Abstract
Fostering children is common in sub-Saharan Africa, but few studies examine these children’s mental health needs. This study investigated the impact of living in a foster family on the mental health of HIV-positive, HIV-affected and HIV-unaffected children (n = 681 aged 10–17) in rural Rwanda. Regression analyses assessed the impact of living in a foster family on mental health, parenting, and daily hardships; multiple mediation analyses assessed whether family factors mediated the association between foster status and mental health. HIV-positive children were eight times more likely to live in foster families than HIV-unaffected children. Being HIV-affected was predictive of depression and irritability symptoms after controlling for family factors. Controlling for HIV-status, foster children had more symptoms of depression, anxiety, and irritability than non-fostered children. Positive parenting fully mediated the association between foster status and mental health. Mental health and parenting interventions for foster children and HIV-affected children may improve child outcomes.
Keywords: HIV, Adolescents, Foster children, Mental health, Sub-Saharan Africa
Background
In many parts of the world, the combination of HIV and AIDS, conflict, and chronic poverty have left thousands of children living with caregivers who are not their biological parents. In Rwanda, it is estimated that over half a million children have lost one or both of their parents [1]. Extended family networks were destroyed after the 1994 Genocide through the death of nearly a million people (10 % of the population), displacement of more than two million refugees, and mass imprisonment [2]. The AIDS epidemic in Rwanda has also contributed to tremendous family separation and loss [3]. According to UNAIDs, there were 22,000 children in Rwanda living with HIV in 2014 and 85,000 orphans due to AIDS in 2014 [4]. Although it is likely that Rwanda’s comprehensive HIV/AIDS response has prevented the pandemic from spreading at rates similar to other countries in sub-Saharan Africa (SSA), HIV/AIDS remains a significant contributor of vulnerability in children [4].
Loss of support from an adult exposes children to distress resulting from lack of affection, insecurity, fear, loneliness, grief, or despair [5]. This study examines the role of HIV in the family on the likelihood of living in a foster home without a biological parent and how family factors such as parenting, support, and hardships differ between foster and non-foster families and contribute to mental health outcomes in children affected and unaffected by HIV.
In Rwanda, as in the rest of SSA, fostering of orphaned or abandoned children is common [6]. In SSA, nearly all orphans are taken in by extended family members [6] and the economic burden on foster families can be high [7]. Further, the safety net for orphaned and abandoned children is thinning, with communities overwhelmed and unable to absorb all of the children, yet there is a push for family-based care over institutions [8]. Quality of care in foster families may be affected by socioeconomic challenges, such as high dependency ratios with a large population of children relying on much smaller population of working-age adults for support [6] and a need for extensive support [9].
AIDS-orphaned children often face compounded adversities such as poverty and stigma that further complicate the process of adjusting to parental death [10]. Often these children end up in informal foster care, child-headed households, or orphanages. Orphaned children living in foster families may face maltreatment or inequality in the household [11, 12], more engagement in child labor [13], school dropout [14] or falling behind in school [14, 15], poorer health outcomes, and greater psychological distress [16, 17]. In Rwanda, children living with HIV and children living with a caregiver with HIV have much higher rates of depression, anxiety, conduct problems and functional impairment compared with HIV-unaffected children [18]. One reason for the increased mental health risk observed in HIV-positive and HIV-affected children may be differences in parenting practices between biological parents and foster families, as HIV-affected and HIV-positive children in Rwanda are more likely to have experienced the death of a caregiver, and HIV-positive children are less likely to have their biological mother as their primary caregiver [18].
Positive home environments are critical for children’s mental health; inadequate parenting and child maltreatment cause toxic levels of stress that can contribute to delinquency and greater risk of depression and anxiety [19–21]. An extensive body of research has shown how support from caregivers can protect children from the negative, compounding effects of stress even in the face of adversities such as poverty or chronic illness [22]. Studies have shown that the family environment of AIDS-orphaned children, such as having ill caregivers or experiencing maltreatment, can mediate depression in children [23]; however, more research is needed to better understand the experiences and potential risk factors of children living in foster families as there is little research on parenting practices in these households.
