A 51-year-old African American woman presented with 6 months of progressively worsening left frontal headaches, 1 week of blurred vision in her left eye, and 1 day of nausea and vomiting. She denied other neurologic or respiratory symptoms.
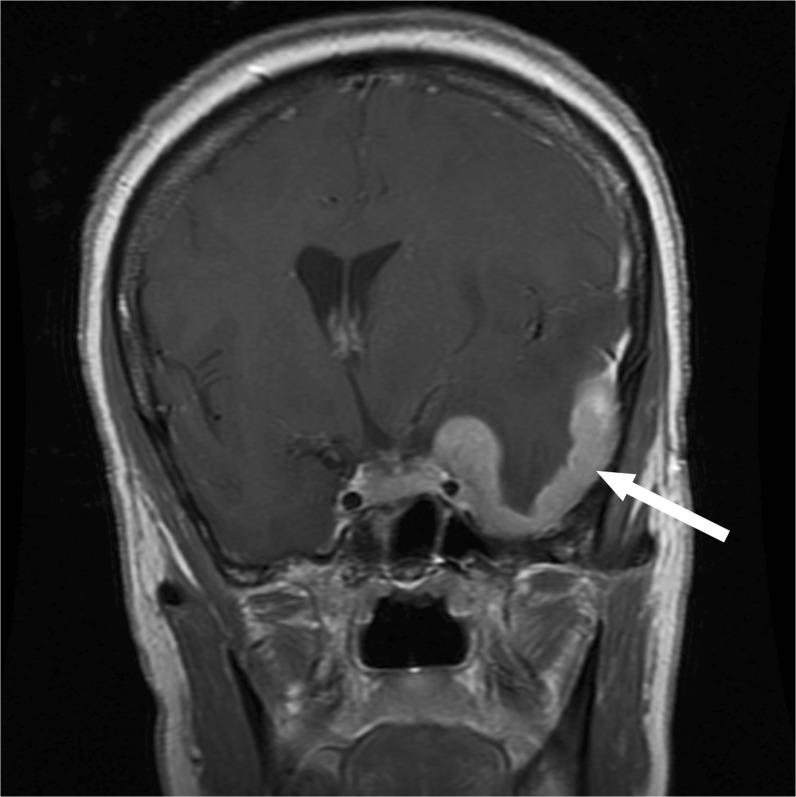
Examination revealed decreased visual acuity and a mild afferent pupillary defect in the left eye. MRI of the brain revealed a dural-based mass centered on the left sphenoid wing with significant vasogenic edema and midline shift (Fig. 1). Computed tomography of the chest demonstrated multiple opacities in the upper and mid-lung fields and bilateral mediastinal and hilar lymphadenopathy. Further workup was negative, and biopsy of the brain lesion revealed non-caseating granulomatous inflammation consistent with sarcoidosis.
Figure 1.
Coronal T1-weighted MRI scan of the brain with gadolinium enhancement, initial presentation. Arrow indicates dural-based mass over the left sphenoid wing.
Neurologic complications occur in only 5–10 % of sarcoidosis cases, and may not be associated with other systemic manifestations.1 The most common presenting symptom is cranial neuropathy, most frequently of the facial or optic nerve.1 Leptomeningeal disease accounts for 10–20 % of neurosarcoidosis, and can manifest as aseptic meningitis or a dural mass lesion, as in this patient.2
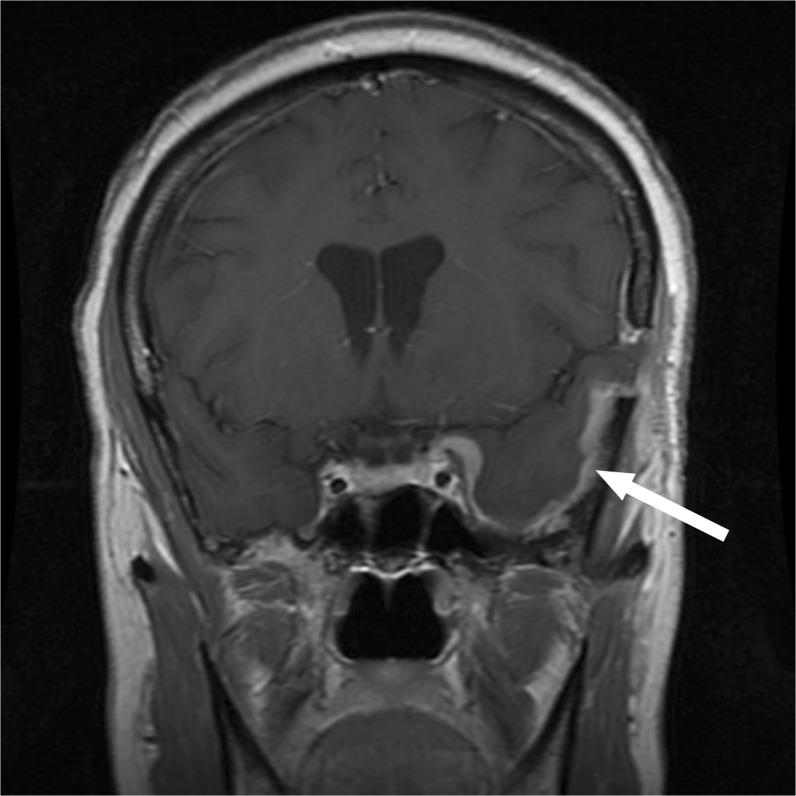
Our patient improved rapidly with corticosteroids (Fig. 2), which is the first-line therapy for neurosarcoidosis. Combination therapy with TNF-alpha antagonists and steroid-sparing agents may be considered in refractory or severely disabling cases.1 , 2
Figure 2.
Coronal T1-weighted MRI scan of the brain with gadolinium enhancement, status post 4 weeks of high-dose corticosteroid therapy. Significant decrease in size of the dural-based mass (arrow) and resolution of midline shift are noted.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Contributor Information
Jennifer Y. Wang, Email: jennifer.wang@hhs.sccgov.org.
David F. Jacobson, Phone: (408) 885-6305, Email: david.jacobson@hhs.sccgov.org.
References
- 1.Tavee JO, Stern BJ. Neurosarcoidosis. Clin Chest Med. 2015;36(4):643–656. doi: 10.1016/j.ccm.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Krumholz A, Stern BJ. Neurologic manifestations of sarcoidosis. Handb Clin Neurol. 2014;119:305–333. doi: 10.1016/B978-0-7020-4086-3.00021-7. [DOI] [PubMed] [Google Scholar]