Abstract
Background
As the US transitions to value-based healthcare, physicians and payers are incentivized to change healthcare delivery to improve quality of care while controlling costs. By assisting with the management of common chronic conditions, community health workers (CHWs) may improve healthcare quality, but physicians and payers who are making choices about care delivery also need to understand their effects on healthcare spending.
Methods
We searched PubMed, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, PsycINFO, Embase, and Web of Science from the inception of each database to 22 June 2015. We included US-based studies that evaluated a CHW intervention for patients with at least one chronic health condition and reported cost or healthcare utilization outcomes. We evaluated studies using tools specific to study design.
Results
Our search yielded 2,941 studies after removing duplicates. Thirty-four met inclusion and methodological criteria. Sixteen studies (47%) were randomized controlled trials (RCTs). RCTs typically had less positive outcomes than other study designs. Of the 16 RCTs, 12 reported utilization outcomes, of which 5 showed a significant reduction in one or more of ED visits, hospitalizations and/or urgent care visits. Significant reductions reported in ED visits ranged from 23%–51% and in hospitalizations ranged from 21%–50%, and the one significant reduction in urgent care visits was recorded at 60% (p < 0.05 for all).
Discussion
Our results suggest that CHW interventions have variable effects, but some may reduce costs and preventable utilization. These findings suggest that it is possible to achieve reductions in care utilization and cost savings by integrating CHWs into chronic care management. However, variations in cost and utilization outcomes suggest that CHWs alone do not make an intervention successful. The paucity of rigorous studies and heterogeneity of study designs limited conclusions about factors associated with reduced utilization.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-016-3922-9) contains supplementary material, which is available to authorized users.
KEY WORDS: community health workers, systematic review, healthcare costs, healthcare utilization, chronic disease management, community health
INTRODUCTION
Global and capitated payment models are changing healthcare delivery. These payment models set up incentives for practices to reduce use of costly services, while maintaining or improving health outcomes. Relative to a fee-for-service model, global payments give hospitals and primary care practices more flexibility to fund new ways of delivering care. Consequently, physicians and practice managers need to understand the evidence base on the value of care models.
Community health workers (CHWs), who have minimal formal training in healthcare and are hired primarily for their connection to a community,1 have long been employed by primary care practices. Typically grant funded and not reimbursed through fee for service, they focus on health education, prevention, or chronic disease management for vulnerable and minority populations.1 – 3 As value-based payment models expand, providers will have more flexibility to fund CHWs with global budgets, or payers may elect to reimburse for CHW services.4 – 6
The emerging evidence base on CHW programs7 for the prevention and management of chronic diseases includes systematic reviews concluding that CHW interventions can improve overall health outcomes8 and outcomes for patients with heart disease, stroke,9 type II diabetes,10 – 12 HIV,13 and asthma2 , 14 and for vulnerable patients with or at risk for a variety of chronic diseases or cancer.15 Other systematic reviews have also documented the costs and cost-effectiveness of CHW programs,15 but none, outside of low and middle-income countries,16 have examined the impact of CHWs on the utilization of health services by patients with chronic conditions. Because of their focus on prevention and disease management, CHWs have the potential to reduce use of certain preventable, costly healthcare services, such as emergency department (ED) or urgent care visits. In deciding whether to incorporate CHWs into a primary care practice, physicians and payers would benefit from an understanding of how CHWs impact spending and the populations in which CHWs may bring about the greatest savings.
In this context, we conducted a systematic review of studies that have a cost or healthcare utilization outcome, evaluate CHW interventions for chronic disease management, and are relevant to primary care. We can understand the effects of CHWs either directly, by measuring costs, or indirectly, by measuring how CHWs change potentially preventable utilization, an outcome that affects payers and practices using global or bundled payment models, but also affects healthcare efficiency and quality. Ours is the first systematic review to focus solely on the financial impacts of CHWs for chronic care management in the US. We limited our search to chronic care management because it is an area in which CHWs have potential to reduce spending, as patients with chronic conditions are among the most expensive and have the most preventable healthcare use.17 , 18 These findings may inform physicians and payers and will help prioritize gaps for future research to address.
METHODS
This systematic review was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.19 Protocol information can be accessed on the PROSPERO International register of systematic reviews online.
Search Strategy
We searched PubMed (1809–22 June 2015), Cochrane Database of Systematic Reviews (2000–22 June 2015), Cochrane Central Register of Controlled Trials (1992–22 June 2015), PsycINFO (1872–22 June 2015), Embase (1947–22 June 2015), and Web of Science (1900–22 June 2015). Our search strategy identified articles containing one or more terms related to the following three ideas: (1) CHWs, (2) cost or healthcare utilization related to chronic care management, and (3) a United States setting (see Appendix 1, available online, for complete search strategy). We searched both free text and controlled vocabulary words and translated search terms into syntax appropriate for each database.
In order to capture the breadth of CHW job titles, we drew search terms from: (1) previous systematic reviews on CHWs,8 , 20 – 22 (2) specific job titles used for CHWs in Massachusetts, based on a survey of CHW programs conducted by the Massachusetts Department of Public Health,23 , 24 and (3) additional terms on health coaching and doulas, some of which were added after consulting with staff at the Massachusetts Department of Public Health’s Office of CHWs. Massachusetts is one of two states25 with an office of CHWs and has a range of CHW programs, making the list of job titles broad.
Eligibility Criteria
We included peer-reviewed, primary research studies published in English that met the PICOS criteria displayed in Table 1.
Table 1.
Eligibility Criteria
| Studies were included if they met the following PICOS criteria: | |
|---|---|
| Patients | • Have at least one chronic disease • Adults or children |
| Intervention | • CHWs must play a primary role in the intervention, with CHW defined as individuals who work primarily in a health-related role, have no professional or paraprofessional training in healthcare or social work, and were selected for their role largely because of their familiarity with a community or population (consistent with the Massachusetts Department of Public Health and American Public Health Association definitions of CHWs)1
,
23
• Other health professionals or community workers may participate in the intervention, as long as CHWs play the main role • CHWs are paid for their work • CHWs manage a condition that is relevant to primary care and not typically handled by specialists (such as cancer treatment navigation) • The intervention does not primarily address a public health concern, such as vaccination for an entire community • The intervention does not primarily address maternal and infant health or screening, as these are not relevant to chronic disease management |
| Comparison | • Cohort, pre-post, or randomized controlled trial design |
| Outcome | • Report on healthcare costs or utilization, including ED visits, urgent care visits, primary care visits, or medication use* • Quantitative outcome |
| Setting | • United States • Not at a worksite |
*We included adherence to medication as an outcome because medications contribute to healthcare costs, both in the short term (potential increase) and long term (potential decrease). For example, asthma, a condition that CHWs commonly treat, have medications that are used only or more often if the disease is poorly controlled (rescue inhalers), making medication a form of preventable utilization
Study Selection
Two researchers (SA, HJ) independently screened the titles, abstracts, and full texts of all studies, reconciling any differences through discussion and excluding studies that did not meet eligibility criteria. A third reviewer (ES) acted as a tiebreaker for any inclusion/exclusion disagreements. Following the full text screen, we screened the bibliographies of the included studies and articles that cited the studies. Any relevant titles were screened by abstract then by full text, as in the original screening process. Selected studies were incorporated into the final list of included studies. A primary care provider (RP) reviewed the list of included studies and excluded any studies not relevant to a primary care setting.
Studies were also assessed for methodological rigor. A team of two researchers (SA, LS) reviewed and evaluated studies by design type using the following scales: Jadad Scale for RCTs,26 Quality Assessment Tool for Quantitative Studies for pre-post (single arm) studies,27 Newcastle-Ottawa Scale for non-randomized matched cohort design,28 and Consensus on Health Economic Criteria for the cost-effectiveness studies.29 (Details on study exclusion at this step are presented in Appendix 2, available online.) Studies were not compared across scales, as there was no way to standardize ratings. Instead, we provide each study’s design (Table 2), outcomes (Table 3), and risk of bias (Appendix 2) to facilitate interpretation of results.
Table 2.
