Abstract
Objective
Familial aspects of pediatric obsessive-compulsive disorder (OCD) including accommodation and treatment have received notable and warranted attention. However, individual perspectives of its repercussions on family functioning, including emotional parental burden, have not been closely examined. The present study details this topic utilizing a large, multi-center sample.
Method
Participants included 354 youth affected with OCD, mothers and fathers ascertained through pediatric OCD programs in Boston, USA (n=180) and Vancouver, Canada (n=174). The validated OCD Family Functioning (OFF) Scale and standard OCD measures were completed. Descriptive, between-site and cross-perspective comparative analyses were followed by regression model testing to predict family impairment.
Results
Family functioning was negatively impacted from youth, mother, and father perspectives. Impairment was reportedly more extensive at the time of worst OCD severity and was greater from maternal versus paternal viewpoints. Most frequently impacted family tasks and implicated OCD symptoms included morning and bedtime routines and intrusive thoughts. Emotional repercussions included stress and anxiety, followed by frustration/anger in youth and sadness in parents. Nearly half of mothers and a third of fathers reported daily occupational impairment. Compared to youth self-report, parents perceived fewer social and academic impacts on their child. Family accommodation most consistently predicted family impairment, especially from parent perspectives. OCD and compulsion severity, contamination and religious obsessions, and comorbidities also predicted various perspectives of family subdomain impairment.
Conclusion
This study quantitatively details the pervasive burden that pediatric OCD places on families, as reported from complementary relative perspectives. Further attention to this topic is warranted in clinical and research realms.
Keywords: obsessive-compulsive disorder, child, adolescent, family, parents
INTRODUCTION
Obsessive-compulsive disorder (OCD) frequently onsets in childhood and is characterized by unwanted recurrent obsessions and/or compulsions. Identified as a leading global cause of non-fatal illness burden by the World Health Organization,1 OCD is significantly impairing to both affected individuals and family members.2–4
OCD is unique in the degree to which family members become enmeshed with symptom expression. Family accommodation in pediatric OCD has been well documented,5–6 including ritual facilitation (i.e., hearing “confessions”), reassurance-giving, and enabling avoidance of triggers (i.e., abstaining from saying certain words).7 Although well-intentioned, family accommodation inadvertently worsens OCD symptoms and is associated with increased disease severity, overall functioning impairment, and poor treatment response.5,8–10
Even in the absence of family accommodation, general impacts of OCD on family life is often extensive for those living in the home.4,7,11–13 In comparison to relatives of those with moderate to severe clinical depression, families of individuals affected with OCD experience greater burden and impaired functioning, partially due to greater expressed anger of the affected individual when family members do not accommodate.14
A robust body of research has explored the influence of family factors on OCD, specifically with respect to relative15 and parent16–17 expressed emotion (EE) and over-involvement18, and impacts of parental blame, conflict, and cohesion on treatment outcomes. 19–20 Associations have been demonstrated between pediatric OCD and select aspects of family impairment, such as family accommodation, strain, and stress 21, and a study has captured simultaneous child and mother perspectives.22
Despite the above, little research has been done to capture simultaneous perspectives of OCD-affected youth and their mothers and fathers, or that reports on quantitative measures of emotional and overall family functioning and its subdomains. Until recently, the only validated measure designed to specifically capture family aspects of pediatric OCD was the Child Obsessive Compulsive Impact Scale (COIS).23 However, given its broader scope, this measure does not assess family members’ emotional functioning, symptom-specific impairment, more than one time period (current versus worst OCD), or individual perspectives.
The OFF Scale was designed and validated24 to capture family impairment holistically, and has subsequently been translated and utilized by numerous international clinical and research programs. A key feature of the OCD Family Functioning (OFF) Scale is the light it sheds on divergent family perspectives, which is of importance due to the low parent–child agreement in symptom severity reports for anxiety disorders25 and OCD.26
Specific aims of the current study are as follows: 1) To detail aspects of family functioning impairment in pediatric OCD; 2) To compare OCD impacts on family function between current and worst-ever time points; 3) To compare child versus parent perspectives of family functioning; and 4) To identify correlates and predictors of family impairment in pediatric OCD.
We hypothesized that pediatric OCD has negative impacts on routines, socio-occupational/academic and emotional functioning in the majority of affected families; that impairment is greater at times of worse OCD severity; and that parents view OCD as causing greater family impacts versus youth perspectives. Furthermore, we hypothesized that earlier onset, compulsion severity, treatment history, family accommodation, and family OCD history (first-degree) would predict OCD-related family impairment overall. Finally, we hypothesized that unspecified distinct predictors would emerge for youth- versus parent-reported impacts on impairment subdomains.
METHOD
Participants
This study reports on 354 participants recruited between 2008 and 2016 in Boston, USA and Vancouver, Canada, with 118 complete trio units comprising probands affected by OCD (7–19 years, 55.3% male), their mothers, and their fathers. Inclusion criteria required a current diagnosis of OCD according to DSM-IV-TR criteria27 and written informed consent/assent of all participants. Probands with schizophrenia, severe intellectual disability, or OCD occurring exclusively in the context of depression were excluded. This study was approved by institutional ethics review boards at Massachusetts General Hospital (MGH), McLean Hospital, and the University of British Columbia (UBC).
