Abstract
Background and Purpose
Cervical artery dissection is a common cause of stroke in young people. The temporal profile of stroke risk after cervical artery dissection presenting without ischemia remains uncertain.
Methods
We performed a crossover-cohort study using administrative claims data on all emergency department visits and acute care hospitalizations from 2005–2011 in California, 2006–2013 in New York, and 2005–2013 in Florida. Using previously validated ICD-9-CM codes, we identified patients with a cervical artery dissection and no prior or concurrent stroke or TIA diagnosis. We compared the risk of stroke in successive 2-week periods during the 12 weeks after dissection versus the corresponding 2-week period 1 year later. Absolute risk increases were calculated using McNemar’s test for matched data. In a sensitivity analysis, we limited our population to patients presenting with typical symptoms of cervical artery dissection.
Results
We identified 2,791 patients with dissection without ischemia. The absolute increase in stroke risk was 1.25% (95% CI, 0.84–1.67%) in the first 2 weeks after dissection compared to the same time period 1 year later. The absolute risk increase was 0.18% (95% CI 0.02–0.34%) during weeks 3–4, and was no longer significant during the remainder of the 12 week post-dissection period. Our findings were similar in a sensitivity analysis identifying patients who presented with typical symptoms of acute dissection.
Conclusions
The risk of stroke following cervical artery dissection unaccompanied by ischemia at time of diagnosis appears to be limited to the first 2 weeks.
Keywords: Stroke, Internal Carotid Artery Dissection, Vertebral Artery Dissection, Healthcare Administrative Claims
Subject Terms: Cerebrovascular Disease/Stroke, Ischemic Stroke, Risk Factors
Cervical artery dissection is a common cause of stroke in the young.1–3 Dissections can result from trauma or occur spontaneously; however, so-called spontaneous dissections may be due to unnoticed minor trauma with or without predisposing factors such as connective tissue disease, hypertension, or smoking.4–8 Population-based studies have documented an annual incidence of cervical artery dissection of 2.6–3.0 per 100,000 persons, with over half presenting with stroke or transient ischemic attack (TIA).9,10 The true incidence may be very much higher, since on top of the at least 6–10% that are diagnosed as asymptomatic cases there may be many times that number of asymptomatic traumatic dissections that never present.10,11 Short- and long-term outcomes of cervical artery dissection are uncertain, with data mostly derived from older, single-center, small retrospective studies with limited follow-up. More recent larger, multicenter, prospective studies demonstrate disparate results. The overall frequency of stroke and frequency of stroke as a first symptom vary widely among studies.12–16 There is a paucity of data regarding the time period during which patients with cervical artery dissection face a heightened stroke risk, though it is commonly thought to be up to weeks to months. Furthermore, nearly all of the literature regarding incidence and timing of stroke following cervical artery dissection focuses on recurrent ischemic events as opposed to incident stroke following a known dissection.16–21 In this study, we used administrative claims data from a large, heterogeneous population to evaluate the time period during which patients with cervical artery dissection who present without TIA or stroke are at increased risk of incident stroke.
Methods
Study Design
We performed a crossover-cohort study using data on all emergency department (ED) visits and inpatient discharges in California, Florida, and New York. These data were collected by the California Office of Statewide Health Planning and Development, the New York Statewide Planning and Research Cooperative System, and the Florida Agency for Health Care Administration. These three agencies provide these data to the Agency for Healthcare Research and Quality for its Healthcare Cost and Utilization Project.22 Each patient is assigned a personal linkage number that allows them to be followed anonymously through all subsequent hospitalizations.23 Up to 25 discharge diagnoses are coded at each encounter using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) system. This study was approved by the institutional review board at Weill Cornell Medicine.
Study Subjects
We defined cervical artery dissection as the presence of carotid artery or vertebral artery dissection using ICD-9-CM codes 443.21 and 443.29 in any ED or hospital discharge diagnosis position. These ICD-9-CM codes have previously been validated with a positive predictive value of 82.1% for dissection.24 We identified adults aged 18 years or older with a diagnosis of cervical artery dissection from 2005–2011 in California, 2006–2013 in New York, and 2005–2013 in Florida. These states were chosen as they encompass a demographically heterogeneous population that represents nearly 20% of the United States population. The dates were chosen because they represent the most up-to-date data that include a linkage variable to allow longitudinal follow-up. In order to assess the time period during which patients with cervical artery dissection are at risk for an incident stroke, we excluded patients who had a stroke prior to or during the index encounter for cervical artery dissection. To ensure that we excluded any patient with a possible stroke prior to or at the same time as the dissection, we used a very inclusive definition of cerebrovascular disease (ICD-9-CM codes 430–438). Finally, we excluded non-residents of California, New York, and Florida in order to maximize the completeness of follow-up.