Description of Included Studies
| Intervention | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Citation | Study design | Number and description of participants | Funding source* | Pediatric/adult | Chronic disease | Healthcare use for inclusion (yes/no) | Insurance status/income status for inclusion (yes/no) | Location (urban or rural; state) | Duration | Setting | Intens-ity† | CHW part of care team? (if yes, description) | Brief description of CHW role‡ |
| Babamoto et al. 200933 | RCT | 318 Hispanic/Latino |
Private foundation; for-profit company | Adult | Type II diabetes | No | None | Urban; CA | 6 months | Community, home, clinic, telephone | NS, NS, 6, 3 | No | Health coaching, health education§ |
| Bryant-Stephens and Li 200835 | RCT | 281 99% African American |
Not stated | Pediatric | Asthma | Yes (≥1 hospitalization for asthma or ≥2 asthma-related emergency visits 1 year before enrollment) | None | Urban; PA | 1 year | Home | 5, NS, 12,1 | No | Home visiting, environmental modification, health education |
| Fisher et al. 200936 | RCT | 191 Predominantly African American area |
State or federal; private foundation; other non-profit organization | Pediatric, adult | Asthma | Yes (hospitalized for asthma) | Yes (Medicaid) | Urban; MS | April 1997–Feb. 1999 | Hospital, home | NS, NS, 24, 1 | No | Home visiting, health coaching, health education |
| Gary et al. 200937 | RCT | 542 African American |
State or federal | Adult | Type II diabetes | No | None | Urban; MD | 24 months | None stated | NS, NS, 24, 1 | Yes (CHW works with nurse case manager to deliver intervention) | Health education, health coaching, home visiting, advocacy, care coordination |
| Hopper et al. 198438 | RCT | 227 77% Black |
State or federal | Adult | Type II diabetes | Yes (regular clinic attendance in 1978) | None | Urban; MS | 18 months | Hospital | NS, NS, 18, 1 | No | Health coaching, health education, home visiting |
| Hunter et al. 200461 | RCT | 101 96% Hispanic |
Not stated | Adult | None | Yes (participated in an initial clinical screening exam) | None | Rural; AZ | 1 year | Home | NS, NS, NS, 1 | No | Home visiting, connecting with health services, health education§ |
| Kangovi et al. 201451 | RCT | 446 93% Black |
Academic institution; healthcare provider | Adult | None | Yes (admitted to a medicine service and expected to be discharged home, as opposed to an acute care facility) | Uninsured or Medicaid and resident of a specified zip code (>30% of residents live below the federal poverty line) | Urban; PA | April 2011–Dec. 2012 | Hospital | NS, NS, 0.5, 1 | No | Health coaching, advocacy, home visiting, connecting with health services, care coordination |
| Krieger et al. 199960 | RCT | 421 79.1% Black |
State or federal | Adult | Elevated blood pressure | No | Yes (<200% of the 1995 federal poverty level) | Urban; WA | 3 months | Home, community sites and centers | NS, NS, NS, 1 | No | Connecting with health services, connecting with social services |
| Krieger et al. 200555 | RCT | 274 12.3% Non-Hispanic White, 31.9% Non-Hispanic African American, 25.4% Vietnamese, 9.4% other Asian, 17.4% Hispanic, 2.6% other |
State or federal; private foundation | Pediatric | Asthma | Yes (prior provider asthma diagnosis per outpatient record or 1 ED discharge with asthma as primary diagnosis) | Yes (<200% of the 1996 federal poverty level) | Urban; WA | 1 year | Home | 5–9, NS, 12, 1 | No | Home visiting, health coaching, health education, environmental modification, connecting to social services§ |
| Krieger et al. 201554 | RCT | 366 46.7% Hispanic |
State or federal | Adult | Asthma | Yes (previous clinical diagnosis) | Yes (<250% of the 2007 federal poverty level) | Urban; WA | 1 year | Home | 5, NS, 7, 1 | No | Health education, home visiting, health coaching, advocacy, connecting with social services, environmental modification, care coordination§ |
| Kronish et al. 201457 | RCT | 600 40% Black, 42% Latino, 13% White, 4% other |
State or federal | Adult | Stroke/“mini-stroke” | Yes (prior treatment for stroke) | None | Urban; NY | 6 months | Community center | 6, 90, 6, 3 | No | Health education, health coaching |
| Martin et al. 201459 | RCT | 101 Hispanic predominantly Puerto Rican |
State or federal | Pediatric | Asthma | Yes (prescribed ICS in past year) | None | Urban; IL | 4 months | Home | 4, NS, 12, 1 | No | Home visiting, health education, health coaching |
| Nelson et al. 201139 | RCT | 247 94% African American, 4.2% White, 1.6% other |
State or federal | Pediatric | Asthma | Yes (ED visit for acute asthma care in preceding 15 months OR primary care diagnosis) | Yes (Medicaid) | Urban; MS | 18 months | Hospital | ≥18, NS, 18, 1 | No | Health coaching, home visiting |
| Parker et al. 200853 | RCT | 328 83% African American, 11% Hispanic, 4% Caucasian, 3% other |
State or federal | Pediatric | Asthma | Yes (doctor prescribed medicine for respiratory symptoms) | None | Urban; MI | 1 year | Home | 9, NS, 12, 1 | No | Connecting with social services, home visiting, connecting with health services, health coaching, environmental modification, health education§ |
| Rothschild et al. 201456 | RCT | 144 Mexican Americans |
State or federal | Adult | Type II diabetes | No | Yes (health insurance or receive care through free clinic) | Urban; IL | 2 years | Home, hospital | 36, 99 avg, 24, 1 | No | Home visiting, health education§ |
| Wang et al. 201234 | RCT | 200 Post incarceration (5.2% Asian, 63.4% Black, 10.4% Hispanic, 20.8% White) |
Private foundation; local government | Adult | At least one chronic illness | No | None | Urban; CA | 1 year | Primary care center | NS, NS, NS, 1 | Yes (CHWs works closely with primary care provider) | Connecting with social services, connecting with health services, home visiting, health education |
| Adair et al. 201247 | Pre-post | 332 43% Black, 49% White, 8% other |
Private foundation | Adult | Hypertension, diabetes, or heart failure | No | None | Urban; MN | 1 year | Primary care center | NS, NS, NS, 1 | No | Health education, care coordination, health coaching, advocacy |
| Ferrer et al. 201348 | Pre-post | 1,500 Hispanic |
Academic institution | Adult | High-risk patients | No | None | Rural; TX | 1 year | Primary care center, community | NS, NS, NS, 3 | Yes (CHWs participate in group visits with team) | Home visiting, care coordination, advocacy, health coaching, health education§ |
| Fox et al. 200745 | Pre-post | 541 14.3% Black, 81.7% Hispanic, 2.2% White |
Private foundation | Pediatric | Asthma | No | Yes (low income) | Urban; CA | 2001–2004 | Primary care center, home | NS, NS, 24, 1 | Yes (CHWs help connect providers to coordinate care and participate in team quality improvement) | Care coordination, health education, connecting with social services, home visiting |
| Margellos-Anast et al. 201241 | Pre-post | 70 Non-Hispanic Black |
State or federal | Pediatric | Asthma | Yes (ED visit or hospitalization in past year) | Yes (low income) | Urban; IL | 6 months | Home | 3–4, NS, 6, 1 | No | Home visiting, health education, connecting with health services, care coordination |
| Michelen et al. 200642 | Pre-post | 711 92% Hispanic, <6% African American, other |
Not stated | Pediatric | None | Yes (3 or more ED utilizations in past 6 months) | None | Urban; NY | 6 months | Home | NS, NS, NS, 1 | No | Care coordination, health education§ |
| Postma et al. 201143 | Pre-post | 866 91% Hispanic, 9% Non-Hispanic |
State or federal; academic institution | Pediatric | Asthma | No | None | Rural; WA | 8 months | Home | 8, NS, 8, 1 | No | Home visiting, health education, health coaching, environmental modification, connecting with social services, connecting with health services |
| Primomo et al. 200646 | Pre-post | 105 68% Caucasian, 19% African American, 5% Samoan, 3% Hispanic, 3% Native American, 3% Chinese, 2% other |
State or federal; academic institution | Pediatric | Asthma | No | None | WA | 2-26 weeks | Home | 2.24 avg, NS, 5 weeks avg, 1 | No | Home visiting, health coaching, health education, environmental modification, advocacy |
| Turyk et al. 201344 | Pre-post | 300 African American |
Private foundation | Pediatric | Asthma | No | Yes (low income) | Urban; IL | 1 year | Home | 6, NS, 12, 1 | No | Home visiting, health education, health coaching, care coordination, environmental modification, connecting with social services, connecting with health services |
| Bryant-Stephens et al. 200949 | Cohort | 264 98% Non-Hispanic Black |
State or federal | Pediatric | Asthma | Yes (≥1 hospitalization due to asthma or ≥2 asthma-related emergency visits 1 year before the time of enrollment) | None | Urban; PA | 1 year | Home | 5, NS, 6, 1 | No | Home visiting, health education, environmental modification |
| Enard and Ganelin 201350 | Cohort | 13,642 15.7% White, 58% Black, 23.1% Hispanic, 2.2% other |
Private foundation; state or federal | Pediatric, adult | None | Yes (at least one “primary-care related” ED use) | None | Urban; TX | 12 months | Hospital, telephone | NS, NS, 24, 1 | No | Health education, connecting with health services, advocacy§ |
| Felix et al. 201152 | Cohort | 2,122 76.9% Black |
Private foundation; state or federal | Adult | Long-term care needs | No | None | Rural; AR | 3 years | Home, community | NS, NS, NS, 1 | No | Connecting patients to social services, advocacy, health education |
| Freeborn et al. 197862 | Cohort | 6,159 No stated description |
State or federal | Pediatric, adult | None | No | Yes: Kaiser Permanente and low income | Urban; OR | Not stated | Primary care center | NS, NS, 12, 1 | Yes (CHWs work with patients during clinic visits) | Health education, connecting with social services |
| Johnson et al. 20125 | Cohort | 448 No stated description |
Private foundation | Adult | None | Yes (3 or more ED visits in one quarter) | Yes (Molina Healthcare of New Mexico) | Urban and rural; NM | 25 months | Not stated | NS, NS, 25, NS | Yes (CHW member of care team and coordinate between providers) | Home visiting, health coaching, health education, advocacy, connecting with health services, connecting with social services |
| Roth et al. 201258 | Cohort | 449 28.9% Black, 65.7% White, 5.4% Other |
State or federal | Adult | HIV-positive | No | Yes (Health Insurance Assistance Program) | Urban; IN | 1 year | Not stated | NS, NS, 12, 1 | No | Health education |
| Brown et al. 201263 | Cost-effect | 46 Hispanic |
State or federal | Adult | Type II diabetes | No | None | Urban; TX | 18 months | Primary care center, home | NS, NS, NS, 2 | Yes (CHW works with nurse practitioner) | Home visiting, health education, health coaching§ |
| Kattan et al. 200540 | Cost-effect | 937 No stated description |
State or federal | Pediatric | Asthma | Yes (at least one hospitalization and 2 unscheduled asthma visits in the 6 months before enrollment) | None | Urban; MA, NY, IL, TX, WA, AZ | 2 years | Home | NS, NS, 24, 1 | No | Home visiting, environmental modification |
| Mirambeau et al. 201330 | Cost-effect | Not stated Not stated |
State or federal; insurance provider; healthcare provider | Adult | Not stated | Yes (patient at the Northeastern Vermont Regional Hospital) | None | Rural; VT | Not stated | Hospital | NS, NS, NS, NS | No | Connecting with social services, care coordination, connecting to health services, health coaching |
| Ryabov 201464 | Cost-effect | 30 Hispanic |
Not stated | Adult | Type II diabetes | No | Yes (low income) | Rural; TX | 2 years | Primary care center | 24, NS, 24, 1 | No | Home visiting, health education, health coaching |
*We reported funding sources as one or more of seven types: private foundation, insurance provider, state or federal, healthcare provider, academic institution, local government, or other non-profit organization
†Intensity: number of visits, average length of visits (min), intervention length months, all group visits = 3, mixed group/one on one = 2, only one on one = 1, NS = Not stated
‡To describe the CHW role, we categorized CHW roles into eight groups: connecting patients with social service, care coordination, connecting patients to health services, health coaching, home visiting, environmental modification, advocacy, and health education. We assigned one or more of these labels to each study to capture all of the activities that the CHWs performed
§Community health workers were explicitly reported as bilingual
Table 3.