Boston Sample
Sixty complete trios were ascertained between 2008 and 2011, with 52 from the OCD Collaborative Genetics Association Study (OCGAS),28 one from an MGH outpatient clinic (Boston, MA), and seven from the McLean OCD Institute intensive residential treatment program (Belmont, MA). See Samuels et al. (2006)28 for a detailed description of the OCGAS diagnosis and screening procedures.
Vancouver Sample
A total of 58 complete trios were ascertained between 2012 and 2016 from the British Columbia Children’s Hospital (BCCH) UBC Provincial OCD Program (UBC-POP) (Vancouver, Canada). Diagnoses were assessed by PhD-level clinical psychologists via the Anxiety Disorders Interview Schedule-Child Version Parent Interview (ADIS-IV-C/P)29 and confirmed by child and adolescent psychiatrists. Additional characterizing details were also collected during initial assessment.
Instruments and Measures
OCD Family Functioning (OFF) Scale.24
The OFF Scale is a 42-item, three-part self-report measure assessing OCD-related family functioning impairment at current and worst-ever symptom time points. It has complementary patient and relative versions to capture different perspectives of family functioning impairment. The scale contains a seven-factor structure, encompassing three impact factors in Part 1 (overall impairment: routine tasks, socio-occupational/academic, and emotions) and four OCD symptom factors in Part 2 (symptom-specific impairment: symmetry, forbidden “intrusive” thoughts, cleaning, and hoarding). While hoarding is now its own diagnosis in the DSM-5,26 questions assessing hoarding behaviour have been retained in the OFF scale, given its presence within many individuals with OCD. Part 3 addresses OCD-related impairment related to fulfillment of individual family roles and is not included in this study, given its suboptimal internal consistency (Cronbach’s α=0.85–0.89). The OFF Scale has been validated via a large sample (N=400) in a previous study, demonstrating strong test-retest reliability, construct validity, as well as convergent and divergent validity.24 Both patient and relative versions of the OFF subscales demonstrated excellent internal consistency for Parts 1 and 2 (Cronbach’s α=0.95–0.96 and 0.90–0.92, respectively). For a detailed description of the scale’s validity and reliability indicators, please refer to Stewart et al. (2011).24
Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS).30
The CY-BOCS is a 10-item clinician-administered instrument that informs on clinical severity of OCD and has a good internal consistency (Cronbach’s α=0.87–0.90), test–retest reliability, and construct validity.
Child Depression Inventory (CDI).31
The CDI, modeled after the Beck Depression Inventory for adults, is a 27-item self-rating scale assessing depression in youth.
Family Accommodation Scale Parent-report (FAS-PR).3
The FAS-PR is a 12-item instrument that assesses parents’ accommodation of the child’s OCD-related rituals and behaviours. CDI and FAS data were only available for the Vancouver sample.
Clinical Global Impression-Severity Scale (CGI-S).32
CGI-S is a clinician rating of the severity of psychopathology on a seven-point scale.
Analysis
All analyses were performed using SPSS 23.0.33 Initial descriptive analyses included all participants, followed by between-site independent samples t-tests for continuous data and chi-square or Fisher’s exact tests (for expected cell count < 5) for categorical data. Paired t-tests compared scores between current and worst severity time points. Omnibus repeated measures analysis of variance (ANOVA) was used to compare across family member perspectives, followed by pairwise analyses.
To gain a clinically meaningful interpretation of overall family functioning impairment, ordinal data in the subscales of family routines and socio-occupational/academic impact were dichotomized to “daily” versus “less than daily,” while emotional impact data was dichotomized to “often/always” versus “never/a little”. Perspectives were analyzed via the Friedman ANOVA test (cut-off at p<.05) and the Wilcoxon signed-rank test for post hoc analysis (Bonferroni-adjusted α=0.017). All tests were two-tailed.
To examine potential predictors of family functioning impairment, correlation and regression analyses were conducted between 15 selected variables of interest including age, gender, lifetime comorbidity, family OCD history, FAS-PR, CDI, intact vs. separated/divorced families, CGI-S and CY-BOCS obsession/compulsion and total scores (clinician-rated), presence of OCD symptom subtypes, and the outcome measures including overall family functioning impairment as well as its three factor domains. The candidate predictor variables were selected due to their known association with pediatric OCD characteristics and outcomes.
Distributions of the outcome variables were examined to ensure that the assumption of normality was met. To identify candidate predictors, correlations (Pearson and point-biserial) between variables of interest and outcome measures were examined (inclusion cut-off at p<.05). After inspecting collinearity statistics, these variables were then entered into a stepwise regression to predict each of the outcome measures. Variables that remained significant (p<.05) in the regression model were subsequently entered into the final regression equation. Residuals were tested for assumptions of normality and for equality of variance.
RESULTS
Descriptive Data
Mean ages of OCD onset and reported worst severity were 8.4 (SD 3.4) and 12.1 (SD 3.2) years, respectively. Reported proband family history revealed 14.6% with a parent diagnosed with OCD, 6% with a sibling diagnosed with OCD, and 18.8% with at least one diagnosed first-degree relative. While mean CY-BOCS scores were higher for the Boston site (t[104]=5.10, p<.001), CGI-S scores were higher for Vancouver participants (t[74]=2.83, p=.006). Fewer Vancouver participants reported receiving pharmacologic and non-pharmacologic OCD treatment. Overall family function impairment (Part 1) scores did not differ between sites for worst-ever OCD (t[111]=1.87; p=.064), but were greater for the Vancouver site at “current” report (t[115]=2.94; p=.004). No between-site differences were identified with respect to gender, ages at ascertainment, OCD onset, or worst OCD severity, or with respect to household composition, diagnosed/suspected family OCD history, additional lifetime comorbidity measures, or OCD symptom types. Details and further descriptive data are summarized in Table S1, available online.
