Abstract
Multiple sclerosis (MS) is a chronic, inflammatory, autoimmune disease of the central nervous system, and is an important cause of disability in young adults. In genetically susceptible individuals, several environmental factors may play a partial role in the pathogenesis of MS. Some studies suggests that high-salt diet (>5 g/day) may contribute to the MS and other autoimmune disease development through the induction of pathogenic Th17 cells and pro-inflammatory cytokines in both humans and mice. However, the precise mechanisms of pro-inflammatory effect of sodium chloride intake are not yet explained. The purpose of this review was to discuss the present state of knowledge on the potential role of environmental and dietary factors, particularly sodium chloride on the development and course of MS.
Keywords: Sodium chloride intake, Multiple sclerosis, Environmental factors in MS, VGSCs
Introduction
Multiple sclerosis (MS) is a chronic, inflammatory, autoimmune disease of the central nervous system (CNS), and is a major cause of disability in young adults [1]. In genetically susceptible individuals, environmental factors play a significant partial role in the pathogenesis of MS [2]. Numerous studies examined the influence of environmental factors, such as Epstein–Barr infection [3–5], vitamin D levels [6–11], smoking [12, 13], obesity [14], sunlight exposure [15, 16], and geographic variation, on MS [17, 18].
Methodology
All quotable references were searched using Pubmed and Google scholar between March and May 2016. References that allowed free access to full text by the Medical University of Silesia were retrieved and read. The oldest publications were retrieved from the Medical University of Silesia Library. One reviewer performed literature searches and two other researchers independently screened the articles. All disagreements were discussed and resolved by the authors or in consultation with other experts. Information used in our review was evaluated using evidence-based medicine. Inclusion criteria for the articles were: original papers, systematic reviews, systematic summaries, and meta-analysis. We excluded publications written in foreign languages, such as Spanish, German, or Russian. Keywords used for literature searches were as follows: “multiple sclerosis”, “MS”, “sodium”, “sodium chloride”, “autoimmunity”, “diet”, and “VGSCs”. All keywords were in accordance with the MeSH terms. To identify the appropriate publications, we searched Pubmed and Google scholar using combinations of keywords in the following order: “MS and diet”, “MS and salt intake”, “MS and environmental factors,” and “MS and VGSCs”. After reading titles and abstracts, some articles from each combination of keywords were excluded. Most of the excluded articles were in a foreign language. The comprehensive literature search identified 907 articles that were relevant for our review. Titles, abstracts, or full articles were reviewed to determine whether each search result matched our selection criteria. We also reviewed the references of the selected original papers and review articles found by our search for additional papers relevant to our review. Only high-quality publications from the last decades were included. In addition, 306 articles were retrieved from the Medical University of Silesia Library. Of these 306 articles, we eliminated those that were too general in scope for our review.
Environmental factors influencing MS
Although some studies confirmed the link between a previous infection with Epstein–Barr virus (EBV) and the development of multiple sclerosis [3–5, 19–21], the involvement of EBV in the etiology of MS is unclear. However, certain viral infections likely increase susceptibility to MS [22]. Sero-epidemiological studies have demonstrated that almost 100% of adult MS patients are infected with EBV [19]. Late childhood infection of EBV is proposed to be the serious risk factor for the disease. Moreover, there is a strong EBV-specific CD8+ response in the blood of MS patients in the beginning of the disease and the intensity decreases in the course of the illness [2–5, 19, 20].
Low serum vitamin D levels are currently one of the most studied environmental factors influencing the development of MS. It has been shown that intake of food rich in vitamin D significantly prevents the development of MS or reduce activity of the disease [6–9, 16]. Nevertheless, some authors did not report a protective role of vitamin D supplementation for the development of MS [9, 10].
Smoking is another possible factor for the development of MS or might be responsible for worst prognosis of course of the disease [13, 23]. Furthermore, smoking cessation improved the prognosis in patients with MS. Ramanujam et al. confirmed that the time to conversion to secondary progressive MS (SPMS) decreases by 4.7% for each additional year of smoking after the diagnosis in patients with RRMS (acceleration factor 1.047; 95% CI 1.023–1.072; P < 0.01) [13].
Obesity is a probable susceptibility factor for MS and several other autoimmune diseases [24], but the relationship between increased body mass index (BMI) and disease activity has not been fully explained. There is no doubt that obesity increases levels of pro-inflammatory cytokines and is associated with low-grade inflammatory state [25]. There are reports providing that RRMS activity is higher in obese and overweight patients than in patients with normal BMI undergoing IFN β treatment [14]. Moreover, Oliveira et al. reported a positive relationship between elevated BMI and disability in MS patients [26].
Ultraviolet radiation was proposed to be a significant environmental factor influencing prevalence of the disease [15]. Reduced risk of MS through exposure to sunlight is probably mediated not only by increased production of vitamin D in the skin, but also by the synthesis of anti-inflammatory factors, such as IL-10, TNF-α, and Treg cells [16]. Therefore, the latitude is nowadays considered to be related with prevalence of MS. The disease is less frequent near the equator and more frequent in northern countries [18, 27]. Exceptions to this trend, namely, Sardinia, where the prevalence of the disease is significantly higher [28], and northern Scandinavia, with markedly low prevalence [29], may be due to genetic and behavioral factors [18].
Influence of diet on MS
It seems that diet might have a significant relationship with the inflammatory process of MS. Many studies have shown that diet plays the role in the pathogenesis of MS [17, 30–32]. Recent studies have provided the evidence for a protective role of polyunsaturated fatty acids on the risk of MS; however, there is no conclusive evidence for a beneficial role of polyunsaturated fatty acid supplementation in patients with MS. Hoare et al. demonstrated that the amount of omega-3 polyunsaturated fatty acids taken orally is inversely proportional to the risk of demyelination in the CNS [33]. Moreover, Khalili et al. found a strong correlation between oral intake of lipoic acid (1.2 mg/day) and decrease in the levels of pro-inflammatory cytokines, including INF-γ, ICAM-1, and anti-inflammatory cytokines, including TGF-β and IL-4, compared with placebo group [35]. On the other hand, Torkildsen et al. showed that consumption of omega-3 fatty acids used as monotherapy or in combination with interferon beta-1a had no beneficial effect on the disease compared to placebo [34]. Retinoic acid (RA), an active metabolite of vitamin A, revealed a strong immunosuppressive activity [36]. RA has been shown to modulate the balance between Th1/Th2 and Th17/Treg cells and B cell function, contributing to augmented tolerance and inhibited inflammatory response. It also contributes to enhanced tolerance and reduction of inflammatory effects [37]. Bitarafan et al. investigated the impact of vitamin A on disease progression in MS patients. The study evaluated the expanded disability status scale (EDSS) and MS functional composite (MSFC). The results showed that vitamin A improved MSFC in RRMS patients, but did not affect EDSS, relapse rate, or active brain lesions in MRI [38]. Ketogenic diet (high amount of fat, decreased protein content, and very low carbohydrates) was shown as potentially therapeutic in progressive forms of MS, which is especially relevant, because currently, there is no treatment for progressive forms of the disease [39, 40]. Kim et al. reported that ketogenic diet improved motor disability and cognitive impairment in mice with experimental autoimmune encephalomyelitis compared with mice on the standard diet. Furthermore, a ketogenic diet reversed structural brain lesions and reduced CNS inflammation and oxidative stress [41]. On the other hand, it was reported that creatine supplementation did not improve muscle capacity or habitual fatigue in MS individuals [42] or that restricted intake of animal fat (no more than 10–15 g/day) caused remission of the disease in patients with RRMS [43].
Polyphenols and carotenoids from vegetables, n-3 PUFA from fish, vitamins A, C, D, and E, thiol compounds, such as lipoic acid, and oligoelements, such as selenium and magnesium, have anti-oxidant properties [44, 45]. Th17 cells, which produce pro-inflammatory cytokines, are increased, whereas Treg cells are decreased in MS, and thus, the balance between Th17 and Treg cells is impaired in this disease. Vitamin A and its active metabolites (all-trans-retinoic acid and 9-cis-retinoic acid) modulate the imbalance of Th17 and Treg cells and might be beneficial to the prevention and treatment of MS [46]. Moreover, this vitamin was proposed to have a beneficial effect during interferon therapy and improved psychiatric outcomes for anti-inflammatory mechanisms [37].
