Abstract
Since its initial discovery in Drosophila, Hedgehog (HH) signaling has long been associated with foregut development. The mammalian genome expresses 3 HH ligands, with sonic hedgehog (SHH) levels highest in the mucosa of the embryonic foregut. More recently, interest in the pathway has shifted to improving our understanding of its role in gastrointestinal cancers. The use of reporter mice proved instrumental in our ability to probe the expression pattern of SHH ligand and the cell types responding to canonical HH signaling during homeostasis, inflammation, and neoplastic transformation. SHH is highly expressed in parietal cells and is required for these cells to produce gastric acid. Furthermore, myofibroblasts are the predominant cell type responding to HH ligand in the uninfected stomach. Chronic infection caused by Helicobacter pylori and associated inflammation induces parietal cell atrophy and the expansion of metaplastic cell types, a precursor to gastric cancer in human subjects. During Helicobacter infection in mice, canonical HH signaling is required for inflammatory cells to be recruited from the bone marrow to the stomach and for metaplastic development. Specifically, polarization of the invading myeloid cells to myeloid-derived suppressor cells requires the HH-regulated transcription factor GLI1, thereby creating a microenvironment favoring wound healing and neoplastic transformation. In mice, GLI1 mediates the phenotypic shift to gastric myeloid-derived suppressor cells by directly inducing Schlafen 4 (slfn4). However, the human homologs of SLFN4, designated SLFN5 and SLFN12L, also correlate with intestinal metaplasia and could be used as biomarkers to predict the subset of individuals who might progress to gastric cancer and benefit from treatment with HH antagonists.
Keywords: Metaplasia, GLI1, SHH, DAMPs, MDSCs, SPEM
Abbreviations used in this paper: ATPase, adenosine triphosphatase; DAMP, damage-associated molecular pattern; GLI, glioma-associated protein; Gr-MDSC, granulocytic myeloid-derived suppressor cell; HH, hedgehog; HHIP, hedgehog-interacting protein; IFN, interferon; IL, interleukin; MDSC, myeloid-derived suppressor cell; Mo-MDSC, monocytic myeloid-derived suppressor cell; mRNA, messenger RNA; PTCH, Patched; SHH, sonic hedgehog; SLFN4, Schlafen 4; SMO, Smoothened; SP, spasmolytic polypeptide; SPEM, spasmolytic polypeptide–expressing mucosa; SST, somatostatin; TLR, Toll-like receptor
Summary.
Hedgehog signaling plays an essential role in gastric development, homeostasis, and neoplastic transformation. This article reviews the evidence for its role in the initiation of gastric inflammation due to Helicobacter infection but then chronically polarizes myeloid cells into myeloid-derived suppressor cells creating a microenvironment favoring cancer development.
Hedgehog (HH) signaling initiates cancer in several organ systems,1, 2 but a clear etiologic role has not been shown for this pathway in gastric cancer. Because HH inhibitors currently are undergoing clinical trials for different types of cancer, understanding the role of HH signaling in regulating the tumor microenvironment becomes an important target to consider.3 Based on prior mouse studies of increased HH signaling in preneoplastic lesions,4, 5, 6 we have suggested that the use of HH inhibitors in human subjects chronically infected with Helicobacter might prevent progression of chronic atrophic gastritis to mucous gland metaplasias, a sentinel lesion that increases the likelihood of gastric cancer.7, 8, 9, 10 Thus, the focus of the current review is to understand the basis for HH signaling in normal adult stomach and how this developmental pathway might play a role in neoplastic transformation. Because our current understanding of HH signaling in the stomach arises from transgenic mouse models, the information presented refers to the mouse except when information from human studies exists.
Role of Hedgehog Signaling in Gastric Homeostasis
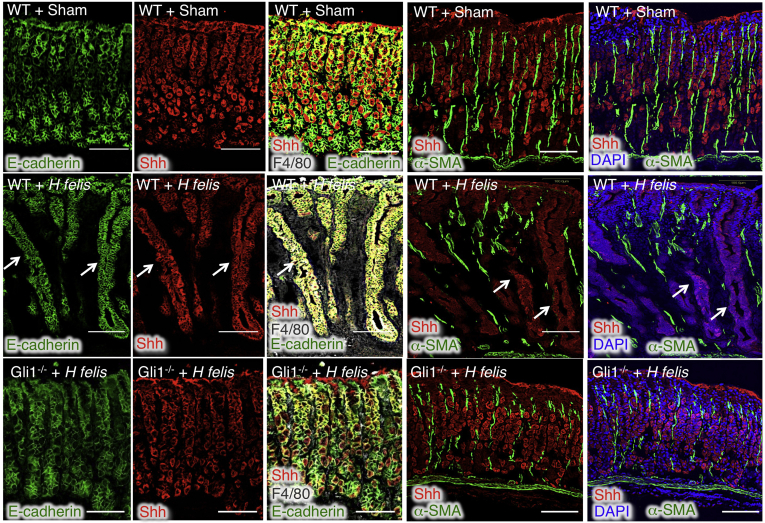
To date, there are 3 known mammalian genes encoding the hedgehog ligands: Sonic hedgehog (SHH), Indian hedgehog, and Desert hedgehog.11, 12, 13 During embryonic development, SHH is expressed throughout the gut and in other foregut-derived organs (eg, lung, pancreas).14, 15, 16 Although its function in mature gastric epithelium was not initially studied in adult mammals, it became apparent that SHH remains highly expressed in the stomach once expression in the intestine diminishes.17, 18 Subsequently, it was reported that SHH regulates epithelial cell maturation and differentiation in the adult stomach.19, 20 Normally, SHH is expressed in mature acid-secreting glands of the adult mouse and human stomachs, primarily within parietal cells19, 21, 22, 23 (Figure 1). During progression from the inflamed stomach to gastric cancer, the acid-producing parietal cells fail to produce acid and eventually are replaced by mucous-secreting cells that express spasmolytic polypeptide (SP) or trefoil factor 2.7, 24 Mostly in mice, but also in human subjects, SP-expressing mucosa (SPEM) is a type of oxyntic gland atrophy.25, 26 In concert with parietal cell atrophy, SHH expression in these acid-producing cells also is lost.23, 27 Although SHH expression diminishes along with loss of parietal cells, the expanding mucous cell compartment or SPEM continues to produce SHH in both human subjects20, 23 and rodents,4, 27 but remains unprocessed, maintaining the full-length 45-kilodalton form28 (Figure 1). Surprisingly, even unprocessed Hedgehog protein (Drosophila) shows activity where it traffics to the cell membrane to participate in cell–cell signaling.29 This result suggests that aberrant HH signaling in cancer might function as an autocrine or paracrine regulator, especially in the stem cell niche.30, 31, 32
Figure 1.
