Abstract
Background
Parental perception of their infants and confidence/beliefs about their parenting are among the most salient factors influencing outcomes of preterm infants.
Objectives
The purpose of this study was to assess the psychometric properties of scores on the Neonatal Intensive Care Unit Parent Belief Scale (NICU PBS) in a sample of mothers and fathers of preterm infants receiving intensive care. The NICU PBS is a rating instrument designed to assess parental beliefs about their premature infant and their role during hospitalization.
Methods
The sample consisted of 245 mothers and 143 fathers. As part of the Creating Opportunities for Parent Empowerment (COPE) trial, participants completed the NICU PBS four to eight days after NICU admission and again approximately four days prior to discharge. Validation data were obtained at various times throughout the study. Confirmatory factor analysis was used to evaluate the NICU PBS factor structure.
Results
A three-factor solution was accepted (Parental Role Confidence, Parent-Baby Interaction, and Knowledge of the NICU). Reliability of scores on the total scale and subscales was high; Cronbach’s alpha ranged from .75 to .91. Test-retest correlations ranged from .84 to .92. Younger maternal age, birth of another child, and return to work within the past 12 months, and lower stress, depression, and anxiety were all significantly associated with higher scores on all subscales and the total score. Lower education, lower household income, receipt of Medicaid, and non-White race were associated with higher scores on the Parent Role Confidence subscale and total. Lower household income and receipt of Medicaid were associated with higher Parent-Baby Interaction scores.
Discussion
The NICU PBS can be used reliably with mothers and fathers of premature infants who are hospitalized in the NICU, and it may be a useful scale in predicting parental stress, depression, and anxiety.
Keywords: neonatal intensive care, parenting, preterm infants, reliability, validity
In 2010, an estimated 14.9 million infants (11.1%) worldwide were prematurely born. The highest preterm birth rates occurred in sub-Saharan Africa and South Asia. Although rates tend to be highest in low-income countries, several high-income countries (e.g., U.S. and Austria) ranked among the higher preterm birth rates across the globe in 2010 (Blencowe et al., 2012). Overall, preterm birth rates have remained stable or increased over the last decade throughout the world; however, survival rates vary drastically between low- and high-income countries (Beck et al., 2010; Blencowe et al., 2012). These infants and their families spend days, weeks, and even months in the Neonatal Intensive Care Unit (NICU), which results in substantial psychological and economic burden for families and health care systems.
A number of adverse outcomes are associated with premature birth and parenting. These outcomes include an increased risk for poor parent mental health (e.g., anxiety, depression, post-traumatic stress disorder; Brooks, Rowley, Broadbent, & Petrie, 2012; Melnyk, Feinstein, & Fairbanks, 2006; Treyvaud et al., 2010; Zelkowitz, Na, Wang, Bardin, & Papageorgiou, 2011), dysfunctional parenting (Bagner, Sheinkopf, Vohr, & Lester, 2010; Gray, Edwards, O’Callaghan, & Cuskelly, 2012), negative parent-infant interactions (Bagner et al., 2010; Cho, Holditch-Davis, & Miles, 2008; Gray et al., 2012), and child emotional, behavioral, and cognitive problems that often persist through adolescence (Huhtala et al., 2011; Zelkowitz et al., 2011). It is well documented that the NICU is often stressful for parents of premature infants due to the presence of frightening medical equipment, unfamiliar staff, restrictive hospital policies, the infant’s appearance, behaviors and health, and a disruption in parental role and parent-infant interactions (Erdeve et al., 2009; Melnyk, Crean, Feinstein, & Fairbanks, 2008). The tendency for some parents of premature infants to be overprotective, depressed, and anxious contributes to the increased occurrence of developmental and behavioral problems among these children who are already at risk for delays due to their prematurity (Zelkowitz et al., 2011).
One of the most salient factors in predicting outcomes among preterm children is early parent-infant interaction, which some researchers suggest may be the mediating role in the relationship between parental anxiety and infant behavioral and developmental outcomes (Forcada-Guex, Pierrehumbert, Borghini, Moessinger, & Muller-Nix, 2006). Parents’ beliefs regarding their role and their infant’s behaviors, characteristics, and vulnerability also have been associated with their stress, anxiety, and depression, often persisting well beyond discharge from the NICU (Melnyk et al., 2008). Currently, there are no validated instruments to assess these important constructs in parents of premature infants.
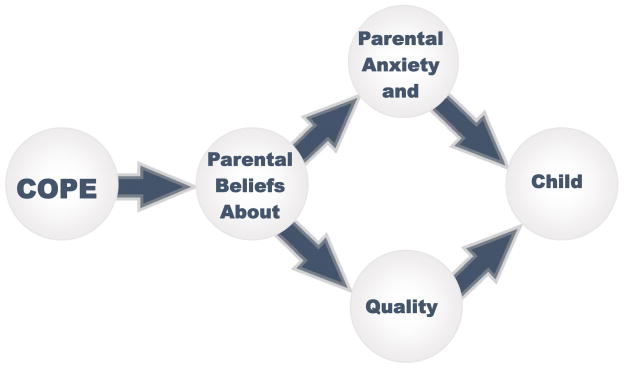
The Creating Opportunities for Parent Empowerment (COPE) program was originally created for parents of hospitalized and critically ill children to strengthen their cognitive beliefs and confidence about parenting their ill children, and enhance their ability to help their children cope with hospitalization (Melnyk, 1994; Melnyk et al., 2004). Because the program showed positive effects on outcomes with parents of hospitalized/critically ill children, it was refined for parents of premature infants. COPE is a manualized intervention that consists of four audiotaped educational sessions, and a workbook that contains activities to help parents put into practice what they are learning in the educational sessions. Educational information in the COPE program includes content that: (a) teaches parents about what to expect in the behaviors and physical characteristics of their premature infants; and (b) how best to parent them and enhance their development. Workbook activities include parents learning their infant’s awake states, recording their infant’s stress signals, and noting the best actions to comfort their infant. Findings from two intervention studies testing the program indicated that the effects of the COPE program on parental outcomes were mediated by parents’ beliefs about their infant and their parental role, as measured by the NICU Parental Belief Scale (see Figure 1). This was consistent with findings from other intervention studies using various versions of COPE with parents of hospitalized and critically ill children that supported the mediating effect of parental beliefs about their children and their roles, assessed with the Parental Belief Scale, on parental and child outcomes (Melnyk, 1994; Melnyk et al., 2004; Melnyk, Crean, Feinstein, Fairbanks, & Alpert-Gillis, 2007).