Measurements
All patients were followed for the primary outcome of ischemic stroke, defined as ICD-9-CM codes 433.x1, 434.x1, or 436 in any diagnosis code position in the absence of a primary discharge code for rehabilitation (V57) or any codes for subarachnoid hemorrhage (430), intracerebral hemorrhage (431), or brain trauma (800–804 and 850–854). This combination of diagnosis codes has been found to have a sensitivity of 86% and a specificity of 95% for ischemic stroke.25
Statistical Analysis
Patients with multiple visits for cervical artery dissection were entered into the analysis at their index visit for dissection. The risk of ischemic stroke was assessed during successive 2-week periods from the time of the index visit for cervical artery dissection until 12 weeks after the visit. The risk in each of these 2-week periods was compared with the corresponding 2-week period 1 year later. This design allowed patients to serve as their own controls, thus mitigating the effects of unmeasured confounders. Absolute risk increases were calculated using McNemar’s test for matched data via Stata’s mcc command.
We performed four sensitivity analyses. In the first sensitivity analysis, to help ensure that we evaluated the risk of stroke after acute dissection, we limited our population to only patients that presented with typical symptoms of cervical artery dissection such as headache, neck pain, cranial nerve palsies referable to the cavernous sinus or hypoglossal nerve, Horner syndrome, hoarseness, or symptoms referable to the posterior fossa, such as tinnitus or vertigo. In the second sensitivity analysis, we evaluated only those patients who underwent magnetic resonance imaging (MRI) at the initial encounter for dissection so as to ensure exclusion of patients who already had infarction at the time of dissection. Of note, information regarding the use of MRI was only available for patients from New York. In the third sensitivity analysis, we assessed the risk of ischemic stroke after cervical artery dissection using a more inclusive definition of stroke (ICD-9-CM codes 430–438 in any diagnosis code position). In the final sensitivity analysis, to assess the impact of mortality or out-of-state migration, we limited our cohort to patients who had at least one ED visit or hospitalization after the crossover period 1 year after the index visit for dissection.
To assess whether or not traumatic dissections might have a different risk and timing of stroke, we performed a subgroup analysis evaluating patients with concomitant trauma of the head or neck (ICD-9-CM codes 800–806, 839.1, 839.2, 847.0, 850–854.1, 900.x, 920, 952.2, 959.0).
All statistical analyses were performed using Stata/MP (version 13, College Station, TX). The threshold of statistical significance was set at α = 0.05.
Results
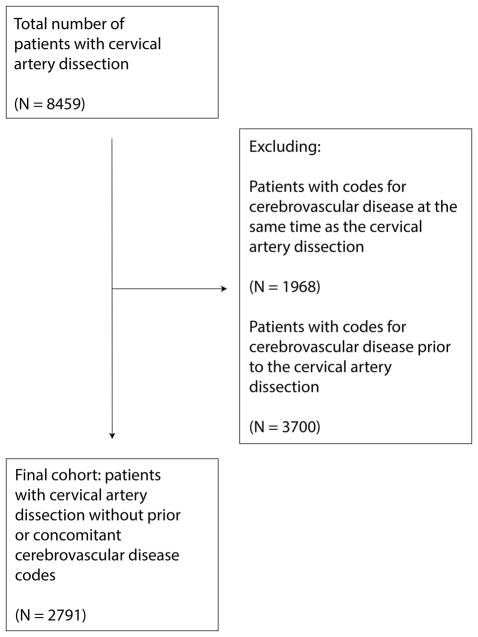
We identified 2,791 patients with an index visit for cervical artery dissection without concomitant stroke or TIA (Figure 1) in whom the mean age was 49.9 (±16.6) years and 46.5% were women (Table 1). In the 12 weeks after cervical artery dissection, 47 patients (1.68%) developed a stroke, as compared to zero strokes in the corresponding 12-week period 1 year later.
Figure 1.
Cohort Ascertainment
Legend: Flow-chart describing the ascertainment of patients with cervical artery dissection.
Table 1.