Sodium channels in MS
Voltage-gated sodium channels (VGSCs) are key mediators of action potential initiation and propagation in excitable cells [47–49]. Their expression has also been reported in cell types that are traditionally regarded as non-excitable, including glia, human vascular endothelial cells, human epidermal keratinocytes, and carcinoma cells, where their role is less clear [50–55]. Aberrant functional expression/activity of VGSCs has been identified as a major contributing factor in a number of human pathologies, including cardiac arrhythmia [55], epilepsy [56, 57, 58], pain [59, 60], periodic paralysis [61, 62], migraine [63], MS [64], and cancer [65]. VGSCs exist as heteromeric membrane-bound protein complexes that typically consist of a single pore-forming α subunit in association with one or more β subunits [66, 67].
The mammalian sodium channels include ten members (Nav1.1–Nav1.9 and Nax) encoded by genes SCN1A–SCN11A. While substantial homology exists between the isoforms, differences in amino acid sequence confer distinct voltage dependence, kinetic and pharmacological properties on each of the isotypes [68, 69]. Data concerning the location and function of each VGSCs subunit are included in Table 1.
Table 1.
Voltage-gated sodium channels (VGSCs)
| Protein | Human gene | Location | Function |
|---|---|---|---|
| (A) The α subunits | |||
| Nav1.1 | SCN1A | CNS, PNS, heart | CBH, dementia [70], Dravet syndrome [71], epilepsy [71, 72] |
| Nav1.2 | SCN2A | CNS, PNS | CBH, dementia [70], epilepsy [73, 74], autism [74] |
| Nav1.3 | SCN3A | CNS, PNS | Diabetes [75], neuropathic pain [76–78] |
| Nav1.4 | SCN4A | Skeletal muscle, heart | Brugada syndrome [79], myotonia, periodic paralysis [80] |
| Nav1.5 | SCN5A | Uninnervated skeletal muscle, heart, brain | Breast cancer [81, 82], arrhythmia [83], Brugada syndrome [84], angiogenic disorders [85] |
| Nav1.6 | SCN8A | CNS, PNS, heart | Epilepsy [86], cervical cancer [87] |
| Nav1.7 | SCN9A | PNS, neuroendocrine cells, sensory neurons | Angiogenic disorders [85], paroxysmal extreme pain disorder [88] |
| Nav1.8 | SCN10A | Sensory neurons | Prostate cancer [89], cardiac arrhythmia [90], MS [90, 91] |
| Nav1.9 | SCN11A | Sensory neurons | Congenital insensitivity [92], cold-aggravated pain [93] |
| Nax | SCN6A, SCN7A | Heart, uterus, skeletal muscle, astrocytes, DRG | Atopic dermatitis [94], hypertension [95] |
| (B) The β subunits | |||
| β1 | SCN1B | Heart, skeletal muscle, CNS, glia, PNS | Epilepsy [96], cardiac arrhythmia [97], cancer [98] |
| β1A(β1B) | SCN1B | Heart, skeletal muscle, adrenal gland, PNS | Epilepsy [96] |
| β2 | SCN2B | CNS, PNS, heart, glia | Altered pain response [59], MS [99] |
| β3 | SCN3B | CNS, adrenal gland, kidney, PNS | Cancer [98] |
| β4 | SCN4B | Heart, skeletal muscle, CNS, PNS | Huntington’s disease [100] |
CNS central nervous system, MS multiple sclerosis, PNS peripheral nervous system, CBH chronic brain hypoperfusion
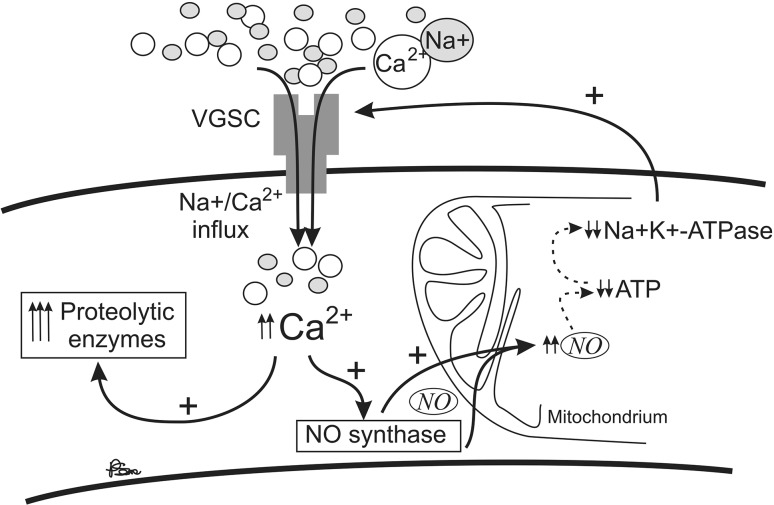
β subunits (β1–β4) combine in vivo with either β1 or β3 through non-covalent bonding and with either β2 or β4 via a covalent bond [101–104]. Numerous studies have revealed the presence of Nav1.1, Nav1.2, Nav1.3 [105], Nav1.6 [106], and Nav1.5 [107] in rodent astrocytes. Sodium channels in these glial cells are localized to the plasma membrane, where they mediate sodium currents [108]. The star-shaped glial cells situated in the CNS take an essential part in the response of the CNS to injury, including inflammation and degeneration in MS. Herzog et al. have shown that VGSCs can contribute to axonal injury in MS by providing a pathway for sustained sodium influx that drives the Na+/Ca2+ exchanger to import calcium into axons [109]. Elevated calcium levels can activate nitric oxide synthase and deleterious proteolytic enzymes [109–112]. The harmful effects of nitric oxide on mitochondrial function include a reduction in adenosine triphosphate (ATP) levels and an exhaustion of sodium–potassium adenosine triphosphatase (Na+K+-ATPase), hence compromising the axons’ capacity to maintain normal transmembrane sodium gradient. This action provides a positive feedback loop that imports even more intracellular calcium, thereby further enhancing the damage [113]. Consequently, these mechanisms lead to axonal injury and further to disability (Fig. 1).
Fig. 1.
Positive feedback loop of Na/Ca influx to the neuron cell with a potential damaging effect in multiple sclerosis (VGSC voltage-gated sodium channel, NO nitric oxide, ATP adenosine triphosphate, Na+K+-ATPase sodium–potassium adenosine triphosphatase)
Numerous studies have shown that partial blockade of voltage-gated sodium channels could result in neuroprotection in patients with MS [112]. Indeed, the axonal protection has been demonstrated in animals with experimental autoimmune encephalomyelitis (EAE) by means of the sodium channel blocking drugs flecainide [114, 115], safinamide [115], phenytoin [116], and, recently, lamotrigine [117]. Neuroprotection is emerging as a potentially important strategy for preventing disability progression in MS [118]. In contrast, some clinical studies do not support the protective role of VGSC blockers in MS. Counihan et al. studied 400 patients, 51 of whom received CBZ symptomatic therapy (average duration of therapy was 27 months), and showed that the long term exposure to the VGSC-blocking drug CBZ does not affect the long-term disability and disease progression in MS patients, despite studies in animals suggesting a neuroprotective role of VGSC blockers [119]. Furthermore, using CSF neurofilament (NfH) as a good surrogate marker of neurodegeneration in MS, Gnanapavan et al. revealed no benefit of lamotrigine in the prevention of axonal breakdown by lowering NfH levels compared to the placebo arm [120]. The protective role of lamotrigine is also disputed by Kapoor et al. [121], but it is premature to fully dismiss this hypothesis.
Sodium chloride intake and MS
High intake of sodium chloride is currently considered to be a potentially important factor influencing the onset of MS. Changes in eating habits that have occurred in recent decades in developed countries may account for an increase in incidence of MS and other autoimmune diseases [122]. Today’s typical Western diet includes more sodium chloride than it was in the past [123]. Therefore, popular processed meals, such as “fast food”, contain approximately 100 times more sodium chloride than homemade meals [124, 125]. Increased hypertonicity can stimulate the immune system [126], and furthermore, superior sodium chloride uptake can affect the innate immune system [127].