Figure 1.
Effects of the COPE Program on Parental and Child Outcomes
Purpose
The purpose of this study was to examine the psychometric properties of the Neonatal Intensive Care Unit Parental Beliefs Scale (NICU PBS) used in the COPE educational and skills building intervention for parents of premature infants, and investigate whether these beliefs differed between mothers and fathers. The NICU PBS is an adaptation of the original PBS designed for use with parents of hospitalized and critically ill children (Melnyk, 1995). Content validity for the original PBS was established with eight clinical nurse specialists. Reliability estimated using Cronbach’s alpha was .86 for the total scale and .76 and .84 for the subscales (Beliefs about Child Behaviors and Parental Role Beliefs, respectively; Melnyk, 1994; Melnyk, 1995). The original PBS psychometric analyses were carried out only with mothers and supported the two-factor structure of the instrument. In this study, data were obtained from fathers in order to examine the psychometric properties of their data and determine if there was measurement invariance with data from mothers.
Theoretical Framework
Self-regulation theory contends that knowing what to expect in a stressful situation enhances the formation of cognitive schema that supports information processing as the event unfolds and guides responses and behaviors during the event (Johnson, 1999). Knowing and attending to concrete objective aspects of a stressful experience facilitates information processing as the event unfolds. As a result, coping ability is enhanced (Johnson, Fieler, Jones, Wlasowicz, & Mitchell, 1997).
The original PBS was designed to assess parental beliefs about their hospitalized children and parental role in an intervention study with mothers whose young children faced an unplanned hospital admission. The original PBS was adapted from a 15 item beliefs scale based on self-regulation theory (Johnson, 1999). Previous COPE studies in which the PBS was used report both direct and indirect associations between higher parental beliefs and less negative maternal mood states, fewer child externalizing adjustment problems, reduced maternal anxiety, and increased maternal participation in their children’s care (Melnyk, 1994; Melnyk et al., 2007). The positive effects of COPE on parent outcomes were found to be mediated through their cognitive beliefs about their hospitalized/critically ill children and their role (Melnyk et al., 2007). Therefore, it was posited that providing parents of infants in the NICU with concrete objective information about the behaviors and characteristics of their premature infants as compared to normal full-term infants, one component of the COPE intervention, would help them to form a clear, unambiguous schema about what to realistically expect in their premature infants. This clear schema was then expected to lead to stronger beliefs about their ability to understand and predict their infants’ behaviors. The schema, in turn, was predicted to result in an enhanced ability to cope because parents could anticipate their infant’s needs and have greater parenting confidence (stronger beliefs in their parenting abilities). Thus, parents who received COPE were expected to have less anxiety, depression, and stress related to the NICU (the emotional outcome of coping) and demonstrate a higher quality of parenting (the functional outcome of coping) than parents who did not receive this information. As a result of less anxiety and a higher quality of parenting, it was predicted that the premature infants would be discharged earlier and have better outcomes (see Figure 1).
Methods
Participants and Settings
A total of 240 mothers and 240 fathers were targeted for recruitment in the COPE NICU study (120 mothers and 120 fathers at each site). Sample size for evaluation of the original COPE intervention was based on a power of .8 at the .05 level of significance, the medium to large positive effects found for the COPE program on the primary outcome variable of infant cognitive development in the pilot study and the statistical procedures to be used in data analysis; a sample size of 144 mothers and 144 fathers (72 mothers and 72 fathers in each study group) was required to test the study hypotheses (Cohen, 1992). Recruiters screened 1278 premature births, with 562 meeting the eligibility criteria. Of the 562 eligible births, 254 (45.2%) families refused participation, with the majority of parents stating that they were too stressed or tired to participate, they wanted to only concentrate on their infant, or they believed that participation would take time away from the other children at home. Recruiters were unable to contact the parents of 48 (8.5%) premature infants who met eligibility criteria. The final sample after randomization comprised 258 mothers (147 in the COPE group and 113 in the comparison group) and 154 fathers/significant others (81 in the COPE group and 73 in the comparison group).
Parents were recruited from two NICUs: (a) URMC’s 55-bed NICU, which is part of a 720-bed medical center in Upstate New York (the site of the pilot study); and (b) Crouse Hospital’s (CH) 60-bed NICU, which is part of a 566-bed medical center in Syracuse, New York. The CH NICU was chosen as the second site because of similar practices of the two NICUs. Mothers and fathers, ages 18 years and older, who could read and speak English, who never had another infant admitted to NICU, and whose infants met the following criteria were eligible for participation: (a) gestational age of 26 to 34 weeks inclusive; (b) birth weight of less than 2500 grams; (c) anticipated survival; (d) singleton birth; (e) no severe handicapping conditions; (f) not small for gestational age; (g) no Grade III or IV intraventricular hemorrhage (IVH); and (h) born at the study sites. Parents were excluded from the study if they made a personal decision to withdraw from the study, or if their infant had positive drug testing. The study was conducted between September 2001 and October 2004.