SHH expression in the stomach corpus of wild-type (WT) and Gli1-/-mice. Shown is the co-localization of SHH with E-cadherin, F4/80 (macrophage/myeloid marker), or α-smooth muscle actin (SMA) (myofibroblasts) protein markers in the absence or presence of Helicobacter felis infection. 4′,6-diamidino-2-phenylindole (DAPI) indicates cell nuclei. Arrows indicate the presence of SPEM.
Reprinted with permission from El-Zaatari et al.4 Scale bars = 100 μm.
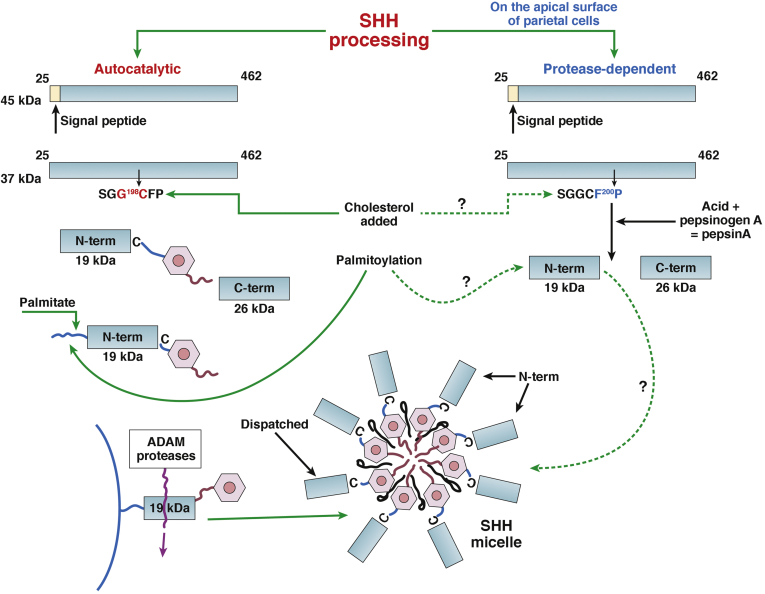
Processing of SHH to its active form (19 kilodaltons) in parietal cells becomes compromised in the absence of gastric acid.28 Atrophy of parietal and zymogenic (chief cell) lineages result in hypochlorhydria and reduced serum pepsinogen I (A) levels compared with pepsinogen II (C).33, 34, 35, 36, 37, 38, 39 These zymogens are proteins encoded by different gene loci that are used clinically to indicate preneoplastic changes in the stomach.38, 39 Pepsinogens A and C are converted to the enzymatically active aspartic proteinases, pepsin A and pepsin C, through intramolecular self-cleavage.39, 40 We showed previously that pepsinogen A is produced primarily in the mouse corpus by parietal cells, whereas pepsinogen C is produced primarily by both mucous neck and chief cells throughout the stomach.28 This result is consistent with the exclusive expression of pepsinogen A in the human corpus and not the antrum, whereas pepsinogen C marks mucous cells of both the antrum and corpus (www.proteinatlas.org). Pepsin A prefers to cleave proteins at hydrophobic and aromatic residues, particularly at phenylalanine (F) when the pH is less than 2. By contrast, pepsin C recognizes a broader consensus site and uses a wider pH spectrum than pepsin A.40, 41 Specifically, we showed using site-directed mutagenesis that pepsin A cleaves the nascent 45-kilodalton SHH polypeptide at residue 200 (SGGCF200|P) to generate the active 19-kilodalton form, whereas pepsin C does not cleave SHH peptide28 (Figure 2).
Figure 2.
SHH processing methods compared. Two mechanisms for processing SHH ligand have been reported. The best known is the autocatalytic mechanism of SHH in which the C-terminus functions as a cholesterol esterase by adding the sterol to cysteine residue 199 followed by adding the fatty acid palmitate to residue 25. The fatty acid permits SHH to be tethered to the plasma membrane until it is cleaved by A Disintegrin and Metalloproteinase Domain Containing Protein protease. The cleaved SHH molecules form miscelles in the presence of a transport protein called Dispatched. This mechanism has been described for Drosophila cells and mammalian cells derived from the mesenchyme. By contrast, parietal cells produce both gastric acid and pepsinogen A, a zymogen that undergoes autocatalytic cleavage at a low pH (pH < 2). Thus, in the stomach SHH is cleaved by the acid-dependent aspartic proteinase at the C-terminal side of the phenylalanine (at residue 200), suggesting that the addition of lipid is not required, perhaps facilitating its solubility in a more polar microenvironment. Nevertheless, whether SHH produced from the parietal cell is modified post-translationally with cholesterol or a fatty acid is not known.
Reprinted with permission from Merchant.6
Processing of Sonic Hedgehog
Perhaps because of difficulties in measuring SHH protein during development, most studies primarily have relied on messenger RNA (mRNA) levels and not protein to study SHH expression. Nevertheless, prior studies examining generation of SHH protein showed that the protein undergoes a complex series of processing steps that includes the initial generation of a 45-kilodalton precursor polypeptide, subsequent removal of the N-terminal 24 amino acid residue signal peptide, and then cleavage of the amino terminus to generate a 19-kilodalton protein that can be modified post-translationally by palmitate and cholesterol42, 43, 44, 45 (Figure 2). These studies performed initially in Drosophila showed that cholesterol transferase activity resides in the C-terminal portion of the Hedgehog molecule such that esterification of cysteine 198 by the transferase results in intramolecular autocatalytic cleavage of the 45-kilodalton precursor46 (Figure 2). Additional studies have shown that the extent of lipid modification modulates SHH diffusion away from the cell of origin. Apparently, a shorter range of diffusion correlates with a higher degree of lipid (palmitate) modification and membrane association.47, 48
By contrast, we showed in the adult mouse and human stomach that both SHH processing and gene expression are linked to acid secretion.28 Specifically, infusion of the hormone gastrin over 2 weeks using osmotic pumps stimulates SHH gene expression in a hypochlorhydric gastrin-deficient mouse in concert with re-establishing acid secretion.28 Moreover, post-translational processing of SHH precursor to its secreted form depends on cleavage by the acid-activated protease pepsin A generated from pepsinogen A. Thus, we concluded that generation of the biologically active form of SHH in the stomach is regulated. If gastric acidity is reduced, as a result of inhibition of acid secretion (omeprazole therapy) or loss of the parietal cell (atrophy), then pepsin A is not activated and most of the precursor SHH protein produced is not cleaved into its functionally active 19-kilodalton form.28 These observations are consistent with the finding that oxyntic gland atrophy (specifically loss of the parietal cell) correlates with reduced pepsinogen A to C ratios.38 More importantly, these observations suggest that SHH is processed within parietal cells. SHH co-localizes to the tubulovesicle fraction with the H+, K+-adenosine triphosphatase (ATPase) enzyme. With the addition of a secretogogue, movement of the SHH precursor to the canalicular membrane coincides with insertion of the proton pump into the apical membrane.49 This thesis would account for the ability of SHH processing and secretion to coincide with the production of gastric acid. Moreover, this mechanism would predict that a significant amount of SHH would be less lipid-modified and capable of diffusing both basolaterally and apically throughout the gastric gland and into the circulation.49 Indeed, we and others have found that blood levels of SHH peptide originate in part from the parietal cell50, 51 and can be detected in the circulation of human volunteers.52
