaluation Plast Reconstr Surg 19991042566–569., discussion 570–573 [DOI] [PubMed] [Google Scholar]
- 12.Altinors D D, Akça S, Akova Y A. et al. Smoking associated with damage to the lipid layer of the ocular surface. Am J Ophthalmol. 2006;141(6):1016–1021. doi: 10.1016/j.ajo.2005.12.047. [DOI] [PubMed] [Google Scholar]
- 13.Tan K S, Oh S-R, Priel A, New York: Springer; 2011. Surgical anatomy of the forehead, eyelids, and midface for the aesthetic surgeon; pp. 11–24. [Google Scholar]
- 14.Castanares S. Blepharoplasty for herniated intraorbital fat; anatomical basis for a new approach. Plast Reconstr Surg (1946) 1951;8(1):46–58. [PubMed] [Google Scholar]
- 15.McCollough E G, English J L. Blepharoplasty. Avoiding plastic eyelids. Arch Otolaryngol Head Neck Surg. 1988;114(6):645–648. doi: 10.1001/archotol.1988.01860180059030. [DOI] [PubMed] [Google Scholar]
- 16.Garcia R E, McCollough E G. Transcutaneous lower eyelid blepharoplasty with fat excision: a shift-resisting paradigm. Arch Facial Plast Surg. 2006;8(6):374–380. doi: 10.1001/archfaci.8.6.374. [DOI] [PubMed] [Google Scholar]
- 17.Beare R. St. Louis, MO: Mosby; 1967. Surgical treatment of senile changes in the eyelids: the McIndoe-Beare technique; pp. 362–366. [Google Scholar]
- 18.Massiha H. Combined skin and skin-muscle flap technique in lower blepharoplasty: a 10-year experience. Ann Plast Surg. 1990;25(6):467–476. doi: 10.1097/00000637-199012000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Pack S, Quereshy F A, Altay M A, Baur D A. Transconjunctival lower blepharoplasty. Atlas Oral Maxillofac Surg Clin North Am. 2016;24(2):147–151. doi: 10.1016/j.cxom.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 20.Zarem H A Resnick J I Expanded applications for transconjunctival lower lid blepharoplasty Plast Reconstr Surg 199910331041–1043., discussion 1044–1045 [DOI] [PubMed] [Google Scholar]
- 21.Baylis H I, Long J A, Groth M J. Transconjunctival lower eyelid blepharoplasty. Technique and complications. Ophthalmology. 1989;96(7):1027–1032. doi: 10.1016/s0161-6420(89)32787-4. [DOI] [PubMed] [Google Scholar]
- 22.Undavia S, Briceño C A, Massry G G. Quantified incision placement for postseptal approach transconjunctival blepharoplasty. Ophthal Plast Reconstr Surg. 2016;32(3):191–194. doi: 10.1097/IOP.0000000000000459. [DOI] [PubMed] [Google Scholar]
- 23.Hamra S T The role of the septal reset in creating a youthful eyelid-cheek complex in facial rejuvenation Plast Reconstr Surg 200411372124–2141., discussion 2142–2144 [DOI] [PubMed] [Google Scholar]
- 24.Netscher D T, Patrinely J R, Peltier M, Polsen C, Thornby J. Transconjunctival versus transcutaneous lower eyelid blepharoplasty: a prospective study. Plast Reconstr Surg. 1995;96(5):1053–1060. doi: 10.1097/00006534-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg R A, Edelstein C, Shorr N. Fat repositioning in lower blepharoplasty to maintain infraorbital rim contour. Facial Plast Surg. 1999;15(3):225–229. doi: 10.1055/s-2008-1064322. [DOI] [PubMed] [Google Scholar]
- 26.Loeb R. Fat pad sliding and fat grafting for leveling lid depressions. Clin Plast Surg. 1981;8(4):757–776. [PubMed] [Google Scholar]
- 27.Goldberg R A, Edelstein C, Balch K, Shorr N. Fat repositioning in lower eyelid blepharoplasty. Semin Ophthalmol. 1998;13(3):103–106. doi: 10.3109/08820539809066085. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg R A Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket Plast Reconstr Surg 20001052743–748., discussion 749–751 [DOI] [PubMed] [Google Scholar]
- 29.Mohadjer Y, Holds J B. Cosmetic lower eyelid blepharoplasty with fat repositioning via intra-SOOF dissection: surgical technique and initial outcomes. Ophthal Plast Reconstr Surg. 2006;22(6):409–413. doi: 10.1097/01.iop.0000243607.36661.be. [DOI] [PubMed] [Google Scholar]
- 30.Yoo D B, Peng G L, Massry G G. Transconjunctival lower blepharoplasty with fat repositioning: a retrospective comparison of transposing fat to the subperiosteal vs supraperiosteal planes. JAMA Facial Plast Surg. 2013;15(3):176–181. doi: 10.1001/jamafacial.2013.749. [DOI] [PubMed] [Google Scholar]
- 31.McCord C D Boswell C B Hester T R Lateral canthal anchoring Plast Reconstr Surg 20031121222–237., discussion 238–239 [DOI] [PubMed] [Google Scholar]
- 32.Jelks G W Glat P M Jelks E B Longaker M T The inferior retinacular lateral canthoplasty: a new technique Plast Reconstr Surg 199710051262–1270., discussion 1271–1275 [DOI] [PubMed] [Google Scholar]
- 33.Lelli G J Jr, Lisman R D. Blepharoplasty complications. Plast Reconstr Surg. 2010;125(3):1007–1017. doi: 10.1097/PRS.0b013e3181ce17e8. [DOI] [PubMed] [Google Scholar]
- 34.Patipa M The evaluation and management of lower eyelid retraction following cosmetic surgery Plast Reconstr Surg 20001062438–453., discussion 454–459 [DOI] [PubMed] [Google Scholar]
- 35.Carraway J H, Mellow C G. The prevention and treatment of lower lid ectropion following blepharoplasty. Plast Reconstr Surg. 1990;85(6):971–981. doi: 10.1097/00006534-199006000-00025. [DOI] [PubMed] [Google Scholar]
- 36.Fitzpatrick R E. Treatment of inflamed hypertrophic scars using intralesional 5-FU. Dermatol Surg. 1999;25(3):224–232. doi: 10.1046/j.1524-4725.1999.08165.x. [DOI] [PubMed] [Google Scholar]