The sample for this psychometric evaluation consisted of 245 mothers, ranging from 18 to 43 years (M = 27.8) and 143 fathers, who ranged in age from 18 to 49 years (M = 30.7), who had completed the NICU PBS scale for the first time when their infant was four to eight days old. Eighty five percent of the mothers and 89% of fathers had a high school or college education, and 56% had a family income of $40,000 or less. A majority of the mothers and fathers were Caucasian (68.1% and 76.9%, respectively). The number of male (n = 119) and female (n = 128) infants in the study was approximately even. The mean gestational age of the premature infants was 31.3 weeks (SD = 2.45; range = 26 to 35 weeks) and the infants ranged in birth weight from 710 grams to 2570 grams (M = 1658.31 grams; SD = 473.39). The mean illness severity index level using CRIB scores was 1.7 (SD = 2.42; range = 0–10). Total length of stay in the NICU averaged 35.09 days (SD = 27.57; range = 5–163 days).
Procedure
The NICU PBS was completed four to eight days after admission to the NICU (time 1) and, again at approximately four days prior to discharge (time 2). Mothers and biological fathers completed the NICU PBS independently. The study was approved by the University’s Institutional Review Board.
Item Adaptation
The current study with NICU parents used an adapted version of the original PBS that was created for parents of hospitalized and critically ill children (Melnyk, 1994; Melnyk et al., 2004). The original PBS was revised to assess parental beliefs among NICU parents of prematurely born children. Based on the theoretical framework for the original PBS instrument, it was expected that the confirmatory factor analysis of the NICU PBS items would yield two subscales (Beliefs about Baby and Confidence in Parental Role). The NICU PBS consists of 18 statements about parental beliefs regarding their hospitalized infant (e.g., “I know what behaviors to expect in my infant while he (or she) is in the hospital”; “I know what my baby will do when he/she is stressed.”) and their role as parents (e.g., “I am clear about the things that I can do to best help my infant.”; “I feel comfortable in caring for my baby in the NICU.”). Mothers and fathers were asked to indicate agreement with each item on a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The items are summed to yield a total score ranging from 18 to 90, with higher scores indicating more positive parental beliefs about their infant and greater confidence in their parental role. Eight neonatal specialists supported the content validity of the revised overall scale and two subscales.
Statistical Methods
Data from time 1 were used to confirm the factor structure, reliability, and validity of the resulting subscales and total score. Time 1 and time 2 data were used for the test-retest analysis. For multigroup confirmatory factor analysis (CFA), the first step is to ascertain whether the model with the same factor structure fits the data for each group. If so, then the groups’ data can be pooled and tested for measurement invariance. However, model fit statistics should not be the only criteria used in determining factor structure, reliability, and validity of the scale items (Browne & Cudeck, 1992; Myung, 2000; Pitt, Myung, & Zhang, 2002). Model fit criteria should be balanced with reliability estimates that reflect the accuracy and precision of the measurement instrument (Suhr & Shay, n.d.).
Reporting practices for CFA typically include selection of the input matrix and estimation method, examination of the distributional characteristics of the data (e.g., outliers, univariate and multivariate normality) based on the planned estimation method, and analysis and handling of missing data (Boomsma, 2000; Jackson, Gillaspy, & Purc-Stephenson, 2009; Schreiber, Amaury, Stage, Barlow, & King, 2006). A covariance matrix structure with maximum likelihood estimation was specified using Mplus V7. Data were screened for normality and outliers and no data transformations were required. Missing data were minimal and were handled through multiple imputation for maximum likelihood estimation.
Factorability was assessed by examining the item correlation matrices for mothers and fathers. Scree plots for data from the mothers and fathers were examined to determine if the a priori two-factor solution was supported. Measurement invariance using multiple group analysis was carried out testing a series of three nested models based on a two-factor solution (Sousa, West, Moser, Harris, & Cook, 2012). The first model of the nested series was the least restrictive: the intercepts, factor loadings, and residual variances were free across groups and factor means fixed at zero for both groups. The second model factor loadings were constrained to be equal across groups, intercepts and residual variances were freely estimated, and factor means fixed at zero for both groups. In the last model (most restrictive), the intercepts and factor loadings were constrained to be equal across groups, residual variances were freely estimated, and factor means set to zero for mothers and freely estimated for fathers. For all models the correlation between factors was set to 0. The likelihood ratio test was used to compare the fit between each pair of the nested models (χ2 difference test). If these differences are significant, it implies that the constraints imposed by the more restrictive model may be too stringent.
Cronbach’s alpha coefficients were calculated for each subscale and the total score. Test-retest correlations were computed and convergent and discriminant validity examined. The variables included for the convergent and discriminant validity correlational analyses (selected based on a literature review and theoretical relevance) were: parental age, education, income, use of Medicaid, race, parental stress, depression, state anxiety, any subsequent birth, mother employment, both parents participating in the study, routine prenatal care, report of a consistent health care provider, high-risk pregnancy, gravidity, Clinical Risk Index for Babies (CRIB) scores (de Courcy-Wheeler et al., 1995), birth weight, and NICU length of stay.
