Key Clinical Message
Although there are many causes of pain right lower abdomen, stump appendicitis should always strike a clinician in postappendectomy patients even if it is a rare diagnosis. Here, we are discussing a 35‐year female with stump appendicitis who underwent completion appendectomy.
Keywords: Acute appendicitis, completion appendectomy, stump appendicitis
Introduction
Acute appendicitis is the commonest surgical operation, and appendectomy forms a major bulk of the emergency surgery performed in the emergency room. Although stump appendicitis is a complication of appendectomy, it is rare, while wound infection, pelvic abscess, and adhesive bowel obstruction are more commonly seen among others. We clinicians do not consider stump appendicitis as a differential diagnosis when evaluating a patient with right lower abdomen pain who has undergone appendectomy in the past. Here, a 35‐year female with stump appendicitis is described, with a previous history of appendectomy.
Case History/Examination
A 35‐year female presented to our hospital with recurrent pain in right lower abdomen for 4 months which had increased in intensity in the last 24 h. She used to have on and off passage of altered blood in stool during previous attacks of pain but absent on this presentation. She had undergone open appendectomy four‐and‐half months back at another center. Her last pain episode was 1 month ago and was diagnosed as ileocolic intussusception and was managed conservatively, at another center without an adverse outcome.
On clinical examination, the patient was afebrile and her vital signs were otherwise normal. Physical examination revealed a tender mass in right iliac fossa of 3 × 2 cm2 without evidence of guarding, rebound tenderness, or other peritoneal signs. Routine laboratory studies were remarkable for a WBC count of 10,000/mm3 with 88% neutrophils. Urinalysis was negative.
An ultrasound of the abdomen and pelvis was performed which showed invagination of one bowel loop into another bowel loop with characteristic target sign which suggested the preoperative diagnosis of ileocolic intussusception. Exploratory laparotomy with a lower midline incision was performed under general anesthesia. The operative findings were adhered inflamed omentum forming a lump over the ileocecal junction with inflamed surrounding mesentery and acutely inflamed stump of appendix (~2 cm). Rest of the bowel was normal. As shown in Figures 1 and 2, completion appendectomy was performed and the postoperative period was uneventful, and on postoperative day 4, the patient was discharged. Her histopathological report showed acutely inflamed appendix, and she is asymptomatic till date.
Figure 1.
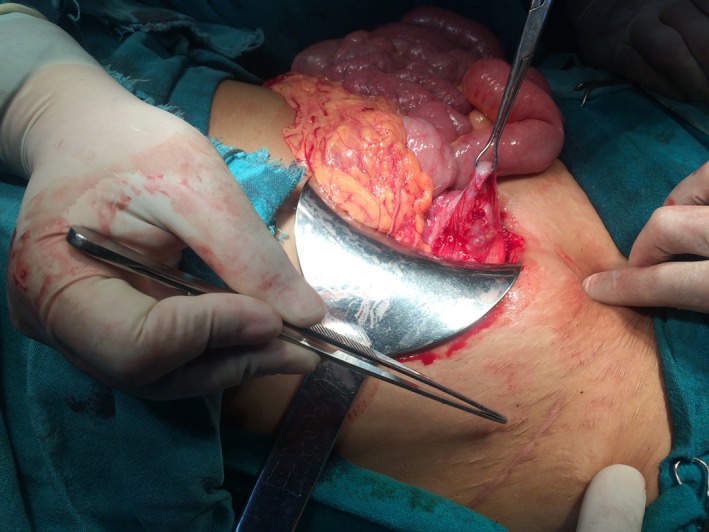
Operative finding showing stump appendicitis and the previous scar.
Figure 2.

Stump appendicitis with ileocecal junction in view.
Discussion
Acute appendicitis is the commonest abdominal surgical emergency encountered by a general surgeon 1. It is a clinical diagnosis, and the patient usually presents with periumbilical pain that radiates to the right lower abdomen 2. But then, it always poses a dilemma when a patient with a history of appendectomy presents with right iliac fossa pain.
The first appendectomy was performed in 1735 by Claudius Amyand, and in 1886, Reginald Fitz described the clinicopathological features, while Rose described stump appendicitis for the first time in 1945 3. There is a whole list of complications following appendectomy, the common ones being wound infection and pelvic abscesses 4.
Stump appendicitis is defined as a rare complication following appendectomy caused by inflammation of the residual portion of the appendix left behind. The clinical presentation of stump appendicitis is similar to that of acute appendicitis 5. Stump appendicitis has an incidence of one in 50,000 cases 6. Clinically, these patients have the symptoms and signs similar to appendicitis. Stump appendicitis poses a dilemma if the clinician is not aware of this uncommon presentation.
Stump appendicitis is associated with late diagnosis and therefore has higher rate of perforation with increased morbidity 7. The factors leading to stump appendicitis can be either anatomical or surgical. Anatomically, it can be retrocecal in position posing difficulty 8. While the surgical factors include inadequate identification of the base of appendix because of local inflammation, difficult dissection or leaving a long stump behind due to fear of injury to cecum 9. This can be seen in either open or laparoscopic approach 10, 11.
Generally, adequate visualization of the appendix base and the ileocecal region and a stump of <5 mm reduces the risk of stump appendicitis 12, 13. Although stump appendicitis is thought to be a recent phenomenon that is mainly seen in laparoscopically performed appendectomies 14, the literature shows that 66% of stump appendicitis occurred after open appendectomy 15.