Characteristics of Patients with Dissection
| Characteristica | No Stroke (N = 2744) |
|---|---|
| Age, mean (SD), y | 49.9 (16.6) |
| Female | 1,297 (46.5) |
| Raceb | |
| White | 1,923 (70.1) |
| Black | 223 (8.1) |
| Hispanic | 327 (11.9) |
| Asian | 115 (4.2) |
| Other | 157 (5.7) |
| Payment source | |
| Medicare | 479 (17.2) |
| Medicaid | 293 (10.5) |
| Private | 1,685 (60.4) |
| Self-pay | 137 (4.9) |
| Other | 197 (7.1) |
| Income quartile | |
| 1 | 475 (17.3) |
| 2 | 614 (22.4) |
| 3 | 723 (26.4) |
| 4 | 927 (33.8) |
| Hypertension | 1,139 (40.8) |
| Diabetes | 309 (11.1) |
| Congestive heart failure | 92 (3.3) |
| Coronary heart disease | 263 (9.4) |
| Peripheral vascular disease | 66 (2.4) |
| Chronic obstructive pulmonary disease | 107 (3.8) |
| Chronic kidney disease | 70 (2.5) |
| Atrial fibrillation | 147 (5.3) |
| Tobacco use | 193 (6.9) |
| Alcohol use | 444 (15.9) |
Abbreviations: IQR, interquartile range; SD, standard deviation
Data are presented as number (%) unless otherwise specified.
Self-reported by patients or their surrogates. Numbers do not sum to group totals because of missing race/ethnicity data in 1.6% of patients.
There were significantly more strokes within the 0–2 week period after cervical artery dissection than during the same period 1 year later (47 vs. 0 events), corresponding to an absolute risk difference of 1.25% (95% Confidence Interval [CI], 0.84–1.67%). The absolute risk increase was 0.18% (95% CI, 0.02–0.34%) in the 3–4 week post-dissection period. Starting at 5 weeks after dissection, the risk of stroke was no longer significantly elevated (Table 2).
Table 2.
Risk of Stroke during Sequential 2-Week Intervals after Cervical Artery Dissectiona,b
| Time Interval after Dissection | Case Period (%) | Crossover Period (%) | Absolute Risk Difference (95% CI) |
|---|---|---|---|
| Weeks 0–2 | 1.25 | 0 | 1.25 (0.84–1.67) |
| Weeks 3–4 | 0.18 | 0 | 0.18 (0.02–0.34) |
| Weeks 5–6 | 0.11 | 0 | 0.11 (−0.01–0.23) |
| Weeks 7–8 | 0.04 | 0 | 0.04 (−0.03–0.11) |
| Weeks 9–10 | 0.04 | 0 | 0.04 (−0.03–0.11) |
| Weeks 11–12 | 0.07 | 0 | 0.07 (−0.03–0.17) |
Abbreviations: CI, confidence interval
Data for the case period are for the indicated interval after cervical artery dissection. Data for the crossover period are for the indicated interval plus 1 year after cervical artery dissection.
In a sensitivity analysis that identified 541 patients with dissections associated with symptoms, 1.84% (95% CI, 0.53–3.17%) developed a stroke, all of which occurred within the first four weeks after dissection. This temporal profile of stroke risk after dissection was unchanged in a sensitivity analysis using more inclusive diagnosis codes for stroke. Similarly, there was no significant change in our results when we included only patients with MRI performed at the index visit for dissection. Data regarding use of MRI was available for 461 patients, 277 of whom were confirmed to have undergone MRI. Five out of those 277 patients (1.08%; 95% CI, 0–2.25%) developed a stroke after dissection, and all occurred within the first 2-week period after diagnosis, as compared to no events in the same 2-week period 1 year later.
We identified 840 patients with traumatic cervical artery dissections, 12 of whom developed subsequent stroke. The stroke risk in patients with traumatic cervical artery dissections was not significantly different to those without evidence of a traumatic dissection (1.43%; 95% CI, 0.51–2.35% vs. 1.79%; 95% CI, 1.15%–2.43%, p = .49). The temporal profile of the stroke risk was similar between the groups.
Lastly, our findings were unchanged in a sensitivity analysis limited to patients who had at least one visit after the crossover period, thereby assuring that they remained alive and resident in the same U.S. state throughout follow-up.
Discussion
In a large, heterogeneous patient population presenting with cervical artery dissection in the absence of TIA or stroke, we found that approximately 1.7% developed a stroke in the first 12 weeks following the diagnosis of dissection, and that almost all of the strokes occurred in the first 2 weeks. Our findings were essentially unchanged in several sensitivity analyses.