Results
Factor Structure
Although the covariance matrix was analyzed, for ease of interpretation of the interrelationships among items, Table 1 presents the correlation matrices for mothers and fathers along with the associated means and standard deviations. The majority of items for both parents had correlation coefficients ≥ .3; thus, the study proceeded with the confirmatory factor analysis. Measurement invariance was not observed for any of the two-factor models tested indicating that the factor structure for mothers and fathers differed. Inspection of the fit statistics (χ2, RMSEA, SRMR, and CFI) revealed poor fit to the data for the three models tested under a two-factor solution. Removing items with low factor loadings for both groups, and repeating the two-factor solution and analyzing a single factor structure, did not result in any significant improvement in model fit (data not shown). Therefore, based on the scree plot, a three-factor model was specified with configural invariance between models for mothers and fathers; results were compared to the nested two-factor model findings. For this model, the intercepts, factor loadings, and residual variances were free across groups; factor means fixed at zero for both groups, and the correlation between factors was set to 0. The most parsimonious model from the two-factor solution was then tested against the alternative three-factor model. The fit statistics for the three two-factor models and the three-factor model are presented in Table 2. Although the three-factor solution resulted in substantial improvement in model fit, it still did not meet the minimum criteria for good fit. The findings of the model fit analyses must be interpreted with caution. These results may be unstable because the ratio of observations to parameters was 6.5:1 for mothers and 3.8:1 for fathers; below the recommended 10:1 ratio. As a result, as stated above, this study sought to balance model fit criteria with the reliability and validity results. Standardized factor loadings and associated standard errors for each item in the final three-factor solution for mothers and fathers are shown in Table 3. For the majority of items, the item loadings were congruent between mothers and fathers, suggesting that the final factor structure may not differ between parents.
Table 1.
Correlations, Means, and Standard Deviations for NICU PBS Items by Parent Gender
| PB1 | PB2 | PB3 | PB4 | PB5 | PB6 | PB7 | PB8 | PB9 | PB10 | PB11 | PB12 | PB13 | PB14 | PB15 | PB16 | PB17 | PB18 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PB1 | 1.0 | .33 | .25 | .67 | .48 | .29 | .49 | .20 | .38 | .29 | .10 | .36 | .34 | .42 | .38 | .13 | .31 | .27 | 3.15 | .99 |
| PB2 | .22 | 1.0 | .40 | .35 | .50 | .49 | .27 | .44 | .46 | .36 | .31 | .32 | .58 | .09 | .27 | .11 | .14 | .34 | 3.81 | .99 |
| PB3 | .34 | .38 | 1.0 | .35 | .37 | .34 | .16 | .32 | .30 | .24 | .21 | .13 | .38 | .15 | .27 | .06 | .16 | .26 | 3.95 | .88 |
| PB4 | .58 | .28 | .47 | 1.0 | .52 | .32 | .48 | .32 | .45 | .40 | .24 | .40 | .43 | .31 | .37 | .13 | .42 | .29 | 3.32 | .96 |
| PB5 | .37 | .46 | .45 | .51 | 1.0 | .55 | .35 | .35 | .50 | .51 | .33 | .29 | .55 | .30 | .43 | .16 | .26 | .33 | 3.44 | .94 |
| PB6 | .29 | .36 | .42 | .36 | .51 | 1.0 | .33 | .44 | .49 | .35 | .42 | .23 | .54 | .23 | .30 | .14 | .17 | .36 | 3.61 | .87 |
| PB7 | .42 | .23 | .39 | .51 | .40 | .33 | 1.0 | .34 | .41 | .40 | .28 | .31 | .39 | .53 | .35 | .16 | .43 | .34 | 3.34 | .91 |
| PB8 | .28 | .36 | .43 | .37 | .42 | .44 | .39 | 1.0 | .48 | .32 | .35 | .26 | .47 | .12 | .35 | .19 | .25 | .36 | 2.88 | 1.10 |
| PB9 | .40 | .37 | .52 | .54 | .56 | .54 | .43 | .54 | 1.0 | .48 | .32 | .45 | .61 | .18 | .52 | .22 | .40 | .47 | 3.46 | .94 |
| PB10 | .33 | .30 | .36 | .44 | .46 | .46 | .40 | .45 | .62 | 1.0 | .52 | .27 | .38 | .17 | .36 | .10 | .27 | .39 | 3.54 | .86 |
| PB11 | .25 | .27 | .30 | .35 | .46 | .35 | .35 | .44 | .48 | .52 | 1.0 | .14 | .31 | .12 | .18 | .13 | .10 | .23 | 3.39 | .93 |
| PB12 | .37 | .13 | .17 | .40 | .37 | .27 | .37 | .31 | .46 | .42 | .44 | 1.0 | .48 | .23 | .43 | .28 | .50 | .38 | 3.40 | .94 |
| PB13 | .36 | .36 | .42 | .51 | .61 | .44 | .47 | .45 | .65 | .52 | .53 | .52 | 1.0 | .20 | .45 | .29 | .40 | .54 | 3.49 | .91 |
| PB14 | .36 | .07 | .07 | .34 | .34 | .13 | .35 | .23 | .33 | .36 | .31 | .54 | .42 | 1.0 | .30 | .09 | .30 | .28 | 3.86 | .77 |
| PB15 | .29 | .20 | .23 | .39 | .42 | .31 | .39 | .35 | .45 | .43 | .39 | .52 | .59 | .51 | 1.0 | .29 | .38 | .66 | 3.49 | .87 |
| PB16 | .18 | .17 | .20 | .10 | .24 | .26 | .16 | .22 | .34 | .21 | .18 | .31 | .33 | .31 | .39 | 1.0 | .31 | .19 | 4.51 | .62 |
| PB17 | .36 | .14 | .25 | .44 | .37 | .24 | .25 | .24 | .36 | .38 | .36 | .56 | .44 | .41 | .52 | .17 | 1.0 | .48 | 3.38 | .89 |
| PB18 | .23 | .24 | .23 | .35 | .38 | .28 | .35 | .31 | .41 | .47 | .48 | .39 | .53 | .36 | .51 | .20 | .57 | 1.0 | 3.22 | .89 |
| M | 3.19 | 3.74 | 3.80 | 3.30 | 3.37 | 3.61 | 3.50 | 3.02 | 3.48 | 3.57 | 3.45 | 3.59 | 3.65 | 3.89 | 3.70 | 4.51 | 3.47 | 3.44 | ||
| SD | .98 | 1.01 | .91 | .98 | 1.03 | 1.02 | .87 | 1.09 | .96 | .96 | .96 | .92 | .90 | .86 | .92 | .66 | .92 | .91 |
Note. Correlations for fathers are presented above the diagonal, and correlations for mothers are presented below the diagonal. Means and standard deviations fathers are presented in the vertical columns; means and standard deviations for mothers are presented in the horizontal rows. Items are listed in Table 3.
