Abstract
Background:
Patient-centered care requires knowledge of patients’ goals of care (GoC) on the part of health care providers (HCPs). Whether HCPs caring for in-center hemodialysis patients meet this criterion is uncertain.
Objective:
We designed and conducted a GoC survey among patients and HCPs within a single in-center hemodialysis (ICHD) program to determine whether HCPs have an understanding of their patients’ GoC.
Design:
This was a prospective comparative quantitative survey study.
Setting:
The study included a single Canadian maintenance ICHD center.
Participants:
These included hemodialysis patients and their primary nephrologists, nurses, social workers, pharmacists, and dietitians.
Methods and Measurements:
Two surveys, one for patients and another for primary HCPs, were designed, piloted, and administered. For each participating patient, HCPs consisted of the primary nephrologist, nurse, social worker, pharmacist, and dietitian. Surveys included questions pertaining to 7 GoC themes. Patient-HCP agreement on the importance of each domain individually and the most important domain overall was assessed with kappa statistics. Factors influencing agreement were assessed with logistic regression in a secondary analysis.
Results:
A total of 173 patients were invited to participate, of whom 137 (79%) completed surveys. Fifty HCPs completed 623 corresponding surveys: 132 by physicians, 112 by nurses, 126 by pharmacists, 127 by social workers, and 126 by dietitians. A total of 70.1% and 78.8% of patients agreed with the importance of and would feel comfortable having GoC discussions, respectively, with their HCPs; 42.7% of physicians reported not having provided prognostic information to the corresponding patient. Patient-HCP agreement regarding GoC was poor (all κ < .25, all P values > .05). In adjusted analyses, only patients choosing “Be Cured” as the most important GoC was significantly associated with poorer HCP-patient agreement than expected (odds ratio, 0.04; 95% confidence interval, 0.01-0.18).
Limitations:
This is a single-center study involving only ICHD patients.
Conclusions:
HCP perceptions of GoC did not agree with patients’ reported GoC. This study suggests the need for the design and validation of interventions to improve HCPs’ understanding of their patients’ GoC.
Keywords: end-stage renal disease, hemodialysis, goals of care
Abrégé
Mise en contexte:
Pour offrir des soins qui sont axés sur les patients, il importe que les professionnels de la santé connaissent les objectifs de ceux-ci en ce qui concerne les soins qui leur seront prodigués. Quant à savoir si les soins prodigués par les professionnels de la santé aux patients pratiquant l’hémodialyse en centre hospitalier satisfont ce critère, la réponse est incertaine.
Objectifs de l’étude:
Nous avons préparé et mené un sondage sur les objectifs en matière de soins auprès des patients et des professionnels de la santé au sein d’un programme d’hémodialyse en centre hospitalier pour déterminer si les fournisseurs de soins sont bien au fait des objectifs de soins de leurs patients.
Cadre et type d’étude:
L’étude prospective, comparative et quantitative a été menée par sondage au sein d’une seule unité d’hémodialyse en centre hospitalier canadienne.
Participants:
Le bassin de répondants était constitué de patients sous hémodialyse et de leur néphrologue principal, ainsi que des infirmières, des travailleurs sociaux, des pharmaciens et des diététistes pratiquant dans l’unité d’hémodialyse concernée par l’étude et ayant de près ou de loin prodigué des soins à ces patients.
Méthodologie:
Deux versions d’un sondage, une première destinée aux patients et l’autre aux principaux fournisseurs de soins, ont été rédigées, pré-testées, et administrées. Nous avons sondé chaque patient, son néphrologue principal, son infirmière, son travailleur social, son pharmacien ainsi que son diététiste. Les sondages comportaient des questions relatives à sept thèmes reliés aux objectifs des patients en matière de soins. L’accord des patients et des fournisseurs de soins sur l’importance de chacun des thèmes ainsi que sur le thème qu’ils considéraient comme le plus important des sept ont été évalués par la méthode d’analyse statistique kappa. Les facteurs influençant l’entente patient-fournisseur de soins a fait l’objet d’une analyse secondaire par régression logistique.
Résultats:
Un total de 173 patients ont été invités à répondre au sondage, desquels 137 (79%) ont rempli le questionnaire. Les fournisseurs de soins, au nombre de 50, ont rempli un total de 623 questionnaires correspondants, soit 132 questionnaires remplis par les médecins, 112 par les infirmières, 126 par les pharmaciens, 127 par les travailleurs sociaux et 126 par les diététistes. Parmi les réponses fournies par les patients, 70.1% ont mentionné qu’il était important de discuter de leurs objectifs en matière de soins, et 78.8% se sont dits à l’aise avec l’idée d’avoir une telle discussion avec leurs fournisseurs de soins. Les médecin ont rapporté, dans une proportion de 42.7%, ne pas avoir communiqué les informations relatives au pronostic à leurs patients correspondants. L’accord patient-fournisseur de soins en regard des objectifs en matière de soins s’est avéré faible (toutes les valeurs d’analyses kappa à moins de 0.25 et toutes les valeurs de p à plus de 0.05). Dans les analyses ajustées, seuls les patients ayant choisi « être guéri » comme objectif le plus important en matière de soins ont été associés de façon significative avec un accord plus faible que prévu entre les vues du patient et la perception de son fournisseur de soins (rapport de cotes: 0.04 ; IC 95 % entre 0.01 et 0.18).