This study is a secondary analysis of existing data on HIV-positive children, HIV-affected (i.e., HIV-negative children with an HIV-positive caregiver), and HIV-unaffected children in Rwanda [18]. The goals of the present study were to compare symptoms of depression, anxiety, irritability, and conduct problems among fostered children and children living with at least one biological parent before and after controlling for HIV-status. The study further assesses whether family factors, including family unity, parenting, and daily hardships, mediate associations between foster status and mental health. It was hypothesized that HIV-positive children would be more likely to live in foster homes, that children living in foster families would have worse mental health outcomes, and that family factors would act as mediators in this relationship.
Methods
Participants
This study received approval from the Harvard T.H. Chan School of Public Health Office of Human Research Administration and the Rwanda National Ethics Committee and was a collaboration between the Harvard School of Public Health, Partners In Health/Inshuti Mu Buzima (PIH/IMB), and the Rwandan Ministry of Health. Parent/guardian informed consent and child assent were obtained from all study participants. This study was conducted from March to December 2012 and detailed methods have been published previously [18]. Children between the ages of 10–17 living in southern Kayonza and Kirehe Districts were recruited in three groups based on HIV status: HIV-positive, HIV-affected (HIV-negative children living with an HIV-positive caregiver) and HIV-unaffected. Children were eligible for the study if they were 10–17 years of age and had resided in southern Kayonza or Kirehe Districts for at least one month. For each child, a co-resident adult caregiver was enrolled and asked to report on household characteristics and their own mental health; ‘caregiver’ was defined as an adult living in the household that serves as the primary caregiver to the child in the study. For fostered children, caregivers were predominantly relatives (86.6 %). In the case of non-fostered children, the co-resident adult caregiver was a biological parent. Participants were excluded if trained study members identified cognitive impairment compromising the child’s ability to understand the assent procedures and measures. Interviews were conducted by local research assistants blinded to the child’s HIV-status who were trained in research ethics and how to respond in the case of severe mental health symptoms, abuse, or suicidal ideation. Each assenting/consenting participant took part in an approximately 2-h interview. Child and caregiver interviews were conducted in the local language (Kinyarwanda) simultaneously in private locations apart from one another.
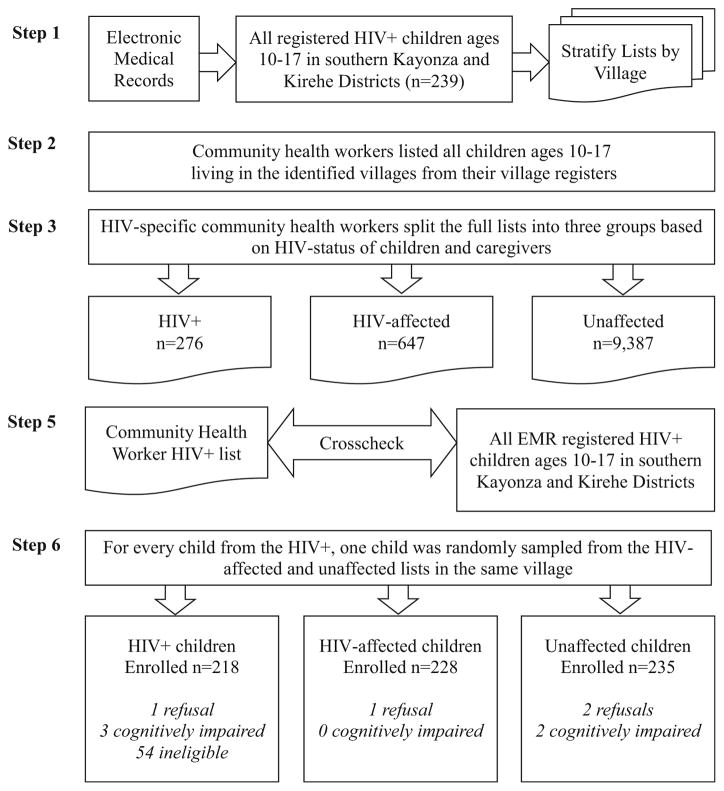
Sampling Procedure
The sampling procedure followed steps outlined in Fig. 1. First, HIV-positive children ages 10–17 were identified in the public health system’s electronic medical records (EMR), which maintains records of all identified HIV-positive patients in the study districts. HIV-positive children were stratified by their village of residence. Next, community health workers (CHWs) listed all children ages 10–17 in the identified villages using village registers which include demographic information for every resident in the village. Then specialized CHWs responsible for providing community-based HIV care to known HIV-positive patients split the list of all children into three groups based on HIV-status of children and the caregivers in the home: HIV-positive children, HIV-affected children, and unaffected children. HIV-affected children were identified as any children on the list living with a known HIV-positive caregiver. Lists of HIV-positive children from CHWs and the EMR were crosschecked, resulting in the identification of an additional 37 HIV-positive children not yet entered in the EMR. Cases of individuals not entered in the EMR can be due to a number of reasons such as relocation or a backlog of entering patient information into the system. Fifty-four HIV-positive children were ineligible primarily because they had moved out of the study area (39 % of ineligible children), were unable to be located based on geographic information (31 %), or had since retested HIV-negative (19 %).