Table 2.
Fit Statistics: Measurement Invariance of 2-Factor and 3-Factor Models for the NICU Parental Beliefs Scale
| Model | Number of Factors | Description | χ2 (df) | RMSEA | SRMR | CFI | Comparison | Δχ2 (Δdf) | p |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | Intercepts, factor loadings, and residual variances free across groups; factor means fixed at zero in all groups | 3044.99 (290) | .22 | .33 | .27 | - | ||
| 2 | 2 | Factor loadings equal across groups; intercepts; residual variances free; factor means fixed at zero in all groups | 3356.67 (286) | .24 | .28 | .18 | 2 vs. 1 | 311.68 (4) | < .0005 |
| 3 | 2 | Intercepts and factors loadings equal across groups; residual variances free; factor means zero for mothers and free for fathers | 3422.02 (302) | .23 | .28 | .17 | 3 vs. 2 | 65.35 (16) | < .0005 |
| 4 | 3 | Configural invariance | 490.33 (133) | .08 | .20 | .87 | 4 vs. 1 | 254.66 (157) | < .0001 |
Note. CFI = comparative fit index; df = degrees of freedom; RMSEA = root mean square error of approximation; SRMR = standardized root mean square residual.
N = 388. Factor correlations were set to 0 in all models.
Table 3.
Parental Beliefs Scalea: Standardized Factor Structure (Three-factor Model with Configural Invariance)
| Item | I. Parental Role Confidence
|
II. Parent-Baby Interaction
|
III. Knowledgeb
|
Uniqueness
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mother
|
Father
|
Mother
|
Father
|
Mother
|
Father
|
|||||||||
| Est. | (SE) | Est. | (SE) | Est. | (SE) | Est. | (SE) | Est. | (SE) | Est. | (SE) | Mother | Father | |
| 1 Characteristics/behaviors common to premature babies in NICU | .71 | (.04) | .80 | (.04) | .53 | .39 | ||||||||
| 2 What I do for my baby will be what’s best to help him/her deal with being in the NICU | .74 | (.02) | .80 | (.02) | .84 | .56 | ||||||||
| 3 Feel comfortable caring for my baby in the NICU | .68 | (.04) | .54 | (.06) | .52 | .59 | ||||||||
| 4 Know what characteristics and behaviors to expect while baby is in the NICU | .85 | (.03) | .85 | (.04) | .31 | .28 | ||||||||
| 5 Sure about things I can do to help my baby get through NICU experience | .79 | (.03) | .79 | (.03) | .50 | .41 | ||||||||
| 6 Sure that I can meet baby’s emotional needs while in NICU | .72 | (.03) | .73 | (.04) | .60 | .42 | ||||||||
| 7 Know why baby has characteristics and behaviors he/she does in the NICU | .70 | (.04) | .66 | (.05) | .43 | .50 | ||||||||
| 8 Feel confident in telling nurses and doctors what will best help my baby while in the NICU | .71 | (.03) | .66 | (.05) | .70 | .78 | ||||||||
| 9 Clear about how to help take care of my baby in the NICU | .87 | (.02) | .80 | (.03) | .30 | .38 | ||||||||
| 10 Know how my baby will respond to me while in the NICU | .76 | (.03) | .66 | (.05) | .47 | .48 | ||||||||
| 11 Sure about how my emotions will affect baby while in the hospital | .67 | (.04) | .42 | (.07) | .55 | .74 | ||||||||
| 12 Clear about how my baby will react when getting too much stimulation in NICU | .74 | (.03) | .65 | (.05) | .44 | .55 | ||||||||
| 13 Sure about things I can do to make my baby feel most secure while in the NICU | .83 | (.02) | .81 | (.03) | .29 | .33 | ||||||||
| 14 Know how my baby’s appearance and behaviors are different from a full-term baby | .64 | (.04) | .42 | (.07) | .48 | .51 | ||||||||
| 15 Know the best times to communicate or interact with my baby | .78 | (.03) | .74 | (.04) | .38 | .39 | ||||||||
| 16 Confident in asking doctors and nurses questions about baby’s medical condition | .44 | (.05) | .39 | (.08) | .37 | .33 | ||||||||
| 17 Know what my baby will do when stressed | .70 | (.04) | .62 | (.06) | .48 | .53 | ||||||||
| 18 Clear about what my baby will look or act like when ready to communicate with me | .71 | (.03) | .75 | (.04) | .46 | .39 | ||||||||
Note. Est. = factor loading; SE = standard error.
Copyright 1997 by Bernadette Mazurek Melnyk, PhD, RN-CS-PNP, FAAN; used with permission.
Knowledge of Characteristics & Behaviors in the NICU.
Reliability
Reliability estimated using Cronbach’s alpha is shown in Table 4 for each subscale and the total score on time 1 and time 2 for mothers and fathers. The coefficients ranged from .79 to .93. The instrument demonstrated sensitivity to change over the baby’s NICU hospitalization as evidenced by statistically significant increases in each subscale score and the total score at time 2. The mean Parental Role Confidence score increased from 26.12 (SD = 5.20) to 29.23 (SD = 4.21) (p < .0001). The mean Parent-Baby Interaction score was 27.85 (SD = 5.43) at time 1 compared to a mean of 30.67 (SD = 4.64) at time 2 (p < .0001). The mean Knowledge about the NICU increased from 9.92 (SD = 2.34) at time 1 to 11.45 (SD = 2.00) at time 2 (p < .0001). The mean total PBS score at time 1 was 63.90 (SD = 10.49) and increased to a mean of 71.35 (SD = 9.02) at time 2 (p < .0001).