Limites de l’étude:
Cette étude s’est effectuée au sein d’un seul centre de soin et n’implique que des patients sous hémodialyse traités en centre hospitalier.
Conclusions:
La perception des fournisseurs de soins en matière d’objectifs de soins des patients s’est avérée bien loin des préoccupations réelles de ceux-ci rapportées dans le questionnaire. Cette étude suggère que des mesures d’intervention validées devraient être mises en œuvre de façon à améliorer la compréhension des fournisseurs de soins envers les besoins et des objectifs de leurs patients en matière de soins.
What Was Known Before
Having a good understanding of patients’ goals of care (GoC) is a critical element in the shared decision-making process and important in avoiding unnecessary admissions to hospital, invasive procedures, suffering, and prolongation of the dying process.
What This Add
Health care providers’ understanding of their hemodialysis patients’ GoC was found to have poor agreement with their patients’ reported GoC. This finding supports the importance of frequent and effective goals of care discussions and illness education for this population.
Introduction
Shared decision making requires health care providers (HCPs) to understand the goals patients have for their care that allows recommendation of consistent treatment plans.1 Concurrently, patients must have an understanding of their illness to meaningfully reflect on their goals of care (GoC) and effectively participate in shared decision making. Clarity and transparency regarding GoC are particularly relevant within the dialysis population, given a high level of comorbid illness, variable prospects for renal transplantation, and high mortality risk. The consequences of not understanding dialysis patients’ GoC include unnecessary admissions to hospital, invasive procedures, suffering, and prolongation of the dying process.2
The prior work has operationalized the general concept of GoC into 7 distinct themes—be cured, live longer, improve function, maintain function, achieve life goals, be comfortable, and provide support to family members.3 These have been used to develop and validate survey tools for assessing patients’ GoC in several health care settings.4,5 Using these GoC themes, the primary objective of the current study was to examine the level of agreement between patients and their HCPs with respect to the importance of each GoC theme pertaining to dialysis treatment.
Methods
Study Participants
All patients receiving maintenance in-center hemodialysis (ICHD) on July 1, 2014, at Sunnybrook Health Sciences Centre in Toronto, Canada, were considered potentially eligible to participate. For each patient, we identified 5 primary HCPs, including the primary nephrologist, dialysis nurse, pharmacist, dietitian, and social worker, and requested that they participate in the study. Both patients and HCPs were recruited in person with patients recruited first. Patients who had been receiving dialysis for less than 90 days, those with insufficient cognitive capacity, those with both insufficient English fluency and without available translation services, and those who were unable or unwilling to give informed consent were excluded. The latter 3 factors were assessed by consensus of the patients’ HCPs. For efficiency of data collection, we did not seek to enroll home hemodialysis, satellite hemodialysis, or peritoneal dialysis patients.
Survey Development and Piloting
Details of the prior identification of the 7 GoC themes and the development and validation of patients and HCP survey instruments are described in supplemental Appendices 1 to 5. We developed 2 pen-and-paper–based survey instruments, one for administration to patients and another for their primary HCPs (Supplemental Appendices 2 and 4). The patient survey consisted of 4 sections: demographics, background information on patient’s experience and perceptions, 7 GoC domains for patients to choose, and final items relating to patients’ willingness to engage in further, more detailed, GoC discussions. For the GoC theme selection, we asked patients to first identify any of the 7 that they felt represented their goals for dialysis treatment and then to choose the one that was most important to them. For patients who had physical difficulty filling out the survey, either because of poor vision or inability to write, research personnel read the questions to the patients and wrote their answers down on the survey forms. For those patients who indicated that there were survey items or response choices that they did not understand, research personnel provided clarification using standardized, scripted responses (Supplemental Appendix 2).
For each participating patient, the 5 primary HCPs were identified: Within the Sunnybrook ICHD unit, patients, physicians, pharmacists, dietitians, and social workers are assigned to particular dialysis shifts that permitted the linkage of participating patients with primary HCPs. The unit operates on a primary-nurse care model which allowed for the identification of a primary dialysis nurse for each participating patient. Note that we define “primary” to indicate the provider most familiar with the patient rather than the family physician or primary care nurse practitioner. Each identified HCP was requested to complete a HCP survey instrument with respect to the participating patient to be completed during non-work hours and outside of the ICHD unit. The HCP survey instrument consisted of items to determine the individual’s role (physician, nurse, social worker, pharmacist, or dietitian), a self-assessment of HCPs’ degree of familiarity with the patient in question, their perception of how well the patients understood their illness, their predictions for the health of their patient in the coming year, and whether information regarding prognosis had been communicated to their patient. HCPs were then asked to predict which of the 7 GoC themes the participating patient would choose as relating to the goals for continued dialysis treatment, as well as which GoC theme would be chosen as most important. HCP surveys were distributed concurrently with the patient surveys.