Family Perspectives of Impact at Current and Worst OCD Severity
Across family perspectives, scores were rated as more impairing at the most severe OCD time point compared to the current time of assessment across all OFF Part 1 and 2 domains. Regarding overall family impairment, mothers reported greater family impacts than fathers for worst OCD severity (38.04±15.26 vs. 34.52±15.38, F[2, 215]=3.58, p=.03), but no cross-perspective differences were reported for current scores. Symptom-specific impairment scores did not differ between family members at either time point (F[2, 200]=1.72, p=.18 at worst OCD; F[2, 188]=1.09, p=.34 at current). Table S2 (available online) presents details of cross-perspective OFF subscale scores at current and worst OCD.
Impact on Family Routines (Part 1a)
Table 1 presents frequencies of daily impact on family routines. As cross-perspective differences were not identified for either time point, individual perspectives are not presented or compared at an item level. Similar patterns were observed for worst and current time points, with the most commonly disrupted activities including bedtime routines (69.5% vs. 37.5%, respectively), morning routines (65% vs. 35.4%), and mealtimes (44.4% vs. 20.6%). Appointments (20.5% vs. 5.3%) and religious worship (13.3% vs. 6.8%) were least likely to have daily OCD-related impact.
Table 1.
Prevalence of Daily Obsessive-Compulsive Disorder (OCD)-Related Impairment of Family Routines a
| Worst Ever OCD (%) | Current OCD (%) | |
|---|---|---|
| Bedtime routines | 69.5 | 37.5 |
| Morning routines | 65.0 | 35.4 |
| Mealtimes | 44.4 | 20.6 |
| Social/family events | 43.5 | 19.7 |
| Lateness to work/school | 43.4 | 18.1 |
| Planning/scheduling | 42.2 | 23.0 |
| Trips | 31.0 | 12.4 |
| Going to restaurants | 24.2 | 6.4 |
| Shopping | 23.1 | 7.2 |
| Appointments | 20.5 | 5.3 |
| Religious | 13.3 | 6.8 |
Note: no significant score differences were identified across youth, mother, and father groups for this subscale total at current or worst-ever time points (see Table 1, p ≥ .15)
Percentages represent proportion of total respondents who answered “Daily.”
Social and Occupational/Academic Functioning (Part 1b)
Individual perspectives regarding personal impacts for the respondent, for the OCD-affected youth, and for other relatives in the family are presented in Table 2. Compared to youth self-report for worst OCD severity, fewer parents perceived daily social impacts (69.1% youth, 55.3% mothers, 49.1% fathers, χ2[2, n=114]=11.63, p=.003) and fewer fathers perceived daily academic impacts (45.6% fathers, 60.7% mothers, 69.3% youth, χ2[2, n=105]=16.33, p<.001) of OCD on their child’s functioning. Regarding broader OCD impacts, fewer youth perceived daily impairment of other family members’ occupational/academic functioning compared to mothers’ perspectives (33.9% youth, 50% mothers, p=.004).
Table 2.
Emotional, Social and School/Work Impairment of Obsessive-Compulsive Disorder (OCD)-Affected Family Members
| Worst Ever OCD |
Current OCD |
|||||||
|---|---|---|---|---|---|---|---|---|
| Respondent (%)a |
Omnibus p |
Respondent (%)a |
Omnibus p |
|||||
| Youth | Mom | Dad | Youth | Mom | Dad | |||
| Emotional impact – always/often | ||||||||
| Stressed/anxious | 87.6 | 85.0 | 77.4 | .078 | 59.3 | 61.5 | 50.9 | .099 |
| Frustrated/angry | 76.6 | 68.7 | 64.9 | .238 | 52.1 | 47.4 | 36.8 | .032c |
| Sad | 69.0 | 81.7* | 67.5 | .002b,d | 45.7 | 59.5 | 44.0 | .010d |
| Guilt | 56.8 | 35.9 | 30.4 | .011c | 36.0 | 25.5 | 16.5 | .004c |
| Social life impact – daily | ||||||||
| Impact on OCD-affected child | 69.1* | 55.3 | 49.1 | .003b,c | 40.0 | 27.4 | 27.0 | .022c |
| Impact on respondent | 69.1* | 48.2 | 41.2 | <.001b,c | 40.0* | 25.2 | 22.6 | .003b,c |
| Impact on others in family | 58.2 | 59.1 | 56.1 | .709 | 29.6 | 27.2 | 25.7 | .721 |
| School/work performance – daily | ||||||||
| Impact on OCD-affected child | 69.3 | 60.7 | 45.6* | <.001c,d | 42.7* | 27.0 | 26.1 | <.001b,c |
| Impact on respondent | 69.3* | 45.1 | 33.3 | <.001b,c | 42.7* | 19.1 | 17.5 | <.001b,c |
| Impact on others in family | 33.9 | 50.0 | 50.0 | .017b | 15.0 | 26.3 | 25.2 | .062 |
Note. Boldface and italics indicate that significant reported differences exist between the identified group and the other two respondent groups for that time period and domain of functioning.
Percentages represent proportion of respondents who answered “Always/Often” for emotional impact and “Daily” for social and school/work activities. Omnibus p values calculated via Friedman analysis of variance test, and pair-wise differences calculated via the Wilcoxon signed-rank test.