Table 4.
Cronbach’s Alpha Coefficients by Time: Mothers and Fathers
| Scale | Mothers
|
Fathers
|
||
|---|---|---|---|---|
| Time 1 (n = 245) | Time 2 (n = 241) | Time 1 (n = 143) | Time 2 (n =134) | |
| Parent Role Confidence | .85 | .87 | .83 | .80 |
| Parent-Baby Interaction | .85 | .86 | .78 | .83 |
| Knowledgea | .75 | .79 | .78 | .83 |
| PBS (total score) | .91 | .93 | .90 | .91 |
Knowledge of Characteristics/Behaviors in the NICU.
Concurrent and Predictive Validity
For convergent and discriminant validity assessment, correlation analysis of the time 1 data was used for assessment of the NICU PBS with maternal demographic characteristics (age, education, employment status), mental health, stress, pregnancy history variables (gravidity, high-risk status, subsequent pregnancy in 12 months), and baby outcome variables (CRIB scores, birth weight, NICU length of stay). These variables were selected based on a literature review and theoretical relevance (Table 5). Higher total PBS scores were associated with younger maternal age, lower education, lower income, receipt of Medicaid, minority status, mothers’ employment, no biological father in the study, higher gravidity, and having had another child in the past 12 months, shorter NICU length of stay, and lower stress, anxiety, and depression.
Table 5.
Correlations with the NICU Parental Belief Scales
| Correlate | PRC | PBI | Knowledge | PBS |
|---|---|---|---|---|
| Maternal age (years) | −.27*** | −.22** | −.13* | −.26*** |
| Maternal education | −.24** | −.09 | .02 | −.15* |
| Income | −.25*** | −.17** | −.06 | −.21** |
| On public assistance/Medicaid | .26*** | .20* | .10 | .24** |
| White | −.26*** | −.11 | −.11 | −.20** |
| Parental Stress Scale | −.23*** | −.28*** | −.19** | −.28*** |
| Beck Depression Inventory | −.25*** | −.18** | −.20** | −.24*** |
| State Anxiety Inventory | −.31*** | −.25*** | −.28*** | −.32*** |
| Subsequent child in past 12 months | .15* | .18** | .13* | .19** |
| Mother employed | .17** | .13* | .07 | .16* |
| Biological father in study | −.18** | −.17** | −.07 | −.18** |
| Prenatal care | −.11 | −.06 | −.10 | −.10 |
| Gravidity | .11 | .09 | .13* | .12* |
| CRIB score | −.11 | −.04 | −.07 | −.08 |
| Birth weight | .03 | .08 | .04 | .06 |
| NICU length of stay | −.11 | −.12 | −.11 | −.13* |
| Bayley Mental Development Index | .06 | .02 | .004 | .03 |
Note. PRC = Parental Role Confidence; PBI = Parent-Baby Interaction; PBS = Parental Beliefs Scale (total score).
N = 388.
Knowledge of characteristics and behaviors in the NICU.
p < .05;
p < .01;
p < .0001.
Discussion
This study provides preliminary evidence of the validity and reliability of the final 18-item NICU PBS. Confirmatory factor analysis demonstrated that the model fit indices were not unanimous in indicating overall good fit of the data to the models that were estimated, although the three-factor solution was the closest. High Cronbach’s alpha coefficients, however, indicated that the reliabilities of the total scale and subscales for mothers and fathers are very good. Results suggest that the NICU PBS can be used reliably with mothers and fathers of premature infants who are hospitalized in the NICU, and that it may be a useful scale in identifying individuals at risk for parental stress, depression, and anxiety in parents of preterm infants. Parents with unrealistic beliefs/expectations about parenting and child development frequently exhibit higher levels of stress due to the pressure to accomplish unrealistic goals (Bornstein, Cole, Haynes, Huan, & Park, 2010). Meanwhile, consistent with previous findings, high parental beliefs/confidence appear to be protective against parental stress (Liu, Chen, Yeh, & Hsieh, 2012), depression (Leahy-Warren, McCarthy, & Corcoran, 2012), and anxiety (Reck, Noe, Gerstenlauer, & Stehle, 2012).
The availability of a measure that can be used to examine parental beliefs about their hospitalized infants and their ability to parent them is a significant contribution for parent/child researchers, particularly due to the predictive relationship between the NICU PBS and other psychological measures (Melnyk et al., 2008). Use of the NICU PBS as a screening tool for enrollment in an intervention program or individualized care would be a fast, easy, and low-cost solution to identifying individuals who are at risk for experiencing significant parental stress, depression, and anxiety while in the NICU. Findings from prior studies using the COPE intervention with parents of prematurely born children have demonstrated that COPE strengthens parents’ beliefs about their infant and their parental role, leading to less stress, anxiety, and depressive symptoms during and after hospitalization. COPE could be one potential intervention option for those parents with low NICU PBS scores (see Figure 1).
Several unexpected correlations were found between the NICU PBS and other study variables. Surprisingly, characteristics of participants typically at high risk for poor parenting and child outcomes (non-White, young parents with low education and household income who receive Medicaid) were associated with higher NICU PBS total scores. Several possible explanations are provided. Typically, older and more educated parents with higher socioeconomic status tend to have higher levels of parenting knowledge (Bornstein et al., 2010; Morawska, Winter, & Sanders, 2009). However, more educated parents also may have higher expectations for themselves and, consequently, rate themselves harder on parenting as evidenced by the lower parental belief scores among more educated parents (Morawska et al., 2009). Additionally, previous research indicates that beliefs/confidence in parenting are not always associated with knowledge of child development and parenting. Therefore, they are not necessarily predictive of parenting quality, particularly in predominantly White, well-educated, middle-class families (Conrad, Gross, Fogg, & Ruchala, 1992; Hess, Teti, & Hussey-Gardner, 2004; Morawska, et al., 2009). The correlations among the NICU PBS total score and parent characteristics indicate a need to assess parenting and child development knowledge along with parental beliefs/confidence when screening parents for enrollment in a parenting intervention. Assessment of parent knowledge may be especially important when using the NICU PBS with non-White participants, who tend to overestimate their parenting abilities (Hess et al., 2004).