Fig. 1.
Sampling procedure
Measures
Previous qualitative studies including free-listing and key informant interviews were used to identify mental health symptoms of children affected by HIV in Rwanda and relevant protective factors such as positive parenting and family support [24, 25]. Mixed methods were used to develop, adapt, and validate mental health measures and measures of protective processes in the family and community in Rwanda during earlier phases of research [26–28]. Standardized measures were reviewed and used when they showed alignment with local constructs in related qualitative data (i.e., at least half of the items were conceptually equivalent to local indicators of mental health syndromes or protective factors) [24, 29]. These measures were then adapted and translated using a rigorous process of forward and backward translations [26, 27].
The Center for Epidemiological Studies Depression Scale for Children (CES-DC) [30] was adapted to measure depression (agahinda kenshi and kwiheba) [25]. The adapted CES-DC [26] contains the 20 original items and 10 items from qualitative data. The original scale was validated by comparing scores on the CES-DC with a clinical assessment completed by a Rwandan psychologist using a structured diagnostic interview tool, the Mini International Neuropsychiatric Interview for Children [31]. The CES-DC scale was scored 0 (never) to 3 (often), and the scale score was the sum. The complete 30-item CES-DC performed well in our validation study (α = .86, test–retest r = .85), and internal reliability in this sample was excellent (α = .92).
An adapted Youth Self-Report (YSR) Internalizing Subscale [32] measured symptoms of internalizing problems or mixed anxiety and depression symptoms (guhan-gayika) [25]. The adapted YSR contains 23 items, 16 from the original scale and 7 derived from qualitative data. Scoring was 0 (not at all true) to 2 (often true), and scored as the mean. The adapted internalizing problems scale performed well in our validation study (α = .93, test–retest r = .85) and internal reliability in this sample was excellent (α = .92).
Conduct problems (uburara) were measured using a scale derived from qualitative data that included salient indicators of conduct problems since standardized measures of conduct disorder did not match well with local constructs [28]. The scale contains 11 items scored 0 (never) to 3 (often) and was scored as the mean. Examples of items included “I fought,” “I spoke rudely,” and “I roamed around.” The scale performed well in validity testing (α = .89, test–retest r = .58) and internal reliability in this sample was excellent (α = .89).
Irritability (umushiha) was measured by an adapted Irritability Questionnaire [33] containing 27 items, 21 from the original measure and 6 drawn from qualitative data. Items were scored from 0 (never) to 3 (often), and the scale score was the mean. The scale performed well in our validation study (α = .92, test–retest r = .84), and the internal reliability of this sample was excellent (α = .92).
Parenting was measured using measures of positive parenting and harsh discipline. Positive parenting was measured by 16 locally derived items to capture the concept “uburere bwiza” (good parenting) [24] and 16 items from the Parental Acceptance and Rejection Questionnaire [34]. Positive parenting was scored on four-point Likert scale 0 (never) to 3 (every day) and the scale score was the mean with higher scores indicating more positive parenting behaviors. Examples of locally derived parenting items included, “My caregiver converses with me,” “My caregiver raises me well for the good of Rwanda,” and “My caregiver expresses love to me.” The local positive parenting scale performed well in validity testing (α = .94, test–retest r = .87) and the combined scale had excellent internal reliability in this sample (α = .93).
Two types of harsh discipline, psychological aggression and physical punishment, were measured by a 12-item scale adapted from UNICEF’s Multiple Indicator Cluster Survey [35] (α = .78 in this sample). Items were scored 0 = No, 1 = Yes, and the subscales for physical punishment and psychological aggression were scored as a binary variable of whether or not the child reported each form of punishment in the past month.