Cost and Utilization Outcomes
| Utilization | |||||||
|---|---|---|---|---|---|---|---|
| Citation and patient population | Study design | Methodology score | ED visits | Hospitalizations | Urgent care visits | Medication use | Other healthcare use |
| Babamoto et al. 200933
Adult, type II diabetes |
RCT | 3 (5) | Change from baseline CHW grp: total visit decrease 11% Care management grp: total visit increase 40% Control grp: increase 15%† |
N/A | N/A | Change from baseline CHW grp: adherence increase 10% Care management grp: adherence decrease 22% † Control grp: decrease 17% † |
N/A |
| Bryant-Stephens and Li 200835
Pediatric asthma |
RCT Control not randomized |
2 (5) | Mean ED visits before/after intervention HV grp: 1.99/1.02†* Obs. grp: 2.20/1.09† Control grp: 0.69/1.48 *HVE vs. CTRL: (p < 0.01) |
Mean hosp. days before/after intervention HV grp: 0.66/0.33†* Obs. grp: 0.56/0.32† Control grp: 0.59/1.20 *HVE vs. CTRL: (p < 0.05) |
Mean sick visits before/after intervention HV grp: 1.32/0.84† (p < 0.05)* Obs. grp: 1.31/1.05 Control: 0.67/1.35 *HVE vs. CTRL: (p < 0.05) |
Albuterol use from baseline HV grp: decrease 25% † Obs. grp: decrease 22% Controller Meds use from baseline HVE grp: increase 3% Obs. grp: increase 2% |
N/A |
| Fisher et al. 200936
Pediatric and adult asthma |
RCT | 4 (5) | For ED visits not followed by a hospitalization (1+ visits) Intervention grp: 64%, Control grp: 54% (p = 0.11) |
Hospitalizations Intervention grp: 36.5% Control grp: 59.1% (p < 0.002)* One or more hospitalization during study period: Relative risk of hospitalization Intervention grp: 0.61 (0.45–0.83)* Main effect of intervention was significant (p < 0.001)* Controlling for admissions the prior year |
N/A | N/A | N/A |
| Gary et al. 200937
Adult, type II diabetes mellitus |
RCT | 4 (5) | Relative risk 24 months after start Intervention grp: 0.77 (0.59–1.00)* Relative risk 36 months after start Intervention grp: 0.80 (0.62–1.03) |
Relative risk 24 months after start Intervention grp: 0.91 (0.64–1.19) Relative risk 36 months after start Intervention grp: 0.79 (0.59–1.06) |
N/A | N/A | N/A |
| Hopper et al. 198438
Adult, diabetes mellitus |
RCT | 2 (5) |
Intervention grp: decreased -0.02 (-1.92–1.88) Control grp: increased 0.24 (-0.41–0.89) |
N/A | N/A | N/A | Mean eye clinic visits per year change from baseline Intervention grp: increase 0.42 (0.12–0.72)† Control grp: decrease 0.02 (-0.28–0.25) |
| Hunter et al. 200461
Adult, none |
RCT | 2 (5) | N/A | N/A | N/A | N/A | Relative risk of return visit Intervention grp: increase 35%, 1.35 (0.95–1.92) |
| Kangovi et al. 201451
Adult, none |
RCT | 4 (5) | N/A | Percent sample readmitted: Intervention grp: 15.0% Control grp: 13.6%, (p = 0.68) Multiple readmissions: Intervention grp: 2.3% Control grp: 5.5% (p = 0.08) |
N/A | N/A | Odds ratio: timely post-hospital primary care visit Intervention grp: 1.52 (1.03–2.23)* Odds ratio Multiple readmissions sub-group: Intervention grp: 0.4 (0.14–1.06) |
| Krieger et al. 199960
Adult, elevated blood pressure |
RCT | 4 (5) | N/A | N/A | N/A | N/A | Completions of follow-up visit Intervention grp: 39.4% higher from usual care (p < 0.001)* |
| Krieger et al. 200555
Pediatric asthma |
RCT | 4 (5) | N/A | N/A |
High intensity grp: decreased 15% from baseline (p <0.001)† Low intensity grp: decreased 3.9% from baseline |
N/A | N/A |
| Krieger et al. 201554
Adult asthma |
RCT | 4 (5) | N/A | N/A | Change in mean urgent care visits Intervention grp: 3.46 to 1.99 from baseline (p < 0.001)† Control grp: 3.30 to 1.96 from baseline (p < 0.005)† Intervention effect: -0.07 (p = 0.83) |
Days of rescue medication (2-week frame) Intervention grp: 7.30 to 4.50 (p < 0.001)† Control grp: 7.40 to 6.08 (p < 0.005)† Intervention effect: -1.38 (p = 0.01)* Mean oral steroid use (12-month frame) Intervention grp: 3.94 to 1.16 (p = 0.21) Control grp: 5.68 to 2.45 (p = 0.33) Intervention effect: -1.18 (p = 0.42) |
N/A |
| Kronish et al. 201457
Adult, reported occurrence of stroke or “mini-stroke” in past 5 years |
RCT | 4 (5) | N/A | N/A | N/A | Antithrombotic adherence: Intervention grp: increase 1% from baseline Control grp: stagnant 84% from baseline Not significant across groups (p = 0.79) |
N/A |
| Martin et al. 201459
Pediatric persistent/uncontrolled asthma |
RCT | 4 (5) | N/A | N/A | N/A | Correct steps for inhaler use at 12 months Intervention grp (2): 14.2% more than control grp (p < 0.01)* Odds ratio for corticosteroid use Intervention grp (1): 0.2 (0.0–0.8)* |
N/A |
| Nelson et al. 201139
Pediatric asthma |
RCT | 5 (5) | Relative risk compared to control Intervention grp: 0.94 (0.77–1.15) |
Relative risk compared to control Intervention grp: 0.91(0.59–1.41) |
N/A | N/A | Relative risk asthma monitoring primary care visit Intervention grp: 1.21 (1.04–1.41)* Relative risk non-asthma primary care visit Intervention grp: 1.47 (1.04–2.08)* |
| Parker et al. 200853
Pediatric asthma |
RCT | 3 (5) | N/A | N/A | Odds ratio unscheduled medical care intervention effect Intervention grp: 0.4 (p = 0.004)* |
N/A | N/A |
| Rothschild et al. 201456
Adult, type II diabetes treated with at least 1 oral hypoglycemic agent |
RCT | 3 (5) | N/A | N/A | N/A | No change in medication adherence observed Overlapping confidence intervals |
N/A |
| Wang et al. 201234
Adult, at least one chronic illness, including mental health and addiction |
RCT | 4 (5) | Incident rate ratio of annual visit Intervention grp: 0.49 (0.34–0.70)* |
Incidence rate ratio of Hospitalization Intervention grp: 0.89 (0.44–1.82) |
N/A | N/A | N/A |
| Adair et al. 201247
Adult, hypertension, diabetes, or heart failure |
Pre-post | Moderate (1) | Total number of visits decreased 310 to 259 (year during intervention) to 269 (year post) | Total number decreased from 188 to 166 (year during intervention) to 177 (year post) | N/A | No change in ACEI/ARB use (p = 0.549); aspirin use increase 10% from baseline (p < 0.001)† | N/A |
| Ferrer et al. 201348
Adult, high-risk patients |
Pre-post | Weak (3) | 12% total visit increase from baseline | 24% total visit decrease from baseline | N/A | N/A | N/A |
| Fox et al. 200745
Pediatric asthma |
Pre-post | Weak (2) | 18.3% total visit decrease from baseline† (p < 0.0001) | 6.9% total visit decrease from baseline† (p < 0.0001) | 30.8% total visit decrease from baseline† (p < 0.0001) | Total count frequent use of rescue medication: 30.5% decrease from baseline† (p < 0.0001) | N/A |
| Margellos-Anast et al. 201241
Pediatric asthma |
Pre-post | Weak (3) | Median number of ED visits decreased from 2.0 to 0.0 (p < 0.0001)† | Median number of hospitalizations 0.0 to 0.0 (p < 0.0001)† Range decreased 0–6 at baseline to 0–3 follow-up |
Median number of urgent care visits1.0 to 1.0 (p = 0.003)† Range decreased 0–12 at baseline to 0–8 at follow-up |
N/A | Median general clinic visits increased from 2.5 to 3.5 (p = 0.9215) |
| Michelen et al. 200642
Pediatric, none |
Pre-post | Weak (2) |
Pearson correlation associated with decrease in ED use
Providing health education: r = 0.299 (p < 0.000)† Teaching patients to use healthcare system: r = 0.259 (p < 0.000)† Providing counseling on social/emotional issues: r = 0.408 (p < 0.001)† |
