Abstract
Objective:
Atrial fibrillation (AF) is the most common arrhythmia following coronary artery by-pass graft surgery (CABG). The value of SYNTAX score to predict postoperative atrial fibrillation (PoAF) has not been clearly addressed. We aimed to evaluate this relationship in patients undergoing isolated CABG.
Methods:
This study was designed as a single-center, non-randomized, observational, prospective study. Ninety-four patients undergoing isolated on-pump CABG, who had sinus rhythm and were older than 18 years, were enrolled. Demographic characteristics of the patients were recorded; SYNTAX score was calculated preoperatively for each patient. The univariate and multivariate logistic regression analysis were used to determine for predictors of PoAF.
Results:
The median SYNTAX score of the enrolled patients was 21, (56–5). PoAF was observed in 31 (33.3%) patients. Univariate logistic regression showed that age, chronic obstructive pulmonary disease (COPD), red blood cell distribution width (RDW), urea, initial troponin I, peak postoperative troponin I, interventricular septum, left atrial diameter, and SYNTAX score were significantly associated with the frequency of PoAF following CABG. An independent association was identified with age [b 0.088, p:0.023, OR: 1.092, 95% CI (1.012–1.179)], COPD [(b: 2.222, p:0.003, OR: 9.228, 95% CI (2.150–39.602)], and SYNTAX score [(b: 0.130, p:0.002, OR: 1.139, 95% CI (1.050–1.235)].
Conclusion:
This study showed that a higher SYNTAX score was related to more frequent PoAF in patients undergoing isolated on-pump CABG.
Keywords: postoperative atrial fibrillation, SYNTAX score, coronary artery bypass grafting surgery
Introduction
Atrial fibrillation (AF) is the most common arrhythmia following coronary artery bypass graft surgery (CABG) with a reported incidence of 5%–40% (1–3). Despite the improvements in myocardial protection, cardiovascular anesthesia, and surgical technics, atrial fibrillation is still frequently observed postoperatively after CABG probably due to aging patient population (4). Postoperative atrial fibrillation (PoAF) adversely affects mortality and morbidity and also increases the costs because it prolongs the duration of hospitalization (5). SYNTAX score (synergy between percutaneous coronary intervention with Taxus and cardiac surgery) is a scoring system evaluating the complexity of the lesions in coronary angiography (6). Its prognostic value was studied in patients with 3-vessel or left main coronary artery disease who need to decide between percutaneous coronary intervention (PCI) and CABG (7–10). It was reported that SYNTAX score reflected coronary complexity and helped the clinician to predict major complications after PCI and CABG (11, 12). We hypothesized that increasing coronary lesion complexity may be associated with PoAF. The value of SYNTAX score to predict PoAF has not been clearly addressed. Thus, we aimed to evaluate this relationship in patients undergoing isolated CABG.
Methods
This study was designed as a single-center, non-randomized, observational, prospective study. It was conducted to evaluate the relationship between preoperative SYNAX score and PoAF in patients undergoing isolated on-pump CABG. Ninety-four patients undergoing isolated CABG at our institution were included. The study was approved by the local institutional Ethical Committee; oral and written informed consent was obtained from all study participants.
Study design and participants
Isolated on-pump CABG patients older than 18 years with sinus rhythm were consecutively enrolled. Patients with ST-elevation myocardial infarction (STEMI); those undergoing off-pump coronary surgery; those with a history of previous arrhythmia (including permanent AF and paroxsymal AF); those who had postoperative bleeding; those with current use of sotalol, amiodarone, non-steroidal anti-inflammatory drugs, or corticosteroid; and those with concomitant valvular pathology requiring surgery and ischemic mitral regurgitation, left atrial diameter >50 mm (13), hyperthyroidism, neo-plastic and rheumatic disease, hepatic failure, or serious infection were excluded.
Surgical revascularization was performed in the presence of at least 70% stenosis lesion on at least one epicardial coronary artery including left anterior descending coronary artery or at least 50% stenosis on left main coronary artery (LMCA).
Patients with LMCA stenosis were labeled as 2-vessel disease when the right coronary system was dominant and 3-vessel disease when the left coronary system was dominant.
Patients who had ≥20 minutes resting angina, new-onset Canadian Cardiovascular Society (CCS) Class II-III angina, increased anginal severity to CCS III-IV in patients with stable angina pectoris and post-myocardial infarction (post-MI) angina, and cardiac biomarker-positive patients with ischemic angina were diagnosed with non-ST-elevation acute coronary syndrome (non-STE-ACS) (14).
Stable coronary artery disease was defined according to the current guidelines of European Society of Cardiology (ESC) (15). Hypertension was defined as arterial blood pressure >140/90 mm Hg or receiving antihypertensive treatment. Diabetes mellitus (DM) was defined as fasting plasma glucose level ≥126 mg/dL or random plasma glucose ≥200 mg/dL plus diabetic symptoms or 2-hour plasma glucose ≥200 mg/dL in oral glucose tolerance test or HbA1C level ≥6.5.