Our results are in line with the CADISS trial, a large, multicenter study that randomized patients presenting with cervical artery dissection to either anticoagulation or antiplatelet agents, and found an overall stroke recurrence rate of 2% at 3 months, with all recurrences occurring within the first 10 days.19 Unlike our study, the majority of patients (195/225) in the CADISS trial presented with stroke. All strokes following randomization in the CADISS trial occurred in patients who initially presented with stroke. The CADISP Study, a large observational study of consecutive admissions with cervical artery dissection in which most (64%) presented with stroke, found a similar rate of new stroke at 3 months (2.7%).18 Among the 198 patients in CADISP who did not initially present with stroke, 3 (1.5%) developed an incident event within 3 months. The number of events was too small to precisely establish the temporal profile of stroke risk. Our findings build on these prior studies by establishing that the risk of incident stroke after presentation with cervical artery dissection is essentially limited to the first 2 weeks after diagnosis. This is useful because headache and neck pain are the most frequent initial symptoms of cervical artery dissection cases15–16,26 while cerebral or retinal infarction is the inaugural event in only 11–33% of cases.10–11 Our findings may aid in counseling patients regarding their risk of stroke.
Trauma, as a distinct cause of cervical artery dissection that can cause ischemia, is worth considering separately. Prior studies found that up to 60% of patients who suffer blunt cerebrovascular injury and present without stroke will develop stroke if left untreated, although since none of these studies evaluated all trauma cases with angiography regardless of suspicion for vessel injury, the true rate could be significantly lower.27–29 Many of these patients have suffered significant neurological injury at the time of injury. In a single-center retrospective review, the stroke rate after blunt cerebrovascular injury was reduced to 4% with early treatment.29 Little data exist to inform stroke risk after discharge following traumatic dissection without concomitant neurological injury. One series of 16 patients with traumatic dissection found that the mean time between trauma and stroke was 4.8 days with a range from 0 to 31 days.16 In our study of over 800 patients with traumatic cervical artery dissection presenting without stroke, the risk of stroke was 1.43%, not significantly different from that of non-traumatic dissections.
The results of our study must be considered in light of its limitations. First, we did not have access to information describing patients’ symptomatology, imaging characteristics, or treatment. As such, even with well-validated diagnostic codes, some patients may have escaped diagnosis and inclusion in our study as radiographic data could not be reviewed. Moreover, we cannot aid in settling the controversy regarding treatment with antiplatelet agents versus anticoagulation, and can only assume that patients were treated with one or the other in line with current guidelines.30 Second, we likely missed cases of asymptomatic or minimally symptomatic cervical artery dissection that did not come to medical attention. However, this would be a conservative bias since these milder cases would be expected to face an even lower and briefer risk of stroke. Third, some patients may have presented in a delayed fashion following the onset of symptoms, obscuring the true timing of stroke risk following acute dissection. Our sensitivity analysis including only patients presenting with acute symptoms of dissection may mitigate this limitation as these patients are less likely to delay presentation. Fourth, our use of administrative claims may have led to misclassification of stroke events. However, the diagnosis code algorithms we used have good sensitivity and specificity. More importantly, misclassification would not be expected to vary over 2-week time blocks and thus should not have significantly affected our main finding regarding the temporal pattern of stroke risk. Fifth, some patients may have migrated out of state after the 3-month post-dissection period. This would have lowered our risk estimates since, in these patients, strokes during the crossover period would not have been captured. However, our findings were unchanged in a sensitivity analysis limited to patients who had at least one visit in the same state after the crossover period, thus ensuring that they were subject to full follow-up throughout the study period. Sixth, while it may be informative to evaluate the more chronic risk of incident stroke after dissection, the crossover design of the study does not lend itself to such an analysis. Future studies will need to evaluate long-term risk. Finally, stroke risk immediately after dissection was compared with the risk 1 year later, and it could be argued that this comparison period is an artificially high-risk period because patients may have continued to be at a higher risk of stroke given a persistent dissection. However, this is not the case in our data since we found no stroke diagnoses during the 1-year control period after dissection.
Conclusions
Among patients presenting with acute cervical artery dissection and no evidence of stroke, we found that the risk of incident stroke was clustered mainly within the first 2 weeks. Further research is necessary to delineate the optimal type and duration of antithrombotic therapy for stroke prevention in these patients.