Statistical Analysis
Data from the surveys were double-entered into a research database for analysis. For descriptive purposes, categorical variables were summarized with percentages and continuous variables with means and standard deviations. For the primary analysis, un-weighted kappa statistics and their standard errors were computed for the degree of agreement between patients and their HCPs regarding the importance of each of the 7 GoC themes.6 Z statistics for kappa were computed as kappa/SE (kappa). For survey questions in which more than 1 GoC could be selected as being important, kappa statistics were computed from 2 × 2 tables for each of the 7 GoCs and for each of the 5 HCP roles (ie, 35 tables). For the survey question in which patients and their HCPs were asked to pick the one most important GoC, kappa statistics were computed from 7 × 7 tables for each of the 5 HCP roles. The significance of the difference between kappa values across HCP roles was calculated with a chi-square statistic.6 Because of multiple statistical tests, the Holm procedure was used to adjust the nominal P value of .05.7
In a secondary analysis, a logistic regression analysis was performed in which the dependent variable was a binary indicator of whether at least 1 HCP’s assessment of the most important GoC coincided with the patient’s choice. The explanatory variables included whether or not the patient’s age was less than 65, whether the patient expected to receive a renal transplant, whether the patient’s most important GoC was to be cured of kidney disease, whether or not the patient had received at least some pre-dialysis nephrology care, a score indicating the amount of discordance between the assessments of patients and their HCPs with respect to the degree to which patients were informed regarding their illness (see Supplemental Appendix 6 for details of the latter calculation), and the patients’ estimate of the number of years they had been on dialysis. In the secondary analysis, a 95% confidence interval (CI) that excluded an odds ratio (OR) of 1.0 was considered to indicate statistical significance.
Informed consent was obtained from patient and HCP participants. The Research Ethics Board of Sunnybrook Health Sciences Centre granted approval for the study.
Results
Participant Characteristics
Patient and HCP recruitment and surveying occurred from July 1 to September 30, 2014. Of 173 potentially eligible patients, 15 patients declined to participate, 10 patients could not participate secondary to a language barrier and the unavailability of translation services, 9 patients were not present at their designated dialysis sessions during the period that the researchers were conducting surveys, and 2 patients’ surveys were incorrectly completed, yielding 137 patients who successfully completed the survey. A total of 125 patients completed the survey while on dialysis treatment and 12 completed the instrument at home; 50 HCPs completed surveys, comprising 6 staff physicians, 3 dietitians, 3 pharmacists, 2 social workers, and 36 primary nurses.
Among 137 patients who completed the survey, 56 (41%) were female, 97 (70.8%) were 61 years old or older, the mean (SD) duration of pre-dialysis care was 3.1 (4.6) years, and the mean duration on dialysis at the time of the survey was 5.1 (5.3) years (Table 1). Seventy-six (55.5%) patients spoke English as their primary language. A total of 104 (75.9%) patients required help with reading the survey or filling in their responses and 97 (70.8%) patients required explanations or clarifications of survey questions (Table 1). Fifty-one (37.2%) patients reported that they were on the waiting list for a kidney transplant. Of these, 16 were actually wait-listed, 15 were potentially eligible for transplantation but were awaiting further work-up, 9 had been assessed and found not to qualify for a transplant, 1 patient had previously declined transplant evaluation when offered, and 10 had never been evaluated for a transplant.
Table 1.
Characteristics of Participating In-Center Hemodialysis Patients (N = 137).
| Variable | n (%) or mean (SD) |
|---|---|
| N | 137 |
| Female, n (%) | 56 (40.9) |
| Age range, n (%) | |
| Under 40 | 10 (7.3) |
| 40-50 | 10 (7.3) |
| 51-55 | 10 (7.3) |
| 56-60 | 10 (7.3) |
| 61-65 | 18 (13.1) |
| 66-70 | 20 (14.6) |
| 71-75 | 18 (13.1) |
| 76-80 | 13 (9.5) |
| Over 80 | 28 (20.4) |
| Religious group, n (%) | |
| Christian | 81 (59.1) |
| Hindu | 2 (1.5) |
| Jewish | 17 (12.4) |
| Muslim | 14 (10.2) |
| None | 22 (16.1) |
| Other | 1 (0.7) |
| Ethnic group, n (%) | |
| African | 11 (8) |
| Caribbean | 16 (11.7) |
| Caucasian | 27 (19.7) |
| East Asian | 14 (10.2) |
| East Indian | 9 (6.6) |
| European | 19 (13.9) |
| Filipino | 17 (12.4) |
| Jewish | 14 (10.2) |
| Middle Eastern | 2 (1.5) |
| Other | 8 (5.8) |
| Duration of pre-dialysis care (years), mean (SD) | 3.1 (4.6) |
| Dialysis duration (years), mean (SD) | 5.1 (5.3) |
| Expecting transplant, n (%) | 51 (37.2) |
| English as primary language, n (%) | 76 (55.5) |
| Interpretation required, n (%) | 7 (5.1) |
| Interpreter, n (%) | |
| Family | 3 (2.2) |
| None | 130 (94.9) |
| Staff | 4 (2.9) |
| Aid required, n (%) | 104 (75.9) |
| Assistance needed, n (%) | 121 (88.3) |
| Assistance provided, n (%) | 97 (70.8) |
| Assisted by, n (%) | |
| Family | 3 (2.2) |
| None | 16 (11.7) |
| Researcher | 117 (85.4) |
| Blank | 1 (0.7) |
| Researcher present, n (%) | 125 (91.2) |
| Family present, n (%) | 11 (8) |
| Family responded, n (%) | 7 (63.6) |
Note. “Researcher present” implies that research personnel were present during patients’ completion of survey; “Family present” implies that 1 or more family members were present during patients’ completion of survey; “Family responded” implies that 1 or more family members responded to 1 or more survey questions on the patients’ behalf.