Family-level factors included family trust and unity, daily hardships, and household socio-economic status (SES). Family trust and unity (kwizerana) [24], was assessed by a scale derived from locally relevant indicators of the construct drawn from a prior qualitative research in Rwanda [24]. The scale contains 15 items scored 0 (never) to 3 (every day) with a total score comprising the mean. Examples of items are, “We are united,” and “we are happy and joyful together”. The scale performed well during validity testing (α = .93, test–retest r = .76) and showed excellent internal consistency in this sample (α = .93). Daily hardships were measured by an adapted version of the Post-War Adversities Index (18 items) [36], which had been used previously in SSA and included items such as food insecurity and conflict or illness in the family. Internal consistency in this sample was good (α = .80).
Caregivers completed the wealth index [37] from the Rwanda Demographic and Health Survey as an indicator of SES. Caregiver’s mental health was assessed using the Hopkins Symptom Checklist, a 25-item measure of depression and anxiety previously tested and validated for use in Rwanda [38] (α = .94 in this sample).
Data Analysis
T-tests and Chi squared tests were used to assess differences in demographic characteristics among fostered and non-fostered children. Effect size for differences among fostered and non-fostered children were calculated using Cohen’s d. Logistic regression was used to assess the likelihood of HIV-status predicting living in a foster family. Multiple linear regression analyses were used to assess the association of living in a foster family with mental health outcomes of depression, anxiety, conduct problems, and irritability in a multi-step procedure that assessed HIV-status and foster family status independent of parenting and family level factors, then measures of positive parenting, psychological aggression, physical punishment, and daily hardships were added to the model. Multiple linear regressions were also used to assess the association of living in a foster family with parenting practices. Preacher and Hayes’ multiple mediation approach [39] using bias-corrected bootstrapped confidence intervals from 5000 repetitions was used to assess the significance of the indirect effects from living in a foster family to child mental health for each family-level factor. All final regression models controlled for age, sex, and socio-economic status. Data was analyzed using STATA version 12.0 [40].
Results
HIV and Foster Family-Status
The final sample was 681 children, with 17 % of children (n = 119) living in a foster family. Within the sample, 218 (32.0 %) children were HIV-positive, 228 (33.5 %) HIV-affected, and 235 (34.5 %) unaffected by HIV. Demographic information by foster status is in Table 1. The great majority of foster children (86.6 %) were living with other family members. HIV-positive children were almost eight times more likely to live in foster families than unaffected children (Odds Ratio [OR] 7.88, 95 % Confidence Interval [CI] 4.45–13.93, p <.001); however, HIV-affected children were not more likely to live in foster homes (OR 1.27, 95 % CI 0.64–2.50, p = .49) than unaffected children. Households with foster children reported significantly higher SES (Mean [M] = .18, SD = 1.1) than households without foster children (M = −.41, SD = .97; t(667) = −2.24, p = .03).
Table 1.
Demographic characteristics
| All (N = 681)a | Foster children (N = 119) | Non-fostered children (N = 552) | Test statistic t(669) or X2 p |
Cohen’s d (95 % CI) | |
|---|---|---|---|---|---|
| Child characteristics, n (%) unless otherwise noted | |||||
| Age, mean (SD) | 13.60 (2.19) | 13.95 (2.28) | 13.53 (2.16) | t = −1.93 p = .054 |
0.19 (−.004, .39) |
| Female | 346 (51.56) | 60 (50.42) | 286 (51.81) |