Supplementary Material
Acknowledgments
The authors are grateful to Monica Chen for copyediting and clerical assistance.
Sources of Funding: This study was supported by grant K23NS082367 (Dr. Kamel) from the National Institute of Neurological Disorders and Stroke, a grant from the Michael Goldberg Stroke Research Fund (Dr. Kamel), and funding from the Feil Family Foundation (Dr. Gialdini).
Footnotes
Disclosures: None.
References
- 1.Caplan LR, Zarins CK, Hemmati M. Spontaneous dissection of the extracranial vertebral arteries. Stroke. 1985;16:1030–1038. doi: 10.1161/01.str.16.6.1030. [DOI] [PubMed] [Google Scholar]
- 2.Putaala J, Metso AJ, Metso TM, Konkola N, Kraemer Y, Haapaniemi E, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki young stroke registry. Stroke. 2009;40:1195–1203. doi: 10.1161/STROKEAHA.108.529883. [DOI] [PubMed] [Google Scholar]
- 3.Yesilot Barlas N, Putaala J, Waje-Andreassen U, Vassilopoulou S, Nardi K, Odier C, et al. Etiology of first-ever ischaemic stroke in European young adults: the 15 cities young stroke study. Eur J Neurol. 2013;20:1431–1439. doi: 10.1111/ene.12228. [DOI] [PubMed] [Google Scholar]
- 4.Schievink WI. Spontaneous Dissection of the Carotid and Vertebral Arteries. NEJM. 2001;344:898–906. doi: 10.1056/NEJM200103223441206. [DOI] [PubMed] [Google Scholar]
- 5.Schievink WI, Michels VV, Piepgras DG. Neurovascular manifestations of heritable connective tissue disorders: a review. Stroke. 1994;25:889–903. doi: 10.1161/01.str.25.4.889. [DOI] [PubMed] [Google Scholar]
- 6.Nedeltchev K, Baumgartner RW. Traumatic cervical artery dissection. Front Neurol Neurosci. 2005;20:54–63. doi: 10.1159/000088149. [DOI] [PubMed] [Google Scholar]
- 7.Esnault P, Cardinale M, Boret H, D’Aranda E, Montcriol A, Bordes J, et al. Blunt cerebrovascular injuries in severe traumatic brain injury: incidence, risk factors, and evolution.[published online ahead of print July 29, 2016] [Accessed November 4, 2016];J Neurosurg. 2016 doi: 10.3171/2016.4.JNS152600. http://thejns.org/doi/pdf/10.3171/2016.4.JNS152600. [DOI] [PubMed]
- 8.Davis JW, Holbrook TL, Hoyt DB, Mackersie RC, Field TO, Jr, Shackford SR. Blunt carotid artery dissection: incidence, associated injuries, screening, and treatment. J Trauma. 1990;30:1514–1517. [PubMed] [Google Scholar]
- 9.Giroud M, Fayolle H, André N, Dumas R, Becker F, Martin D, et al. Incidence of internal carotid artery dissection in the community of Dijon. J Neurol Neurosurg Psychiatry. 1994;57:1443. doi: 10.1136/jnnp.57.11.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee VH, Brown RD, Jr, Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809–1812. doi: 10.1212/01.wnl.0000244486.30455.71. [DOI] [PubMed] [Google Scholar]
- 11.Schievink WI, Mokri B, Whisnant JP. Internal carotid artery dissection in a community. Rochester, Minnesota, 1987–1992. Stroke. 1993;24:1678–1680. doi: 10.1161/01.str.24.11.1678. [DOI] [PubMed] [Google Scholar]
- 12.Ehrenfeld WK, Wylie EJ. Spontaneous dissection of the internal carotid artery. Arch Surg. 1976;111:1294–1301. doi: 10.1001/archsurg.1976.01360290128019. [DOI] [PubMed] [Google Scholar]
- 13.Fisher CM. The headache and pain of spontaneous carotid dissection. Headache. 1982;22:60–65. doi: 10.1111/j.1526-4610.1982.hed2202060.x. [DOI] [PubMed] [Google Scholar]
- 14.Biller J, Hingtgen WL, Adams HP, Smoker WRK, Godersky JC, Toffol GJ. Cervicocephalic arterial dissections: a ten year experience. Arch Neurol. 1986;43:1234–1238. doi: 10.1001/archneur.1986.00520120019010. [DOI] [PubMed] [Google Scholar]