A diagnosis of chronic obstructive pulmonary disease (COPD) was established using spirometry test in patients with chronic cough, sputum, and dyspnea, based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines (16).
Demographic and baseline clinical characteristics, two dimensional (2D) echocardiographic parameters, and laboratory tests were performed the day before surgery, and preoperative medications were recorded.
Surgical technique
All patients were given morphine and diazepam (0.1 mg/kg) preoperatively. General anesthesia was induced by using etomidate (0.3 mg/kg), midazolam (0.1 mg/kg), and sufentanil (1–2 µg/kg). The operations were performed by standard midline sternotomy. The left internal mammary artery (LIMA) was used to graft the left anterior descending coronary artery and saphenous vein grafts were used for the remaining coronary arteries. Intravenous bolus of heparin was administered (150 IU/kg) to obtain activated clotting time (ACT) of ≥480 seconds. Additional bolus of heparin was injected when required to keep ACT at the appropriate level. Myocardial protection was achieved with antegrade or retrograde cold blood cardioplegia with high potassium level. After completion of the anastomosis, protamine sulfate was administered to neutralize the effect of heparin. Cardiopul-monary bypass time, temperature, and cross-clamp times were recorded for each patient. After the surgical procedure, patients were followed up at the cardiovascular intensive care unit and extubated when hemodynamic stabilization, normothermia, an adequate pain control, and consciousness were achieved. All patients were given antiplatelet therapy for the first 24 hours.
Atrial fibrillation (AF)
After surgery, subjects were followed for at least 72–96 hours by continuous telemetry. A 12-lead electrocardiography (ECG) was obtained from the subjects every 12 or 24 hours at the intensive care and in-patient units, respectively. Additional 12-lead ECG was taken when the subjects complained of dyspnea, palpitation, or angina. Rhythm monitoring was continued until the discharge of the patients from the hospital. PoAF was described as irregular, fast oscillations, or fibrillatory waves instead of regular P waves at ECG. An AF episode lasting longer than 5 minutes was accepted as PoAF (17). Standard treatment was given to patients with PoAF. Medical cardioversion was conducted with amiodarone (5 mg/kg) for 30 minutes, followed by 1200 mg/day. Systolic blood pressure under 90 mm Hg was defined as hemodynamic instability, and electrical cardioversion was performed. Standard anticoagulant therapy was established with heparin.
Laboratory examination
Laboratory parameters were studied from venous blood sampled before the surgery. The highest troponin value was recorded as the peak troponin level in the postoperative period, and the postoperative neutrophil/lymphocyte ratios for each patient were calculated.
SYNTAX score
SYNTAX score was calculated from coronary angiographic views before CABG for each patient using the SYNTAX score calculator, Version 2.11 (available at: http://www.syntax-score.com). The vessels with a diameter of ≥1.5 mm and the lesions with ≥50% stenosis were scored. Scoring was performed for each patient according to the following parameters: coronary dominance; number of lesions; segments involved per lesion; the presence of total occlusion, trifurcation, bifurcation, aor-to-osteal lesion, severe tortuosity, calcification, thrombus, and diffuse/small vessel disease; and lesion length >20 mm. Scoring was performed by an experienced interventional cardiologist.
Echocardiographic examination
Baseline echocardiographic examinations were performed with standard commercial ultrasound system (Vivid 3, General Electric Vingmed, Horten, Norway) using 2.5–3.5-MHz multiphase-array probe before the operation. Echocardiographic examinations were performed at patient’s bedside by a single investigator. Left ventricular dimensions were measured using M-mode and parasternal long-axis view. Ejection fraction was calculated by the modified Simpson’s method from apical 4- and 2-chamber views. Left atrial diameter was measured as the anteroposterior diameter from the parasternal long-axis. Interventricular septum and posterior wall thicknesses were measured from parasternal long-axis view at end-diastole. Diastolic parameters were measured according to the American Society of Echocardiography guidelines (18).
Statistical analysis
The data were expressed as mean (±SD) and median (range) for continuous variables and as percentage for categorical variables. Kolmogorov–Smirnov test was used to identify distribution of variables. Unpaired t-test or Mann–Whitney U test were used to compare continuous variables as appropriate. Fisher’s exact and continuity correction (Yate’s correction) tests were used compare categorical variables.
The baseline variables which were found significant (p<0.05) in the univariate analysis were included in the multivariate logistic regression analysis (forward stepwise model) to determine the independent components of PoAF. The results of the model were reported as odds ratio (OR), 95% confidence interval, beta, and p values. Receiver-operating characteristic (ROC) curve for the prediction of PoAF after CABG was constructed and the area under the curve (AUC) was calculated for SYNTAX score. The cut-off value for SYNTAX score was calculated using the sensitivity and specificity estimates. For all tests, a p value of <0.05 was considered statistically significant. Statistical Package for the Social Sciences (SPSS version 11.0, SPSS Inc., Chicago, IL, USA) software was used to perform analysis.