Statistically significant Bonferroni-adjusted (p < .017) pairwise difference between patient and mother.
Statistically significant Bonferroni-adjusted (p < .017) pairwise difference between patient and father.
Statistically significant Bonferroni-adjusted (p < .017) pairwise difference between mother and father.
Impact on Emotions (Part 1c)
Across time points and perspectives, stress/anxiety was the most commonly reported emotion (occurring “often” to “always” in 77.4–87.6% at worst OCD), followed by sadness for parents (67.5–81.7%) and frustration/anger for the youth (76.6%). Regardless of time point, fewer fathers reported guilt (16.5–30.4%) compared to youth (36–56.8%, p≤.001), and fewer fathers reported sadness (44–67.5%) compared to mothers (59.5–81.7%, p=.003–.006). More youth reported frustration/anger compared to fathers (52.1% vs 36.8%, p=.013) at current OCD, and fewer reported sadness compared to mothers at worst OCD severity (69.0–81.7%, p=.006).
Symptom-Specific Family Impairment (Part 2)
The differential impact of OCD symptom types on family functioning is summarized in Table S3, available online. Across perspectives at worst OCD, intrusive thoughts (77.6%), “just right” compulsions (77.2%), and perfectionism-related symptoms (70.3%) were most frequently associated with family impairment. The first two of these were also the most frequently associated OCD symptoms with current family impairment (68.2% and 69.1%, respectively).
Predicting Family Functioning Impairment
Correlation results identified between two to four out of 15 variables as potential predictors (p<.05 correlations) for entry into regression models for Part 1 total scores as reported from different perspectives. These included FAS (p=.048) for mother-report, FAS (p<.001) and marital status (p=.009) for father-report, CY-BOCS compulsion severity (p=.005) for youth-report, and FAS (p=.002), lifetime comorbidity (p=.005), and contamination obsessions (p=.045) for combined family-report. FAS survived as the only predictor for mother, father, and combined family perspectives of overall family impairment (p=.006, adjusted R2 =14.3%; p=.025, adjusted R2 = 9.0%; and p=.002, adjusted R2 = 12.1%, respectively). CY-BOCS compulsion severity was the only predictor for youth-reported family impairment (p=.04; adjusted R2 = 3.1%). Statistical tests suggested that multicollinearity was not a concern, and normality was reasonable.
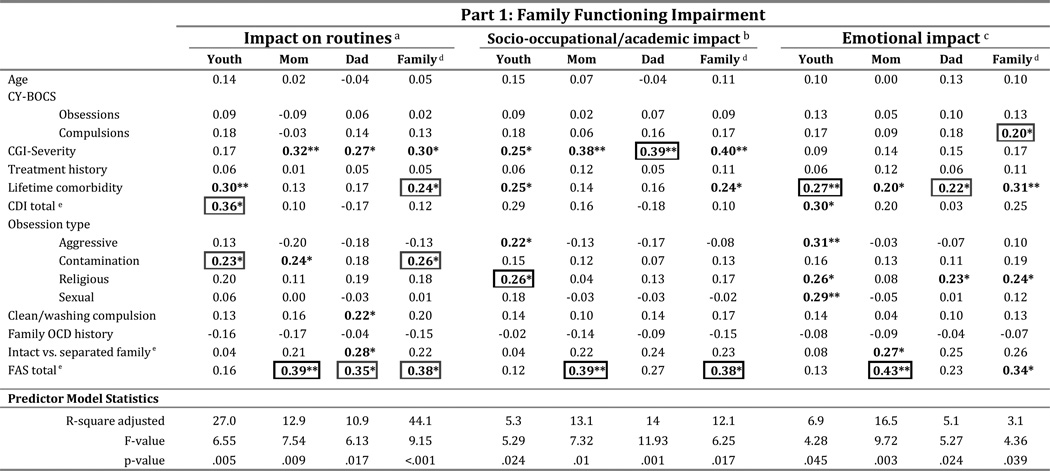
Predicting Family Function Domain Impairment
Table 3 presents correlations and predictor model statistics (adjusted R2, F- and p-values) for youth, mother, father, and combined perspectives of routine task, socio-occupational/academic and emotional aspects of family functioning. Potential predictor candidates (in boldface) were entered in separate regression models and, if found statistically significant, re-entered in a final regression model. Distinct variables (boxed numbers) were identified that significantly predicted individual perspectives and subdomains of OCD-related family impairment.
Table 3.
Correlation Coefficients for Candidate Predictors of Family Functioning Impairment at Current Obsessive-Compulsive Disorder (OCD)
Note: Boldface items indicate significant correlations and variables that were placed into the initial regression analysis. Significant correlated at the 0.01 level (2-tailed) is denoted by **, while significant correlations at the 0.05 level is denoted by *. Boxed items indicate the variables that were revealed to be significant in the final regression model. CDI = Child Depression Inventory; CGI = Clinical Global Impression; CY-BOCS = Children’s Yale-Brown Obsessive-Compulsive Scale; FAS = Family Accommodation Scale.
Impact on routines was calculated by averaging OFF scale scores for items #1–11.
Socio-occupational/academic impact was calculated by averaging OFF scale scores for items #12–17.
Emotional impact was calculated by averaging OFF scale scores for items #18–21.
Family data was calculated by averaging scores from youth, mom, and dad reports for each domain.
CDI and FAS total scores as well as whether the family is intact or separated are only available for the Vancouver site trios.