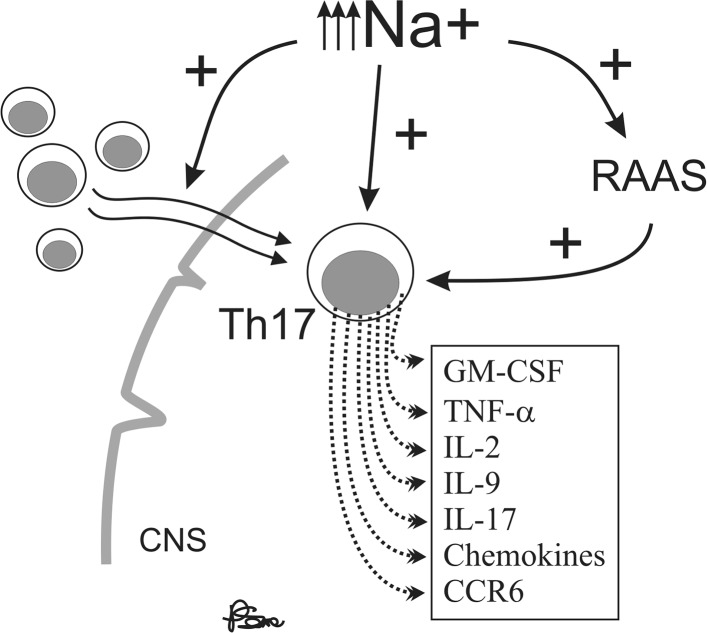
Recent studies have demonstrated the importance of interleukin-17 (IL-17)-induced CD4+ Th17 cell population in autoimmune diseases [128]. Kleinewietfield et al. showed that the addition of a modest amount of NaCl (40 mM) to a culture of differentiating Th17 cells caused a roughly logarithmic augmentation of IL-17A in naïve CD4 cells in vitro and this process was mediated by p38/MAPK, NFAT5, and SGK [122]. Moreover, high-salt concentration results in growth of pathogenic phenotype of Th17 cells [122, 129, 130]. Thus, the change in eating habits that includes a high amount of salt may contribute to the recent increase in MS incidence through the induction of pathogenic Th17 cells [122, 126, 128]. The Th17 cells induced by high-salt concentration upregulate the production of pro-inflammatory cytokines GM-CSF, TNFα, IL-2, IL-9, several chemokines [131, 132], and CCR6 [133], which are essential for the autoimmune function of Th17 cells. Higher Na+ concentration, such as that between 160 and 250 mM, in the interstitium and lymphoid tissue and significantly lower concentration of Na+ in plasma, approximately 140 mM, are likely to be the mechanism for decreasing the inflammatory response in the blood while favoring immune activation in lymphoid tissues or with migration of cells into tissue [127, 134]. Otherwise, diet rich in salt can affect the severity of the disease. Kleinewietfeld et al. showed that mice fed salty meals developed deterioration of EAE, with an increase in Th17 cell number and augmented infiltration of Th17 cells into the CNS [122]. Moreover, in an observational trial on 122 MS patients, Farez et al. demonstrated that the disease exacerbation rate was 2.75-fold in participants with medium salt intake (2–4.8 g/day) (95% CI 1.3–5.8) and 9.95-fold in participants with high sodium intake (4.8 g/day or more) (95% CI 1.4–11.2) compared with the low-intake group (under 2 g/day) [135]. This finding may be due to the fact that sodium concentration is tightly regulated within narrow limits regardless of large variations in sodium consumption, due to its importance in general metabolism [136]. The renin–angiotensin–aldosterone system (RAAS), which is a major regulator of blood pressure, also significantly affects autoimmunity in many diseases which include MS and its animal model—EAE. Han et al. showed that peptides related to the RAAS are present in CNS lesions of MS patients [137]. Sodium chloride, among many other physiological effects, modulates the renin–angiotensin system [138]. Interestingly, the activation of renin and angiotensin has been implicated in the pathogenesis of EAE [139]. Furthermore, increases in systolic blood pressure similar to those observed with high-salt consumption have recently been shown to be associated with the disruption of white matter integrity in young normotensive individuals [140]. In addition, Platten et al. demonstrated an increase in the expression of angiotensin receptor 1 (AT1R) in lymph node cells, indicating that AT1R is activated in antigen-specific T cells during the peripheral immune response to autoantigens. In addition, angiotensin II (AII) binding was augmented in Periodate–Lysine–Paraformaldehyde (PLP)-activated CD4 + T cells and to a lesser extent in activated CD11b + monocytes. Immunization with PLP139–151 led to an induction of AII in CD4 + T cells, CD11b + monocytes, and to an increase in serum AII levels, demonstrating that the RAAS is activated in peripheral immune cells. Pretreatment of mice immunized with PLP139–151 with the angiotensin converting enzyme (ACE) inhibitor lisinopril {N2-[(S)-1-carboxy-3-phenylpropyl]-L-lysyl-l-proline} or the AT1R antagonist candesartan (3-{[2′-(2 H -tetrazol-5-yl)biphenyl-4-yl]methyl}-2-ethoxy-3 H -benzo[d]imidazole-4-carboxylic acid) resulted in suppression of Th1 and Th17 cytokine release and up-regulation of immunosuppressive cytokines, such as IL-10 and transforming growth factor-β (TGF-β) [141]. Probable impact of high sodium diet on immune functions in MS patients was presented in Fig. 2.
Fig. 2.
Probable impact of high sodium diet on immune functions in multiple sclerosis patients (CNS central nervous system, RAAS renin–angiotensin–aldosterone system)
Hucke et al. revealed a multidirectional activity of sodium chloride-rich diet in both humans and mice. Sodium chloride-rich diet promotes CNS autoimmunity, increases macrophage responses, skews the balance towards a pro-inflammatory M1 phenotype in macrophages, alters MAPK signaling in macrophages, and induces a pro-inflammatory phenotype in human monocytes [142]. In addition, Yi et al. demonstrated that high-salt intake promotes an increase in human serum monocytes, which play a pivotal role in the development of various immunological diseases [143]. Furthermore, Jörg et al. showed that a high-salt diet in the early phase of neuroinflammation mainly acts on Th17 cells and is independent of myeloid cells. This finding can help elucidate the impact of a high-salt diet on the emergence and course of autoimmune diseases [144]. Krementsov et al. demonstrated an increase in blood–brain barrier permeability and brain pathology in mice as a consequence of a high-salt diet, but did not demonstrate augmentation of Th17 or Th1 responses. Moreover, this study showed that the effects of dietary sodium on autoimmune neuroinflammation are sex-specific, genetically dependent, and CNS-mediated [145]. Furthermore, Zhou et al. demonstrated that a short-term increase in dietary salt intake could induce the expansion of CD14++CD16+ monocytes, as well as an increase in monocyte platelet aggregates (MPAs), which might be the cellular basis of high-salt-induced end organ inflammation and potential thromboembolic risk, independent of changes in blood pressure [146]. In addition, Hernandez et al. reported that excess dietary sodium intake lowers immunosuppressive actions of human and murine Foxp3+ Tregs in vitro and in vivo and is associated with increased Treg IFNγ secretion in vivo [147]. Data concerning the immunological effects of sodium chloride intake are shown in Table 2.
Table 2.