HCPs caring for the participating patients completed 623 of 685 (90.9%) corresponding surveys. For the 137 participating patients, 132 (96.4%), 112 (81.8%), 127 (92.7%), 126 (91.8%), and 128 (93.4%) corresponding surveys were completed by physicians, nurses, social workers, pharmacists, and dietitians, respectively (Table 2).
Table 2.
Responses of In-Center Hemodialysis Patient Surveys (n = 137) and HCPs’ Surveys (n = 623 surveys from 50 HCPs).
| Patients |
HCPs |
|
|---|---|---|
| Variable | n (%) or mean (SD) | n (%) or mean (SD) |
| Closest family member aware of GoC, n (%) (S2, Q13) | ||
| Not applicable | 24 (17.5) | — |
| Somewhat poorly | 5 (3.6) | — |
| Somewhat well | 19 (13.9) | — |
| Very poorly | 6 (4.4) | — |
| Very well | 83 (60.6) | — |
| Comfort with GoC discussion, n (%) (S2, Q14) | ||
| Somewhat comfortable | 20 (14.6) | — |
| Somewhat uncomfortable | 9 (6.6) | — |
| Very comfortable | 108 (78.8) | — |
| Importance of GoC discussion, n (%) (S2, Q15) | ||
| Not important at all | 6 (4.4) | — |
| Not that important | 9 (6.6) | — |
| Somewhat important | 26 (19) | — |
| Very important | 96 (70.1) | — |
| Importance of more kidney info, n (%) (S2, Q16; S4, Q8) | ||
| Blank | 0 (0) | 7 (1.1) |
| Not important at all | 10 (7.3) | 0 (0) |
| Not that important | 13 (9.5) | 159 (25.5) |
| Somewhat important | 32 (23.4) | 302 (48.5) |
| Very important | 82 (59.9) | 155 (24.9) |
| Familiarity level, n (%) (S4, Q2) | ||
| A little | — | 147 (23.6) |
| Blank | — | 2 (0.3) |
| Fairly well | — | 249 (40) |
| Not at all | — | 20 (3.2) |
| Not well | — | 39 (6.3) |
| Very well | — | 166 (26.6) |
| Patient’s illness comprehension, n (%) (S4, Q3) | ||
| Blank | — | 2 (0.3) |
| Somewhat poorly | — | 112 (18) |
| Somewhat well | — | 323 (51.8) |
| Very poorly | — | 7 (1.1) |
| Very well | — | 179 (28.7) |
| Prognosis, n (%) (S4, Q6) | ||
| Blank | — | 19 (3) |
| Die within 12 months | — | 19 (3) |
| Get better | — | 24 (3.9) |
| Get worse | — | 152 (24.4) |
| Stay the same | — | 409 (65.7) |
| Prognostic information provided, n (%) (S4, Q7) | ||
| Blank | — | 9 (1.4) |
| Die within 12 months | — | 1 (0.2) |
| Get better | — | 12 (1.9) |
| Get worse | — | 14 (2.2) |
| No info provided | — | 479 (76.9) |
| Stay the same | — | 108 (17.3) |
Note. Variable names in the leftmost column of the table correspond to survey questions for patients and HCPs as shown in Supplemental Appendices 2 and 4 (S2 and S4), respectively. Qx corresponds to question number “x” in the corresponding survey. HCP = health care providers.
Patient and HCP GoC Choices
When asked to choose any of the 7 GoC that applied to their continued dialysis treatment, patients were most likely to choose “live longer” (116 patients, 84.7%). Sixty-nine patients (50.4%) chose “be cured” as one of their goals for continuing dialysis. Among the latter, 25 (36.2%) believed they were wait-listed for a renal transplant, and 15 (21.7%) were actually listed or being assessed for transplant suitability. HCPs predicting the GoC of their patients chose “live longer” most often as well (504 HCP surveys, 80.9%), but only chose “be cured” as a predicted goal for patients continuing dialysis in 46 surveys (7.4%; Figure 1). When patients were asked to choose the GoC that was most important to their continued dialysis treatment, they chose “live longer” more than the other 6 GoC (48 patients, 35.6%). Twenty-six (19.3%) patients chose “be cured” as their most important goal for continuing dialysis. Among the latter, 15 (57.7%) believed that they would receive a transplant, whereas 7 (26.9%) were actually listed or being assessed for transplant suitability. HCPs predicted that patients would choose “live longer” as their most important goal in 189 HCP surveys (31.8%) but predicted that patients’ most important goal would be “be cured” in only 22 surveys (3.7%; Figure 2).
Figure 1.