Results
In all, 143 consecutive patients referred for CABG were evaluated. The following patients were excluded: 8 with STEMI, 6 with AF, 12 who underwent off-pump coronary surgery, 5 with renal failure, 7 who required concomitant valvular surgery, and 11 who were using antiarrythmics or non-steroidal anti-inflammatory drugs. Mean age of the 94 (22 female, 72 male) patients enrolled was 62±8 years. Patients’ clinical characteristics and drug uses are presented in Table 1. The median SYNTAX score of the patients enrolled was 21 (5–56). PoAF was observed in 31 (33.3%) patients. In two of these patients, sinus rhythm was restored with electrical cardioversion because they had hemodynamic instability.
Table 1.
Clinical characteristics of the study population
| Patient group n=94 | |
|---|---|
| Age, years | 62±8 |
| Gender, n (male %) | 72 (75.8) |
| Hypertension, n (%) | 57 (61.3) |
| Diabetes mellitus, n (%) | 41 (43.6) |
| Current smoking, n (%) | 51 (54.8) |
| Hyperlipidemia, n (%) | 21 (22.3) |
| Previous MI, n (%) | 29 (30.9) |
| Previous CHF, n (%) | 25 (26.6) |
| Chronic renal failure, n (%) | 3 (3.2) |
| Previous stroke, n (%) | 11 (11.8) |
| PAD, n (%) | 4 (4.3) |
| COPD, n (%) | 21 (22.3) |
| Carotid artery disease, n (%) | 12 (12.8) |
| Stable angina pectoris, n (%) | 55 (59.1) |
| Non-STE-ACS, n (%) | 38 (40.9) |
| Post-op MI, n (%) | 54 (58.7) |
| Post-op AF, n (%) | 31 (33.3) |
| AF duration (h) | 9 (72–1) |
| Three or more stenotic vessels, n (%) | 48 (51.6) |
ACEIs - angiotensin converting enzyme inhibitors; AF - atrial fibrillation; CHF - congestive heart fail-ure; COPD - chronic obstructive pulmonary disease; h - hour; MI - myocardial infarction; Non-STE ACS - non-ST-elevation acute coronary syndrome; PAD - peripheral artery disease; Post-op - postoperative
In Table 2, the clinical, laboratory, and echocardiographic variables of patient with and without PoAF were compared. Age (59±8 vs. 66±8, p:0.001), COPD (9% vs. 48%, p<0.001), Red blood cell distribution width (RDW), (15±1.2 vs. 15±1.4, p:0.032), urea mg/dL (37±11 vs. 44±15, p:0.013) creatinine mg/dL [0.78 (4.30–0.39) vs. 0.90 (7.80–0.51), p:0.012], left atrial diameter (3.6±0.3 cm vs. 3.8±0.3 cm, p:0.013) septum thickness [1 (1.4–0.6) vs. 1.1 (1.6–0.7), p:0.047], and SYNTAX score (18±7 vs. 28±11, p<0.001) were different between two groups.
Table 2.
Comparison of variables between postoperative AF negative/positive groups
| Postop AF (-)n=63 | Postop AF (+)n=31 | P | Postop AF (-)n=63 | Postop AF (+)n=31 | P | ||
|---|---|---|---|---|---|---|---|
| Age, years | 59±8 | 66±8 | 0.001 | CRP, mg/dL | 0.85 (9.21–0.12) | 1.11 (11.2–0.17) | 0.192 |
| Gender, n (male %) | 44 (71) | 27 (87) | 0.142 | Urea, mg/dL | 37±11 | 44±15 | 0.013 |
| Hypertension, n (%) | 35 (57) | 22 (71) | 0.297 | Creatinine, mg/dL | 0.78 (4.30–0.39) | 0.90 (7.80–0.51) | 0.012 |
| Diabetes mellitus, n (%) | 29 (46) | 12 (38) | 0.605 | LDL-C, mg/dL | 130±40 | 125±36 | 0.653 |
| Current smoking, n (%) | 33 (54) | 17 (54) | 1 | HDL-C, mg/dL | 40±9 | 38±9 | 0.285 |
| Hyperlipidemia, n (%) | 17 (27) | 4 (12) | 0.187 | TG, mg/dL | 186±94 | 153±55 | 0.110 |