DISCUSSION
This study is the first to quantitatively highlight and detail the notable OCD-related family functioning impairment experienced by affected youth and their parents. Strengths of its design include the use of complete trios (i.e. youth, mother, and father perspectives are captured for each participating family) and recruitment of a large, multi-site sample to optimize generalizability of the findings. In this study, use of the self-report OFF scale captured impacts that would not have been revealed via standard OCD measures such as the CY-BOCS, the COIS, or the FAS-PR. Moreover, identifying correlates and predictors of OCD-related family impairment has emboldened the understanding of this important factor within the existing foundation of knowledge regarding pediatric OCD.
Cross-Site Findings
The generalizability of this study’s findings is supported by its large size and consistent findings regarding family impacts at “worst-ever” OCD across the two diverse and independent sites. The Vancouver site’s significantly greater score for “current” OCD family impairment may reflect recruitment site differences. Ages of the affected youth at ascertainment, OCD onset, and worst severity were nearly identical, indicating similar disease duration across sites. However, while many Boston participants were recruited from facilities where they received ongoing care, Vancouver participants were recruited during initial OCD program assessment, reporting significantly less treatment history (p≤.001). Vancouver participants also had higher global OCD severity scores (CGI-S, p=.006).
Family Routine Disruption
This study identified morning and bedtime routines as family activities with greatest daily impact, thus prompting clinicians to actively target these in assessment and treatment of pediatric OCD. The fallout of disrupted morning routines and concerns over late arrival at school or work may increase vulnerability to family accommodation, which is associated with poorer clinical outcomes in both adult and child populations. Interference with bedtime routines also presents a challenge with respect to maintaining stabilizing family structure. Sleep-related problems are common in OCD34, including pre-sleep arousal, decreased quality, and duration.35 In the absence of daytime distractions, youth may be increasingly distressed by obsessions prior to sleep,34 and complex bedtime rituals may become compulsive or avoidant in nature. Subsequent to sleep disruption, fatigue, lowered resilience and decreased ritual resistance may play a role in increasing OCD severity, creating a cycle by further impacting sleep problems. Parents may be enticed to provide any accommodation necessary in this setting, including sleeping in the same room as the child.34 Thus, in addition to treatment of OCD symptoms, direct coaching by the treatment team is advisable regarding sleep hygiene, management of bedtime routines, and reduction/prevention of related parental accommodation.
Emotional Family Impacts
Family function impairment was found to be greatest within emotional domains, including resultant anxiety, sadness, anger, frustration, and guilt. It is striking that the majority of youth, mothers, and fathers reported living with stress and anxiety either often or always, both at the time of assessment and at worst OCD severity. This has strong clinical implications, given that distress tolerance is required by family members in order to resist family accommodation. It suggests that modalities such as mindfulness skills training may be beneficial for family members as observed in a pilot study of parents of OCD-affected youth, in which distress tolerance was improved.36 In addition, the frequent sadness reported by parents may represent a grieving process related to their child’s diagnosis, which could lead to treatment-interfering behaviors in the home such as minimization or catastrophizing of symptoms.
Over half of youth at the time of assessment (52.1%) and over three quarters (76.6%) at worst OCD severity reported feeling frustrated and/or angry either often or all of the time. This complements recent literature based on parent and clinician reports regarding the previously under-recognized challenges of disruptive behaviour and rage in pediatric OCD.37–39 Participation in family-based CBT may assist in amelioration of both family accommodation and coercive and disruptive behaviours.40 Moreover, potential benefits of Parent Management Training augmentation of cognitive-behavioral therapy (CBT) warrant future investigation.
The fact that more youth reported ongoing guilt than fathers is also noteworthy. The role of guilt in OCD pathology has been associated with the forbidden thought symptom dimension and has been identified as a needed research area,41 given its deleterious impact on symptom disclosure, which may limit treatment gains. As such, the clinical importance of addressing underlying guilt, in addition to other emotions, is critical in OCD treatment.
Family Social, Workplace and School Impacts
Extensive socio-occupational/academic impacts and divergent perspectives across family members were found in this study. Youth reported greater personal social and school impairment related to OCD compared to their parents’ perspectives. As previously described by Peris et al.,42 psychoeducation and family therapy should focus on educating families around the functional impacts of OCD and reducing the differences in perceived impairment. This can reduce parental blame for a youth’s deteriorating grades or social isolation, thus strengthening that relationship in the fight against OCD.
Study findings also highlight the importance of seeking multiple perspectives during assessment and treatment, as these may reflect conflicting priorities and goals. For example, parents might be more concerned with their child’s academic work or family routines, and may overlook social impacts that obstruct developmental milestones related to separation and individuation.
An important yet under-recognized outcome of pediatric OCD highlighted by this study is its social and occupational impact on parents. Nearly one half of mothers (45.1%) and one third of fathers (33.3%) reported daily occupational impacts at worst OCD severity. This reflects indirect societal costs of OCD that are rarely discussed and likely underestimated.
Clinical Utility of OFF Scale Data
The importance of considering family factors in pediatric OCD assessment and treatment has become increasingly recognized over the past decade. In a clinical setting, the OFF may be used as a practical tool to target specific symptoms with greatest family impact. In this study, intrusive thoughts OCD were most often reported to cause family impairment (82.5% and 68.2% at worst ever and current timepoints, respectively), which was unexpected, as compulsions were hypothesized to exert greater family impact versus obsessions. The OFF may also identify the need for respite services (with cases of extreme emotional impacts on parents) or social services (with parental job loss, etc.).