Immunological effects of sodium chloride intake
| Examined subjects | Time (days) | Sodium intake | Observed effects | |
|---|---|---|---|---|
| C57BL/6J mice | 20 | Na+-rich diet | Increase in Th17 cells proliferation Exacerbation of EAE |
[121] |
| Human and rabbit PBMC | – | Na+ hipertonic medium 25–30 mM (in vitro) | T cell proliferation was doubled in 25 mM medium Increased hypertonicity (>40 mM in human cells; >80 mM in rabbit cells) caused progressive Suppression of proliferation monocyte functions augmentation |
[126] |
| Cd4 Cre Sgk1 fl/fl mice and WT mice | 21 | High-salt diet | Increase in EAE severity in WT mice, but not in SGK1-deficient mice Increase of Th17 cells in mLN and CNS of WT mice, but not in SGK1-deficient mice Increase in IFN production by T cells in the CNS in WT mice Increase in IL-17 synthesis by CD4+ T cells |
[130] |
| RRMS patients | 720 | Dietary 2–4.8 g/day of Na+ intake | Increase in exacerbation rate (2–4 fold) in patients with medium or high sodium diet Increase in the risk of developing a new MRI lesions in high Na+ diet patients |
[135] |
| C57BL/6J mice | 50 | Na+-rich diet | Increase in murine Th17 and Th1 cells Increase in IL-17A and IFN-γ secretion |
[144] |
| C57BL6/J mice and SJL/JCrHsd mice | – | High-salt diet | Exacerbation of disease in M and F of C57BL6/J mice but only in F of SJL/JCrHsd mice No influence on C57BL6/J mice carrying a 129/Sv-derived interval on chromosome 17 No influence on Th17 or Th1 cells Increase in blood–brain barrier permeability and brain pathologies |
[145] |
| Foxp3-GFP reporter mice | 21 | Na+-rich diet | Induction of Th1-type phenotype Impairement in Treg function (IFNγ-dependent) |
[147] |
| Healthy human | 205 | Dietary NaCl reduction | Decrease in monocytes counts Decrease in IL-6 (30%), IL-23 (90%) and IL-17 concentration Increase in IL-10 level (threefold) Slightly decrease in VEGF-C serum concentration |
|
| Healthy human | 17 | High-to-low NaCl diet | Increase in CD14++ and CD16+ monocytes proliferation Increase in intracellular ROS production |
EAE experimental autoimmune encephalomyelitis, PBMC peripheral blood mononuclear cells, ROS reactive oxygen species
In conclusion, recent reports have demonstrated a potential pro-inflammatory role of excess sodium chloride intake in the pathogenesis of autoimmune and neurodegenerative diseases, both in vitro and in vivo, although the outcomes of these studies are not unanimous. Nevertheless, the current knowledge suggests that a low-salt diet (<5 g/day) might be beneficial in the prevention and treatment of autoimmune diseases, including MS.
Compliance with ethical standards
Conflict of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Moghadasi AN, Pourmand S, Sharifian M, et al. Behavioral neurology of multiple sclerosis and autoimmune encephalopathies. Neurol Clin. 2016;34(1):17–31. doi: 10.1016/j.ncl.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Mandia D, Ferraro OE, Nosari G, et al. Environmental factors and multiple sclerosis severity: a descriptive study. Int J Environ Res Public Health. 2014;11(6):6417–6432. doi: 10.3390/ijerph110606417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ascherio A, Munger KL, Lennette ET, et al. Epstein-Barr virus antibodies and risk of multiple sclerosis: a prospective study. JAMA. 2001;286(24):3083–3088. doi: 10.1001/jama.286.24.3083. [DOI] [PubMed] [Google Scholar]
- 4.Farrell RA, Antony D, Wall GR, et al. Humoral immune response to EBV in multiple sclerosis is associated with disease activity on MRI. Neurology. 2009;73(1):32–38. doi: 10.1212/WNL.0b013e3181aa29fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramroodi N, Niazi AA, Sanadgol N, et al. Evaluation of reactive Epstein-Barr Virus (EBV) in Iranian patient with different subtypes of multiple sclerosis (MS) Braz J Infect Dis. 2013;17(2):156–163. doi: 10.1016/j.bjid.2012.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierrot-Deseilligny C. Clinical implications of a possible role of vitamin D in multiple sclerosis. J Neurol. 2009;256(9):1468–1479. doi: 10.1007/s00415-009-5139-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cline J. Calcium and vitamin d metabolism, deficiency, and excess. Top Companion Anim Med. 2012;27(4):159–164. doi: 10.1053/j.tcam.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Holmøy T, Torkildsen Ø, Myhr KM, et al. Vitamin D supplementation and monitoring in multiple sclerosis: who, when and wherefore. Acta Neurol Scand Suppl. 2012;195:63–69. doi: 10.1111/ane.12028. [DOI] [PubMed] [Google Scholar]
- 9.Steffensen LH, Brustad M, Kampman MT. What is needed to keep persons with multiple sclerosis vitamin D-sufficient throughout the year? J Neurol. 2013;260(1):182–188. doi: 10.1007/s00415-012-6611-6. [DOI] [PubMed] [Google Scholar]
- 10.Kampman MT, Steffensen LH, Mellgren SI, et al. Effect of vitamin D3 supplementation on relapses, disease progression, and measures of function in persons with multiple sclerosis: exploratory outcomes from a double-blind randomised controlled trial. Mult Scler. 2012;18(8):1144–1151. doi: 10.1177/1352458511434607. [DOI] [PubMed] [Google Scholar]
- 11.Stein MS, Liu Y, Gray OM, et al. A randomized trial of high-dose vitamin D2 in relapsing-remitting multiple sclerosis. Neurology. 2011;77(17):1611–1618. doi: 10.1212/WNL.0b013e3182343274. [DOI] [PubMed] [Google Scholar]
- 12.Hedström AK, Olsson T, Alfredsson L. Smoking is a major preventable risk factor for multiple sclerosis. Mult Scler. 2016;22(8):1021–1026. doi: 10.1177/1352458515609794. [DOI] [PubMed] [Google Scholar]
- 13.Ramanujam R, Hedström AK, Manouchehrinia A, et al. Effect of smoking cessation on multiple sclerosis prognosis. JAMA Neurol. 2015;72(10):1117–1123. doi: 10.1001/jamaneurol.2015.1788. [DOI] [PubMed] [Google Scholar]
- 14.Kvistad SS, Myhr KM, Holmøy T, et al. Body mass index influence interferon-betatreatment response in multiple sclerosis. J Neuroimmunol. 2015;288:92–97. doi: 10.1016/j.jneuroim.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Sloka S, Silva C, Pryse-Phillips W, et al. A quantitative analysis of suspected environmental causes of MS. Can J Neurol Sci. 2011;38(1):98–105. doi: 10.1017/s0317167100011124. [DOI] [PubMed] [Google Scholar]
- 16.Bäärnhielm M, Hedström AK, Kockum I, et al. Sunlight is associated with decreased multiple sclerosis risk: no interaction with human leukocyte antigen-DRB1*15. Eur J Neurol. 2012;19(7):955–962. doi: 10.1111/j.1468-1331.2011.03650.x. [DOI] [PubMed] [Google Scholar]
- 17.Marrie RA. Environmental risk factors in multiple sclerosis aetiology. Lancet Neurol. 2004;3(12):709–718. doi: 10.1016/S1474-4422(04)00933-0. [DOI] [PubMed] [Google Scholar]
- 18.Pugliatti M, Sotgiu S, Rosati G. The worldwide prevalence of multiple sclerosis. Clin Neurol Neurosurg. 2002;104(3):182–191. doi: 10.1016/s0303-8467(02)00036-7. [DOI] [PubMed] [Google Scholar]
- 19.Munger KL, Levin LI, O’Reilly EJ, et al. Anti-Epstein-Barr virus antibodies as serological markers of multiple sclerosis: a prospective study among United States military personnel. Mult Scler. 2011;17(10):1185–1193. doi: 10.1177/1352458511408991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Villoslada P, Juste C, Tintore M, et al. The immune response against herpesvirus is more prominent in the early stages of MS. Neurology. 2003;60(12):1944–1948. doi: 10.1212/01.wnl.0000069461.53733.f7. [DOI] [PubMed] [Google Scholar]