| Previous MI, n (%) | 16 (25) | 13 (41) | 0.178 | Initial Troponin I, | 0.01 (1.52–0) | 0.02 (22–0) | 0.091 |
| ng/mL | |||||||
| Previous CHF, n (%) | 16 (25) | 9 (29) | 0.934 | Pre-op peak | 0.01 (50–0) | 0.05 (29–0) | 0.133 |
| Troponın I, ng/mL | |||||||
| Chronic renal failure, n (%) | 1 (1.6) | 2 (6) | 0.257 | Post-op peak | 5.1 (50–0) | 4.6 (50–0.52) | 0.346 |
| Troponin I, ng/mL | |||||||
| Previous stroke, n (%) | 6 (9) | 5 (16) | 0.498 | LVEF, % | 55 (65–30) | 55 (65–20) | 0.403 |
| PAD, n (%) | 3 (4) | 1 (3) | 1 | LVESD, cm | 3.1 (5.5–2.4) | 3.3 (5.2–2.8) | 0.082 |
| COPD, n (%) | 6 (9) | 15 (48) | <0.001 | LVEDD, cm | 4.96±0.48 | 5.07±0.53 | 0.320 |
| Stable angina pectoris, n (%) | 41 (66) | 14 (45) | 0.086 | LAD, cm | 3.6±0.3 | 3.8±0.3 | 0.013 |
| Non STE ACS, n (%) | 21 (33) | 17 (54) | 0.086 | Septum, cm | 1 (1.4–0.6) | 1.1 (1.6–0.7) | 0.047 |
| Post-op MI, n (%) | 34 (54) | 20 (66) | 0.397 | E wave, mm/sn | 99±17 | 101±21 | 0.627 |
| Three or more stenotic vessels, n (%) | 30 (48) | 18 (58) | 0.509 | A wave, mm/sn | 91±17 | 95±19 | 0.337 |
| Laboratory | E’ wave, cm/sn | 10±1.9 | 10±1.8 | 0.765 | |||
| WBC, µL | 8.3±2.2 | 8.1±2.2 | 0.620 | E/A ratio | 1.14±0.34 | 1.14±0.46 | 0.942 |
| Hemoglobin, g/dL | 13.5±1.5 | 13.1±1.5 | 0.261 | E/E’ ratio | 9.8±1 | 9.9±2.3 | 0.673 |
| Platelet,103/µL | 231±57 | 253±68 | 0.105 | Posterıor wall, cm | 1 (1.3–0.8) | 1 (1.7–0.8) | 0.061 |
| Mean platelet volume, fL | 7.4±0.9 | 7.5±0.9 | 0.600 | Syntax Score | 18±7 | 28±11 | <0.001 |
| Red cell distribution width, % | 15±1.2 | 15±1.4 | 0.032 |
A wave - late ventricular filling velocity; AF - atrial fibrillation; CHF - congestive heart failure; COPD - chronic obstructive pulmonary disease; CRP - C reactive protein; E wave - early ventricular filling velocity; E’ - left ventricular tissue Doppler early diastolic velocity; HDL-C - high-density lipoprotein cholesterol; LAD - left atrial diameter; LDL-C - low-density lipoprotein cholesterol; LVEDD - left ventricle end-diastolic diameter; LVEF - left ventricle ejection fraction; LVESD - left ventricle end-systolic diameter; MI - myocardial infarction; Non-STE-ACS - non-ST-elevation acute coronary syndrome; PAD - peripheral artery disease; Pre-op - preoperative; Post-op - postoperative; TG - triglycerides; WBC - white blood cells
Unpaired t-test or Mann–Whitney U test were used to compare continuous variables as appropriate. Fisher’s exact and continuity correction (Yate’s correction) tests were used compare categorical variables
Univariate logistic regression showed that age, COPD, red blood cell distribution width (RDW), urea, initial troponin I, peak postoperative troponin I, left atrial diameter, interventricular septum, and SYNTAX score were significantly associated with the frequency of PoAF following CABG (Table 3). A multivariate logistic regression analysis was performed to determine the independent predictors of PoAF. Age [(b: 0.088, p:0.023, OR: 1.092, 95% CI (1.012–1.179)], COPD [(b: 2.222, p:0.003, OR: 9.228, 95% CI (2.150–39.602)], and SYNTAX score [b: 0.130, p:0.002, OR: 1.139, 95% CI (1.050–1.235)] were independently associated with PoAF (Hosmer and Lemeshow Test; p:0.602, Nagelkerke R Square: 0.522)] (Table 4).
Table 3.