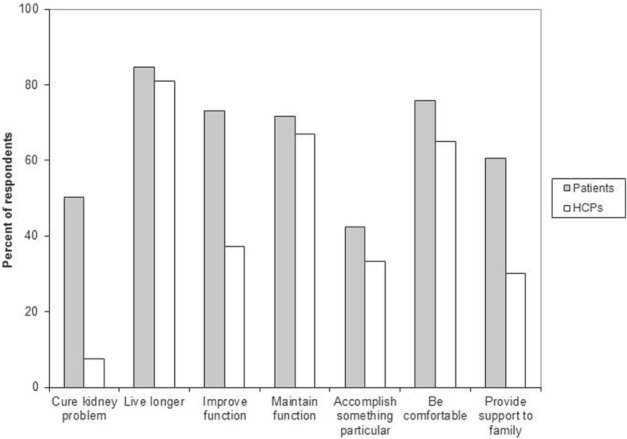
Which GoC are relevant to your continued dialysis treatment? Choose any that apply. Histogram of the frequency that patients and HCPs selected particular GoC as being important.
Note. For HCPs, the responses indicate their prediction of the GoC themes that would be selected by the associated patient. Participants could choose 1 or more GoC themes as being important. HCP = health care provider; GoC = goals of care.
Figure 2.
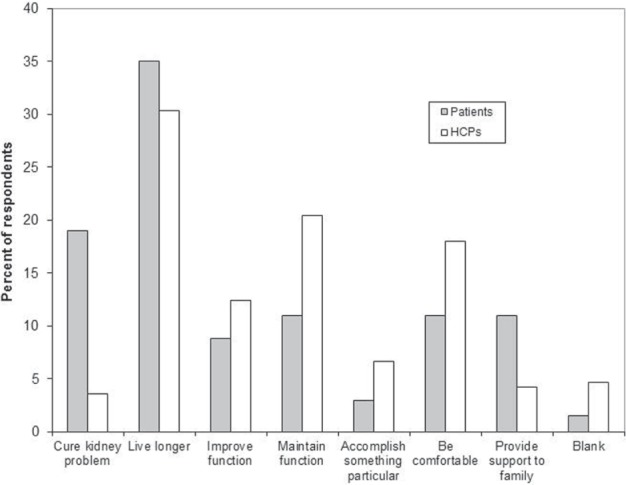
Which is the most important goal you have for your continued dialysis treatment? Histogram of the frequency that patients and HCPs selected each of the 7 GoC themes as being most important.
Note. For HCPs, the responses indicate their prediction of the GoC theme that would be selected as being most important by the associated patient. HCP = health care provider; GoC = goals of care.
Agreement Between Patient and HCP GoC Choices
Kappa scores for the degree of agreement between patients and HCPs by HCP role for each of the 7 GoC domains (when both patients and HCP could choose 1 or more of the 7 themes) are shown in Figure 3. After adjustment of the nominal significance value of .05 according to the Holm procedure, we were unable to reject the null hypothesis of no greater degree of agreement between patients and HCPs than that expected by chance. A similar lack of agreement was found between patients’ selection of their most important GoC for continuing dialysis and their HCPs’ prediction (κ scores < .15; Figure 4). We found no significant difference in kappa scores among HCP role types for each of the 7 GoC themes individually (χ2, < 0.01-0.71; all P values > .1) or for the most important GoC (χ2, 0.024; P value, .31). In a fully adjusted logistic regression analysis, the odds of at least 1 agreement between patients’ GoC and their HCPs’ predictions was only significantly associated with patients choosing “Be cured” as their most important GoC (OR, 0.04; 95% CI, 0.01-0.18; Table 3). We found a trend toward reduced odds of at least 1 GoC agreement for each year of dialysis duration (OR, 0.06; 95% CI, 0.89-1.03; Table 3).
Figure 3.
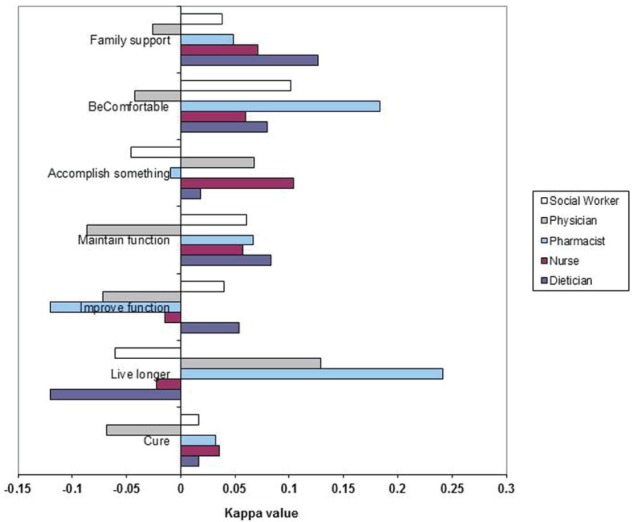
Extent of agreement between the choices of important GoC themes between patients and HCPs by GoC theme and HCP role type.
Note. In this analysis, patients and HCPs could choose more than 1 GoC theme as being important. Bar graphs in the figure represent Z statistics where Z = kappa/SE (kappa). Kappa represents the agreement between patients and HCPs beyond chance and SE (kappa) represents its standard error. A kappa Z value of ±1.96 indicates nominal statistical significance; however, the level of significance required for a given test was determined by the Holm procedure (see the text for details). GoC = goals of care; HCP = health care provider.