- 21.Yea C, Tellier R, Chong P, et al. Canadian pediatric demyelinating disease network. Epstein-Barr virus in oral shedding of children with multiple sclerosis. Neurology. 2013;81(16):1392–1399. doi: 10.1212/WNL.0b013e3182a841e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buljevac D, Flach HZ, Hop WC, et al. Prospective study on the relationship between infections and multiple sclerosis exacerbations. Brain. 2002;125(Pt5):952–960. doi: 10.1093/brain/awf098. [DOI] [PubMed] [Google Scholar]
- 23.Versini M, Jeandel PY, Rosenthal E, et al. Obesity in autoimmune diseases: not a passive bystander. Autoimmun Rev. 2014;13(9):981–1000. doi: 10.1016/j.autrev.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Cao H. Adipocytokines in obesity and metabolic disease. J Endocrinol. 2014;220(2):T47–T59. doi: 10.1530/JOE-13-0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oliveira SR, Simão AN, Kallaur AP, et al. Disability in patients with multiple sclerosis: influence of insulin resistance, adiposity, and oxidative stress. Nutrition. 2014;30(3):268–273. doi: 10.1016/j.nut.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Simpson S, Jr, Blizzard L, Otahal P, et al. Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82(10):1132–1141. doi: 10.1136/jnnp.2011.240432. [DOI] [PubMed] [Google Scholar]
- 27.Harbo HF, Utsi E, Lorentzen AR, et al. Low frequency of the disease-associated DRB1*15-DQB1*06 haplotype may contribute to the low prevalence of multiple sclerosis in Sami. Tissue Antigens. 2007;69(4):299–304. doi: 10.1111/j.1399-0039.2007.00803.x. [DOI] [PubMed] [Google Scholar]
- 28.Kingwell E, Marriott JJ, Jetté N, et al. Incidence and prevalence of multiple sclerosis in Europe: a systematic review. BMC Neurol. 2013;13:128. doi: 10.1186/1471-2377-13-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kantarci O, Wingerchuk D. Epidemiology and natural history of multiple sclerosis: new insights. Curr Opin Neurol. 2006;19(3):248–254. doi: 10.1097/01.wco.0000227033.47458.82. [DOI] [PubMed] [Google Scholar]
- 30.Coo H, Aronson KJ. A systematic review of several potential non-genetic risk factors for multiple sclerosis. Neuroepidemiology. 2004;23(1–2):1–12. doi: 10.1159/000073969. [DOI] [PubMed] [Google Scholar]
- 31.Smolders J, Damoiseaux J, Menheere P, et al. Vitamin D as an immune modulator in multiple sclerosis, a review. J Neuroimmunol. 2008;194(1–2):7–17. doi: 10.1016/j.jneuroim.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Pantzaris MC, Loukaides GN, Ntzani EE, et al. A novel oral nutraceutical formula of omega-3 and omega-6 fatty acids with vitamins (PLP10) in relapsing remitting multiple sclerosis: a randomised, double-blind, placebo-controlled proof-of-concept clinical trial. BMJ Open. 2013;3(4):e002170. doi: 10.1136/bmjopen-2012-002170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torkildsen O, Wergeland S, Bakke S, et al. ω-3 fatty acid treatment in multiple sclerosis (OFAMS Study): a randomized, double-blind, placebo-controlled trial. Arch Neurol. 2012;69(8):1044–1051. doi: 10.1001/archneurol.2012.283. [DOI] [PubMed] [Google Scholar]
- 34.Khalili M, Azimi A, Izadi V, et al. Does lipoic acid consumption affect the cytokine profile in multiple sclerosis patients: a double-blind, placebo-controlled, randomized clinical trial. Neuroimmunomodulation. 2014;21(6):291–296. doi: 10.1159/000356145. [DOI] [PubMed] [Google Scholar]
- 35.Vergelli M, Olivotto J, Castigli E, et al. Immunosuppressive activity of 13-cis-retinoic acid in rats: aspects of pharmacokinetics and pharmacodynamics. Immunopharmacology. 1997;37(2–3):191–197. doi: 10.1016/s0162-3109(97)00048-9. [DOI] [PubMed] [Google Scholar]
- 36.Hall JA, Grainger JR, Spencer SP, et al. The role of retinoic acid in tolerance and immunity. Immunity. 2011;35(1):13–22. doi: 10.1016/j.immuni.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bitarafan S, Saboor-Yaraghi A, Sahraian MA, et al. Effect of vitamin A supplementation on fatigue and depression in multiple sclerosis patients: a double-blind placebo-controlled clinical trial. Iran J Allergy Asthma Immunol. 2016;15(1):13–19. [PubMed] [Google Scholar]
- 38.Storoni M, Plant GT. The therapeutic potential of the ketogenic diet in treating progressive multiple sclerosis. Mult Scler Int. 2015;2015:681289. doi: 10.1155/2015/681289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Allen BG, Bhatia SK, Anderson CM, et al. Ketogenic diets as an adjuvant cancer therapy: history and potential mechanism. Redox Biol. 2014;2:963–970. doi: 10.1016/j.redox.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim do Y, Hao J, Liu R, et al. Inflammation-mediated memory dysfunction and effects of a ketogenic diet in a murine model of multiple sclerosis. PLoS One. 2012;7(5):e35476. doi: 10.1371/journal.pone.0035476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malin SK, Cotugna N, Fang CS. Effect of creatine supplementation on muscle capacity in individuals with multiple sclerosis. J Diet Suppl. 2008;5(1):20–32. doi: 10.1080/19390210802328974. [DOI] [PubMed] [Google Scholar]
- 42.Swank RL, Goodwin J. Review of MS patient survival on a Swank low saturated fat diet. Nutrition. 2003;19(2):161–162. doi: 10.1016/s0899-9007(02)00851-1. [DOI] [PubMed] [Google Scholar]
- 43.Riccio P, Rossano R. Nutrition facts in multiple sclerosis. ASN Neuro. 2015;7(1):1759091414568185. doi: 10.1177/1759091414568185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Plemel JR, Juzwik CA, Benson CA, et al. Over-the-counter anti-oxidant therapies for use in multiple sclerosis: a systematic review. Mult Scler. 2015;21(12):1485–1495. doi: 10.1177/1352458515601513. [DOI] [PubMed] [Google Scholar]
- 45.Abdolahi M, Yavari P, Honarvar NM, et al. Molecular mechanisms of the action of vitamin A in Th17/Treg axis in multiple sclerosis. J Mol Neurosci. 2015;57(4):605–613. doi: 10.1007/s12031-015-0643-1. [DOI] [PubMed] [Google Scholar]
- 46.Bitarafan S, Saboor-Yaraghi A, Sahraian MA, et al. Impact of vitamin A supplementation on disease progression in patients with multiple sclerosis. Arch Iran Med. 2015;18(7):435–440. [PubMed] [Google Scholar]
- 47.Hille B. Ionic channels in excitable membranes. Current problems and biophysical approaches. Biophys J. 1978;22(2):283–294. doi: 10.1016/S0006-3495(78)85489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hodgkin AL, Huxley AF. A quantitative description of membrane current and its application to conduction and excitation in nerve. J Physiol. 1952;117:500–544. doi: 10.1113/jphysiol.1952.sp004764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barres BA, Chun LL, Corey DP. Ion channels in vertebrate glia. Annu Rev Neurosci. 1990;13:441–474. doi: 10.1146/annurev.ne.13.030190.002301. [DOI] [PubMed] [Google Scholar]
- 50.Gautron S, Dos Santos G, Pinto-Henrique D, et al. The glial voltage-gated sodium channel: cell- and tissue-specific mRNA expression. Proc Natl Acad Sci USA. 1992;89(15):7272–7276. doi: 10.1073/pnas.89.15.7272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gosling M, Harley SL, Turner RJ, et al. Human saphenous vein endothelial cells express a tetrodotoxin-resistant, voltage-gated sodium current. J Biol Chem. 1998;273(33):21084–21090. doi: 10.1074/jbc.273.33.21084. [DOI] [PubMed] [Google Scholar]
- 52.Diss JK, Fraser SP, Djamgoz MB. Voltage-gated Na+ channels: multiplicity of expression, plasticity, functional implications and pathophysiological aspects. Eur Biophys J. 2004;33(3):180–193. doi: 10.1007/s00249-004-0389-0. [DOI] [PubMed] [Google Scholar]