Hedgehog Signaling in the Adult Stomach
Canonical HH signaling involves epithelial expression of ligand (typically SHH in the stomach), which subsequently binds to its receptor Patched (PTCH) and relieves its inhibitory influence on an adjacent transmembrane HH activator called Smoothened (SMO). Once SMO inhibition is relieved, glioma-associated protein 2 (GLI2) is processed to an activator form, translocates to the nucleus, and then binds to the promoters of HH effectors including PTCH, hedgehog-interacting protein (HHIP), and GLI1.53, 54 Thus, GLI1, PTCH, and HHIP are transcriptional read-outs of canonical HH signaling activity.55
The extracellular signals regulating shh gene expression in the stomach are not well defined but might correlate with those reported in other tissues. For example, during pancreatic development, shh expression appears to be regulated by activin A.56 During limb bud development, fibroblast growth factors and bone morphogenetic proteins regulate shh expression.57, 58 Shh null (shh-/-) mice do not survive past postnatal day 1.18 However, the stomachs of these mice were hyperplastic and further underscored that loss of HH signaling shows important functional consequences.18 Subsequent studies have been performed in adult mice using a H+,K+-ATPase-Cre transgene to delete the shh gene locus only in parietal cells. Conditional deletion of the shh gene resulted in parietal cell atrophy and foveolar hyperplasia.28, 59, 60 Indeed, SHH signaling is required for optimal H+,K+-ATPase expression.22 In addition, a prior study in a gastric cancer cell line showed that increased gastric acidity stimulates shh expression.61 Accordingly, modulators of gastric acid such as gastrin and somatostatin (SST) have been shown to modulate SHH levels and HH signaling.28, 49, 62, 63
Inflammation Regulates Gastric Acid Secretion and SHH
We previously examined modulation of gastric acid secretion by proinflammatory cytokines and reported that both gastrin and SST are regulated, albeit in a reciprocal manner, by cytokines in vivo and in primary cell cultures.64, 65 Interferon γ (IFNγ), a T1-helper cytokine, stimulated gastrin and inhibited SST, and interleukin-4 (IL4), a T2-helper cytokine, stimulated SST and inhibited gastrin.39 Thus, similar to the negative feedback regulation known to exist for gastrin and SST, immune modulators impart parallel control of these peptides and therefore acid secretion. Teleologically, it makes sense that the innate immune system regulates gastric acid because acid is one of the first defense mechanisms that is activated by the gastrointestinal tract to combat invading organisms. However, prior studies by Beales66 and other investigators67, 68, 69 have shown by using a rabbit primary culture system that either IL1β or tumor necrosis factor-α infusion into rodents suppresses acid secretion. Subsequently, more ominous implications became attributed to cytokine suppression of acid secretion when El-Omar et al70 and other investigators71, 72, 73 showed that IL1β, but not tumor necrosis factor-α polymorphisms, predispose human subjects to gastric atrophy and gastric cancer. Testing the significance of the polymorphism, Tu et al74 reported that transgenic overexpression of IL1β in mouse parietal cells induced gastric inflammation and dysplasia. By contrast, IFNγ polymorphisms do not appear to correlate with gastric atrophy.75 Indeed, we reported that proinflammatory cytokines show differential effects on SHH expression with IFNγ stimulating SHH expression and IL1β inhibiting expression when added acutely (6 h) to parietal cell cultures.63 It generally has been assumed that all proinflammatory cytokines generated during bacterial colonization exert the same effect on gastric cells. However, our results in primary parietal cell cultures coupled with differences in the association of cytokine polymorphisms support the likelihood that the effects of these proinflammatory cytokines on parietal cells are distinct.
SHH Regulates Gastrin and Gastric Acidity
To examine the impact of HH signaling in vivo, we generated a transgenic mouse that secreted the natural -inhibitor of HH ligands called HHIP expressed from the cell-specific H+,K+-ATPase β subunit promoter.62 Our results showed that loss of HH signaling in parietal cells, caused by the production of secreted HHIP, reduced H+,K+-ATPase gene expression and gastric acid.62 Normally, hypochlorhydria stimulates gastrin gene expression through a decrease in SST.76 Accordingly, we found coincident with increased plasma gastrin occurring in the hhip transgenic mice that sst gene expression also decreased. This result showed that modulation of HH signaling in parietal cells is sufficient to activate the normal feedback mechanisms typically attributed to gastrin and SST. Indeed, we reported that both antral G and D cells possess primary cilia, organelles protruding from the plasma membrane, which transduce HH signaling.77, 78 Therefore, gastric endocrine cells are capable of responding directly to the SHH ligand. We showed that transgenic overexpression of GLI2 suppresses gastrin gene expression.5 Thus, gastrin stimulates gastric acid and SHH expression whereas HH signaling suppresses gastrin expression. Taken together, the production of SHH by parietal cells and the ability of gastric endocrine cells to sense the ligand through primary cilia are consistent with a central role for HH signaling in the feedback regulation of gastric acidity.