- 15.Mokri B, Sundt TM, Jr, Houser OW, Piepgras DG. Spontaneous dissection of the cervical internal carotid artery. Ann Neurol. 1986;19:126–138. doi: 10.1002/ana.410190204. [DOI] [PubMed] [Google Scholar]
- 16.Biousse V, D’Anglejan-Chatillon J, Toouboul PJ, Amarenco P, Bousser MG. Time course of symptoms in extracranial carotid artery dissections: a series of 80 patients. Stroke. 1995;26:235–239. doi: 10.1161/01.str.26.2.235. [DOI] [PubMed] [Google Scholar]
- 17.Touzé E, Gauvrit JY, Moulin T, Meder JF, Bracard S, Mas JL, et al. Risk of stroke and recurrent dissection after a cervical artery dissection: a multicenter study. Neurology. 2003;61:1347–1351. doi: 10.1212/01.wnl.0000094325.95097.86. [DOI] [PubMed] [Google Scholar]
- 18.Debette S, Grond-Ginsbach C, Bodenant M, Kloss M, Engelter S, Metso T, et al. Differential features of carotid and vertebral artery dissections: the CADISP study. Neurology. 2011;77:1174–81. doi: 10.1212/WNL.0b013e31822f03fc. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy F, Lanfranconi S, Hicks C, Reid J, Gompertz P, Price C, et al. Antiplatelets vs anticoagulation for dissection: CADISS nonrandomized arm and meta-analysis. Neurology. 2012;79:686–689. doi: 10.1212/WNL.0b013e318264e36b. [DOI] [PubMed] [Google Scholar]
- 20.Weimar C, Kraywinkel K, Hagemeister C, Haab A, Katsarava Z, Brunner F, et al. Recurrent stroke after cervical artery dissection. J Neurol Neurosurg Psychiatry. 2010;81:869–873. doi: 10.1136/jnnp.2009.192153. [DOI] [PubMed] [Google Scholar]
- 21.Beletsky V, Nadareishvili Z, Lynch J, Shuaib A, Woolfenden A, Norri JW, et al. Cervical arterial dissection: time for a therapeutic trial? Stroke. 2003;34:2856–2860. doi: 10.1161/01.STR.0000098649.39767.BC. [DOI] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality. [Accessed April 3, 2016];Healthcare Cost and Utilization Project. http://hcupnet.ahrq.gov.
- 23.Agency for Healthcare Research and Quality. [Accessed April 3, 2016];HCUP methods series: methodological issues when studying readmissions and revisits using hospital administrative data. http://www.hcup-us.ahrq.gov/reports/methods/2011_01.pdf.
- 24.Qureshi AI, Shaudhry SA, Hassan AE, Zacharatos H, Rodriguez GJ, Suri FK. Thrombolytic treatment of patients with acute ischemic stroke related to underlying arterial dissection in the United States. Arch Neurol. 2011;68:1536–1542. doi: 10.1001/archneurol.2011.213. [DOI] [PubMed] [Google Scholar]
- 25.Tirschwell DL, Longstreth WT. Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 26.Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and cervical artery dissections. Neurology. 1995;45:1517–1522. doi: 10.1212/wnl.45.8.1517. [DOI] [PubMed] [Google Scholar]
- 27.DiCocco JM, Emmett KP, Fabian TC, Zarzaur BL, Williams JS, Croce MA. Blunt cerebrovascular injury screening with 32-channel multidetector computed tomography: more slices still don’t cut it. Ann Surg. 2011;253:444–450. doi: 10.1097/SLA.0b013e31820d946b. [DOI] [PubMed] [Google Scholar]
- 28.Berne JD, Cook A, Rowe SA, Norwood SH. A multivariate logistic regression analysis of risk factors for blunt cerebrovascular injury. J Vasc Surg. 2010;51:57–64. doi: 10.1016/j.jvs.2009.08.071. [DOI] [PubMed] [Google Scholar]
- 29.Callcut RA, Hanseman DJ, Solan PD, Kadon KS, Ingalls NK, Fortuna GR, et al. Early treatment of cerebrovascular injury with concomitant hemorrhagic neurologic injury is safe and effective. J Trauma Acute Care Surg. 2012;72:338–45. doi: 10.1097/TA.0b013e318243d978. [DOI] [PubMed] [Google Scholar]
- 30.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke. 2014;45:2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.