Change in family impairment over time can be efficiently captured by comparing mean Part 1 scores from all perspectives at follow-up versus baseline. In a recent trial, it demonstrated sensitivity to change over time and significant improvement following group, family-based CBT (Stewart et al, submitted for publication). This contrasts with measures such as the family environment scale (FES), which captures trait-like aspects of family style that may be more resistant to change and less specific to OCD.
Predictors and Correlates of OCD-Related Family Impairment
The identification of predictors of family function and its domains was illuminating. Family accommodation emerged as the only significant predictor for overall family impairment, as reported from combined (p=.002; adjusted R2= 12.1%), mother (p=.006; adjusted R2= 14.3%) and father (p=.025; adjusted R2= 9.0%) perspectives. Whereas compulsion severity was the only predictor of the youth’s perspective, this latter model captured very little variance in the data (p=.04; adjusted R2=3.1%), decreasing the utility of this finding. However, it is of interest that compulsion severity has also been identified as a predictor of parental accommodation in pediatric OCD.43
Regarding function domains, as demonstrated by the adjusted R-square values found in Table 3 for overall family reports, predictor models captured more variance for family routine disruption (R square adj= 44.1%, p<.001) compared to those for socio-occupational/academic (R square adj= 12.1%, p=.017) and emotional (R square adj= 3.1%, p=.039) family impacts. This may reflect the fact that family routines are more readily and objectively observable than experienced emotions.
With respect to family routine task impairment, contamination obsessions and lifetime comorbidity/depression severity were identified as significant predictors in addition to family accommodation. Of note, comorbidity has also been identified as a predictor of poor CBT outcome in pediatric OCD.44 Regression models for socio-occupational/academic impact prediction differed across family members, with religious obsessions, family accommodation, and overall CGI severity as the sole identified predictors for youth, mother, and father perspectives, respectively. Compulsion severity predicted emotional impacts from combined perspectives, with comorbidity predicting youth and father reports and family accommodation predicting mother reports.
Reinforcing the urgency to clinically address this factor, increased family accommodation emerged as a significant predictor of either combined family, mother, or father reports of overall family impairment and all of its subdomains. Whereas family accommodation did not predict any youth-reported scores, this factor was more important from maternal perspectives where it significantly predicted across all domains. Hence, OCD-related family impairment has now been added to the empirically demonstrated list of negative outcomes associated with family accommodation.
While excluded from the final prediction models, several other factors were initially entered into regression analyses due to significant correlations with aspects of family functioning. Intrusive thoughts were correlated with youth-reported emotional and socio-occupational academic impairment. This suggests that OCD symptom type impacts the domain of impairment, with contamination obsessions interfering with home routines and sexual/religious obsessions interfering with function outside the home in social, academic, and work domains. Non-intact marital status was also found to be an important variable as it correlated with paternal views of increased family routine impairment and with maternal views of increased family emotion impacts. These potential associations are worthy of future study and consideration in clinical settings.
There are several methodological limitations that must be acknowledged. Recruitment sites differed with respect to diagnostic assessment, treatment history, CGI, CY-BOCS, and current family functioning scores. However, the consistency in reported impairment scores for worst illness severity across sites lends support to the findings with respect to the extent of family impairment and recall of this experience. While the large majority of participants received structured interviews to confirm OCD diagnosis, participants from MGH and OCDI (n=8 trios), received diagnostic confirmation through clinician assessments only. Although this theoretically introduces the risk for inclusion of non-OCD probands, the expertise and OCD specialization of these MD- and PhD-level clinicians mitigates this limitation.
The OFF scale solicits information about routine task impairment frequency, which is influenced by the variable expected frequency for separate routines. Impacts on family appointments, restaurant outings, religious events, and shopping may have been underrepresented as they are not typically daily events, and as the scale captures temporal impacts rather than the proportion of these events that are impacted.
Statistically significant differences identified across relative perspectives were based upon relatively small absolute score differences, which may or may not translate into clinically meaningful differences. However, the identification of distinct, clinically-based predictors of these different perspectives suggests that identified differences are relevant. This requires further study. While missing data for variables considered in correlation and regression analyses limited statistical power of regression analyses, this study did succeed in identifying significant predictors of impairment.
In conclusion, this multi-site study details significant familial impacts of pediatric OCD, changes with illness severity, and contrasting perspectives across relatives. It utilizes the validated OFF scale to capture disease morbidity from a non-traditional yet clinically relevant angle. Clinically, these results highlight the need for routine screening and a multi-informant approach with respect to family impacts in pediatric OCD. It behooves clinicians and future researchers to fully consider the multidimensional and far-reaching impacts of pediatric OCD.
Supplementary Material
Clinical Guidance.
Pediatric OCD-related family impairment is predicted by increased family accommodation and should not be underestimated.
Meals, mornings, and bedtimes are commonly disrupted family routines, as predicted by family accommodation, contamination obsessions, and comorbidities.
Parents under-recognize social and academic impacts of OCD on their child, potentially driving misdirected blame for deteriorating grades and social isolation.
Occupational impacts occur on a daily basis in nearly one half of mothers (45.1%) and one third of fathers (33.3%) of youth with OCD, urging appropriate intervention.
Multiple perspectives are required to obtain an accurate assessment of family impairment in pediatric OCD.