Univariate analysis of postoperative AF frequency
| OR | 95% CI | OR | 95% CI | ||
|---|---|---|---|---|---|
| Age, years | 1.103 | 1.038–1.173 | Platelet | 1.006 | 0.999–1.013 |
| Gender | 2.761 | 0.845–9.028 | Mean platelet volume | 1.127 | 0.724–1.755 |
| Hypertension | 1.816 | 0.719–4.588 | Red cell distribution width | 1.410 | 1.013–1.964 |
| Diabetes mellitus | 0.719 | 0.299–1.730 | Syntax score | 1.131 | 1.058–1.210 |
| Current smoking | 1.030 | 0.432–2.455 | CRP | 1.155 | 0.897–1.487 |
| Hyperlipidemia | 0.392 | 0.119–1.288 | Urea | 1.041 | 1.006–1.077 |
| Previous MI | 2.076 | 0.834–5.171 | Creatinine | 1.662 | 0.745–3.708 |
| Previous CHF | 1.176 | 0.450–3.077 | Initial Troponin I | 4.928 | 1.076–22.562 |
| Chronic renal failure | 4.207 | 0.366–48.30 | Pre-op peak Troponin I | 0.936 | 0.953–1.045 |
| Previous stroke | 1.763 | 0.492–6.310 | Post-op peak Troponin I | 1.037 | 1.001–1.075 |
| PAD | 0.720 | 0.065–6.574 | LVEF | 0.973 | 0.935–1.012 |
| COPD | 8.750 | 2.919–26.22 | LAD | 4.878 | 1.313–18.120 |
| Stable angina pectoris | 0.422 | 0.175–1.018 | E wave | 1.006 | 0.983–1.029 |
| Non STE ACS | 2.371 | 0.982–5.724 | A wave | 1.012 | 0.988–1.037 |
| Post-op MI | 1.647 | 0.664–4.088 | E wave | 1.035 | 0.829–1.291 |
| Three or more stenotic vessels | 1.477 | 0.619–3.525 | E/E’ ratio | 1.060 | 0.812–1.384 |
| WBC | 0.951 | 0.781–1.158 | Septum | 53.369 | 1.630–1949 |
| Hemoglobin | 0.853 | 0.646–1.125 | Posterior wall | 26.595 | 0.626–1130.5 |
A wave - late ventricular filling velocity; AF - atrial fibrillation; CHF - congestive heart failure; COPD - chronic obstructive pulmonary disease; CRP - c reactive protein; E wave - early ventricular filling velocity; E’ - left ventricular tissue Doppler early diastolic velocity; LAD - left atrial diameter; LVEF - left ventricle ejection fraction; MI - myocardial infarction; Non STE ACS - non ST elevation acute coronary syndrome; PAD - peripheral artery disease; Pre-op - pre-operative; Post-op - post-operative; WBC -white blood cells
Multivariate logistic regression analysis to determine the independent components of PoAF
Table 4.
Multivariate analysis for independent predictors of post-operative atrial fibrillation after coronary artery bypass graft surgery
| β | P | OR | 95% CI | |
|---|---|---|---|---|
| Age, years | 0.088 | 0.023 | 1.092 | 1.012–1.179 |
| COPD | 2.222 | 0.003 | 9.228 | 2.150–39.602 |
| Syntax score | 0.130 | 0.002 | 1.139 | 1.050–1.235 |
COPD - chronic obstructive pulmonary disease
An ROC curve analysis was used to determine a cut-off value for SYNTAX score (Fig. 1). SYNTAX score >18.75 had 85.7% sensitivity and 55.1% specificity to predict PoAF (area under curve: 0.756, p<0.001, 95% CI (0.645–0.868).
Figure 1.
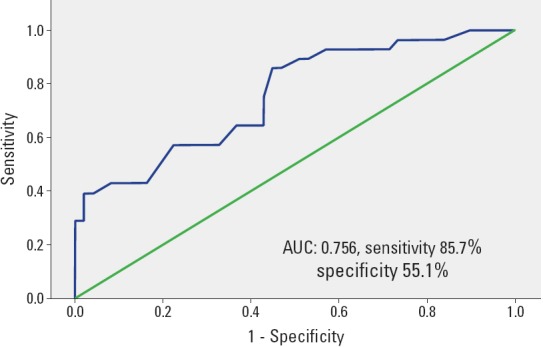
ROC analysis for SYNTAX score with cut-off. Area under curve (AUC), 95% CI, and P were reported
Discussion
With this study we observed that advanced age, COPD, and SYNTAX score were independent predictors of PoAF in patients undergoing isolated on-pump CABG surgery. Additionally, a SYNTAX score of >18.75 predicted PoAF with a sensitivity of 85.7% and a specificity of 55.1%. To the best of our knowledge, this is the first study reporting that the STNTAX score is associated with PoAF incidence in this patient population.
Atrial fibrillation is the most common arrhythmia after cardiac surgery. Despite improved surgical, myocardial protection, and anesthetic techniques, atrial fibrillation is still frequently observed in the elderly patients undergoing cardiac surgery (4). The incidence of postoperative atrial fibrillation following CABG surgery is seen in 25%–40% of cases. However, its frequency reaches to 62% following combined coronary artery bypass grafting and valve surgery (19). As a consequence of PoAF mortality and morbidities like embolic events increase and the duration of hospitalization is prolonged (20). The risk of PoAF in valvular and combined surgery, including coronary and valvular, was reported to be higher than that in coronary surgery alone. Mariscalco et al. (21) identified the PoAF rates as 22.9%, 39.8%, and 45.2% for the isolated CABG, valve surgery, and combined surgery, respectively. PoAF is more frequent during cardiac surgery than during non-cardiac surgery (22). In a meta-analysis by Møller et al. (23), on-pump and off-pump CABG were compared in terms of PoAF and was reported to be lower in patients undergoing off-pump surgery. In our study patients, the incidence of PoAF was 33%, which is consistent with the previous reports.