The results of previous intervention studies in various populations have consistently demonstrated the important meditational role of parental beliefs on key outcome measures, including anxiety, depression, and stress (Melnyk, 1994; Melnyk et al., 2007). Consistent with the COPE program’s proposed theoretical model, the beneficial effects of the COPE program on depression, anxiety, and stress in the NICU for parents of premature infants operate indirectly by strengthening parental beliefs about what to expect regarding their preterm baby’s characteristics/behaviors and how to parent them. Therefore, this evidence supports self-regulation theory. Findings from our prior studies that indicate that cognitive beliefs can be impacted with an educational-behavioral intervention, and that cognitive beliefs mediate the effects of the COPE intervention on parents’ emotional and functional coping outcomes (Melnyk, 1994; Melnyk et al., 2007).
Limitations
An important limitation to this study must be considered. Although the NICU PBS has good psychometric properties in this sample, approximately two thirds of the participants were Caucasian and over 85% had at least a high school education. Therefore, some caution must be taken when interpreting PBS NICU scores obtained from parents from more diverse populations. Future research should focus on testing the validity and reliability of the NICU PBS in diverse cultural populations.
Conclusion
The NICU PBS is a valid and reliable instrument that can be used to investigate the effect of various parent education programs on numerous outcomes, such as parent and child mental health along with child behavior and development. A better understanding of the beliefs held by parents of premature infants may facilitate the development or implementation of programs for this highly vulnerable population and ultimately benefit both parent and infant outcomes.
Acknowledgments
The authors acknowledge funding support for this study from NIH/National Institute of Nursing Research: R01#05077.
Footnotes
Note to Karina:
Table 3: as set up, there is a line return after the last character in each cell entry for the “Item” column. I think it makes the table more readable, but may not be worth the extra space it takes up. Also, as shown, the table note is on the third page of this three page table.
Table 5: the columns with numeric entries should be decimal aligned. (Thanks for your help with this detail.)
The authors have no conflicts of interest to report.
Contributor Information
Bernadette Melnyk, Ohio State University.
Krista L. Oswalt, Arizona State University
Kimberly Sidora-Arcoleo, Ohio State University.
References
- Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Parenting intervention for externalizing behavior problems in children born premature: An initial examination. Journal of Developmental and Behavioral Pediatrics. 2010;31:209–216. doi: 10.1097/DBP.0b013e3181d5a294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Van Look PFA. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bulletin of the World Health Organization. 2010;88:31–38. doi: 10.2471/BLT.08.062554. doi: http://dx.doi.org/10.1590/S0042-96862010000100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Lawn JE. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. The Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- Boomsma A. Reporting analyses of covariance structures. Structural Equation Modeling. 2000;7:461–483. doi: 10.1207/S15328007SEM0703_6. [DOI] [Google Scholar]
- Bornstein MH, Cote LR, Haynes OM, Hahn CS, Park Y. Parenting knowledge: Experiential and sociodemographic factors in European American mothers of young children. Developmental Psychology. 2010;46:1677–1693. doi: 10.1037/a0020677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S, Rowley S, Broadbent E, Petrie KJ. Illness perception ratings of high-risk newborns by mothers and clinicians: Relationship to illness severity and maternal stress. Health Psychology. 2012;31:632–639. doi: 10.1037/a0027591. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1992;21:230–258. doi: 10.1177/0049124192021002005. [DOI] [Google Scholar]
- Cho J, Holditch-Davis D, Miles MS. Effects of maternal depressive symptoms and infant gender on the interactions between mothers and their medically at-risk infants. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2008;37:58–70. doi: 10.1111/j.1552-6909.2007.00206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Conrad B, Gross D, Fogg L, Ruchala P. Maternal confidence, knowledge, and quality of mother-toddler interactions: A preliminary study. Infant Mental Health Journal. 1992;13:353–362. doi: 10.1002/1097-0355(199224)13:4<353::AID-IMHJ2280130410>3.0.CO;2-#. [DOI] [Google Scholar]
- de Courcy-Wheeler RH, Wolfe CD, Fitzgerald A, Spencer M, Goodman JD, Gamsu HR. Use of the CRIB (clinical risk index for babies) score in prediction of neonatal mortality and morbidity. Archives of Diseases in Children. 1995;73:F32–F36. doi: 10.1136/fn.73.1.f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdeve O, Arsan S, Canpolat FE, Ertem IO, Karagol BS, Turmen T. Does individual room implemented family-centered care contribute to mother–infant interaction in preterm deliveries necessitating neonatal intensive care unit hospitalization? American Journal of Perinatology. 2009;26:159–164. doi: 10.1055/s-0028-1095186. [DOI] [PubMed] [Google Scholar]
- Forcada-Guex M, Pierrehumbert B, Borghini A, Moessinger A, Muller-Nix C. Early dyadic patterns of mother-infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118:e107–e114. doi: 10.1542/peds.2005-1145. [DOI] [PubMed] [Google Scholar]