Acknowledgments
This work was supported by funding from the Michael Smith Foundation for Health Research (MSFHR) and the Canadian Institutes for Health Research (CIHR) awarded to Dr. Stewart, and funding from the National Institute of Mental Health (NIMH) awarded to Dr. Pauls.
The authors would like to acknowledge the OCD Collaborative Genetics Association Study (OCGAS) and the PI, Gerry Nestadt, MBBCh, MPH, from the main Johns Hopkins site.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This study was presented as an abstract at the American Academy of Child and Adolescent Psychiatry’s 62nd Annual Meeting, San Antonio, TX, October 26–31, 2015. Dr. Pauls served as the statistical expert for this research.
Disclosure: Dr. Stewart serves on the Scientific and Clinical Advisory Board of the International OCD Foundation and served as a Medical Advisory Board Member of the Tourette Association of America between 2012–2016. Dr. Geller has received grant or research support from the National Institute of Mental Health, Pfizer, Eli Lilly and Co., GlaxoSmithKline, Otsuka, Forest, Shire, and Neurocrine. He has received honoraria from the American Academy of Child and Adolescent Psychiatry and the Massachusetts General Hospital Psychiatry Academy. He has served on the speakers’ bureau of Eli Lilly and Co. Drs. Hu, Leung, Pauls and Mss. Chan, Hezel, Lin, Belschner, Walsh report no biomedical financial interests or potential conflicts of interest.
REFERENCES
- 1.Ayuso-Mateos J. Global Burden of obsessive-compulsive disorder in the year 2000. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 2.Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D. Family accommodation in obsessive-compulsive disorder: Relation to symptom dimensions, clinical and family characteristics. Psychiatry Res. 2010;179:204–211. doi: 10.1016/j.psychres.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Calvocoressi L, Lewis B, Harris M, et al. Family accommodation in obsessive-compulsive disorder. Am J Psychiatry. 1995;152:441–443. doi: 10.1176/ajp.152.3.441. [DOI] [PubMed] [Google Scholar]
- 4.Cooper M. Obsessive-compulsive disorder: effects on family members. Am J Orthopsychiatry. 1996;66:296–304. doi: 10.1037/h0080180. [DOI] [PubMed] [Google Scholar]
- 5.Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. J Consult Clin Psychol. 2009;77:355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of Accommodation of Pediatric Obsessive-Compulsive Disorder: Parent, Child, and Family Characteristics. J Am Acad Child Adolesc Psychiatry. 2008;47:1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waters TL, Barrett PM. The role of the family in childhood obsessive-compulsive disorder. Clin Child Fam Psychol Rev. 2000;3:173–184. doi: 10.1023/a:1009551325629. [DOI] [PubMed] [Google Scholar]
- 8.Stewart SE, Beresin C, Haddad S, Egan Stack D, Fama J, Jenike M. Predictors of family accommodation in obsessive-compulsive disorder. Ann Clin Psychiatry. 2008;20:65–70. doi: 10.1080/10401230802017043. [DOI] [PubMed] [Google Scholar]
- 9.Storch EA, Geffken GR, Merlo LJ, et al. Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol. 2007;36:207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- 10.Van Noppen B, Steketee G. Testing a conceptual model of patient and family predictors of obsessive compulsive disorder (OCD) symptoms. Behav Res Ther. 2009;47:18–25. doi: 10.1016/j.brat.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Freeman JB, Garcia AM, Fucci C, Karitani M, Miller L, Leonard HL. Family-based treatment of early-onset obsessive-compulsive disorder. J Child Adolesc Psychopharmacol. 2003;13(Suppl 1):71–80. doi: 10.1089/104454603322126368. [DOI] [PubMed] [Google Scholar]
- 12.Garcia AM, Sapyta JJ, Moore PS, et al. Predictors and Moderators of Treatment Outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I) J Am Acad Child Adolesc Psychiatry. 2010;49:1024–1033. doi: 10.1016/j.jaac.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smorti M. The Impact of Family on Obsessive Compulsive Disorder in Children and Adolescents: Development, Maintenance, and Family Psychological Treatment. J Adv in Psychol. 2012;1:86–94. [Google Scholar]
- 14.Vikas A, Avasthi A, Sharan P. Psychosocial impact of obsessive-compulsive disorder on s and their caregivers: a comparative study with depressive disorder. Int J Soc Psychiatry. 2011;57:45–56. doi: 10.1177/0020764009347333. [DOI] [PubMed] [Google Scholar]
- 15.Chambless DL, Bryan AD, Aiken LS, Steketee G, Hooley JM. Predicting expressed emotion: a study with families of obsessive-compulsive and agoraphobic outpatients. J Fam Psychol. 2001;15:225–240. doi: 10.1037//0893-3200.15.2.225. [DOI] [PubMed] [Google Scholar]
- 16.Hibbs ED, Zahn TP, Hamburger SD, Kruesi MM, Rapoport JL. Parental expressed emotion and psychophysiological reactivity in disturbed and normal children. Br J Psychiatry. 1992;160:504–510. doi: 10.1192/bjp.160.4.504. [DOI] [PubMed] [Google Scholar]