X2 = .08 p = .78 |
−0.03 (−.25, .19) |
| Attending school | 602 (90.25) | 110 (94.02) | 492 (89.45) |
X2 = 2.28 p = .13 |
0.34 (−.11, .79) |
| HIV-positive | 218 (32.01) | 82 (68.91) | 132 (23.91) |
X2 = 91.24 p <.001 |
1.08 (.84, 1.32) |
| HIV-affected | 228 (33.48) | 20 (16.81) | 205 (37.14) |
X2 = 18.16 p <.001 |
0.59 (.31, .87) |
| Unaffected | 235 (34.51) | 17 (14.29) | 215 (38.95) |
X2 = 26.33 p <.001 |
0.74 (1.04, .44) |
| Any caregiver death | 190 (28.66) | 72 (61.02) | 118 (21.65) |
X2 = 73.52 p <.001 |
0.96 (.72, 1.19) |
| Mother diedb | 54 (8.02) | 29 (24.58) | 23 (4.22) |
X2 = 55.61 p <.001 |
1.1 (.78, 1.43) |
| Father diedb | 137 (20.33) | 41 (34.75) | 93 (17.03) |
X2 = 18.90 p <.001 |
0.53 (.28, .77) |
| Caregiver abandonment | 55 (8.20) | 11 (9.48) | 42 (7.69) |
X2 = 0.42 p = .52 |
0.01 (−.37, .39) |
| Caregiver characteristics, n (%) unless otherwise noted | |||||
| Age, mean (SD) | 44.63 (11.35) | 50.55 (18.69) | 43.41 (8.57) | t = −6.40 p <.001 |
0.65 (.45, .85) |
| Female | 542 (79.59) | 100 (84.03) | 433 (78.44) |
X2 = 1.87 p = .17 |
0.2 (−.09, .50) |
| SES, mean (SD) | .003 (1.00) | .18 (1.12) | −.04 (.97) | t(667) = −2.24 p = .03 |
0.23 (.03, .42) |
| Relative of foster child | – | 103 (86.55) | – | ||
| Ever attended school | 477 (70.04) | 42 (35.29) | 190 (34.42) |
X2 = .03 p = .86 |
0.01 (−.14, .16)) |
| Married/living with partner | 326 (47.94) | 44 (36.97) | 279 (50.64) |
X2 = 7.31 p = .007 |
−0.31 (−.53, −.08) |
| # Children in household, mean (SD) | 4.30 (1.85) | 3.72 (2.05) | 4.42 (1.78) | t = 3.80 p <.001 |
0.38 (.19, .58) |
| Mental health, mean (SD) | 1.09 (.63) | .96 (.60) | 1.11 (.64) | t = 2.43 p = .02 |
0.25 (.05, .44) |
| Child mental health outcomes, mean (SD) | |||||
| Depression | 29.58 (18.45) | 32.71 (18.58) | 28.94 (18.35) | t = −2.03 p = .04 |
0.21 (.01, .40) |
| Anxiety | .59 (.46) | .70 (.50) | .57 (.45) | t = −3.02 p = .003 |
0.31 (.11, .50) |
| Conduct problems | .38 (.54) | .41 (.56) | .37 (.54) | t = −0.77 p = .44 |
0.08 (−.12, .28) |
| Irritability | 1.00 (.56) | 1.11 (.59) | .98 (.55) | t = −2.39 p = .02 |
0.24 (.04, .44) |
| Child reported parenting/household factors, mean (SD) | |||||
| Positive parenting | 2.38 (.54) | 2.23 (.63) | 2.42 (.52) | t = 3.42 p <.001 |
0.35 (.15, .54) |
| Psychological aggression | .50 (.50) | .61 (.49) | .47 (.50) | t = −2.83 p = .005 |
0.29 (.09, .48) |
| Physical punishment | .63 (.48) | .66 (.48) | .62 (.49) | t = −0.77 p = .44 |
0.08 (−.12, .28) |
| Family unity | 2.50 (.60) | 2.29 (.77) | 2.55 (.55) | t = 4.39 p <.001 |
0.44 (.24, .64) |
| Daily hardships | 3.11 (3.11) | 3.09 (3.04) | 3.10 (3.12) | t = .05 p = .96 |
0.005 (−.19, .20) |
Not all rows add up to 681 due to missing reports on some variables
These may be underestimates, as the response options only allowed children to report if either their mother or father had died, but not both. We are therefore also unable to report rates of double-orphans
Mental Health and Parenting by Foster Family-Status
See Table 1 for complete results. Compared to children living with at least one biological parent, children living in foster families were much more likely to report greater symptoms of depression (M = 32.71, SD = 18.58 foster children vs. M = 28.94, SD = 18.35 non-fostered children; t(669) = −2.03, p = .04), anxiety (M = .70, SD = .50 vs. M = .57, SD = .45; t(669) = −3.02, p = .003), and irritability (M = 1.11, SD = .59 vs. M = .98, SD = .55; t(669) = −2.39, p = .02). They also reported less positive parenting practices (M = 2.23, SD = .63 vs. 2.42, SD = .52; t(669) = 3.42, p <.001), greater use of psychological aggression as a form of discipline by their caregiver (M = .61, SD = .49 vs. M = .47, SD = .50; t(669) = −2.83, p = .005) and less family unity (M = 2.29, SD = .77 vs. M = 2.55, SD = .55; t(669) = 4.39, p <.001).