N/A | N/A | N/A | N/A |
| Postma et al. 201143
Pediatric asthma |
Pre-post | Strong (0) | Mean visits per patient decreased 0.46 to 0.22† (p < 0.005) | Mean admissions per patient decreased 0.15 to 0.01 (p < 0.0005)† | N/A | Rescue medication adherence: 32.5% increase from baseline (p < 0.0005)† Medication refilled before running out: 34.4% increase from baseline (p < 0.0005)† |
N/A |
| Primomo et al. 200646
Pediatric asthma |
Pre-post | Weak (3) | 5% total visit decrease from baseline (p = 0.3) | 12.9% total visit decrease from baseline (p = 0.01)† | Total count unscheduled doctor visits: increase 4% (p = 0.66) | Total count long-term asthma control prescription: 7% increase (p = 0.224) Quick relief prescriptions: 10% increase (p = 0.028)† |
N/A |
| Turyk et al. 201344
Pediatric asthma |
Pre-post | Moderate (1) | 22.9% decrease from baseline (p < 0.0001)† | 11% decrease from baseline (p < 0.0001)† | 26.7 decrease from baseline (p < 0.0001)† | Controller use: 13.6% increase from baseline (p < 0.0001)† | N/A |
| Bryant-Stephens et al. 200949
Pediatric asthma |
Cohort | 5 (9) | 30% decrease in mean number of visits per year per patient from baseline† (2.3 to 1.6) (p < 0.001) | 53% decrease in mean number of visits per year per patient from baseline (0.89–0.43) (p < 0.001)† | N/A | Total frequency in albuterol use: 0.01 decrease (p = 0.89) | N/A |
| Enard and Ganelin 201350
Pediatric and adult, none |
Cohort | 7 (9) | >1 Primary care-related ED visits prior to intervention: mean visit decreased by 0.9 per patient† (p < 0.001) >5 Primary care-related ED visits prior to intervention: mean visits decrease by 3.4 per patient (p < 0.001) |
N/A | N/A | N/A | N/A |
| Felix et al. 201152
Adult, long-term care needs |
Cohort | 8 (9) | N/A |
Intervention grp: inpatient hospital costs decreased $433 per person; outpatient hospital decreased $6 Comparison grp: inpatient hospital costs decreased $713 per person; outpatient hospital costs increased $152 per patient |
N/A | N/A | N/A |
| Freeborn et al. 197862
Pediatric and adult, none |
Cohort | 7 (9) | N/A | N/A | N/A | N/A | Ambulatory care Intervention groups: 146% increase for males (p < 0.001)* 139% increase for females (p < 0.004)* |
| Johnson et al. 20125
Not stated, none |
Cohort | 7 (9) |
Intervention grp: mean visits per patient decreased from 5.9 ($1,453 avg.) to 1.8 post intervention ($570 avg.) Comparison grp: mean visits per patient decreased from 4.5 ($1,051 avg.) to 1.0 post intervention ($272 avg.)* Comparison group decreased significantly across the study period (p < 0.01) |
Admissions per patient Intervention grp: mean 0.4 visits ($2358 avg.) to 0.1 visits post intervention ($410 avg.)* Comparison grp: 0.1 visits ($1,184 avg.) to 0.1 visits post intervention ($458 avg.) Intervention group decreased significantly across study period (p < 0.01) |
N/A | Non-narcotic prescriptions per patient Intervention grp: 49.8 per person ($2,409 avg.) to 18.6 per person ($848) post intervention Comparison grp: 14.2 per person ($429 avg.) to 9.1 per person post intervention ($396 avg.)* Narcotic prescriptions per patient Intervention grp: 6.6 per person ($180 avg.) to 2.3 per person ($75 avg.) post intervention Comparison grp: 1.8 per person ($31 avg.) to 0.8 per person ($22 avg.) Comparison group decreased significantly across study period (p < 0.01) |
N/A |
| Roth et al. 201258
Adult, HIV-positive |
Cohort | 7 (9) | N/A | N/A | N/A | Odds ratio adherence to HIV med Intervention grp: OR 1.83 (p = 0.046)* Viral load studies more likely in intervention group OR 3.05 (p = 0.04)* Viral load under control more likely OR 2.01 (p = 0.011)* |
N/A |
| Brown et al. 201263
Adult, type II diabetes |
cost-effectiveness | 14 (19) | N/A | N/A | N/A | N/A | N/A |
| Kattan et al. 200540‡ Pediatric, physician-diagnosed asthma |
cost-effectiveness | 16 (19) | Difference in mean ED visits: intervention vs. control: −0.10 (p = 0.30) |
Difference in mean inpatient days: intervention vs. control: -0.11 (p = 0.39) |
Difference in mean unscheduled visits: 19% decrease relative to control (p = 0.03)* | Difference in mean inhalers: intervention vs. control: -0.86 (p < 0.001)* |
Difference in mean scheduled medical visits: intervention vs. control: -0.07 (p = 0.62) |
| Mirambeau et al. 201330
Not stated, not stated |
cost-effectiveness | 13 (19) | N/A | N/A | N/A | N/A | N/A |
| Ryabov 201464
Adult, type II diabetes |
cost-effectiveness | 13 (19) | N/A | N/A | N/A | N/A | N/A |
*Indicates significance between groups (control-intervention)
†Indicates significance within groups (pre-post single sample)
‡This cost-effectiveness study also included some outcome results reported relative to a randomized control and is considered an RCT in discussions of those outcomes
Data Collection and Synthesis
We extracted data based on a codebook developed by members of the research team (SA, HJ). The codebook included definitions for each indicator and sample extractions. Indicators selected are displayed in the top row of Tables 2 and 3 and adhered to the PICOS criteria: patient (participant characteristics), intervention, comparison (study design and comparison group if present), outcome, and setting. Two researchers (HJ, SA) piloted the codebook on a small sample of studies and compared data extracted for consistency. The codebook was revised based on inconsistencies. Based on preliminary analysis of the data, we classified CHW activities into eight categories (Table 2) and described each intervention using one or more activity labels. As we extracted cost or outcome data, we maintained the units and format of data as the initial study presented it. We considered a p-value of less than 0.05 statistically significant. Because of variation in intervention and outcome reporting, we were not able to conduct a meta-analysis of study findings and thus had no specific summary measures. We compared the characteristics (displayed in Table 3) of RCTs with significant or non-significant results for the most costly utilization indicators (hospitalizations, urgent care visits, and ED visits) to look for trends and develop hypotheses about which features contribute to positive outcomes. We focused on RCTs in these comparisons because of their increased methodological rigor and decreased susceptibility to publication bias.31 , 32 To examine trends in CHW intervention efficacy by population, we examined outcomes of studies addressing certain key conditions (asthma, diabetes) and targeting low-income populations.
To facilitate comparison between studies, we grouped the studies by outcome for our analysis and compared studies only within each outcome. We indicate only the direction of change and its statistical significance (significant, not significant, not calculated). Studies were considered statistically significant if they had p < 0.05. Detailed information about the outcomes of each study is displayed in Table 3.
In this review, we aim to test the hypotheses that:
CHWs reduce healthcare costs and utilization.
Interventions that have CHWs integrated into the care team will have more positive results than those that do not integrate CHWs.