Cross-Talk Between Gastric Epithelium and Mesenchyme
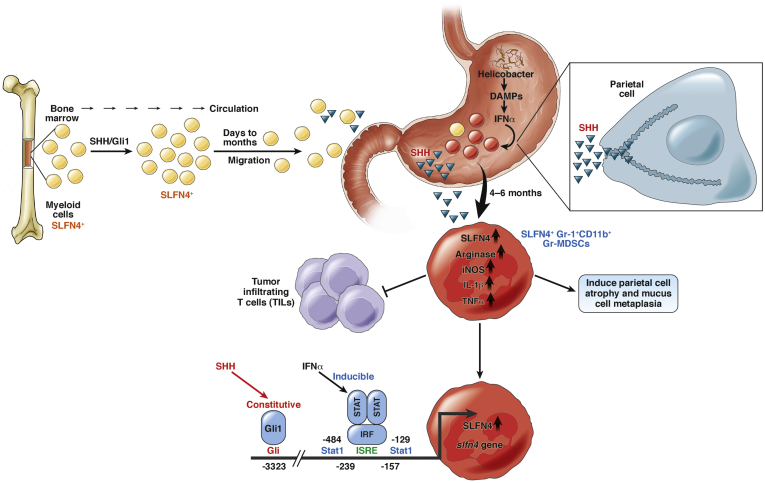
Canonical HH signaling typically involves cross-talk between epithelial cells that produce the ligands, for example, SHH, Indian hedgehog, and cells that express the receptor-signaling complexes, such as PTCH, SMO, HHIP, and transcription factors GLI1, GLI2, and GLI3. Therefore, to identify gastric cells that respond to HH ligands in the absence and presence of Helicobacter, we used the Gli-LacZ reporter mouse. The β-galactosidase complementary DNA was recombined into the gli1 gene locus to create heterozygous or homozygous genotypes.53 In the absence of a Helicobacter infection, we found that α-smooth muscle actin–positive myofibroblasts were the major population expressing the LacZ reporter.4 However, during a Helicobacter infection, the LacZ+ cells infiltrating the gastric mesenchyme were myeloid cells and correlated with parietal cell atrophy and the emergence of SPEM.4 Strikingly, when either the Gli1LacZ/+ or Gli1LacZ/LacZ mice were infected, they did not develop SPEM. This result showed that canonical HH signaling was required for SPEM.79 Use of microarray analysis to identify GLI1 target genes showed that induction of a myeloid differentiation factor called Schlafen 4 (SLFN4) contributed to the GLI1-dependent development of SPEM. However, the induction of slfn4 mRNA coincident with SPEM was time-dependent, and required 6 months to be expressed in wild-type mice or 4 months in the presence of constitutively elevated levels of SHH ligand (pCMVShh).4 Overexpression of SHH accelerated the development of SPEM, but only in the presence of a Helicobacter infection.51 Therefore, both SPEM and the appearance of SLFN4+ myeloid cells required GLI1. We concluded that HH signaling is required to polarize a subset of myeloid cells and transition gastric mucosa from a proinflammatory to a preneoplasia state, but only in the presence of the bacterial infection (Figure 3).
Figure 3.
Schematic of SLFN4-positive cells migrating from the bone marrow during a Helicobacter infection. SHH released by parietal cells into the circulation is sensed by SLFN4-positive myeloid cells (yellow cells). Presumably, the concentration of SHH is highest in the acid-secreting stomach (blue triangles), which encourages the SLFN4-positive cells to home to the infected stomach. Eventually, the SLFN4-positive myeloid cells become polarized to Gr-MDSCs (red cells) by tissue IFNα induced by DAMP signals that accumulate as a result of cellular atrophy during chronic Helicobacter infection. The genes expressed by SLFN4-positive-Gr-MDSCs are indicated (expanded red cell), as well as how slfn4 gene expression is regulated by both HH signaling (Gli1) and the inducible inflammatory signal (IFNα). Therefore, polarization to Gr-MDSCs can be achieved only in the infected stomach where the SLFN4-positive myeloid cells encounter increased IFNα inducing maximal SLFN4 levels. ISRE, interferon-stimulated response element.
Modified with permission from Ding et al.51
The heterogeneous populations of myeloid cells that emerge during chronic atrophic gastritis are phenotypically myeloid-derived suppressor cells (MDSCs). MDSCs show both monocytic (Mo-MDSC) and granulocytic (Gr-MDSC) features, suggesting that they might represent the reprogramming of monocytes and neutrophils recruited to the tissue.80 MDSCs suppress T-cell function by consuming L-arginine through arginase 1 and inducible nitric oxide synthase activated to generate reactive oxygen species. L-arginine is required for T-cell proliferation and its ability to block cancer growth.81 Therefore, the presence of MDSCs has been strongly linked to tumor promotion, owing to their immunosuppressive role once cancer has emerged.82 By contrast, our recent studies strongly have suggested that a subset of MDSCs appear during the preneoplastic phase of cancer development and require HH signaling.51
Schlafens are a family of molecules strongly induced by type 1 IFNs (IFNα), and their expression typically correlates with immune cell quiescence.83, 84 Specifically, SLFN4 modulates myelopoiesis.85 Coincident with the apoptosis of parietal cells, tissue levels of damage-associated molecular patterns (DAMPs) accumulate, culminating in increasing IFNα secretion from plasmacytoid-derived dendritic cells.51, 86 Toll-like receptors (TLRs) 3, 7, 8, and 9 are the intracellular TLRs that recognize DAMPs by initiating a complex cascade of signaling molecules (eg, myeloid differentiation primary response gene 88, interferon factor regulatory transcriptions, and signal transducer and activator of transcriptions) that ultimately induce expression of type 1 interferons (IFNα and IFNβ)87 (Figure 3). Recent studies have indicated that chronic Helicobacter infection in both mice and human beings induces TLR9 expression.88 Apparently, DAMPs and their subsequent activation of TLR9 are associated with immune suppression.89, 90 Moreover, there is an increased incidence of gastric neoplasia in subjects with TLR9 polymorphisms and H pylori infection.91, 92 Increased tissue levels of type I interferons can suppress inflammation.89 In addition, DAMPs have been implicated in the reprogramming of monocytic cells to become Mo-MDSCs.80 In addition, our results show that DAMP signals also polarize Gr-MDSCs as observed for Mo-MDSCs (Figure 3). In particular, the novelty of this observation is that Gr-MDSCs appear during the metaplastic phase of the transforming gastric mucosa before frank cancer emerges.
Collectively, the emergence of SLFN4+ MDSCs might be cogent biomarkers because the slfn4 promoter remains quiescent until both transcriptional regulators—one constitutive (GLI1) and one inducible (IRFs/STAT)—engage the promoter (Figure 3). In this way, immune suppressor function only becomes active under the appropriate conditions (ie, to dampen the chronic gastritis initiated by Helicobacter). The T-cell suppressor activity exerted by immature myeloid cells occurs because they restrict T-cell access to L-arginine, a substrate for the MDSC enzymes arginase 1 and inducible nitric oxide synthase.81 We showed previously that small interfering RNA knockdown of slfn4 significantly reduces arg1 and inos mRNA in SLFN4+ MDSCs,51 suggesting that SLFN4 is required for myeloid cells to acquire their immune-suppressor function.
Because GLI1 gene expression blocks maturation of an immature myeloid cell subpopulation, creating a gastric microenvironment favorable for metaplasia and transformation, we examined the pattern for SLFN4 homologs in human subjects.51, 93 Human SLFN 5, SLFN12, and SLFN12L show the closest homology to mouse SLFN4 protein (the slfn4 gene does not exist in the human genome). Consistent with the mouse model, we recently reported in a 13-year follow-up study that SLFN5 is increased most significantly in those subjects with intestinal metaplasia whose lesions progressed to gastric cancer.93 Although SLFN5 is expressed in myeloid cells, we found that its expression also occurred primarily in T cells.93 When we examined the expression pattern of SLFN12L, we found its expression correlated with the human surface markers for Gr-MDSCs.51 Therefore, human myeloid cells express SLFN12L as observed for SLFN4 in mice.51 Furthermore, we would predict that increased SLFN12L levels, like SLFN5, might predict those individuals with metaplasia who are more likely to develop gastric cancer.