A preoperative diagnosis can be made by USG and CT scan 16. However, USG is user dependent and a high suspicion for stump appendicitis is required. While CT scan is said to be superior to USG 17, but in a developing country like Nepal, CT scan is not readily available and relatively expensive to be done routinely. Also, laparoscopy has an important role in the diagnosis and has therapeutic value 18.
However, in our patient, stump appendicitis was an intraoperative diagnosis. We were misled by the previous history of appendectomy and USG finding of intussusception at this presentation. But intraoperatively, on finding omental lump over the ileocecal junction with an inflamed appendicular stump clenched the diagnosis of stump appendectomy. We then performed completion appendectomy, and the postoperative period was uneventful. The patient is asymptomatic since.
The treatment of choice is completion appendectomy, either open or laparoscopically 19. Sometimes ileocolic resection may be required depending on the clinical presentation and inflammation around ileocecal region 20.
Conclusion
Although stump appendicitis is a rare complication after appendectomy, either open or laparoscopically, a clinician should keep in mind this possibility as the cause of right lower abdomen pain in a patient with previous history of appendectomy because of the increased risk of perforation and misdiagnosis.
Authorship
TS and RKG: participated in study conception and design. TS: involved in acquisition of data. TS and RJK: analyzed and interpreted the data. TS, RKG, and CSA: drafted the manuscript. TS, RKG, and RJK: performed critical revision.
Conflict of Interest
None declared.
Acknowledgment
The abstract titled: Recurrent pain abdomen following appendectomy: stump appendicitis, a surgeon's dilemma by Tuhin Shah, Rakesh Gupta, Rikesh Jung Karkee, and Chandra Shekhar Agarwal has been published in the Abstract Journal for General Surgery, ANZ J. Surg. 2016; 86 (S1) 62.
References
- 1. Humes, DJ , J Simpson. 2006. Acute appendicitis. BMJ 333(7567):530–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kozol, R. A. , Farmer D. L., Tennenberg S. D., and Mulligan M.. 1999. Surgical pearls. FA Davis, Philadelphia. [Google Scholar]
- 3. Rose, T. 1945. Recurrent appendiceal abscess. Med. J. Aust. 32:659–662. [Google Scholar]
- 4. Cama, J. K. 2010. Recurrent abdominal pain post appendectomy: a rare case. Pac. Health Dialog 16:78–81. [PubMed] [Google Scholar]
- 5. Aschkenasy, M. T. , and Rybicki F. J.. 2005. Acute appendicitis of the appendiceal stump. J. Emerg. Med. 28:41–43. [DOI] [PubMed] [Google Scholar]
- 6. Harris, C. R. 1989. Appendiceal stump abscess ten years after appendectomy. Am. J. Emerg. Med. 7:411–412. [DOI] [PubMed] [Google Scholar]
- 7. Roche‐Nagle, G. , Gallagher C., Kilgallen C., and Caldwell M.. 2005. Stump appendicitis: a rare but important entity. Surgeon 3:53–54. [DOI] [PubMed] [Google Scholar]
- 8. Clark, J. , and Theodorou N.. 2004. Appendicitis after appendicectomy. J. R. Soc. Med. 97:543–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mangi, A. A. , and Berger D. L.. 2000. Stump appendicitis. Am. Surg. 66:739–741. [PubMed] [Google Scholar]
- 10. Werbin, N. 2005. Unfinished surgery. Harefuah 144:894–908. [PubMed] [Google Scholar]
- 11. Roberts, K. E. , Starker L. F., Duffy A. J., and Bell R. L.. 2011. Stump appendicitis: a surgeon's dilemma. JSLS 15:373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Humes, D. J. , and Simpson J.. 2006. Acute appendicitis. BMJ 333:530–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bickell, N. A. , Aufses A. H. Jr, Rojas M., and Bodian C.. 2006. How time affects the risk of rupture in appendicitis. J. Am. Coll. Surg. 202:401–406. [DOI] [PubMed] [Google Scholar]
- 14. Greenberg, J. J. , and Esposito T. J.. 1996. Appendicitis after laparoscopic appendectomy: a warning. J. Laparoendosc. Surg. 6:185–187. [DOI] [PubMed] [Google Scholar]
- 15. Liang, M. K. , Lo H. G., and Marks J. L.. 2006. Stump appendicitis: a comprehensive review of literature. Am. Surg. 72:162–166. [PubMed] [Google Scholar]
- 16. Puylaert, J. B. 1986. Acute appendicitis: US evaluation using graded compression. Radiology 158:355–360. [DOI] [PubMed] [Google Scholar]
- 17. Ishikawa, H. 2003. Diagnosis and treatment of Acute Appendicitis. JMAJ 46:217–221. [Google Scholar]
- 18. Watkins, B. P. , Kothari S. N., and Landercasper J.. 2004. Stump appendicitis: case report and review. Surg. Laprosc. Endosc. Percutan. Tech. 14:167–171. [DOI] [PubMed] [Google Scholar]
- 19. O'Leary, D. P. , Myers E., Coyle J., and Wilson I.. 2010. Case report of recurrent acute appendicitis in a residual tip. Cases J. 3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. De, U. , and De Krishna K.. 2004. Stump appendicitis. J. Indian Med. Assoc. 102:329. [PubMed] [Google Scholar]