Among the parameters that were mentioned in previous reports, decline in renal functions, RDW, left atrial size, left ventricular hypertrophy, and perioperative troponin I were univariate predictors in our study; however, they were not significant in multivariate analysis (24–28). Likewise, in our study, age had been reported as a major predictor of PoAF and the incidence of PoAF increases progressively after the age of 70 years (29). With advanced age, atrial physiology, stiffness, and atrial excitation are affected (30, 31). Age-related changes, including atrial fibrosis and accumulation of amyloid, can cause intraatrial reentry, which leads to the development of AF (32). Co-morbid conditions increase with advanced age, and this is another reason for more frequent AF in the elderly (33). There was not a hard limit for age in our study, and PoAF increased in parallel with the patient age. This finding is not surprising since age is a risk factor for many cardiovascular pathologic conditions. Our patients’ population was younger than the studies mentioned above; however, the incidence of PoAF was similar. This may have resulted from our inclusion of patients with non-STE-ACS in addition to elective CABG. The pathophysiologic mechanisms in acute cor-onary syndromes might have also interfered in our study with the enrollment of patients with non-STE-ACS. We think that in a younger patient population atrial ischemia/infarct, elevated end-diastolic pressures, and decreased ejection fraction resulted in AF frequency, which was similar to elderly patients.
In our patient population, COPD was an independent predictor of PoAF, which is also consistent with previous studies. The incidence of PoAF increased to 43% in the presence of COPD (29). Mathew et al. (29) have showed that COPD increased the incidence of both persistent and paroxysmal atrial fibrillation. Postoperative hypoxemia was showed to be the most common cause of cardiac arrhythmias (34). However, the exact mechanism that causes development of PoAF in COPD patients remains unclear.
SYNTAX score shows the complexity of coronary artery disease and is able to predict the rate of major advanced cardiovascular events (MACE) after revascularization (6, 7, 35). SYNTAX score has also been shown to predict short- and long-term adverse events following revascularization (7). However, the relationship between the SYNTAX score and PoAF is poorly addressed. Interestingly, SYNTAX score was also an independent predictor of PoAF in our study. In a study by Fukui et al. (12), the combination of SYNTAX score and EUROSCORE 2 was reported to predict early adverse events in patients undergoing CABG. But contrary to our findings, there was no significant difference between high and low SYNTAX score groups for the development of PoAF. However, they used off-pump surgical technique for almost all of their patients and incidence of AF is lower in patients undergoing off-pump surgery (23, 36).
SYNTAX score was established to grade anatomic complexity of the lesions and decide on the re-vascularization strategy; however, its association with major adverse cardiac and cerebrovascular events led us to design this study (37). It is obvious that it is not possible to explain the increased incidence of PoAF with a single scoring system, but SYNTAX score was one of the independent factors in multivariate analysis.
Study limitations
The main limitations of this study are the relatively small sample size and the non-randomized nature of the study. Also, left atrial volume was not calculated and long-term clinical course of the patients is not recorded. In the in-patients unit, electrocardiograms were recorded daily, which could have resulted in missing some of the paroxysmal AF episodes. Inflammatory markers were not measured in our study, although predictive role of those for PoAF had been shown in previous studies. Additionally, all CABG operations were not performed by a single operator or surgical team and this may also be a confounding factor.
Conclusion
In our study, we showed that SYNTAX score was higher in patients with PoAF. SYNTAX score might be helpful for the prediction of PoAF in patients undergoing isolated on-pump CABG.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept- Ç.G., N.Ö., G.B.G., M.C.; Design- T.B., Ö.C., E.G., E.E., M.C.; Supervision-Ç.G., R.D.A., G.B.G., T.U.; Funding-; Materials- R.B.B., R.D.A., E.E., F.Y.; Data collection &/or processing –M.C., T.U., F.Y., E.E., E.G.; Analysis and/or interpretation– G.B.G., E.G., R.D.A., T.U., S.H.; Literature search- Ö.C., F.Y., R.B.B., T.B.; Writing – Ç.G., S.H., N.Ö., T.B.; Critical review- Ç.G., R.B.B., N.Ö., Ö.C., S.H.