Summary
HH signaling in the stomach plays a significant role in gastric development, homeostasis, and neoplastic transformation.6 Although extensive developmental literature on SHH protein and downstream targets exists, essentially none of the information was applied to the stomach, despite the evidence that SHH is highly expressed in gastric cancer cell lines.21 Although increased levels of SHH have been reported in gastric cancers, its specific role in gastric transformation remains elusive but carries significance because of the availability of HH antagonists. Here, we reviewed the role of HH signaling in normal gastric homeostasis, inflammation, and transformation. In particular, we highlighted our studies showing that the phenotype of infiltrating myeloid cells changes over time to become MDSCs and that the polarization requires HH signaling. More importantly, expression of GLI1, which targets SLFN4 (mice) and SLFN12L and SLFN5 (human beings), is an early indicator that the myeloid cells recruited during chronic inflammation have become polarized toward Gr-MDSCs, a cell type that appears to favor neoplastic development. In addition to MDSCs, other bone marrow–derived cells are recruited to the stomach and have been implicated in facilitating gastric transformation.24, 94, 95, 96 The ability to track these cell types in the preneoplastic state broadens options for more effective screening of subjects predisposed to eventually develop gastric cancer as well as to expand options for prophylactic therapy once atrophic gastritis develops, including antagonists of mTOR (mechanistic antagonist of rapamycin).97, 98, 99 Although Hedgehog antagonists have been used for other cancer types, their use in clinical trials for gastric cancer is still in its infancy.1, 31 Where initiated, those trials have focused on targeting CD44-positive gastric stem cells to treat metastatic disease.100
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding Supported by Public Health Service Grant (NIH) P01 DK062041. Dr Merchant was a recipient of the AGA R. Robert & Sally Funderburg Research Award in Gastric Cancer.
References
- 1.Yun J.I., Kim H.R., Park H. Small molecule inhibitors of the hedgehog signaling pathway for the treatment of cancer. Arch Pharm Res. 2012;35:1317–1333. doi: 10.1007/s12272-012-0801-8. [DOI] [PubMed] [Google Scholar]
- 2.Sahebjam S., Siu L.L., Razak A.A. The utility of hedgehog signaling pathway inhibition for cancer. Oncologist. 2012;17:1090–1099. doi: 10.1634/theoncologist.2011-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merchant A.A., Matsui W. Targeting Hedgehog–a cancer stem cell pathway. Clin Cancer Res. 2010;16:3130–3140. doi: 10.1158/1078-0432.CCR-09-2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Zaatari M., Kao J.Y., Tessier A. Gli1 deletion prevents helicobacter-induced gastric metaplasia and expansion of myeloid cell subsets. PLoS One. 2013;8:e58935. doi: 10.1371/journal.pone.0058935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saqui-Salces M., Coves-Datson E., Veniaminova N.A. Inflammation and Gli2 suppress gastrin gene expression in a murine model of antral hyperplasia. PLoS One. 2012;7:e48039. doi: 10.1371/journal.pone.0048039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merchant J.L. Hedgehog signalling in gut development, physiology and cancer. J Physiol. 2012;590:421–432. doi: 10.1113/jphysiol.2011.220681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Zimaity H.M., Ota H., Graham D.Y. Patterns of gastric atrophy in intestinal type gastric carcinoma. Cancer. 2002;94:1428–1436. doi: 10.1002/cncr.10375. [DOI] [PubMed] [Google Scholar]
- 8.Fox J.G., Wang T.C. Inflammation, atrophy, and gastric cancer. J Clin Invest. 2007;117:60–69. doi: 10.1172/JCI30111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu C., Cheng J., Hu S. Reduced proliferation and increased apoptosis of the SGC7901 gastric cancer cell line on exposure to GDC0449. Mol Med Rep. 2016;13:1434–1440. doi: 10.3892/mmr.2015.4677. [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Rahman O. Hedgehog pathway aberrations and gastric cancer; evaluation of prognostic impact and exploration of therapeutic potentials. Tumour Biol. 2015;36:1367–1374. doi: 10.1007/s13277-015-3216-6. [DOI] [PubMed] [Google Scholar]
- 11.Ruiz i Altaba A., Sanchez P., Dahmane N. Gli and hedgehog in cancer: tumours, embryos and stem cells. Nat Rev Cancer. 2002;2:361–372. doi: 10.1038/nrc796. [DOI] [PubMed] [Google Scholar]
- 12.Marigo V., Roberts D.J., Lee S.M. Cloning, expression, and chromosomal location of SHH and IHH: two human homologues of the Drosophila segment polarity gene hedgehog. Genomics. 1995;28:44–51. doi: 10.1006/geno.1995.1104. [DOI] [PubMed] [Google Scholar]
- 13.Katoh Y., Katoh M. Comparative genomics on Sonic hedgehog orthologs. Oncol Rep. 2005;14:1087–1090. [PubMed] [Google Scholar]
- 14.Litingtung Y., Lei L., Westphal H. Sonic hedgehog is essential to foregut development. Nat Genet. 1998;20:58–61. doi: 10.1038/1717. [DOI] [PubMed] [Google Scholar]
- 15.Shannon J.M., Hyatt B.A. Epithelial-mesenchymal interactions in the developing lung. Annu Rev Physiol. 2004;66:625–645. doi: 10.1146/annurev.physiol.66.032102.135749. [DOI] [PubMed] [Google Scholar]
- 16.Kim S.K., Melton D.A. Pancreas development is promoted by cyclopamine, a hedgehog signaling inhibitor. Proc Natl Acad Sci U S A. 1998;95:13036–13041. doi: 10.1073/pnas.95.22.13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willet S.G., Mills J.C. Stomach organ and cell lineage differentiation: from embryogenesis to adult homeostasis. Cell Mol Gastroenterol Hepatol. 2016;2:546–559. doi: 10.1016/j.jcmgh.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramalho-Santos M., Melton D.A., McMahon A.P. Hedgehog signals regulate multiple aspects of gastrointestinal development. Development. 2000;127:2763–2772. doi: 10.1242/dev.127.12.2763. [DOI] [PubMed] [Google Scholar]
- 19.Van Den Brink G.R., Hardwick J.C., Tytgat G.N. Sonic hedgehog regulates gastric gland morphogenesis in man and mouse. Gastroenterology. 2001;121:317–328. doi: 10.1053/gast.2001.26261. [DOI] [PubMed] [Google Scholar]