Caregivers of foster children tended to be older (M = 50.55, SD = 18.69 vs. M = 43.41, SD = 8.57; t(669) = −6.40, p <.001), more educated (72.27 % completed primary school vs. 62.32 %, X2 = .03), currently not married or living with a partner (36.97 vs. 50.64 %; X2 = 7.31, p = .007), have fewer children in the home (M = 3.72, SD = 2.05 vs. M = 4.42, SD = 1.78; t(669) = 3.80, p <.001), when compared to caregivers of non-fostered children. Additionally, caregivers of foster children reported fewer symptoms of distress themselves (M = .96, SD = .60 vs. M = 1.11, SD = .64; t(669) = 2.43, p = .02) compared to caregivers of non-fostered children.
HIV and Foster-Family Status Predicting Parenting, Family Unity, and Daily Hardships
Results of linear regression analyses with family factor outcomes are shown in Table 2. HIV-positive status did not predict any family factors, but children who were HIV-affected reported worse parenting (B = −.12 [95 % CI = −.22, −.02], p = .02), less family unity (B = −.12 [−.23, −.01], p = .03) and more daily hardships (B = .73 [.18, 1.29], p = .01). Children who lived in foster families reported experiencing less positive parenting (B = −.20 [−.31, −.08], p = .001), more psychological aggression (B = .15 [.05, .26], p = .005), and less family unity (B = −.27 [−.39, −.14], p <.001) than children living with at least one biological parent.
Table 2.
Predictors of child-reported parenting practices, family unity and daily hardships
| Variable | Positive parenting
|
Psychological aggression
|
Physical punishment
|
Family unity
|
Daily hardships
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient (95 % CI) | p | Coefficient (95 % CI) | p | Coefficient (95 % CI) | p | Coefficient (95 % CI) | p | Coefficient (95 % CI) | p | |
| Sex | −.03 (−.12, .04) | .34 | .01 (−.07, .08) | .89 | .03 (−.04, .10) | .42 | −.04 (−.13, .05) | .34 | .01 (−.45, .47) | .96 |
| Age | −.03 (−.05, −.02) | <.001 | .02 (.002, .04) | .03 | −.02 (−.04, −.01) | .006 | −.03 (−.05, −.01) | .01 | .29 (.18, .39) | <.001 |
| SES | .06 (.02, .10) | .01 | −.02 (−.06, .02) | .36 | −.02 (−.06, .01) | .24 | .06 (.01, .10) | .02 | −.46 (−.69, −.23) | <.001 |
| HIV-positive | −.03 (−.13, .08) | .63 | −.03 (−.09, .10) | .53 | .07 (−.03, .17) | 0.15 | −.05 (−.17, .06) | .37 | .05 (−.54, .65) | .86 |
| HIV-affected | −.12 (−.22, −.02) | .02 | .004 (−.09, .10) | 0.93 | .04 (−.05, .13) | 0.38 | −.12 (−.23, −.01) | .03 | .73 (.18, 1.29) | .01 |
| Foster family | −.20 (−.31, −.08) | .001 | .15 (.05, .26) | 0.005 | .03 (−.07, .13) | 0.58 | −.27 (−.39, −.14) | <.001 | .10 (−.55, .74) | .77 |
| F(6, 662) = 5.58, p <.001 | F(6, 662) = 2.38, p = .03 | F(6, 662) = 2.02, p = .06 | F(6, 662) = 6.50, p <.001 | F(6, 662) = 8.60, p <.001 | ||||||
| R2 = .06 | R2 = .02 | R2 = .02 | R2 = .06 | R2 = .07 | ||||||
Children living in higher SES families reported better parenting (B = .06 [95 % CI .02, .10], p = .01), more family unity (B = .06 [.01, .10], p = .02), and fewer daily hardships (B = −.46 [−.69, −.23], p <.001). Older children also reported worse parenting (B = −.03 [−.05, −.02], p <.001), receiving more psychological aggression (B = .02 [.002, .04], p = .03) but less physical punishment (B = −.02 [−.04, −.01], p = .006) from their caregivers, less family unity (B = −.03 [−.05, −.01], p = .01), and more daily hardships (B = .29 [.18, .39], p <.001) than younger children.