RESULTS
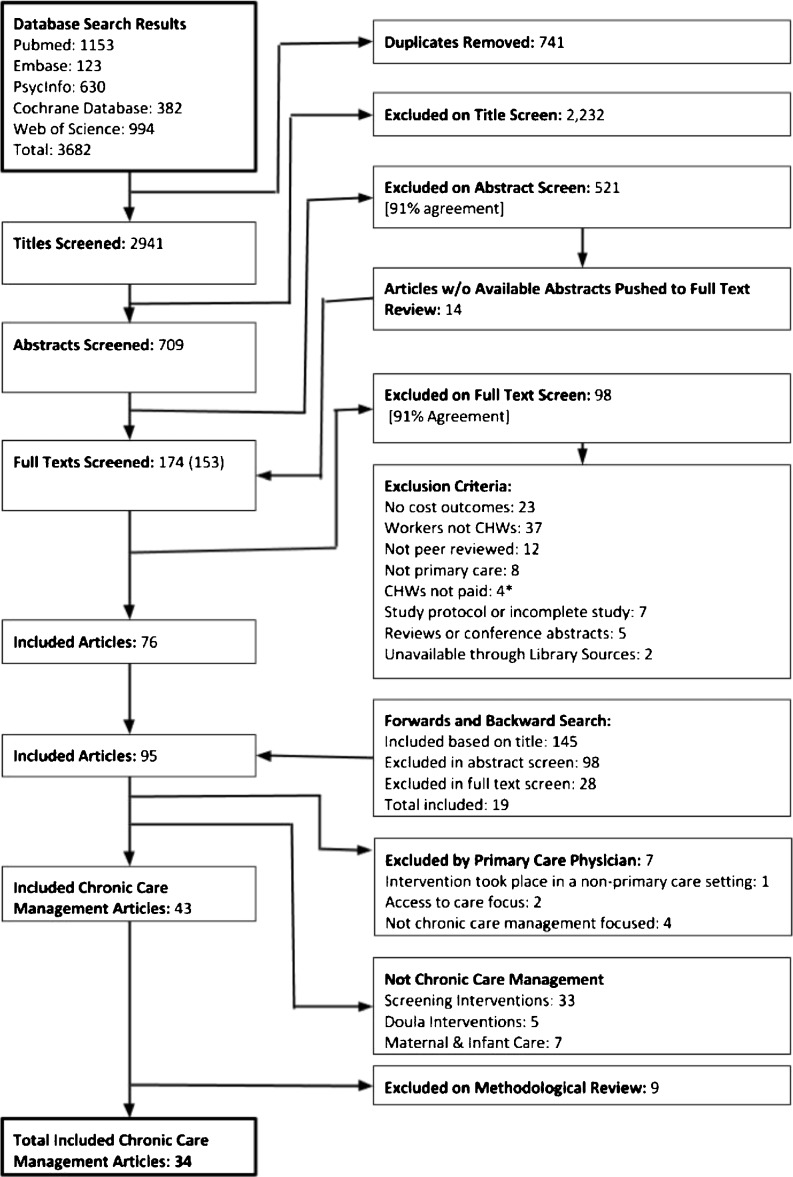
Our search yielded 2,941 results after duplicates were removed, 43 of which satisfied inclusion criteria (Fig. 1). We excluded nine studies based on the methodological review, leaving 34 studies in the final review (Appendix 2, available online). Reviewers were consistent in 91% of inclusion/exclusion decisions in both abstract and full text screens.
Fig. 1.
Flowchart of inclusion and exclusion of studies
Description of Included Studies
Sixteen studies (47%) were randomized control trials (RCTs), eight were pre-post studies (24%), six were cohort studies (18%), and four were cost-effectiveness analyses (12%). Interventions generally targeted either children (n = 13; 38%) or adults (n = 18; 53%), with only three (9%) including both. Most studies included only patients with a specific chronic condition, including asthma (n = 14; 41%), diabetes (n = 6; 18%), hypertension (n = 1; 3%), stroke (n = 1; 3%), or HIV (n = 1; 3%). Some studies had prior preventable healthcare use, such as recent ED visits for asthma, as an inclusion criteria (n = 14; 41%) or included only low-income, Medicaid, or uninsured patients or recruited patients from low-income areas (n = 14; 41%).
Interventions varied in intensity, lasting from two weeks to two years, and consisted of individual visits (n = 28; 82%), group visits (n = 3; 9%), or a combination of the two (n = 1; 3%) (two studies did not specify visit type.) Seven studies (21%) described specific ways in which CHWs were integrated into the care team. Information about the study setting, intervention, and patient population are shown in Table 2.
Emergency Department Visits
Nineteen studies (56%) measured change in ED visits during or after the CHW intervention. Of those, eight were RCTs, and three showed a significant decrease in ED visits during or after the intervention, relative to a randomized control.33 – 35 Five showed no significant difference in ED visits.36 – 40
Of the eight pre-post studies, five showed a significant decrease in ED visits relative to a baseline measurement,41 – 45 and one had no significant decrease.46 Two pre-post studies did not indicate statistical significance; of these, one intervention resulted in a decrease in ED visits47 and one in an increase in ED visits.48 There were three cohort studies that examined ED use, two of which showed significant decreases in ED use in the intervention group.49 , 50
Hospitalizations
Seventeen studies (50%) assessed the effect of the CHW intervention on hospitalizations, primarily during the CHW intervention. Of the seven RCTs, six showed no significant decrease in hospitalizations relative to a control or a randomized observation group.34 , 35 , 37 , 39 , 40 , 51 One showed a significant decrease relative to the control.36 Of the seven pre-post studies that assessed hospitalization, all showed a decrease in hospitalizations,41 , 43 – 48 but only five indicated statistical significance.41 , 43 – 46 Three cohort studies assessed the effect of the intervention on hospitalizations. One showed a decrease in costs without significance given52; two indicated a significant decrease relative to an observation cohort.5 , 49
Urgent Care Visits
Seven studies (21%) measured the effect of the CHW intervention on use of urgent care or other unscheduled outpatient medical services. Two of four RCTs demonstrated a significant decrease relative to control,40 , 53 and two showed no significant decrease relative to control.54 , 55 Of the four pre-post studies measuring this outcome, three demonstrated a statistically significant decrease,41 , 44 , 45 and one showed a non-significant increase.46
Medication Use
Fifteen studies (47%) measured medication use, assessing adherence (six studies), preventable use (six studies), or both (three studies). Of those assessing adherence, three RCTs found no significant change relative to a control.33 , 56 , 57 Of four pre-post studies, three found an increase relative to baseline,43 , 44 , 47 and one cohort study noted increased adherence relative to an observation cohort.58 Of the four RCTs measuring preventable use, three found a statistically significant decrease relative to a control.40 , 54 , 59 Three pre-post studies found a decrease in preventable use relative to baseline.43 , 45 , 46 One cohort study found no change in emergency medication use,49 while another (the only study that measured medication costs) noted a significant decrease in non-narcotic prescription costs for the control cohort relative to the CHW group.5
Scheduled Outpatient Visits
Eight studies (24%) assessed aspects of healthcare utilization other than ED visits, hospitalizations, urgent care, or medication use. Of those, all measured scheduled outpatient visits, such as scheduled primary care provider appointments or maintenance appointments for a chronic condition. Three of six RCTs showed a significant increase in visits relative to a control,39 , 51 , 60 while three had no significant change.38 , 40 , 61 One pre-post study found no significant change in clinic visits,41 and a single cohort study saw a significant increase in ambulatory care.62
Cost reporting
The 17 studies (50%) that reported either program costs, overall costs (including savings from changes in utilization), or both are summarized in Table 4. In the 14 studies that reported on program costs, the cost per patient or family per year ranged from $200 to $1472, but studies were not consistent in which operational costs they included in these totals, which does not enable direct comparison.
Table 4.