- 20.van den Brink G.R., Hardwick J.C., Nielsen C. Sonic hedgehog expression correlates with fundic gland differentiation in the adult gastrointestinal tract. Gut. 2002;51:628–633. doi: 10.1136/gut.51.5.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fukaya M., Isohata N., Ohta H. Hedgehog signal activation in gastric pit cell and in diffuse-type gastric cancer. Gastroenterology. 2006;131:14–29. doi: 10.1053/j.gastro.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 22.Stepan V., Ramamoorthy S., Nitsche H. Regulation and function of the sonic hedgehog signal transduction pathway in isolated gastric parietal cells. J Biol Chem. 2005;280:15700–15708. doi: 10.1074/jbc.M413037200. [DOI] [PubMed] [Google Scholar]
- 23.Shiotani A., Iishi H., Uedo N. Evidence that loss of sonic hedgehog is an indicator of Helicobater pylori-induced atrophic gastritis progressing to gastric cancer. Am J Gastroenterol. 2005;100:581–587. doi: 10.1111/j.1572-0241.2005.41001.x. [DOI] [PubMed] [Google Scholar]
- 24.Petersen C.P., Mills J.D., Goldenring J.R. Murine models of gastric corpus preneoplasia. Cell Mol Gastroenterol Hepatol. 2017;3:11–26. doi: 10.1016/j.jcmgh.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamaguchi H., Goldenring J.R., Kaminishi M. Identification of spasmolytic polypeptide expressing metaplasia (SPEM) in remnant gastric cancer and surveillance postgastrectomy biopsies. Dig Dis Sci. 2002;47:573–578. doi: 10.1023/a:1017920220149. [DOI] [PubMed] [Google Scholar]
- 26.Engevik A.C., Feng R., Choi E. The development of spasmolytic polypeptide/TFF2-expressing metaplasia (SPEM) during gastric repair is absent in the aged stomach. Cell Mol Gastroenterol Hepatol. 2016;2:605–624. doi: 10.1016/j.jcmgh.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suzuki H., Minegishi Y., Nomoto Y. Down-regulation of a morphogen (sonic hedgehog) gradient in the gastric epithelium of Helicobacter pylori-infected Mongolian gerbils. J Pathol. 2005;206:186–197. doi: 10.1002/path.1763. [DOI] [PubMed] [Google Scholar]
- 28.Zavros Y., Waghray M., Tessier A. Reduced pepsin a processing of sonic hedgehog in parietal cells precedes gastric atrophy and transformation. J Biol Chem. 2007;282:33265–33274. doi: 10.1074/jbc.M707090200. [DOI] [PubMed] [Google Scholar]
- 29.Tokhunts R., Singh S., Chu T. The full-length unprocessed hedgehog protein is an active signaling molecule. J Biol Chem. 2010;285:2562–2568. doi: 10.1074/jbc.M109.078626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh S., Wang Z., Liang Fei D. Hedgehog-producing cancer cells respond to and require autocrine Hedgehog activity. Cancer Res. 2011;71:4454–4463. doi: 10.1158/0008-5472.CAN-10-2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Konstantinou D., Bertaux-Skeirik N., Zavros Y. Hedgehog signaling in the stomach. Curr Opin Pharmacol. 2016;31:76–82. doi: 10.1016/j.coph.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saqui-Salces M., Merchant J.L. Hedgehog signaling and gastrointestinal cancer. Biochim Biophys Acta. 2010;1803:786–795. doi: 10.1016/j.bbamcr.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sierra R., Une C., Ramirez V. Association of serum pepsinogen with atrophic body gastritis in Costa Rica. Clin Exp Med. 2006;6:72–78. doi: 10.1007/s10238-006-0098-3. [DOI] [PubMed] [Google Scholar]
- 34.Iijima K., Sekine H., Koike T. Serum pepsinogen concentrations as a measure of gastric acid secretion in Helicobacter pylori-negative and -positive Japanese subjects. J Gastroenterol. 2005;40:938–944. doi: 10.1007/s00535-005-1677-x. [DOI] [PubMed] [Google Scholar]
- 35.Sipponen P., Ranta P., Helske T. Serum levels of amidated gastrin-17 and pepsinogen I in atrophic gastritis: an observational case-control study. Scand J Gastroenterol. 2002;37:785–791. [PubMed] [Google Scholar]
- 36.Nomura A.M., Kolonel L.N., Miki K. Helicobacter pylori, pepsinogen, and gastric adenocarcinoma in Hawaii. J Infect Dis. 2005;191:2075–2081. doi: 10.1086/430353. [DOI] [PubMed] [Google Scholar]
- 37.Kokkola A., Louhimo J., Puolakkainen P. Helicobacter pylori infection and low serum pepsinogen I level as risk factors for gastric carcinoma. World J Gastroenterol. 2005;11:1032–1036. doi: 10.3748/wjg.v11.i7.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shiotani A., Iishi H., Uedo N. Histologic and serum risk markers for noncardia early gastric cancer. Int J Cancer. 2005;115:463–469. doi: 10.1002/ijc.20852. [DOI] [PubMed] [Google Scholar]
- 39.Li P., He C., Sun L. Pepsinogen I and II expressions in situ and their correlations with serum pesignogen levels in gastric cancer and its precancerous disease. BMC Clin Pathol. 2013;13:22. doi: 10.1186/1472-6890-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roberts N.B. Review article: human pepsins - their multiplicity, function and role in reflux disease. Aliment Pharmacol Ther. 2006;24(Suppl 2):2–9. doi: 10.1111/j.1365-2036.2006.03038.x. [DOI] [PubMed] [Google Scholar]
- 41.Fujinaga M., Chernaia M.M., Tarasova N.I. Crystal structure of human pepsin and its complex with pepstatin. Protein Sci. 1995;4:960–972. doi: 10.1002/pro.5560040516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bumcrot D.A., Takada R., McMahon A.P. Proteolytic processing yields two secreted forms of sonic hedgehog. Mol Cell Biol. 1995;15:2294–2303. doi: 10.1128/mcb.15.4.2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wendler F., Franch-Marro X., Vincent J.P. How does cholesterol affect the way Hedgehog works? Development. 2006;133:3055–3061. doi: 10.1242/dev.02472. [DOI] [PubMed] [Google Scholar]
- 44.Goetz J.A., Suber L.M., Zeng X. Sonic Hedgehog as a mediator of long-range signaling. Bioessays. 2002;24:157–165. doi: 10.1002/bies.10056. [DOI] [PubMed] [Google Scholar]
- 45.Lee J.J., Ekker S.C., von Kessler D.P. Autoproteolysis in hedgehog protein biogenesis. Science. 1994;266:1528–1537. doi: 10.1126/science.7985023. [DOI] [PubMed] [Google Scholar]
- 46.Roelink H., Porter J.A., Chiang C. Floor plate and motor neuron induction by different concentrations of the amino-terminal cleavage product of sonic hedgehog autoproteolysis. Cell. 1995;81:445–455. doi: 10.1016/0092-8674(95)90397-6. [DOI] [PubMed] [Google Scholar]
- 47.Gritli-Linde A., Lewis P., McMahon A.P. The whereabouts of a morphogen: direct evidence for short- and graded long-range activity of hedgehog signaling peptides. Dev Biol. 2001;236:364–386. doi: 10.1006/dbio.2001.0336. [DOI] [PubMed] [Google Scholar]
- 48.Goetz J.A., Singh S., Suber L.M. A highly conserved amino-terminal region of sonic hedgehog is required for the formation of its freely diffusible multimeric form. J Biol Chem. 2006;281:4087–4093. doi: 10.1074/jbc.M511427200. [DOI] [PubMed] [Google Scholar]