HIV and Foster-Family Status Predicting Children’s Mental Health Outcomes
Results of linear regression analyses assessing how family factors impact the predictive value of living in a foster family and HIV status on child mental health are presented in Table 3. Model 1 examined the predictive value of HIV-status and living in a foster family, controlling for age, sex, and SES. Model 2 added parenting, psychological aggression, physical punishment, and daily hardships as predictors. Family unity was not included as a predictor because it was highly correlated with parenting, and parenting was more highly correlated with mental health outcomes and was therefore retained as a predictor.
Table 3.
Predictors of child mental health outcomes
| Variable | Depression
|
Anxiety
|
||||||
|---|---|---|---|---|---|---|---|---|
| Model 1
|
Model 2
|
Model 1
|
Model 2
|
|||||
| Coeff. (95 % CI) | p | Coeff. (95 % CI) | p | Coeff. (95 % CI) | p | Coeff. (95 % CI) | p | |
| Sex | 1.73 (−1.01, 4.47) | .22 | 1.22 (−1.22, 3.67) | .33 | .09 (.02, .16) | .01 | .08 (.02, .14) | .01 |
| Age | 1.12 (.50, 1.75) | <.001 | .54 (−.04, 1.12) | .07 | .05 (.03, .07) | <.001 | .03 (.02, .05) | <.001 |
| SES | −2.78 (−4.16, −1.41) | <.001 | −1.54 (−2.78, −.29) | .02 | −.04 (−.08, −.01) | .01 | −.01 (−.04, .02) | .57 |
| HIV-positive | 1.13 (−2.42, 4.68) | .53 | .53 (−2.65, 3.71) | .74 | .02 (−.07, .10) | .72 | .01 (−.07, .08) | .90 |
| HIV-affected | 5.26 (1.95, 8.56) | .002 | 3.05 (.07, 6.02) | .045 | .10 (.02, .18) | .02 | .04 (−.03, .11) | .28 |
| Foster family | 4.51 (.66, 8.36) | .02 | 2.41 (−1.06, 5.89) | .17 | .14 (.05, .24) | .003 | .08 (−.002, .16) | .06 |
| Positive parenting | – | −8.95 (−11.55, −6.34) | <.001 | – | −.27 (−.33, −.21) | <.001 | ||
| Psychological aggression | – | .35 (−2.59, 3.28) | .82 | – | .03 (−.04, .10) | .47 | ||
| Physical punishment | – | 4.62 (1.81, 7.44) | .001 | – | .07 (−.00, .13) | .05 | ||
| Hardships | – | 1.32 (.87, 1.77) | <.001 | – | .03 (.02, .04) | <.001 | ||
| F(6, 662) = 7.26, p <.001 | F(10, 657) = 23.09, p <.001 | F(6, 662) = 11.47, p <.001 | F(10,657) = 31.72, p <.001 | |||||
| R2 = .06 | R2 = .26 | R2 = .09 | R2 = .33 | |||||
|
| ||||||||
| Variable | Conduct problems
|
Irritability
|
||||||
| Model 1
|
Model 2
|
Model 1
|
Model 2
|
|||||
| Coeff. (95 % CI) | p | Coeff. (95 % CI) | p | Coeff. (95 % CI) | p | Coeff. (95 % CI) | p | |
|
| ||||||||
| Sex | −.06 (−.14, .02) | .16 | −.07 (−.15, −.00) | .049 | .10 (.02, .18) | .02 | .08 (.02, .15) | .02 |
| Age | .01 (−.01, .03) | .19 | −.01 (−.02, .01) | .51 | .05 (.03, .07) | <.001 | .03 (.01, .04) | .001 |
| SES | −.04 (−.08, .00) | .07 | −.01 (−.05, .03) | .64 | −.07 (−.11, −.03) | .001 | −.03 (−.06, .01) | .10 |
| HIV-positive | .08 (−.03, .19) | .14 | .07 (−.03, .17) | .16 | .01 (−.10, .12) | .84 | −.00 (−.09, .09) | .99 |
| HIV-affected | .12 (.02, .22) | .02 | .06 (−.03, .15) | .20 | .16 (.07, .26) | .001 | .09 (.01, .18) | .03 |
| Foster family | .03 (−.08, .15) | .58 | −.05 (−.16, .05) | .34 | .16 (.04, .27) | .01 | .07 (−.03, .17) | .17 |
| Positive parenting | – | −.34 (−.41, −.26) | <.001 | – | −.34 (−.41, −.26) | <.001 | ||
| Psychological aggression | – | .10 (.01, .19) | .03 | – | .12 (.04, .20) | .005 | ||
| Physical punishment | – | .02 (−.07, .10) | .71 | – | .07 (−.01, .15) | .09 | ||
| Hardships | – | .02 (.01, .03) | .01 | – | .04 (.03, .05) | <.001 | ||
| F(6, 662) = 2.34, p = .03 | F(10, 657) = 16.78, p <.001 | F(6, 662) = 10.30, p <.001 | F(10, 657) = 36.09, p <.001 | |||||
| R2 = .02 | R2 = .20 | R2 = .09 | R2 = .35 | |||||
Compared to HIV-unaffected children, HIV-affected children reported significantly more depression (B = 5.26 [95 % CI 1.95, 8.56], p = .002), anxiety (B = .10 [.02, .18], p = .02), irritability (B = .16 [.07, .26], p = .001), and conduct problems (B = .12 [.02, .22], p = .02), and continued to report more depression (B = 3.05 [.07, 6.02], p = .045) and irritability (B = .09 [.01, .18], p = .03) after accounting for family factors.