Figure 4.
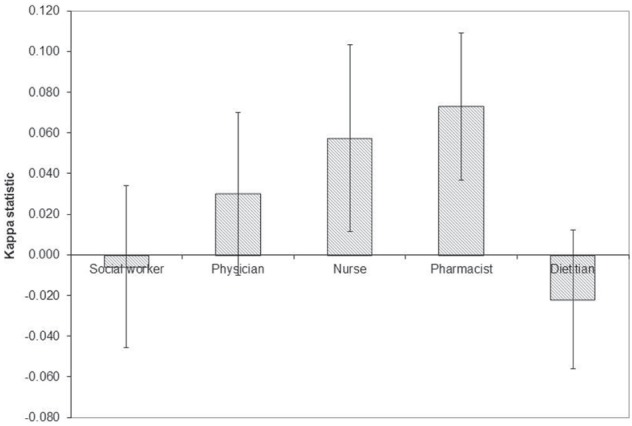
Extent of agreement between the choices of the most important GoC between patients and care givers by GoC theme and HCP role type.
Note. Bar graphs in the figure represent kappa values where kappa represents the agreement between patients and HCPs beyond chance and the error bars represent the standard error of the corresponding kappa statistic. Generally kappa values ≤ .5, >.5 to ≤.6, >.6 to ≤.7, >.7 to ≤.8, >.8 to ≤.9, and >.9 indicate very poor, poor, fair, good, very good, and excellent agreement beyond chance, respectively. Because multiple statistical tests were used, the level of significance required for a given test was determined by the Holm procedure (see the text for details). GoC = goals of care; HCP = health care provider.
Table 3.
Results of Unadjusted and Adjusted Logistic Regression Analysis Where the Binary Response Variable Was Whether at Least 1 HCP Correctly Predicted the Most Important GoC Theme for a Given Patient.
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Age < 65 years | 1.38 (0.7-2.74) | 2.01 (0.78-5.13) |
| IDscore | 0.63 (0.24-1.63) | 0.69 (0.23-2.07) |
| Expecting Tx | 0.93 (0.47-1.87) | 0.82 (0.31-2.14) |
| Primary GoC “Be cured” | 0.05 (0.01-0.2) | 0.04 (0.01-0.18) |
| Had pre-dialysis care | 0.8 (0.38-1.71) | 0.87 (0.36-2.11) |
| Dialysis duration (per year) | 0.99 (0.93-1.05) | 0.96 (0.89-1.03) |
Note. Adjusted ORs were estimated for a model containing all of the listed factors. IDscore is the score indicating the degree to which HCPs and patients agreed on whether patients were informed regarding their health care status (see Supplemental Appendix 6 for the definition); Expecting Tx is a binary indicator of whether patients were expecting to receive a renal transplant (regardless of whether they were actually on the transplant wait list or completing a transplant work-up); Had pre-dialysis care is a binary indicator of whether a patient’s estimate of pre-dialysis nephrology care duration was greater than 0; Dialysis duration is a patient’s estimate of the number of years on dialysis. HCP = health care provider; OR = odds ratio; CI = confidence interval; GoC = goals of care.
Perceptions of Disease Prognosis and Further GoC Discussion
When patients were asked to predict their prognosis over the following year, 51 (37.5%) patients predicted their kidney problem would get better, 62 (45.6%) predicted their kidney problem would stay the same, 15 (11%) predicted their kidney problem would get worse, and 8 (5.9%) predicted they would die in the next year. The patients’ HCPs were significantly less optimistic about their patients’ prognosis (P < .001), with only 6.1% of physician surveys (8 surveys of 131 physician surveys) predicting that a patient’s kidney problem would improve, 67.2% (88 surveys) predicting stable kidney disease, 23.7% (31 surveys) predicting worsening of kidney disease, and 3.1% (4 surveys) predicting death in the next year. However, of the physicians surveyed, 56 of 131 (42.7%) reported having provided no prognostic information to the patient.
Of the 137 patients surveyed, 108 (78.8%) reported that they would feel very comfortable having a GoC discussion with their physician, whereas only 9 (6.6%) reported that they would feel somewhat uncomfortable with such a discussion. A total of 122 (89.1%) patients felt that GoC discussions were somewhat or very important, whereas 15 (10.9%) felt that they were not that important or not important at all. A majority of patients (82 patients, 59.9%) felt that having more information about their kidney illness was very important, whereas 23 (16.8%) patients felt that having more information was not that important or not at all important (Table 2).