Studies that Examined Change in Overall Cost
| Citation | |||||
|---|---|---|---|---|---|
| Study design | Methodology rating | Program costs | Changes in overall costs | Costs calculation | |
| Bryant-Stephens and Li 200835 | RCT | 2 (5) | $675 per family per year | – | |
| Krieger et al. 200555 | RCT | 4 (5) | – | High intensity calculated cost savings: $201-$334 per child; low intensity cost savings: $185-$315 per child‡ | Savings calculated based on visits averted × average cost of visit type |
| Krieger et al. 201554 | RCT | 4 (5) | $1300 per participant per year | – | |
| Rothschild et al. 201456 | RCT | 3 (5) | $1020 per participant per year* | – | |
| Adair et al. 201247 | Pre-post | Moderate (1) | $392 per participant per year* | Net savings $103,065† | Savings calculated based on visits averted × average cost of visit type |
| Ferrer et al. 201348 | Pre-post | Weak (3) | – | 9% decrease in total charges, savings compared with prior year $250,215† | Savings calculated based on matched patient utilization in year prior |
| Margellos-Anast et al. 201241 | Pre-post | Weak (3) | – | Cost saving $2561.60 per participant. ROI: $5.58 per dollar spent† | Savings calculated based on visits averted × average cost of visit type |
| Primomo, et al. 200646 | Pre-post | Weak (3) | $200 per family total* | – | |
| Bryant-Stephens et al. 200949 | Cohort | 5 (9) | $450-$500 per family total* | – | |
| Enard and Ganelin 201350 | Cohort | 7 (9) | $45,880 per CHW per year* | Mean cost savings ranged per person from $331 to $1,369 depending on frequency of use in year prior to intervention† | |
| Felix et al. 201152 | Cohort | 8 (9) | $896,000 total costs* | Physician office spending decreased by $266 per person in the intervention, decreased by $49 per person in the comparison. Cost increased 19.3% over study period intervention compared with 30% increase in case control: total savings per person $1565‡ in intervention. 23.8%‡ net saving per participant 2005–2008 ($2.619 million) |
|
| Johnson et al. 20125 | Cohort | 7 (9) | $559 per participant per year* |
Accrued participant costs over study period
Intervention group: Total ED costs $225,324; Total inpatient costs $183,812‡; Total non-narcotics Rx costs $379,970 Total narcotics Rx costs $33,647 Comparison group: Total ED costs $121,858; Total inpatient costs $205,144; Total non-narcotic Rx costs $171,602 Total narcotic Rx costs $9,812 |
|
| Roth et al. 201258 | Cohort | 7 (9) | – | No significant savings across total claims (pharmacy, outpatient, inpatient, emergency, lab, home health, long-term care, other) | |
| Brown et al. 201263 | Cost-effect | 14 (19) | $783.75 per participant per year* | Incremental cost-effectiveness ratio (ICER): $10,995 to $33,319 per QALY gained | ICER calculated using actual costs and Archimedes Model |
| Kattan et al. 200540 | Cost-effect (RCT) | 16 (19) | $1472 per family total | Intervention costs were $1042 greater than control group; service reductions were unable to offset cost. Subgroup analysis yielded no savings | ICER curve based on average health care costs per symptom-free day |
| Mirambeau et al., 201330 | Cost-effect | 13 (19) | $420,640 total program costs* | – | |
| Ryabov 201464 | Cost-effect | 13 (19) | $824 per participant per year | Incremental cost-effectiveness ratio: $13,810 per QALY gained | ICER calculated using recorded data CDC Diabetes Cost Effectiveness Model |
*Indicates that some program costs, such as salary or benefits, were taken into account in cost reporting
†Indicates that study did not assess significance of reported cost-savings
‡Indicates significance at P < 0.05 level
Eleven studies tracked changes in overall costs, including both the intervention costs and savings from reduced utilization. Seven studies included both the cost of the intervention and overall healthcare cost-related outcomes, and four studies reported cost-related outcomes without directly reporting operational costs. Eight studies found the CHW interventions decreased costs, while three suggested that the CHW interventions yielded no savings.5 , 40 , 58
Two studies, both of which focused on care for adults with type II diabetes in Texas, assessed the cost-effectiveness of a CHW intervention. One found that each additional quality-adjusted life year (QALY) gained as a result of the CHW intervention cost $10,995 to $33,319.63 The other found that each additional QALY cost $13,810.64 The typical benchmark for the cost-effectiveness of an intervention is $50,000 or less per QALY.65
Features of Interventions with Positive Utilization Outcomes
Fourteen studies (41%) demonstrated a statistically significant decrease in ED visits, hospitalizations, or urgent care visits among patients who received a CHW intervention, relative to a randomized control, baseline measure, or observational cohort. An additional three studies reported positive results for these outcome measures, but did not calculate statistical significance. To assess whether interventions with reductions in ED utilization, hospitalizations, and/or urgent care were associated with distinct patient traits, we examined these outcomes across common populations. Of 13 studies focused on pediatric asthma populations, significant reductions were achieved in hospitalization, ED visits, or urgent care visits in 9 of the 10 studies that reported these outcomes. Six studies focused on diabetic populations, where two of three studies achieved key outcome reductions. Fourteen studies focused on low socioeconomic status or public insurance populations, and significant reductions across key outcomes were reported in seven of nine studies. A more detailed examination of utilization indicators by these populations is presented in Appendix 3, available online.
There was a trend for non-randomized studies to have more positive outcomes than RCTs. For both ED visits and hospitalizations, the frequency of positive RCTs was much less than in pre-post studies (ED visits: 3/8 RCTs positive, 5/8 pre-post positive; hospitalizations: 1/6 RCTs positive, 7/7 pre-post positive; urgent care visits: 2/4 RCTs positive, 4/4 pre-post positive). In light of this skew and the increased rigor of RCTs, we examined RCTs to compare the features of interventions that demonstrated a statistically significant decrease in healthcare utilization with those that did not. Of the 17 RCTs, 5 (29%) had statistically significant positive results in at least one of these areas. Seven (41%) showed no significant change in these outcomes. The other RCTs (five studies; 29%) did not measure ED visits, hospitalizations, or urgent care visits. Features and results of positive and negative RCTs are presented in Table 5.
Table 5.
Characteristics and Results of Interventions Evaluated with an RCT
| Prior preventable healthcare use as inclusion criteria | Low-income patients† | Patients with asthma | Home visiting | CHW works one on one with patient | Urban | All or part of intervention delivered in a hospital setting | CHW described as integrated into care team | Intervention lasts for at least 1 year | Average study quality (score on Jadad scale)‡ | |
|---|---|---|---|---|---|---|---|---|---|---|
| RCTs showing a significant difference* (n = 5) | 2/5 (40%) | 1/5 (20%) | 3/5 (60%) | 5/5 (100%) | 5/5 (100%) | 5/5 (100%) | 1/5 (20%) | 2/5 (40%) | 5/5 (100%) | 3.8 |
| RCTs showing no significant difference* (n = 7) | 2/7 (28%) | 4/7 (57%) | 4/7 (57%) | 6/7 (86%) | 6/7 (86%) | 7/7 (100%) | 3/7 (43%) | 0/7 (0%) | 5/7 (71%) | 3.4 |
| Study quality | Score on the Jadad Scale ‡ indicated in parentheses | |||||||||
| RCTs showing a significant result | Fisher et al. 200936 (4); Gary et al. 200937 (4); Parker et al. 200853 (3); Wang et al. 201234 (4); Kattan et al. 200540 (4) | |||||||||
| RCTs showing no significant result | Babamoto et al. 200933 (3); Bryant-Stephens and Li 200835 (2); Hopper et al. 198438 (2); Kangovi et al. 201451 (4); Krieger et al. 200555 (4); Krieger et al. 201554 (4); Nelson et al. 201139 (5) | |||||||||
*Significant difference in ED visits, urgent care visits, or hospitalizations
†Based on insurance status, income status, or residence in low-income area
‡The Jadad Scale provides a quality rating out of 5 for RCTs; a score of 5 indicates greatest rigor
DISCUSSION
Our results provide evidence that CHW-based interventions have the potential to reduce costs and preventable healthcare utilization. We have shown that many, but not all, CHW interventions reduce healthcare utilization (Hypothesis One) and that interventions with CHWs integrated into the care team trend toward better outcomes (Hypothesis Two). Because of the variability in interventions, outcomes, and study quality, our findings do not allow us to draw firm conclusions about the effects of CHW interventions on costs or healthcare utilization.
Of the studies that reported overall costs, the majority found that the CHW interventions were cost saving, and all studies that measured the per-patient annual cost indicated that interventions are low cost, less than $1500 per patient per year. Additionally, while RCTs showed variation in intervention effects, 42% of the RCTs that measured ED visits, hospitalizations, or urgent care visits found that the CHW intervention resulted in a statistically significant decrease in the use of at least one of those services relative to a control. Further, our results suggest that CHWs may be better suited to address the needs of patients who are at high risk of preventable health emergencies, rather than those with more advanced disease, who may require intensive inpatient care: only one RCT found that the CHW-based intervention reduced hospitalizations (1/7), while a much greater fraction of RCTs found that CHW-based interventions could reduce ED or urgent care visits (3/8 and 2/4, respectively).
Prior reviews, many of which concentrate on CHW-based interventions for a specific population, found that some, but not all, CHW-based interventions are cost saving or reduce preventable utilization,2 , 8 , 12 , 15 , 21 findings that correspond with our results. Our review builds on prior reviews that have examined the effects of CHW programs across diagnoses by showing that CHWs can reduce potentially preventable healthcare use for patients with chronic conditions, while prior studies have shown that they can increase appropriate healthcare use (routine or screening visits) for patients who do not yet have a severe, chronic disease.8 , 15 Together, these findings can help payers choose which types of CHW interventions to fund.
Our review shows that costs or utilization was assessed in CHW-based interventions used to meet the needs of patients with five different chronic diseases or a combination of chronic conditions. There was, however, a focus on interventions for patients with asthma. While asthma accounts for a relatively larger number of preventable ED and hospital visits than many chronic conditions,18 , 66 there is a need to explore the role that CHWs can play in improving outcomes and reducing costs for other conditions. For example, none of the studies in this review focused on behavioral health, although CHWs have been involved in mental health and substance use disorder care,67 and behavioral health is often high cost for payers and hospitals.68
The variation in the cost and utilization outcomes suggests that CHWs alone do not make an intervention successful. Like other healthcare workers, CHWs can be deployed in different ways. By examining characteristics of the positive and negative RCTs, we can develop hypotheses about what intervention characteristics may contribute to positive outcomes. Our findings allow us to hypothesize that setting (outside a hospital), integration (CHWs within a care team), and duration (1 year or more) may contribute to successful CHW interventions. These hypotheses warrant further study, as they are based on a small number of heterogeneous studies and observed trends, rather than statistical analysis. Overall, however, there were few apparent differences between the interventions that produced positive results and those that did not. The lack of clear differentiating factors may be, in part, due to the paucity of research on effects of CHW-based interventions in the US, constraining the sample size of this systematic review. There is also variable standardization and detail in descriptions of CHW-based interventions, limiting our ability to identify differentiating factors. To improve published descriptions of future interventions, we propose characteristics that should be reported for all CHW programs in Table 6.
Table 6.