- 53.Káradóttir R, Hamilton NB, Bakiri Y, et al. Spiking and nonspiking classes of oligodendrocyte precursor glia in CNS white matter. Nat Neurosci. 2008;11(4):450–456. doi: 10.1038/nn2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao P, Barr TP, Hou Q, et al. Voltage-gated sodium channel expression in rat and human epidermal keratinocytes: evidence for a role in pain. Pain. 2008;139(1):90–105. doi: 10.1016/j.pain.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 55.Lopez-Santiago LF, Meadows LS, Ernst SJ, et al. Sodium channel Scn1b null mice exhibit prolonged QT and RR intervals. J Mol Cell Cardiol. 2007;43:636–647. doi: 10.1016/j.yjmcc.2007.07.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wallace RH, Wang DW, Singh R, et al. Febrile seizures and generalized epilepsy associated with a mutation in the Na+-channel beta1 subunit gene SCN1B. Nat Genet. 1998;19:366–370. doi: 10.1038/1252. [DOI] [PubMed] [Google Scholar]
- 57.Audenaert D, Claes L, Ceulemans B, et al. A deletion in SCN1B is associated with febrile seizures and early-onset absence epilepsy. Neurology. 2003;61:854–856. doi: 10.1212/01.wnl.0000080362.55784.1c. [DOI] [PubMed] [Google Scholar]
- 58.Scheffer IE, Harkin LA, Grinton BE, et al. Temporal lobe epilepsy and GEFS+ phenotypes associated with SCN1B mutations. Brain. 2007;130(Pt 1):100–109. doi: 10.1093/brain/awl272. [DOI] [PubMed] [Google Scholar]
- 59.Lopez-Santiago LF, Pertin M, Morisod X, et al. Sodium channel beta2 subunits regulate tetrodotoxin-sensitive sodium channels in small dorsal root ganglion neurons and modulate the response to pain. J Neurosci. 2006;26:7984–7994. doi: 10.1523/JNEUROSCI.2211-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cummins TR, Sheets PL, Waxman SG. The roles of sodium channels in nociception: implications for mechanisms of pain. Pain. 2007;131:243–257. doi: 10.1016/j.pain.2007.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fontaine B, Khurana TS, Hoffman EP, et al. Hyperkalemic periodic paralysis and the adult muscle sodium channel alpha-subunit gene. Science. 1990;250:1000–1002. doi: 10.1126/science.2173143. [DOI] [PubMed] [Google Scholar]
- 62.Waxman SG. Channel, neuronal and clinical function in sodium channelopathies: from genotype to phenotype. Nat Neurosci. 2007;10:405–409. doi: 10.1038/nn1857. [DOI] [PubMed] [Google Scholar]
- 63.Dichgans M, Freilinger T, Eckstein G, et al. Mutation in the neuronal voltage-gated sodium channel SCN1A in familial hemiplegic migraine. Lancet. 2005;366:371–377. doi: 10.1016/S0140-6736(05)66786-4. [DOI] [PubMed] [Google Scholar]
- 64.Waxman SG. Axonal conduction and injury in multiple sclerosis: the role of sodium channels. Nat Rev Neurosci. 2006;7:932–941. doi: 10.1038/nrn2023. [DOI] [PubMed] [Google Scholar]
- 65.Fraser SP, Diss JK, Chioni AM, et al. Voltage-gated sodium channel expression and potentiation of human breast cancer metastasis. Clin Cancer Res. 2005;11:5381–5389. doi: 10.1158/1078-0432.CCR-05-0327. [DOI] [PubMed] [Google Scholar]
- 66.Brackenbury WJ, Isom LL. Voltage-gated Na+ channels: potential for beta subunits as therapeutic targets. Expert Opin Ther Targets. 2008;12(9):1191–1203. doi: 10.1517/14728222.12.9.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brackenbury WJ, Djamgoz MB, Isom LL. An emerging role for voltage-gated Na+ channels in cellular migration: regulation of central nervous system development and potentiation of invasive cancers. Neuroscientist. 2008;14(6):571–583. doi: 10.1177/1073858408320293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Roy ML, Narahashi T. Differential properties of tetrodotoxin-sensitive and tetrodotoxin-resistant sodium channels in rat dorsal root ganglion neurons. J Neurosci. 1992;12(6):2104–2111. doi: 10.1523/JNEUROSCI.12-06-02104.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ikeda SR, Schofield GG, Weight FF. Na+ and Ca2+ currents of acutely isolated adult rat nodose ganglion cells. J Neurophysiol. 1986;55(3):527–539. doi: 10.1152/jn.1986.55.3.527. [DOI] [PubMed] [Google Scholar]
- 70.Sun LH, Yan ML, Hu XL, et al. MicroRNA-9 induces defective trafficking of Nav1.1 and Nav1.2 by targeting Navβ2 protein coding region in rat with chronic brain hypoperfusion. Mol Neurodegener. 2015;10:36. doi: 10.1186/s13024-015-0032-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ogiwara I, Miyamoto H, Morita N, et al. Nav1.1 localizes to axons of parvalbumin-positive inhibitory interneurons: a circuit basis for epileptic seizures in mice carrying an Scn1a gene mutation. J Neurosci. 2007;27(22):5903–5914. doi: 10.1523/JNEUROSCI.5270-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Catterall WA, Kalume F, Oakley JC. NaV1.1 channels and epilepsy. J Physiol. 2010;588(Pt 11):1849–1859. doi: 10.1113/jphysiol.2010.187484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Howell KB, McMahon JM, Carvill GL, et al. SCN2A encephalopathy: a major cause of epilepsy of infancy with migrating focal seizures. Neurology. 2015;85(11):958–966. doi: 10.1212/WNL.0000000000001926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gazina EV, Leaw BT, Richards KL, et al. ‘Neonatal’ Nav1.2 reduces neuronal excitability and affects seizure susceptibility and behaviour. Hum Mol Genet. 2015;24(5):1457–1468. doi: 10.1093/hmg/ddu562. [DOI] [PubMed] [Google Scholar]
- 75.Dhalla AK, Yang M, Ning Y, et al. Blockade of Na+channels in pancreatic α-cells has antidiabetic effects. Diabetes. 2014;63(10):3545–3556. doi: 10.2337/db13-1562. [DOI] [PubMed] [Google Scholar]
- 76.Lin CR, Chen KH, Yang CH, et al. Intrathecal miR-183 delivery suppresses mechanical allodynia in mononeuropathic rats. Eur J Neurosci. 2014;39(10):1682–1689. doi: 10.1111/ejn.12522. [DOI] [PubMed] [Google Scholar]
- 77.Tan AM, Samad OA, Dib-Hajj SD, et al. Virus-mediated knockdown of Nav1.3 in dorsal root ganglia of STZ-induced diabetic rats alleviates tactile allodynia. Mol Med. 2015;21:544–552. doi: 10.2119/molmed.2015.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zang Y, He XH, Xin WJ, et al. Inhibition of NF-kappaB prevents mechanical allodynia induced by spinal ventral root transection and suppresses the re-expression of Nav1.3 in DRG neurons in vivo and in vitro. Brain Res. 2010;1363:151–158. doi: 10.1016/j.brainres.2010.09.048. [DOI] [PubMed] [Google Scholar]
- 79.Bissay V, Van Malderen SC, Keymolen K, et al. SCN4A variants and Brugada syndrome: phenotypic and genotypic overlap between cardiac and skeletal muscle sodium channelopathies. Eur J Hum Genet. 2016;24(3):400–407. doi: 10.1038/ejhg.2015.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cannon SC. Channelopathies of skeletal muscle excitability. Compr Physiol. 2015;5(2):761–790. doi: 10.1002/cphy.c140062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nelson M, Yang M, Millican-Slater R, et al. Nav1.5 regulates breast tumor growth and metastatic dissemination in vivo. Oncotarget. 2015;6(32):32914–32929. doi: 10.18632/oncotarget.5441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mohammed FH, Khajah MA, Yang M, et al. Blockade of voltage-gated sodium channels inhibits invasion of endocrine-resistant breast cancer cells. Int J Oncol. 2016;48(1):73–83. doi: 10.3892/ijo.2015.3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Musa H, Kline CF, Sturm AC, et al. SCN5A variant that blocks fibroblast growth factor homologous factor regulation causes human arrhythmia. Proc Natl Acad Sci USA. 2015;112(40):12528–12533. doi: 10.1073/pnas.1516430112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tan BY, Yong RY, Barajas-Martinez H, et al. A Brugada syndrome proband with compound heterozygote SCN5A mutations identified from a Chinese family in Singapore. Europace. 2016;18(6):897–904. doi: 10.1093/europace/euv058. [DOI] [PubMed] [Google Scholar]