Discussion
In this survey of 137 prevalent ICHD patients and 50 HCPs, we found that HCPs were no more likely than chance to predict the GoC that patients would identify as being important. In addition, the data suggest patients may not have an accurate understanding of the nature of their kidney disease, the likely outcome of dialysis therapy, and the realistic chance of kidney transplantation. With each successive year on dialysis, we observed a trend toward HCPs being less likely to correctly predict patients’ GoC. These observations would be consistent with GoC being discussed at dialysis initiation but not subsequently on an ongoing basis. Ongoing reassessment of GoC is necessary, as patients have been shown to perceive more illness and treatment consequences on initiating dialysis and that these perceptions progressively worsen with increased length of time on dialysis.8 Clinical practice guidelines recommend ongoing GoC re-evaluation, particularly after an interim medical event or complication.9
A key finding of our study was that HCPs were significantly less accurate with GoC predictions with patients who chose “Be cured” as their primary GoC. As ICHD does not cure end-stage renal disease (ESRD), patients who have no expectation of transplantation and who choose “be cured” as their primary GoC have a misunderstanding of ESRD and the therapeutic aim of ICHD. Even if such patients considered ICHD a bridge to kidney transplantation, which they may have considered a cure for ESRD, only a minority of patients who chose being cured as their primary goal expected to receive a transplant, and even fewer were actually listed for transplant or actively engaged in a transplant evaluation. Furthermore, kidney transplant is not a true cure for ESRD, as one set of concerns and burdens is traded for another, and patients tend to overestimate quality of life after a kidney transplant.10 Low health literacy is one source of an inaccurate illness understanding, and patients with low health literacy have been previously demonstrated to be more likely to choose more aggressive medical interventions.11 Improved education and more frequent and detailed GoC discussions may improve patients’ understanding of their disease and their HCPs’ understanding of patients’ GoC. Apart from the disagreement regarding the “Be cured” GoC, we found a considerable gap between patients’ expectations of receiving a kidney transplant and their actual transplant status per se. Possible reasons for this may include the complicated process of determining eligibility for transplantation, a lack of education regarding the steps involved in the latter process, lengthy delays between the initiation of the transplant work-up process and ultimate listing, inadequate communication between patient and health care team, poor overall health literacy, and cognitive issues.
Study patients were more likely to predict that their overall health would improve, whereas more physicians predicted that their patients’ health would stay the same or get worse. The lack of agreement regarding prognosis may be a consequence of the fact that 42.7% of physician responses indicating they had not provided patients with prognostic information. Previous reports have outlined that patients who perceive a better prognosis are significantly more likely to choose life-extending therapy, even if it means more discomfort.12 Prior investigations have found that, before initiating dialysis, 97% of patients would want to be provided with life-expectancy information without having to prompt their physician.13 Improved illness understanding would allow for informed contemplation and prioritization of GoC. Several factors may underlie HCPs’ reluctance to discuss GoC, and, in particular, prognosis and end-of-life issues, including fear of taking away hope, fear of upsetting patients and families, a lack of patient readiness, and time requirements.14,15 The findings of this study may serve to allay these fears, as the majority of patients surveyed indicated that discussions regarding GoC are important and that they would be very comfortable having them. The low proportion of HCPs reporting that they had provided prognostic information to patients suggests that further research into whether an educational intervention for HCPs focused on conveying prognostic information would be warranted.
Shared decision making is a collaborative endeavor between the care provider and patient, and requires both to consider patient values, goals, and preferences to ensure an acceptable decision is proposed.16 The main findings of this study are cause for concern, considering several clinical practice guidelines endorse shared decision making when initiating, maintaining, and withdrawing from dialysis.9,17 An accurate illness understanding is required to meaningfully consider and prioritize GoC. Future work could include the development and assessment of targeted educational initiatives to address misconceptions and knowledge gaps in dialysis patients’ understanding of their disease, as well as specifying the necessary frequency with which GoC should be revisited in the dialysis population in the guidelines on the topic. The 7 GoC themes used in this study may serve as a useful interim framework to guide GoC discussions with patients until proven educational interventions are available.
Our single-center study has several limitations. Only ICHD patients were surveyed, and the results may not generalize to patients on home dialysis. Selection bias may have occurred as the assessment of patient eligibility for the study was made by the HCPs who subsequently provided GoC predictions for the patient participants. This was unavoidable, as detailed familiarity with patients was required for both selection and GoC prediction. Although we attempted to mitigate HCP influence on patient survey responses by using a structured patient survey instrument and scripted responses to patient queries regarding the survey, such influence cannot be ruled out definitively. However, HCP influence would be expected to bias the results in favor of concordance and yet we found a lack of concordance between HCP and patient responses.
Some characteristics of the participating patients may have interfered with survey completion: Only 55.5% spoke English as a first language, a majority of patients required physical help with reading or writing, and most patients required explanations or clarifications of survey questions. However, we sought to reduce imprecision in eliciting survey responses by standardizing the phrases surveyors used to respond to patients’ questions. The extent to which assistance was required by the patient participants is noteworthy in itself as it highlights the difficulties that are likely to be encountered in both research and clinical settings when eliciting GoC from elderly, frail, hemodialysis patients who often suffer from multiple comorbid illnesses including defects in cognition. Researchers must balance the need to enroll as many patients as possible to avoid selection bias (and increase generalizability of the findings) versus recruiting only cognitively intact fluent English speakers (which would increase the internal validity of a study).
Definitions of each of the GoC items on the survey were not provided to either HCPs or patient participants and responses were therefore governed by the way in which participants understood the questions and the terms used. We cannot be certain whether discrepancies in responses between HCPs and patients were due to different comprehension of the GoC items on the survey. The development of definitions would aid future research in this area. We endeavored to ensure that our patient participants understood survey questions by using scripted responses to patient queries; however, we cannot be certain that all patients understood every question. Finally, each HCP made GoC predictions on more than 1 patient, but measures of agreement were not adjusted for within-rater correlation. However, given the very poor agreement, such adjustment would be unlikely to materially affect the results.