- 17.Peris TS, Miklowitz DJ. Parental Expressed Emotion and Youth Psychopathology: New Directions for an Old Construct. Child Psychiatry Hum Dev. 2015;46:863–873. doi: 10.1007/s10578-014-0526-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Renshaw KD, Chambless DL, Steketee G. The relationship of relatives’ attributions to their expressed emotion and to patients’ improvement in treatment for anxiety disorders. Behav Ther. 2006;37:159–169. doi: 10.1016/j.beth.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Peris TS, Piacentini J. Optimizing treatment for complex cases of childhood obsessive compulsive disorder: a preliminary trial. J Clin Child Adolesc Psychol. 2013;42:1–8. doi: 10.1080/15374416.2012.673162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peris TS, Sugar CA, Bergman RL, Chang S, Langley A, Piacentini J. Family factors predict treatment outcome for pediatric obsessive-compulsive disorder. J Consult Clin Psychol. 2012;80:255–263. doi: 10.1037/a0027084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy YE, Flessner CA. Family functioning in paediatric obsessive compulsive and related disorders. Br J Clin Psychol. 2015;54:414–434. doi: 10.1111/bjc.12088. [DOI] [PubMed] [Google Scholar]
- 22.Przeworski A, Zoellner LA, Franklin ME, et al. Maternal and child expressed emotion as predictors of treatment response in pediatric obsessive-compulsive disorder. Child Psychiatry Hum Dev. 2012;43:337–353. doi: 10.1007/s10578-011-0268-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M. Functional impairment in childhood OCD: development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale-Revised (COIS-R) J Clin Child Adolesc. 2007;36:645–653. doi: 10.1080/15374410701662790. [DOI] [PubMed] [Google Scholar]
- 24.Stewart SE, Hu YP, Hezel DM, et al. Development and psychometric properties of the OCD Family Functioning (OFF) Scale. J Fam Psychol. 2011;25:434–443. doi: 10.1037/a0023735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav Res Ther. 2004;42:813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- 26.Canavera KE, Wilkins KC, Pincus DB, Ehrenreich-Ma JT. Parent-child agreement in the assessment of obsessive-compulsive disorder. J Clin Child Adolesc Psychol. 2009;38:909–915. doi: 10.1080/15374410903258975. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 28.Samuels JF, Riddle MA, Greenberg BD, et al. The OCD collaborative genetics study: methods and sample description. Am J Med Genet B Neuropsychiatr Genet. 2006;141B:201–207. doi: 10.1002/ajmg.b.30224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV - Child and Parent versions. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 30.Scahill L, Riddle MA, McSwiggin-Hardi M, et al. Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- 31.Kovacs M. Children’s Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- 32.Guy W. Clinical Global Impression Scale (CGI) ECDEU assessment manual for psychopharmacology. Rockville, MD: NIMH, Psychopharmacology Research Branch; 1976. pp. 217–222. [Google Scholar]
- 33.IBM Corp. IBM SPSS Statistics for Macintosh, Version 23.0. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 34.Ivarsson T, Skarphedinsson G. Sleep problems and cognitive behavior therapy in pediatric obsessive-compulsive disorder have bidirectional effects. J Anxiety Disord. 2015;30:28–33. doi: 10.1016/j.janxdis.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Jaspers-Fayer F. A sleep study in pediatric obsessive-compulsive disorder (OCD): Pilot actigraphy findings. Presented as part of The Child and Family Research Institute’s signature seminar series; December 18, 2015; Vancouver, BC. [Google Scholar]
- 36.Bleakley C, Edalati K, Ellwyn R, Jaspers-Fayer F, Stewart SE. Parent Mindfulness Skills Training vs. Peer Support for Parents of Obsessive-Compulsive Disorder affected Children -Early results. Presented as part of 30th Annual University of British Columbia Department of Psychiatry Research Day; June 18, 2015; Vancouver, BC. [Google Scholar]
- 37.Storch EA, Jones AM, Lack CW, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51:582–592. doi: 10.1016/j.jaac.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 38.Lebowitz ER, Storch EA, MacLeod J, Leckman JF. Clinical and Family Correlates of Coercive-Disruptive Behavior in Children and Adolescents with Obsessive-Compulsive Disorder. J of Ch and Family Studies. 2015;24:2589–2597. [Google Scholar]
- 39.Lebowitz ER. Parent-Based Treatment for Childhood and Adolescent OCD. J Obsessive Compuls Relat Disord. 2013;2:425–431. [Google Scholar]
- 40.Bleakley CV, Chan E, Ellwyn R, et al. Coercive and Disruptive Symptoms in Pediatric Obsessive Compulsive Disorder: Prevalence and Response to Treatment. Presented as part of the of the American Academy of Child and Adolescent Psychiatry’s 62nd annual meeting; October 29, 2015; San Antonio, TX. [Google Scholar]
- 41.Shapiro LJ, Stewart ES. Pathological guilt: a persistent yet overlooked treatment factor in obsessive-compulsive disorder. Ann Clin Psychiatry. 2011;23:63–70. [PubMed] [Google Scholar]
- 42.Peris TS, Sugar CA, Bergman RL, Chang S, Langley A, Piacentini J. Family factors predict treatment outcome for pediatric obsessive-compulsive disorder. J Consult Clin Psychol. 2012;80:255–263. doi: 10.1037/a0027084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flessner CA, Freeman JB, Sapyta J, et al. Predictors of Parental Accommodation in Pediatric Obsessive-Compulsive Disorder: Findings from the Pediatric Obsessive-Compulsive Disorder Treatment Study (POTS) Trial. J Am Acad Child Adolesc Psychiatry. 2011;50:716–725. doi: 10.1016/j.jaac.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Storch EA, Merlo LJ, Larson MJ, et al. Impact of comorbidity on cognitive-behavioral therapy response in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:583–592. doi: 10.1097/CHI.0b013e31816774b1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.