Reporting Domains for CHW Interventions
| 1 | CHW background and training: Initial training (hours), competencies covered in training, CHW connection to population served, CHW prior qualifications (for instance, professional degree, bachelor’s degree, or lack thereof) |
| 2 | CHW management and integration: CHW supervisor (job title), CHWs per supervisor, description of supervisor role, description of integration of CHW into care team and CHW role delineation |
| 3 | Intensity of intervention: Amount of CHW-patient contact (hours per month), length of CHW intervention (months), patients per CHW, location of CHW visits, intensity of visits (group, mixed, or individual) |
| 4 | Content of intervention: Description of CHW activities with patients or other care team members (environmental modification, accompaniment, advocacy, etc.) |
| 5 | Patient population: Disease status, prior healthcare utilization, income or insurance status, racial or ethnic background, age, geographic area, education, comorbidities |
| 6 | Financing: Cost of intervention (per patient per year), source of funding for intervention, length of funding availability, benefits, and operational costs |
Our review has a number of limitations. First, there is great heterogeneity in study design, population, reporting of intervention characteristics, and outcomes measured, making it difficult to compare studies or determine which intervention characteristics are associated with positive outcomes. Second, the methodological rigor of the included studies is variable. Many were not RCTs, and some did not include calculations of statistical significance. However, we conducted a detailed methodological review, which improved the quality of evidence included and facilitated interpretation of evidence in light of methodological rigor. Third, the findings of this review are likely affected by publication bias, as studies with negative results are less likely to be published (in particular, non-RCT designs). By using the complete list of CHW job titles collected by the Massachusetts Department of Public Health, however, we were able to identify relevant published studies that may not have been captured in the narrower search strategies used in previous reviews on CHWs. Fourth, CHWs have many positive effects on health, including improving health outcomes and experience of care, that are not captured in the financial impacts that were the focus of this study. These health effects may, in the long-term, reduce costs, but the savings may not be realized within study evaluation periods. Fifth, we excluded interventions in which CHWs were unpaid or received only a stipend, which left out some studies that were part of prior systematic reviews.
The review highlights many opportunities for research. Future studies should test the hypotheses generated in our analysis of effective CHW interventions (setting, duration, and care teams); examine characteristics that have received little attention in the current literature, including supervision structures, smartphone-based strategies combined with CHW care, and alternate settings for chronic condition management; and identify which segments of the population would be most appropriate for CHW interventions, examining diagnosis, disease severity, minority status (racial, ethnic, linguistic), and comorbidities. We should also explore how to scale-up and sustainably fund evidence-based CHW interventions, as few interventions have been scaled at a population level, and there will be greater incentive to develop and test interventions if long-term funding is available.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 29 kb)
Acknowledgements
Contributors
We would like to thank Jessica Alpert, Clemens Hong, David Osterbur, Judith Palfrey, and the staff of the Office of Community Health Workers at the Massachusetts Department of Public Health for their assistance with this review.
Funders
This study received support from the Harvard Medical School Center for Primary Care and the Massachusetts Department of Public Health (grant no. 225307).
Compliance with Ethical Standards
Conflict of Interest
During the majority of the time that this study was being conducted, Dr. Russell Phillips was an advisor to Rise Labs, a start-up that provides web-based nutrition coaching to individuals. He no longer serves in this role. All other authors declare no conflicts of interest.
Footnotes
Protocol registration number: CRD42016035728
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-016-3922-9) contains supplementary material, which is available to authorized users.
References
- 1.Community Health Workers. American Public Health Association. 2015. https://www.apha.org/apha-communities/member-sections/community-health-workers. Accessed October 23 2016.
- 2.Raphael JL, Rueda A, Lion KC, Giordano TP. The role of lay health workers in pediatric chronic disease: a systematic review. Acad Pediatr. 2013;13(5):408–20. doi: 10.1016/j.acap.2013.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wells KJ, Luque JS, Miladinovic B, Vargas N, Asvat Y, Roetzheim RG, et al. Do community health worker interventions improve rates of screening mammography in the united states? A systematic review. Cancer Epidemiol Biomark Prev. 2011;20(8):1580–98. doi: 10.1158/1055-9965.EPI-11-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blewett LA, Owen RA. Accountable care for the poor and underserved: Minnesota’s Hennepin health model. Am J Public Health. 2015;105(4):622–4. doi: 10.2105/AJPH.2014.302432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson D, Saavedra P, Sun E, Stageman A, Grovet D, Alfero C, et al. Community health workers and Medicaid managed care in New Mexico. J Commun Health Publ Health Promot Dis Prev. 2012;37(3):563–71. doi: 10.1007/s10900-011-9484-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islam N, Nadkarni SK, Zahn D, Skillman M, Kwon SC, Trinh-Shevrin C. Integrating community health workers within patient protection and affordable care Act implementation. J Public Health Manag Pract. 2015;21(1):42–50. doi: 10.1097/PHH.0000000000000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kangovi S, Grande D, Trinh-Shevrin C. From rhetoric to reality—community health workers in post-reform US Health care. N Engl J Med. 2015;372(24):2277–9. doi: 10.1056/NEJMp1502569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viswanathan M, Kraschnewski JL, Nishikawa B, Morgan LC, Honeycutt AA, Thieda P, et al. Outcomes and costs of community health worker interventions a systematic review. Med Care. 2010;48(9):792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- 9.Brownstein JN, Bone LR, Dennison CR, Hill MN, Kim MT, Levine DM. Community health workers as interventionists in the prevention and control of heart disease and stroke. Am J Prev Med. 2005;29(5 Suppl 1):128–33. doi: 10.1016/j.amepre.2005.07.024. [DOI] [PubMed] [Google Scholar]
- 10.Little TV, Wang ML, Castro EM, Jimenez J, Rosal MC. Community health worker interventions for Latinos with type 2 diabetes: a systematic review of randomized controlled trials. Curr Diab Rep. 2012;14(12):558–U71. doi: 10.1007/s11892-014-0558-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palmas W, March D, Darakjy S, Findley SE, Teresi J, Carrasquillo O, et al. Community health worker interventions to improve glycemic control in people with diabetes: a systematic review and meta-analysis. J Gen Intern Med. 2015;30(7):1004–12. doi: 10.1007/s11606-015-3247-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shah M, Kaselitz E, Heisler M. The role of community health workers in diabetes: update on current literature. Curr Diab Rep. 2013;13(2):163–71. doi: 10.1007/s11892-012-0359-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kenya S, Chida N, Symes S, Shor-Posner G. Can community health workers improve adherence to highly active antiretroviral therapy in the USA? A review of the literature. HIV Med. 2011;12(9):525–34. doi: 10.1111/j.1468-1293.2011.00921.x. [DOI] [PubMed] [Google Scholar]
- 14.Postma J, Karr C, Kieckhefer G. Community health workers and environmental interventions for children with asthma: a systematic review. J Asthma. 2009;46(6):564–76. doi: 10.1080/02770900902912638. [DOI] [PubMed] [Google Scholar]
- 15.Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. 2016;106(4):e3–e28. doi: 10.2105/AJPH.2015.302987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaughan K, Kok MC, Witter S, Dieleman M. Costs and cost-effectiveness of community health workers: evidence from a literature review. Hum Resour Health. 2015;13(1):1–16. doi: 10.1186/s12960-015-0070-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torio CME, Anne, Andrews, Roxanne M. Trends in potentially preventable hospital admissions among adults and children, 2005–2010. Agency for Healthcare Research and Quality: Rockville, MD; 2013. [PubMed] [Google Scholar]
- 18.Fingar KRB, Marguerite L, Elixhauser A, Stocks C, Steiner CA. Trends in potentially preventable inpatient hospital admissions and emergency department visits. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 20.Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, van Wyk B, et al. Lay health workers in primary and community health care: Cochrane systematic review. Int J Epidemiol. 2005;34(6):1250–1. doi: 10.1093/ije/dyi198. [DOI] [PubMed] [Google Scholar]
- 21.Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–56. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 22.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos—A qualitative systematic review. Am J Prev Med. 2007;33(5):418–27. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 23.Community health workers in Massachusetts: Improving health care and public health: Massachusetts Department of Public Health. 2009.
- 24.Community health workers: Essential to improving health in Massachusetts: Massachusetts Department of Public Health. 2005.