- Gray PH, Edwards DM, O’Callaghan MJ, Cuskelly M. Parenting stress in mothers of preterm infants during early infancy. Early Human Development. 2012;88:45–49. doi: 10.1016/j.earlhumdev.2011.06.014. [DOI] [PubMed] [Google Scholar]
- Hess CR, Teti DM, Hussey-Gardner B. Self-efficacy and parenting of high-risk infants: The moderating role of parent knowledge of infant development. Journal of Applied Developmental Psychology. 2004;25:423–437. [Google Scholar]
- Huhtala M, Korja R, Lehtonen L, Haataja L, Lapinleimu H PIPARI Study Group. Parental psychological well-being and cognitive development of very low birth weight infants at 2 years parental psychological well-being and cognitive outcome in VLBW infants. Acta Pædiatrica. 2011;100:1555–1560. doi: 10.1111/j.1651-2227.2011.02428.x. [DOI] [PubMed] [Google Scholar]
- Jackson DL, Jr, Gillaspy JA, Jr, Purc-Stephenson R. Reporting practices in confirmatory factor analysis: An overview and some recommendations. Psychological Methods. 2009;14:6–23. doi: 10.1037/a0014694. [DOI] [PubMed] [Google Scholar]
- Johnson JE, Fieler VK, Jones LS, Wlasowicz GS, Mitchell ML. Self-regulation theory: Applying theory to your practice. Pittsburgh, PA: Oncology Nursing Press; 1997. [PubMed] [Google Scholar]
- Johnson JE. Self-regulation theory and coping with physical illness. Research in Nursing & Health. 1999;22:435–448. doi: 10.1002/(SICI)1098-240X(199912)22:6<435::AID-NUR2>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- Leahy-Warren P, McCarthy G, Corcoran P. First-time mothers: Social support, maternal parental self-efficacy and postnatal depression. Journal of Clinical Nursing. 2012;21:388–397. doi: 10.1111/j.1365-2702.2011.03701.x. [DOI] [PubMed] [Google Scholar]
- Liu CC, Chen YC, Yeh YP, Hsieh YS. Effects of maternal confidence and competence on maternal parenting stress in newborn care. Journal of Advanced Nursing. 2012;68:908–918. doi: 10.1111/j.1365-2648.2011.05796.x. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Feinstein N, Fairbanks E. Two decades of evidence to support implementation of the COPE program as standard practice with parents of young unexpectedly hospitalized/critically ill children and premature infants. Pediatric Nursing. 2006;32:475–481. [PubMed] [Google Scholar]
- Melnyk BM. Coping with unplanned childhood hospitalization: Effects of informational interventions on mothers and children. Nursing Research. 1994;43:50–55. [PubMed] [Google Scholar]
- Melnyk BM, Alpert-Gillis L, Feinstein NF, Crean HF, Johnson J, Fairbanks E, Corbo-Richert B. Creating opportunities for parent empowerment: Program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics. 2004;113:e597–e607. doi: 10.1542/peds.113.6.e597. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Crean HF, Feinstein NF, Fairbanks E. Maternal anxiety and depression after a premature infant’s discharge from the neonatal intensive care unit: Explanatory effects of the creating opportunities for parent empowerment program. Nursing Research. 2008;57:383–394. doi: 10.1097/NNR.0b013e3181906f59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk BM. Coping with unplanned childhood hospitalization: The mediating functions of parental beliefs. Journal of Pediatric Psychology. 1995;20:299–312. doi: 10.1093/jpepsy/20.3.299. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Crean HF, Feinstein NF, Fairbanks E, Alpert-Gillis LJ. Testing the theoretical framework of the COPE program for mothers of critically ill children: An integrative model of young children’s post-hospital adjustment behaviors. Journal of Pediatric Psychology. 2007;32:463–474. doi: 10.1093/jpepsy/jsl033. [DOI] [PubMed] [Google Scholar]
- Morawska A, Winter L, Sanders MR. Parenting knowledge and its role in the prediction of dysfunctional parenting and disruptive child behaviour. Child: Care, Health and Development. 2009;35:217–226. doi: 10.1111/j.1365-2214.2008.00929.x. [DOI] [PubMed] [Google Scholar]
- Myung IJ. The importance of complexity in model selection. Journal of Mathematical Psychology. 2000;44:190–204. doi: 10.1006/jmps.1999.1283. [DOI] [PubMed] [Google Scholar]
- Pitt MA, Myung IJ, Zhang S. Toward a method of selecting among computational models of cognition. Psychological Review. 2002;109:472–491. doi: 10.1037/0033-295X.109.3.472. [DOI] [PubMed] [Google Scholar]
- Reck C, Noe D, Gerstenlauer J, Stehle E. Effects of postpartum anxiety disorders and depression on maternal self-confidence. Infant Behavior & Development. 2012;35:264–272. doi: 10.1016/j.infbeh.2011.12.005. [DOI] [PubMed] [Google Scholar]
- Schreiber JB, Amaury N, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. Journal of Educational Research. 2006;99:323–338. doi: 10.3200/JOER.99.6.323-338. [DOI] [Google Scholar]
- Sousa KH, West SG, Moser SE, Harris JA, Cook SW. Establishing measurement invariance: English and Spanish Paediatric Asthma Quality of Life Questionnaire. Nursing Research. 2012;61:171–180. doi: 10.1097/NNR.0b013e3182544750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suhr D, Shay M. Guidelines for reliability, confirmatory and exploratory factor analysis. n.d Retrieved from http://www.wuss.org/proceedings09/09WUSSProceedings/papers/anl/ANL-SuhrShay.pdf.
- Treyvaud K, Anderson VA, Lee KJ, Woodward LJ, Newnham C, Anderson PJ. Parental mental health and early social-emotional development of children born very preterm. Journal of Pediatric Psychology. 2010;35:768–777. doi: 10.1093/jpepsy/jsp109. [DOI] [PubMed] [Google Scholar]
- Zelkowitz P, Na S, Wang T, Bardin C, Papageorgiou A. Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age maternal anxiety in the NICU. Acta Pædiatrica. 2011;100:700–704. doi: 10.1111/j.1651-2227.2010.02128.x. [DOI] [PubMed] [Google Scholar]