Conclusions
HCPs’ perceptions of their patients’ GoC were found to have poor agreement with patients’ reported GoC. This finding supports the importance of frequent and effective GoC discussions and illness education within the ICHD population. Future work could involve the design and validation of interventions to improve the HCPs’ understanding of their patients’ GoC.
Acknowledgments
We thank the staff and patients who participated in this study, with special mention to our research assistants, Imadh Bedri and Ayla Lefkowitz, for their help in collecting and compiling the data for this study.
Footnotes
List of Abbreviations: ESRD, end-stage renal disease; GoC, goals of care; HCP, health care provider; HCPs, health care providers; ICHD, in-centre hemodialysis; OR, odds ratio; SD, standard deviation.
Ethics Approval and Consent to Participate: Informed consent was obtained from patient and health care provider participants. The Research Ethics Board of Sunnybrook Health Sciences Centre granted approval for the study.
Consent for Publication: This was not applicable.
Availability of Data and Materials: The datasets supporting the conclusions of this article are not available, as consent for publication of raw data was not specifically obtained.
Author Contributions: All authors contributed to the study design and conception. Acquisition of data was conducted by AL and JB. DN conducted the statistical analysis, and all authors contributed toward the interpretation of the data. AL drafted the manuscript, which was critically revised by all authors. All authors have approved the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: No external grants or commercial sponsorship was obtained for this study. However, limited financial and resource support for this project was gratefully provided by the Nephrology Program at Sunnybrook Health Sciences Centre.
References
- 1. Gillick MR. Re-engineering shared decision-making. J Med Ethics. 2015;41(9):785-788. [DOI] [PubMed] [Google Scholar]
- 2. Davison SN. Advance care planning in patients with chronic kidney disease. Semin Dial. 2012;25(6):657-663. [DOI] [PubMed] [Google Scholar]
- 3. Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Review article—goals of care toward the end of life: a structured literature review. Am J Hosp Palliat Care. 2008;25(6):501-511. [DOI] [PubMed] [Google Scholar]
- 4. Haberle TH, Shinkunas LA, Erekson ZD, Kaldjian LC. Goals of care among hospitalized patients: a validation study. Am J Hosp Palliat Care. 2011;28(5):335-341. [DOI] [PubMed] [Google Scholar]
- 5. Brandt DS, Shinkunas LA, Gehlbach TG, Kaldjian LC. Understanding goals of care statements and preferences among patients and their surrogates in the medical ICU. J Hosp Palliat Nurs. 2012;14(2):126-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fleiss JL, Levin BA, Paik MC. Statistical Methods for Rates and Proportions. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2003. [Google Scholar]
- 7. Holm S. A simple sequentially rejective multiple test procedure. Scand J Statist. 1979;6:65-70. [Google Scholar]
- 8. Jansen DL, Heijmans MJWM, Rijken M, et al. Illness perceptions and treatment perceptions of patients with chronic kidney disease: different phases, different perceptions? Br J Health Psychol. 2012;18(2):244-262. [DOI] [PubMed] [Google Scholar]
- 9. Galla JH. Clinical practice guidelines on shared decision-making in the appropriate initiation of and withdrawal from dialysis. J Am Soc Nephrol. 2000;11:1340-1342. [DOI] [PubMed] [Google Scholar]
- 10. Cleemput I, Kesteloot K, De Geest S, Dobbels F, Vanrenterghem Y. Health professionals’ perceptions of health status after renal transplantation. Transplantation. 2003;76(1):176-182. [DOI] [PubMed] [Google Scholar]
- 11. Volandes AE, Paasche-Orlow M, Gillick MR, et al. Health literacy not race predicts end-of-life care preferences. J Palliat Med. 2008;11(5):754-762. [DOI] [PubMed] [Google Scholar]
- 12. Wachterman MW, Marcantonio ER, Davis RB, et al. Relationship between the prognostic expectations of seriously ill patients undergoing hemodialysis and their nephrologists. JAMA Intern Med. 2013;173(13):1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fine A, Fontaine B, Kraushar MM, Rich BR. Nephrologists should voluntarily divulge survival data to potential dialysis patients: a questionnaire study. Perit Dial Int. 2005;25:269-273. [PubMed] [Google Scholar]
- 14. Ceccarelli CM, Castner D, Haras MS. Advance care planning for patients with chronic kidney disease—why aren’t nurses more involved? Nephrol Nurs J. 2008;35(6):553-557. [PubMed] [Google Scholar]
- 15. Zhou G, Stoltzfus JC, Houldin AD, Parks SM, Swan BA. Knowledge, attitudes, and practice behaviors of oncology advanced practice nurses regarding advanced care planning for patients with cancer. Oncol Nurs Forum. 2010;37(6):e400-e410. [DOI] [PubMed] [Google Scholar]
- 16. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301-312. [DOI] [PubMed] [Google Scholar]
- 17. Moss AH. Revised dialysis clinical practice guideline promotes more informed decision-making. Clin J Am Soc Nephro. 2010;5(12):2380-2383. [DOI] [PubMed] [Google Scholar]