References
- 1.Halpin LS, Barnett SD, Burton NA. National databases and clinical practice specialist:decreas-ing postoperative atrial fibrillation following cardiac surgery. Outcomes Manage. 2004;8:33–8. [PubMed] [Google Scholar]
- 2.Ad N, Barnett SD, Haan CK, O'Brien SM, Milford-Beland S, Speir AM. Does preoperative atrial fibrillation increase the risk for mortality and morbidity after coronary artery bypass grafting? J Thorac Cardiovasc Surg. 2009;137:901–6. doi: 10.1016/j.jtcvs.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 3.Rogers CA, Angelini GD, Culliford LA, Capoun R, Ascione R. Coronary surgery in patients with preexisting chronic atrial fibrillation:early and midterm clinical outcome. Ann Thorac Surg. 2006;81:1676–82. doi: 10.1016/j.athoracsur.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 4.Sanjuán R, Blasco M, Carbonell N, Jordá A, Núñez J, Martínez-León J, et al. Preoperative use of sotalol versus atenolol for atrial fibrillation after cardiac surgery. Ann Thorac Surg. 2004;77:838–43. doi: 10.1016/j.athoracsur.2003.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Aranki SF, Shaw DP, Adams DH, Rizzo RJ, Couper GS, VanderVliet M, et al. Predictors of atrial fibrillation after coronary artery surgery. Current trends and impact on hospital resources. Circulation. 1996;94:390–7. doi: 10.1161/01.cir.94.3.390. [DOI] [PubMed] [Google Scholar]
- 6.Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX Score:an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219–27. [PubMed] [Google Scholar]
- 7.Valgimigli M, Serruys PW, Tsuchida K, Vaina S, Morel MA, Van den Brand MJ, et al. Cyphering the complexity of coronary artery disease using the SYNTAX score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol. 2007;99:1072–81. doi: 10.1016/j.amjcard.2006.11.062. [DOI] [PubMed] [Google Scholar]
- 8.Lemesle G, Bonello L, de Labriolle A, Steinberg DH, Roy P, Pinto Slottow TL, et al. Prognostic value of the SYNTAX score in patients undergoing coronary artery bypass grafting for three-vessel coronary artery disease. Catheter Cardiovasc Interv. 2009;73:612–7. doi: 10.1002/ccd.21883. [DOI] [PubMed] [Google Scholar]
- 9.Capodanno D, Di Salvo ME, Cincotta G, Miano M, Tamburino C, Tamburino C. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv. 2009;2:302–8. doi: 10.1161/CIRCINTERVENTIONS.108.847137. [DOI] [PubMed] [Google Scholar]
- 10.Birim O, van Gameren M, Bogers AJ, Serruys PW, Mohr FW, Kappetein AP. Complexity of coronary vasculature predicts outcome of surgery for left main disease. Ann Thorac Surg. 2009;87:1097–104. doi: 10.1016/j.athoracsur.2008.11.079. [DOI] [PubMed] [Google Scholar]
- 11.Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, et al. Assessment of the SYNTAX score in the SYNTAX study. EuroIntervention. 2009;5:50–6. doi: 10.4244/eijv5i1a9. [DOI] [PubMed] [Google Scholar]
- 12.Fukui T, Uchimuro T, Takanashi S. EuroSCORE II with SYNTAX score to assess risks of coronary artery bypass grafting outcomes. Eur J Cardiothorac Surg. 2015;47:66–71. doi: 10.1093/ejcts/ezu045. [DOI] [PubMed] [Google Scholar]
- 13.Rodrigo R, Korantzopoulos P, Cereceda M, Asenjo R, Zamorano J, Villalabeitia E, et al. A randomized controlled trial to prevent post-operative atrial fibrillation by antioxidant reinforcement. J Am Coll Cardiol. 2013;62:1457–65. doi: 10.1016/j.jacc.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. ESC Committee for Practice Guidelines. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation:The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology. Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 15.Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease:the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003. doi: 10.1093/eurheartj/eht296. [DOI] [PubMed] [Google Scholar]
- 16.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease:GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 17.Özaydın M, Dede O, Varol E, Kapan S, Türker Y, Peker O, et al. Effect of renin- angiotensin aldosteron system blockers on postoperative atrial fibrillation. Int J Cardiol. 2008;127:362–7. doi: 10.1016/j.ijcard.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 18.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults:a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiog-raphy. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 19.Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med. 2001;135:1061–73. doi: 10.7326/0003-4819-135-12-200112180-00010. [DOI] [PubMed] [Google Scholar]
- 20.Mariscalco G, Klersy C, Zanobini M, Banach M, Ferrarese S, Borsani P, et al. Atrial fibrillation after isolated coronary surgery affects late survival. Circulation. 2008;118:1612–8. doi: 10.1161/CIRCULATIONAHA.108.777789. [DOI] [PubMed] [Google Scholar]