- 49.Zavros Y., Orr M.A., Xiao C. Sonic hedgehog is associated with H+,K+-ATPase-containing membranes in gastric parietal cells and secreted with histamine stimulation. Am J Physiol Gastrointest Liver Physiol. 2008;295:G99–G111. doi: 10.1152/ajpgi.00389.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schumacher M.A., Donnelly J.M., Engevik A.C. Gastric Sonic Hedgehog acts as a macrophage chemoattractant during the immune response to Helicobacter pylori. Gastroenterology. 2012;142:1150–1159 e1156. doi: 10.1053/j.gastro.2012.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ding L., Hayes M.M., Photenhauer A. Schlafen 4-expressing myeloid-derived suppressor cells are induced during murine gastric metaplasia. J Clin Invest. 2016;126:2867–2880. doi: 10.1172/JCI82529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.El-Zaatari M., Daignault S., Tessier A. Plasma sHH levels reduced in pancreatic cancer patients. Pancreas. 2012;41:1019–1028. doi: 10.1097/MPA.0b013e31824a0eeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bai C.B., Auerbach W., Lee J.S. Gli2, but not Gli1, is required for initial SHH signaling and ectopic activation of the SHH pathway. Development. 2002;129:4753–4761. doi: 10.1242/dev.129.20.4753. [DOI] [PubMed] [Google Scholar]
- 54.Pan Y., Bai C.B., Joyner A.L. Sonic hedgehog signaling regulates Gli2 transcriptional activity by suppressing its processing and degradation. Mol Cell Biol. 2006;26:3365–3377. doi: 10.1128/MCB.26.9.3365-3377.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van den Brink G.R. Hedgehog signaling in development and homeostasis of the gastrointestinal tract. Physiol Rev. 2007;87:1343–1375. doi: 10.1152/physrev.00054.2006. [DOI] [PubMed] [Google Scholar]
- 56.van Eyll J.M., Pierreux C.E., Lemaigre F.P. SHH-dependent differentiation of intestinal tissue from embryonic pancreas by activin A. J Cell Sci. 2004;117:2077–2086. doi: 10.1242/jcs.01067. [DOI] [PubMed] [Google Scholar]
- 57.Zuniga A., Haramis A.P., McMahon A.P. Signal relay by BMP antagonism controls the SHH/FGF4 feedback loop in vertebrate limb buds. Nature. 1999;401:598–602. doi: 10.1038/44157. [DOI] [PubMed] [Google Scholar]
- 58.Khokha M.K., Hsu D., Brunet L.J. Gremlin is the BMP antagonist required for maintenance of SHH and Fgf signals during limb patterning. Nat Genet. 2003;34:303–307. doi: 10.1038/ng1178. [DOI] [PubMed] [Google Scholar]
- 59.Xiao C., Feng R., Engevik A.C. Sonic Hedgehog contributes to gastric mucosal restitution after injury. Lab Invest. 2013;93:96–111. doi: 10.1038/labinvest.2012.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xiao C., Ogle S.A., Schumacher M.A. Loss of parietal cell expression of Sonic hedgehog induces hypergastrinemia and hyperproliferation of surface mucous cells. Gastroenterology. 2010;138:550–561. doi: 10.1053/j.gastro.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dimmler A., Brabletz T., Hlubek F. Transcription of sonic hedgehog, a potential factor for gastric morphogenesis and gastric mucosa maintenance, is up-regulated in acidic conditions. Lab Invest. 2003;83:1829–1837. doi: 10.1097/01.lab.0000101729.25140.0c. [DOI] [PubMed] [Google Scholar]
- 62.El-Zaatari M., Zavros Y., Tessier A. Intracellular calcium release and protein kinase C activation stimulate sonic hedgehog gene expression during gastric acid secretion. Gastroenterology. 2010;139:2061–2071 e2062. doi: 10.1053/j.gastro.2010.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Waghray M., Zavros Y., Saqui-Salces M. Interleukin-1beta promotes gastric atrophy through suppression of Sonic Hedgehog. Gastroenterology. 2010;138:562–572. doi: 10.1053/j.gastro.2009.10.043. 572 e561–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zavros Y., Rathinavelu S., Kao J.Y. Treatment of Helicobacter gastritis with interleukin-4 requires somatostatin. Proc Natl Acad Sci U S A. 2003;100:12944–12949. doi: 10.1073/pnas.2135193100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zavros Y., Merchant J.L. Modulating the cytokine response to treat Helicobacter gastritis. Biochem Pharmacol. 2005;69:365–371. doi: 10.1016/j.bcp.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 66.Beales I.L. Effect of cytokines on acid secretion and gastrin secretion in Helicobacter pylori infection and aspirin-induced gastritis. Scand J Gastroenterol. 1998;33:1230–1232. doi: 10.1080/00365529850172638. [DOI] [PubMed] [Google Scholar]
- 67.Okumura T., Uehara A., Okamura K. Inhibition of gastric pepsin secretion by peripherally or centrally injected interleukin-1 in rats. Biochem Biophys Res Commun. 1990;167:956–961. doi: 10.1016/0006-291x(90)90616-u. [DOI] [PubMed] [Google Scholar]
- 68.Uehara A., Okumura T., Sekiya C. Interleukin-1 inhibits the secretion of gastric acid in rats: possible involvement of prostaglandin. Biochem Biophys Res Commun. 1989;162:1578–1584. doi: 10.1016/0006-291x(89)90855-3. [DOI] [PubMed] [Google Scholar]
- 69.Wallace J.L., Keenan C.M., Cucala M. Mechanisms underlying the protective effects of interleukin 1 in experimental nonsteroidal anti-inflammatory drug gastropathy. Gastroenterology. 1992;102:1176–1185. [PubMed] [Google Scholar]
- 70.El-Omar E.M., Carrington M., Chow W.H. Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398–402. doi: 10.1038/35006081. [DOI] [PubMed] [Google Scholar]
- 71.Furuta T., El-Omar E.M., Xiao F. Interleukin 1beta polymorphisms increase risk of hypochlorhydria and atrophic gastritis and reduce risk of duodenal ulcer recurrence in Japan. Gastroenterology. 2002;123:92–105. doi: 10.1053/gast.2002.34156. [DOI] [PubMed] [Google Scholar]
- 72.Garza-Gonzalez E., Bosques-Padilla F.J., El-Omar E. Role of the polymorphic IL-1B, IL-1RN and TNF-A genes in distal gastric cancer in Mexico. Int J Cancer. 2005;114:237–241. doi: 10.1002/ijc.20718. [DOI] [PubMed] [Google Scholar]
- 73.Atsuta Y., Ito L.S., Oba-Shinjo S.M. Associations of TNF-A-1031TT and -857TT genotypes with Helicobacter pylori seropositivity and gastric atrophy among Japanese Brazilians. Int J Clin Oncol. 2006;11:140–145. doi: 10.1007/s10147-005-0549-y. [DOI] [PubMed] [Google Scholar]