- 85.Andrikopoulos P, Fraser SP, Patterson L, et al. Angiogenic functions of voltage-gated Na+ channels in human endothelial cells: modulation of vascular endothelial growth factor (VEGF) signaling. J Biol Chem. 2011;286(19):16846–16860. doi: 10.1074/jbc.M110.187559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.O’Brien JE, Meisler MH. Sodium channel SCN8A (Nav1.6): properties and de novo mutations in epileptic encephalopathy and intellectual disability. Front Genet. 2013;4:213. doi: 10.3389/fgene.2013.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hernandez-Plata E, Ortiz CS, Marquina-Castillo B, et al. Overexpression of NaV 1.6 channels is associated with the invasion capacity of human cervical cancer. Int J Cancer. 2012;130(9):2013–2023. doi: 10.1002/ijc.26210. [DOI] [PubMed] [Google Scholar]
- 88.Fertleman CR, Ferrie CD, Aicardi J, et al. Paroxysmal extreme pain disorder (previously familial rectal pain syndrome) Neurology. 2007;69(6):586–595. doi: 10.1212/01.wnl.0000268065.16865.5f. [DOI] [PubMed] [Google Scholar]
- 89.Suy S, Hansen TP, Auto HD et al. (2012) Expression of voltage-gated sodium channel Na(v)1.8 in human prostate cancer is associated with high histological grade. J Clin Exp Oncol. doi:10.4172/2324-9110.1000102 [DOI] [PMC free article] [PubMed]
- 90.Han C, Huang J, Waxman SG. Sodium channel Nav1.8: emerging links to human disease. Neurology. 2016;86(5):473–483. doi: 10.1212/WNL.0000000000002333. [DOI] [PubMed] [Google Scholar]
- 91.Roostaei T, Sadaghiani S, Park MT, et al. Channelopathy-related SCN10A gene variants predict cerebellar dysfunction in multiple sclerosis. Neurology. 2016;86(5):410–417. doi: 10.1212/WNL.0000000000002326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Woods CG, Babiker MO, Horrocks I, et al. The phenotype of congenital insensitivity to pain due to the NaV1.9 variant p. L811P. Eur J Hum Genet. 2015;23(10):1434. doi: 10.1038/ejhg.2015.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Leipold E, Hanson-Kahn A, Frick M, et al. Cold-aggravated pain in humans caused by a hyperactive NaV1.9 channel mutant. Nat Commun. 2015;6:10049. doi: 10.1038/ncomms10049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xu W, Hong SJ, Zhong A, et al. Sodium channel Nax is a regulator in epithelial sodium homeostasis. Sci Transl Med. 2015;7(312):312ra177. doi: 10.1126/scitranslmed.aad0286. [DOI] [PubMed] [Google Scholar]
- 95.Noda M, Hiyama TY. Sodium sensing in the brain. Pflug Arch. 2015;467(3):465–474. doi: 10.1007/s00424-014-1662-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Scheffer IE, Harkin LA, Grinton BE, et al. Temporal lobe epilepsy and GEFS+ phenotypes associated with SCN1B mutations. Brain. 2007;130(Pt 1):100–109. doi: 10.1093/brain/awl272. [DOI] [PubMed] [Google Scholar]
- 97.Watanabe H, Darbar D, Kaiser DW, et al. Mutations in sodium channel beta1- and beta2-subunits associated with atrial fibrillation. Circ Arrhythm Electrophysiol. 2009;2:268–275. doi: 10.1161/CIRCEP.108.779181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Roger S, Rollin J, Barascu A, et al. Voltage-gated sodium channels potentiate the invasive capacities of human non-small-cell lung cancer cell lines. Int J Biochem Cell Biol. 2007;39:774–786. doi: 10.1016/j.biocel.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 99.O’Malley HA, Shreiner AB, Chen GH, et al. Loss of Na+ channel beta2 subunits is neuroprotective in a mouse model of multiple sclerosis. Mol Cell Neurosci. 2009;40(2):143–155. doi: 10.1016/j.mcn.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Oyama F, Miyazaki H, Sakamoto N, et al. Sodium channel beta4 subunit: down-regulation and possible involvement in neuritic degeneration in Huntington’s disease transgenic mice. J Neurochem. 2006;98(2):518–529. doi: 10.1111/j.1471-4159.2006.03893.x. [DOI] [PubMed] [Google Scholar]
- 101.Isom LL, De Jongh KS, Patton DE, et al. Primary structure and functional expression of the beta 1 subunit of the rat brain sodium channel. Science. 1992;256(5058):839–842. doi: 10.1126/science.1375395. [DOI] [PubMed] [Google Scholar]
- 102.Isom LL, Ragsdale DS, De Jongh KS, et al. Structure and function of the beta 2 subunit of brain sodium channels, a transmembrane glycoprotein with a CAM motif. Cell. 1995;83(3):433–442. doi: 10.1016/0092-8674(95)90121-3. [DOI] [PubMed] [Google Scholar]
- 103.Morgan K, Stevens EB, Shah B, et al. beta 3: an additional auxiliary subunit of the voltage-sensitive sodium channel that modulates channel gating with distinct kinetics. Proc Natl Acad Sci USA. 2003;97(5):2308–2313. doi: 10.1073/pnas.030362197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yu FH, Westenbroek RE, Silos-Santiago I, et al. Sodium channel beta4, a new disulfide-linked auxiliary subunit with similarity to beta2. J Neurosci. 2003;23(20):7577–7585. doi: 10.1523/JNEUROSCI.23-20-07577.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Black JA, Westenbroek R, Ransom BR, et al. Type II sodium channels in spinal cord astrocytes in situ: immunocytochemical observations. Glia. 1994;12:219–227. doi: 10.1002/glia.440120307. [DOI] [PubMed] [Google Scholar]
- 106.Reese KA, Caldwell JH. Immunocytochemical localization of NaCh6 in cultured spinal cord astrocytes. Glia. 1999;26:92–96. doi: 10.1002/(sici)1098-1136(199903)26:1<92::aid-glia10>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 107.Black JA, Dib-Hajj S, Cohen S, et al. Glial cells have heart: rH1 Na+ channel mRNA and protein in spinal cord astrocytes. Glia. 1998;23:200–208. [PubMed] [Google Scholar]
- 108.Barres BA, Chun LL, Corey DP. Glial and neuronal forms of the voltage-dependent sodium channel: characteristics and cell-type distribution. Neuron. 1989;2:1375–1388. doi: 10.1016/0896-6273(89)90076-7. [DOI] [PubMed] [Google Scholar]
- 109.Herzog RI, Liu C, Waxman SG, et al. Calmodulin binds to the C terminus of sodium channels Nav1.4 and Nav1.6 and differentially modulates their functional properties. J Neurosci. 2003;23:8261–8270. doi: 10.1523/JNEUROSCI.23-23-08261.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kapoor R. Sodium channel blockers and neuroprotection in multiple sclerosis using lamotrigine. J Neurolog Sci. 2008;274(1–2):54–56. doi: 10.1016/j.jns.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 111.Nikolaeva MA, Mukherjee B, Stys PK. Na+-dependent sources of intra-axonal Ca2+ release in rat optic nerve during in vitro chemical ischemia. J Neurosci. 2005;25:9960–9967. doi: 10.1523/JNEUROSCI.2003-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Waxman SG. Mechanisms of disease: sodium channels and neuroprotection in multiple sclerosis current status. Nat Clin Pract Neurol. 2008;4(3):159–169. doi: 10.1038/ncpneuro0735. [DOI] [PubMed] [Google Scholar]
- 113.Pappalardo LW, Samad OA, Black JA, et al. Voltage-gated sodium channel Nav 1.5 contributes to astrogliosis in an in vitro model of glial injury via reverse Na+/Ca2+ exchange. Glia. 2014;62(7):1162–1175. doi: 10.1002/glia.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bechtold DA, Kapoor R, Smith KJ. Axonal protection using flecainide in experimental autoimmune encephalomyelitis. Ann Neurol. 2004;55(5):607–616. doi: 10.1002/ana.20045. [DOI] [PubMed] [Google Scholar]