- 21.Mariscalco G, Engström KG. Postoperative atrial fibrillation is associated with late mortality after coronary surgery, but not after valvular surgery. Ann Thorac Surg. 2009;88:1871–6. doi: 10.1016/j.athoracsur.2009.07.074. [DOI] [PubMed] [Google Scholar]
- 22.Almassi GH, Schowalter T, Nicolosi AC, Aggarwal A, Moritz TE, Henderson WG, et al. Atrial fibrillation after cardiac surgery:a major morbid event? Ann Surg. 1997;226:501–11. doi: 10.1097/00000658-199710000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Møller CH, Penninga L, Wetterslev J, Steinbrüchel DA, Gluud C. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev. 2012;3:CD007224. doi: 10.1002/14651858.CD007224.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu D, Murakoshi N, Sairenchi T, Irie F, Igarashi M, Nogami A, et al. Anemia and reduced kidney function as risk factors for new onset of atrial fibrillation (from the Ibaraki prefectural health study) Am J Cardiol. 2015;115:328–33. doi: 10.1016/j.amjcard.2014.10.041. [DOI] [PubMed] [Google Scholar]
- 25.Ertaş G, Aydın C, Sönmez O, Erdoğan E, Turfan M, Tasal A, et al. Red cell distribution width predicts new-onset atrial fibrillation after coronary artery bypass grafting. Scand Cardiovasc J. 2013;47:132–5. doi: 10.3109/14017431.2012.736636. [DOI] [PubMed] [Google Scholar]
- 26.Osranek M, Fatema K, Quaddoura F, Al-Saileek A, Barnes ME, Bailey KR, et al. Left atrial volume predicts the risk of atrial fibrillation after cardiac surgery:a prospective study. J Am Coll Cardiol. 2006;48:779–86. doi: 10.1016/j.jacc.2006.03.054. [DOI] [PubMed] [Google Scholar]
- 27.Wachtell K, Lehto M, Gerdts E, Olsen MH, Hornestam B, Dahlof B, et al. Angiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol:the Losartan Intervention For End Point Reduction in Hypertension (LIFE) study. J Am Coll Cardiol. 2005;45:712–9. doi: 10.1016/j.jacc.2004.10.068. [DOI] [PubMed] [Google Scholar]
- 28.Leal JC, Petrucci O, Godoy MF, Braile DM. Perioperative serum troponin I levels are associated with higher risk for atrial fibrillation in patients undergoing coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg. 2012;14:22–5. doi: 10.1093/icvts/ivr019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. Investigators of the Ischemia Research and Education Foundation;Multicenter Study of Perioperative Ischemia Research Group. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–9. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 30.Aldea GS, Soltow LO, Chandler WL, Triggs CM, Vocelka CR, Crockett GI, et al. Limitation of thrombin generation, platelet activation, and inflammation by elimination of cardiotomy suction in patients undergoing coronary artery bypass grafting treated with heparin-bonded circuits. J Thorac Cardiovasc Surg. 2002;123:742–55. doi: 10.1067/mtc.2002.120347. [DOI] [PubMed] [Google Scholar]
- 31.Issac TT, Dokainish H, Lakkis NM. Role of inflammation in initiation and perpetuation of atrial fibrillation:a systematic review of the published data. J Am Coll Cardiol. 2007;50:2021–8. doi: 10.1016/j.jacc.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 32.Nisanoğlu V, Erdil N, Aldemir M, Özgür B, Berat Cihan H, Yoloğlu S, et al. Atrial fibrillation after coronary artery bypass grafting in elderly patients:incidence and risk factor analysis. Thorac Cardiovasc Surg. 2007;55:32–8. doi: 10.1055/s-2006-924711. [DOI] [PubMed] [Google Scholar]
- 33.Valle FH, Costa AR, Pereira EM, Santos EZ, Pivatto Júnior F, Bender LP, et al. Morbidity and mortality in patients aged over 75 years undergoing surgery for aortic valve replacement. Arq Bras Cardiol. 2010;94:720–5. doi: 10.1590/s0066-782x2010005000052. [DOI] [PubMed] [Google Scholar]
- 34.Walsh SR, Tang T, Wijewardena C, Yarham SI, Boyle JR, Gaunt ME. Postoperative arrhythmias in general surgical patients. Ann R Coll Surg Engl. 2007;89:91–5. doi: 10.1308/003588407X168253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–72. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 36.Hashemzadeh K, Dehdilani M, Dehdilani M. Does off-pump coronary artery bypass reduce the prevalence of atrial fibrillation? J Cardiovasc Thorac Res. 2013;5:45–9. doi: 10.5681/jcvtr.2013.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carnero-Alcázar M, Maroto Castellanos LC, Silva Guisasola JA, Cobiella Carnicer J, Alswies A, Fuentes Ferrer ME, et al. SYNTAX Score is associated with worse outcomes after off-pump coronary artery bypass grafting surgery for three-vessel or left main complex coronary disease. J Thorac Cardiovasc Surg. 2011;142:123–32. doi: 10.1016/j.jtcvs.2010.10.036. [DOI] [PubMed] [Google Scholar]