- 25.Kahn-Troster S, Sheedy K. State Community Health Worker Models. In: Models SCHW, editor. State Reforum. Washington, DC: Robert Wood Johnson Foundation National Academy for State Health Policy; 2016. [Google Scholar]
- 26.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 27.Thomas H. Quality assessment tool for quantitative studies. McMaster University, Toronto: Effective Public Health Practice Project; 2003. [Google Scholar]
- 28.Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
- 29.Evers S, Goossens M, De Vet H, Van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. Int J Technol Assess Health Care. 2005;21(02):240–5. [PubMed] [Google Scholar]
- 30.Mirambeau AM, et al. A cost analysis of a community health worker program in rural Vermont. Jcommunity health. 2013;38(6):1050–1057. [DOI] [PMC free article] [PubMed]
- 31.Shrier I, Boivin J-F, Steele RJ, Platt RW, Furlan A, Kakuma R, et al. Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? A critical examination of underlying principles.(Practice of Epidemiology) (Clinical report) Am J Epidemiol. 2007;166(10):1203. doi: 10.1093/aje/kwm189. [DOI] [PubMed] [Google Scholar]
- 32.Easterbrook PJ, Gopalan R, Berlin JA, Matthews DR. Publication bias in clinical research. Lancet. 1991;337(8746):867–72. doi: 10.1016/0140-6736(91)90201-Y. [DOI] [PubMed] [Google Scholar]
- 33.Babamoto KS, Sey KA, Camilleri AJ, Karlan VJ, Catalasan J, Morisky DE. Improving diabetes care and health measures among Hispanics using community health workers: results from a randomized controlled trial. Health Educ Behav. 2009;36(1):113–26. doi: 10.1177/1090198108325911. [DOI] [PubMed] [Google Scholar]
- 34.Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102(9):e22–9. doi: 10.2105/AJPH.2012.300894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bryant-Stephens T, Li Y. Outcomes of a home-based environmental remediation for urban children with asthma. J Natl Med Assoc. 2008;100(3):306–16. doi: 10.1016/S0027-9684(15)31243-8. [DOI] [PubMed] [Google Scholar]
- 36.Fisher EB, Strunk RC, Highstein GR, Kelley-Sykes R, Tarr KL, Trinkaus K, et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adolesc Med. 2009;163(3):225–32. doi: 10.1001/archpediatrics.2008.577. [DOI] [PubMed] [Google Scholar]
- 37.Gary TL, Batts-Turner M, Yeh HC, Hill-Briggs F, Bone LR, Wang NY, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2009;169(19):1788–94. doi: 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hopper SV, Miller JP, Birge C, Swift J. A randomized study of the impact of home health aides on diabetic control and utilization patterns. Am J Public Health. 1984;74(6):600–2. doi: 10.2105/AJPH.74.6.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nelson KA, Highstein GR, Garbutt J, Trinkaus K, Fisher EB, Smith SR, et al. A randomized controlled trial of parental asthma coaching to improve outcomes among urban minority children. Arch Pediatr Adolesc Med. 2011;165(6):520–6. doi: 10.1001/archpediatrics.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kattan M, Stearns SC, Crain EF, Stout JW, Gergen PJ, Evans R, et al. Cost-effectiveness of a home-based environmental intervention for inner-city children with asthma. J Allergy Clin Immunol. 2005;116(5):1058–63. doi: 10.1016/j.jaci.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 41.Margellos-Anast H, Gutierrez MA, Whitman S. Improving asthma management among African-American children via a community health worker model: findings from a Chicago-based pilot intervention. J Asthma. 2012;49(4):380–9. doi: 10.3109/02770903.2012.660295. [DOI] [PubMed] [Google Scholar]
- 42.Michelen W, Martinez J, Lee A, Wheeler DP. Reducing frequent flyer emergency department visits. J Health Care Poor Underserved. 2006;17(1 Suppl):59–69. doi: 10.1353/hpu.2006.0010. [DOI] [PubMed] [Google Scholar]
- 43.Postma JM, Smalley K, Ybarra V, Kieckhefer G. The feasibility and acceptability of a home-visitation, asthma education program in a rural, Latino/a population. J Asthma : Off J Assoc Care Asthma. 2011;48(2):139–46. doi: 10.3109/02770903.2010.529221. [DOI] [PubMed] [Google Scholar]
- 44.Turyk M, Banda E, Chisum G, Weems D, Liu Y, Damitz M, et al. A multifaceted community-based asthma intervention in Chicago: effects of trigger reduction and self-management education on asthma morbidity. J Asthma. 2013;50(7):729–36. doi: 10.3109/02770903.2013.796971. [DOI] [PubMed] [Google Scholar]
- 45.Fox P, Porter PG, Lob SH, Boer JH, Rocha DA, Adelson JW. Improving asthma-related health outcomes among low-income, multiethnic, school-aged children: results of a demonstration project that combined continuous quality improvement and community health worker strategies. Pediatrics. 2007;120(4):e902–11. doi: 10.1542/peds.2006-1805. [DOI] [PubMed] [Google Scholar]
- 46.Primomo J, Johnston S, DiBiase F, Nodolf J, Noren L. Evaluation of a community-based outreach worker program for children with asthma. Public Health Nurs (Boston, Mass) 2006;23(3):234–41. doi: 10.1111/j.1525-1446.2006.230306.x. [DOI] [PubMed] [Google Scholar]
- 47.Adair R, Christianson J, Wholey DR, White K, Town R, Lee S, et al. Care guides: employing nonclinical laypersons to help primary care teams manage chronic disease. J Ambul Care Manag. 2012;35(1):27–37. doi: 10.1097/JAC.0b013e31823b0fbe. [DOI] [PubMed] [Google Scholar]
- 48.Ferrer RL, Schlenker CG, Romero RL, Poursani R, Bazaldua O, Davidson D, et al. Advanced primary care in San Antonio: linking practice and community strategies to improve health. J Am Board Fam Med. 2013;26(3):288–98. doi: 10.3122/jabfm.2013.03.120238. [DOI] [PubMed] [Google Scholar]
- 49.Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health. 2009;99:S657–s65. doi: 10.2105/AJPH.2009.165423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J Healthc Manag. 2013;58(6):412–27. [PMC free article] [PubMed] [Google Scholar]
- 51.Kangovi S, Mitra N, Grande D, White ML, McCollum S, Sellman J, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med. 2014;174(4):535–43. doi: 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 52.Felix HC, Mays GP, Stewart MK, Cottoms N, Olson M. THE CARE SPAN Medicaid savings resulted when community health workers matched those with needs to home and community care. Health Aff. 2011;30(7):1366–74. doi: 10.1377/hlthaff.2011.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parker EA, Israel BA, Robins TG, Mentz G, Lin XH, Brakefield-Caldwell W, et al. Evaluation of community action against asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav. 2008;35(3):376–95. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krieger J, Song L, Philby M. Community health worker home visits for adults with uncontrolled asthma: The HomeBASE trial randomized clinical trial. JAMA Intern Med. 2015;175:109–17. doi: 10.1001/jamainternmed.2014.6353. [DOI] [PubMed] [Google Scholar]
- 55.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–9. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rothschild SK, Martin MA, Swider SM, Lynas CMT, Janssen I, Avery EF, et al. Mexican American trial of community health workers: a randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am J Public Health. 2014;104(8):1540–8. doi: 10.2105/AJPH.2013.301439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kronish IM, Goldfinger JZ, Negron R, Fei KZ, Tuhrim S, Arniella G, et al. Effect of peer education on stroke prevention the prevent recurrence of All inner-city strokes through education randomized controlled trial. Stroke. 2014;45(11):3330–6. doi: 10.1161/STROKEAHA.114.006623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roth AM, Holmes AM, Stump TE, Aalsma MC, Ackermann RT, Carney TS, et al. Can lay health workers promote better medical self-management by persons living with HIV? An evaluation of the Positive Choices program. Patient Educ Couns. 2012;89(1):184–90. doi: 10.1016/j.pec.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 59.Martin MA, Mosnaim GS, Olson D, Swider S, Karavolos K, Rothschild S. Results from a community-based trial testing a community health worker asthma intervention in Puerto Rican youth in Chicago. J Asthma. 2014;52(1):59–70. doi: 10.3109/02770903.2014.950426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Krieger J, Collier C, Song L, Martin D. Linking community-based blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health. 1999;89(6):856–61. doi: 10.2105/AJPH.89.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hunter JB, de Zapien JG, Papenfuss M, Fernandez ML, Meister J, Giuliano AR. The impact of a Promotora on increasing routine chronic disease prevention among women aged 40 and older at the US-Mexico border. Health Educ Behav. 2004;31(4):18S–28S. doi: 10.1177/1090198104266004. [DOI] [PubMed] [Google Scholar]
- 62.Freeborn DK, Mullooly JP, Colombo T, Burnham V. The effect of outreach workers’ services on the medical care utilization of a disadvantaged population. J Community Health. 1978;3(4):306–20. doi: 10.1007/BF01498507. [DOI] [PubMed] [Google Scholar]
- 63.Brown HS, Wilson KJ, Pagan JA, Arcari CM, Martinez M, Smith K, et al. Cost-effectiveness analysis of a community health worker intervention for low-income Hispanic adults with diabetes. Prev Chronic Dis. 2012;9. [DOI] [PMC free article] [PubMed]
- 64.Ryabov I. Cost-effectiveness of community health workers in controlling diabetes epidemic on the US-Mexico border. Public Health. 2014;128(7):636–42. doi: 10.1016/j.puhe.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 65.Grosse SD. Assessing cost-effectiveness in healthcare: History of the $50,000 per QALY threshold. Expert Rev Pharmacoecon Outcomes Res. 2008;8(11):165–78. doi: 10.1586/14737167.8.2.165. [DOI] [PubMed] [Google Scholar]
- 66.Fingar KW. Raynard. Potentially preventable pediatric hospital inpatient stays for asthma and diabetes, 2003-2012. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [PubMed] [Google Scholar]
- 67.Wennerstrom A, Hargrove L, Minor S, Kirkland AL, Shelton SR. Integrating community health workers into primary care to support behavioral health service delivery: a pilot study. J Ambul Care Manag. 2015;38(3):263–72. doi: 10.1097/JAC.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 68.Soni A. Trends in the five most costly conditions among the US civilian noninstitutionalized population, 2002 and 2012. Rockville, MD: Agency for healthcare research and quality2015. Report No.: Statistical brief #470. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 29 kb)