- 115.Morsali D, Bechtold D, Lee W, et al. Safinamide and flecainide protect axons and reduce microglial activation in models of multiple sclerosis. Brain. 2013;136(Pt 4):1067–1082. doi: 10.1093/brain/awt041. [DOI] [PubMed] [Google Scholar]
- 116.Lo AC, Black JA, Waxman SG. Neuroprotection of axons with phenytoin in experimental allergic encephalomyelitis. Neuroreport. 2002;13:1909–1912. doi: 10.1097/00001756-200210280-00015. [DOI] [PubMed] [Google Scholar]
- 117.Bechtold DA, Miller SJ, Dawson AC, et al. Axonal protection achieved in a model of multiple sclerosis using lamotrigine. J Neurol. 2006;253:1542–1551. doi: 10.1007/s00415-006-0204-1. [DOI] [PubMed] [Google Scholar]
- 118.Craner MJ, Damarjian TG, Liu S, et al. Sodium channels contribute to microglia/macrophage activation and function in EAE and MS. Glia. 2005;49(2):220–229. doi: 10.1002/glia.20112. [DOI] [PubMed] [Google Scholar]
- 119.Counihan TJ, Duignan JA, Gormley G, et al. Does long-term partial sodium channel blockade alter disease progression in MS? Evidence from a retrospective study. Ir J Med Sci. 2014;183(1):117–121. doi: 10.1007/s11845-013-1042-7. [DOI] [PubMed] [Google Scholar]
- 120.Gnanapavan S, Grant D, Morant S, et al. Biomarker report from the phase II lamotrigine trial in secondary progressive MS- neurofilament as a surrogate of disease progression. PLoS One. 2013;8(8):e70019. doi: 10.1371/journal.pone.0070019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kapoor R, Furby J, Hayton T, et al. Lamotrigine for neuroprotection in secondary progressive multiple sclerosis: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Neurol. 2010;9(7):681–688. doi: 10.1016/S1474-4422(10)70131-9. [DOI] [PubMed] [Google Scholar]
- 122.Kleinewietfeld M, Manzel A, Titze J, et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013;496(7446):518–522. doi: 10.1038/nature11868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.McGuire S (2010) Institute of Medicine. 2010. Strategies to reduce sodium intake in the United States. The National Academies Press, Washington. Adv Nutr 1:49–50 [DOI] [PMC free article] [PubMed]
- 124.Appel LJ, Frohlich ED, Hall JE, et al. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation. 2011;123:1138–1143. doi: 10.1161/CIR.0b013e31820d0793. [DOI] [PubMed] [Google Scholar]
- 125.Brown IJ, Tzoulaki I, Candeias V, et al. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38:791–813. doi: 10.1093/ije/dyp139. [DOI] [PubMed] [Google Scholar]
- 126.Junger WG, Liu FC, Loomis WH, et al. Hypertonic saline enhances cellular immune function. Circ Shock. 1994;42:190–196. [PubMed] [Google Scholar]
- 127.Machnik A, Neuhofer W, Jantsch, et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat Med. 2009;15(5):545–552. doi: 10.1038/nm.1960. [DOI] [PubMed] [Google Scholar]
- 128.Korn T, Bettelli E, Oukka M, et al. IL-17 and Th17 Cells. Annu Rev Immunol. 2009;27:485–517. doi: 10.1146/annurev.immunol.021908.132710. [DOI] [PubMed] [Google Scholar]
- 129.Ghoreschi K, Laurence A, Yang XP, et al. Generation of pathogenic T(H)17 cells in the absence of TGF-beta signalling. Nature. 2010;467:967–971. doi: 10.1038/nature09447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wu C, Yosef N, Thalhamer T, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013;496(7446):513–517. doi: 10.1038/nature11984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Codarri L, Gyülvészi G, Tosevski V, et al. RORgammat drives production of the cytokine GM-CSF in helper T cells, which is essential for the effector phase of autoimmune neuroinflammation. Nat Immunol. 2011;12:560–567. doi: 10.1038/ni.2027. [DOI] [PubMed] [Google Scholar]
- 132.El-Behi M, Ciric B, Dai H, et al. The encephalitogenicity of T(H)17 cells is dependent on IL-1- and IL-23-induced production of the cytokine GM-CSF. Nat Immunol. 2011;12:568–575. doi: 10.1038/ni.2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Reboldi A, Coisne C, Baumjohann D, et al. C-C chemokine receptor 6-regulated entry of TH-17 cells into the CNS through the choroid plexus is required for the initiation of EAE. Nat Immunol. 2009;10:514–523. doi: 10.1038/ni.1716. [DOI] [PubMed] [Google Scholar]
- 134.Go WY, Liu X, Roti MA, et al. NFAT5/TonEBP mutant mice define osmotic stress as acritical feature of the lymphoid microenvironment. Proc Natl Acad Sci USA. 2004;101:10673–10678. doi: 10.1073/pnas.0403139101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Farez MF, Fiol MP, Gaitán MI, et al. Sodium intake is associated with increased disease activity in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2015;86(1):26–31. doi: 10.1136/jnnp-2014-307928. [DOI] [PubMed] [Google Scholar]
- 136.Fulgoni VL., 3rd Limitations of data on fluid intake. J Am Coll Nutr. 2007;26(5 Suppl):588S–591S. doi: 10.1080/07315724.2007.10719663. [DOI] [PubMed] [Google Scholar]
- 137.Han MH, Hwang SI, Roy DB, et al. Proteomic analysis of active multiple sclerosis lesions reveals therapeutic targets. Nature. 2008;451(7182):1076–1081. doi: 10.1038/nature06559. [DOI] [PubMed] [Google Scholar]
- 138.Goodfriend TL, Elliott ME, Catt KJ. Angiotensin receptors and their antagonists. N Engl J Med. 1996;334:1649–1654. doi: 10.1056/NEJM199606203342507. [DOI] [PubMed] [Google Scholar]
- 139.Stegbauer J, Lee DH, Seubert S, et al. Role of the renin-angiotensin system in autoimmune inflammation of the central nervous system. Proc Natl Acad Sci USA. 2009;106:14942–14947. doi: 10.1073/pnas.0903602106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Maillard P, Seshadri S, Beiser A, et al. Effects of systolic blood pressure on white-matter integrity in young adults in the Framingham Heart Study: a cross-sectional study. Lancet Neurol. 2012;11:1039–1047. doi: 10.1016/S1474-4422(12)70241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Platten M, Youssef S, Hur EM, et al. Blocking angiotensin-converting enzyme induces potent regulatory T cells and modulates TH1- and TH17-mediated autoimmunity. Proc Natl Acad Sci USA. 2009;106(35):14948–14953. doi: 10.1073/pnas.0903958106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hucke S, Eschborn M, Liebmann M, et al. Sodium chloride promotes pro-inflammatory macrophage polarization thereby aggravating CNS autoimmunity. J Autoimmun. 2016;67:90–101. doi: 10.1016/j.jaut.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 143.Yi B, Titze J, Rykova M, et al. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: a longitudinal study. Transl Res. 2015;166(1):103–110. doi: 10.1016/j.trsl.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jörg S, Kissel J, Manzel A, et al. High salt drives Th17 responses in experimental autoimmune encephalomyelitis without impacting myeloid dendritic cells. Exp Neurol. 2016;279:212–222. doi: 10.1016/j.expneurol.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 145.Krementsov DN, Case LK, Hickey WF, et al. Exacerbation of autoimmune neuroinflammation by dietary sodium is genetically controlled and sex specific. FASEB J. 2015;29(8):3446–3457. doi: 10.1096/fj.15-272542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhou X, Zhang L, Ji WJ et al (2013) Variation in dietary salt intake induces coordinated dynamics of monocyte subsets and monocyte-platelet aggregates in humans: implications in end organ inflammation. In: Zirlik A (ed) PLoS One 8(4):e60332 [DOI] [PMC free article] [PubMed]
- 147.Hernandez AL, Kitz A, Wu C, et al. Sodium chloride inhibits the suppressive function of FOXP3+ regulatory T cells. J Clin Investig. 2015;125(11):4212–4222. doi: 10.1172/JCI81151. [DOI] [PMC free article] [PubMed] [Google Scholar]