- 74.Tu S., Bhagat G., Cui G. Overexpression of interleukin-1beta induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell. 2008;14:408–419. doi: 10.1016/j.ccr.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rad R., Dossumbekova A., Neu B. Cytokine gene polymorphisms influence mucosal cytokine expression, gastric inflammation, and host specific colonisation during Helicobacter pylori infection. Gut. 2004;53:1082–1089. doi: 10.1136/gut.2003.029736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brand S.J., Stone D. Reciprocal regulation of antral gastrin and somatostatin gene expression by omeprazole-induced achlorhydria. J Clin Invest. 1988;82:1059–1066. doi: 10.1172/JCI113662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Saqui-Salces M., Keeley T.M., Grosse A.S. Gastric tuft cells express DCLK1 and are expanded in hyperplasia. Histochem Cell Biol. 2011;136:191–204. doi: 10.1007/s00418-011-0831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saqui-Salces M., Dowdle W.E., Reiter J.F. A high-fat diet regulates gastrin and acid secretion through primary cilia. FASEB J. 2012;26:3127–3139. doi: 10.1096/fj.11-197426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Goldenring J.R., Nam K.T. Oxyntic atrophy, metaplasia, and gastric cancer. Prog Mol Biol Transl Sci. 2010;96:117–131. doi: 10.1016/B978-0-12-381280-3.00005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Millrud C.R., Bergenfelz C., Leandersson K. On the origin of myeloid-derived suppressor cells. Oncotarget. 2017;8:3649–3665. doi: 10.18632/oncotarget.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gabrilovich D.I., Ostrand-Rosenberg S., Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12:253–268. doi: 10.1038/nri3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bronte V., Brandau S., Chen S.H. Recommendations for myeloid-derived suppressor cell nomenclature and characterization standards. Nat Commun. 2016;7:12150. doi: 10.1038/ncomms12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Schwarz D.A., Katayama C.D., Hedrick S.M. Schlafen, a new family of growth regulatory genes that affect thymocyte development. Immunity. 1998;9:657–668. doi: 10.1016/s1074-7613(00)80663-9. [DOI] [PubMed] [Google Scholar]
- 84.Puck A., Aigner R., Modak M. Expression and regulation of Schlafen (SLFN) family members in primary human monocytes, monocyte-derived dendritic cells and T cells. Results Immunol. 2015;5:23–32. doi: 10.1016/j.rinim.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.van Zuylen W.J., Garceau V., Idris A. Macrophage activation and differentiation signals regulate schlafen-4 gene expression: evidence for Schlafen-4 as a modulator of myelopoiesis. PLoS One. 2011;6 doi: 10.1371/journal.pone.0015723. e15723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Panda S.K., Kolbeck R., Sanjuan M.A. Plasmacytoid dendritic cells in autoimmunity. Curr Opin Immunol. 2016;44:20–25. doi: 10.1016/j.coi.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 87.Yamamoto M., Takeda K. Current views of toll-like receptor signaling pathways. Gastroenterol Res Pract. 2010;2010:240365. doi: 10.1155/2010/240365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Otani K., Tanigawa T., Watanabe T. Toll-like receptor 9 signaling has anti-inflammatory effects on the early phase of Helicobacter pylori-induced gastritis. Biochem Biophys Res Commun. 2012;426:342–349. doi: 10.1016/j.bbrc.2012.08.080. [DOI] [PubMed] [Google Scholar]
- 89.Varga M.G., Piazuelo M.B., Romero-Gallo J. TLR9 activation suppresses inflammation in response to Helicobacter pylori infection. Am J Physiol Gastrointest Liver Physiol. 2016;311:G852–G858. doi: 10.1152/ajpgi.00175.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hernandez C., Huebener P., Schwabe R.F. Damage-associated molecular patterns in cancer: a double-edged sword. Oncogene. 2016;35:5931–5941. doi: 10.1038/onc.2016.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Varga M.G., Shaffer C.L., Sierra J.C. Pathogenic Helicobacter pylori strains translocate DNA and activate TLR9 via the cancer-associated cag type IV secretion system. Oncogene. 2016;35:6262–6269. doi: 10.1038/onc.2016.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang X., Xue L., Yang Y. TLR9 promoter polymorphism is associated with both an increased susceptibility to gastric carcinoma and poor prognosis. PLoS One. 2013;8:e65731. doi: 10.1371/journal.pone.0065731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Companioni Napoles O., Tsao A.C., Sanz-Anquela J.M. SCHLAFEN 5 expression correlates with intestinal metaplasia that progresses to gastric cancer. J Gastroenterol. 2017;52:39–49. doi: 10.1007/s00535-016-1202-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Donnelly J.M., Engevik A., Feng R. Mesenchymal stem cells induce epithelial proliferation within the inflamed stomach. Am J Physiol Gastrointest Liver Physiol. 2014;306:G1075–G1088. doi: 10.1152/ajpgi.00489.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Petersen C.P., Weis V.G., Nam K.T. Macrophages promote progression of spasmolytic polypeptide-expressing metaplasia after acute loss of parietal cells. Gastroenterology. 2014;146:1727–1738 e1728. doi: 10.1053/j.gastro.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Buzzelli J.N., Chalinor H.V., Pavlic D.I. Il33 is a stomach alarmin that initiates a skewed Th2 response to injury and infection. Cell Mol Gastroenterol Hepatol. 2015;1:203–221. doi: 10.1016/j.jcmgh.2014.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Goldenring J.R. Gastric intestinal metaplasia and tamoxifen: can we reverse the inevitable? Dig Dis Sci. 2014;59:1078–1079. doi: 10.1007/s10620-014-3088-4. [DOI] [PubMed] [Google Scholar]
- 98.Choi E., Hendley A.M., Bailey J.M. Expression of activated Ras in gastric chief cells of mice leads to the full spectrum of metaplastic lineage transitions. Gastroenterology. 2016;150:918–930 e913. doi: 10.1053/j.gastro.2015.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Syu L.-Y., Zhao X., Zhang Y. Invasive mouse gastric adenocarcinomas arising from Lgr5+ stem cells are dependent on crosstalk between the Hedgehog/GLI2 and mTOR pathways. Oncotarget. 2016;7:10255–10270. doi: 10.18632/oncotarget.7182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yoon C., Park D.J., Schmidt B. CD44 expression denotes a subpopulation of gastric cancer cells in which Hedgehog signaling promotes chemotherapy resistance. Clin Cancer Res. 2014;20:3974–3988. doi: 10.1158/1078-0432.CCR-14-0011. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]