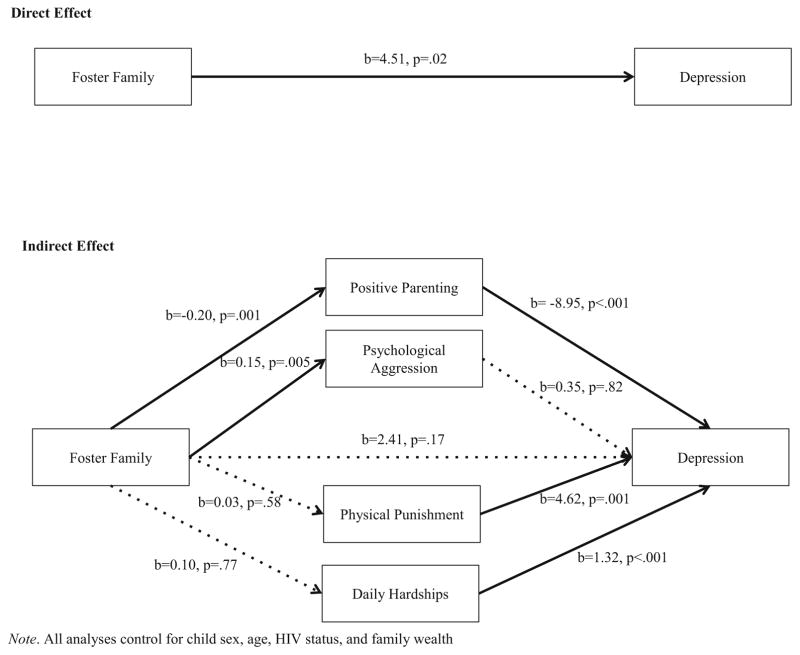
Children living in foster families reported more depression (B = 4.51 [.66, 8.36], p = .02), anxiety (B = .14 [.05, .24], p = .003), and irritability (B = .16 [.04, .27], p = .01) than children living with at least one biological parent. However, these differences were no longer significant after accounting for family factors.
Higher scores on the parenting measure and fewer daily hardships predicted lower levels of depression, anxiety, conduct problems and irritability. Harsh disciplinary practices were associated with poorer mental health outcomes; psychological aggression predicted more conduct problems (B = .10 [.01, .19], p = .03) and irritability (B = .12 [.04, .20], p = .005), while physical punishment predicted more depression (B = 4.62 [1.81, 7.44], p = .001) and anxiety (B = .07 [−.00, .13], p = .05).
Results of multiple mediation analyses to assess the significance of the indirect effect of living in a foster family on child mental health through parenting and family factors are presented in Table 4 and Fig. 2. Results indicated that parenting fully mediated the association between living in a foster family and child depression (B = 1.79 [95 % CI .50, 3.07], p = .007), anxiety (B = .05 [.02, .09], p = .005), irritability (B = .06 [.02, .11], p = .005) and conduct problems (B = .07 [02, .11], p = .004), meaning that children living in foster homes reported worse parenting and subsequently greater distress.
Table 4.
Family factors mediating the association between living in a foster family and child mental health
| Depression
|
Anxiety
|
Conduct problems
|
Irritability
|
|||||
|---|---|---|---|---|---|---|---|---|
| B (95 % CI) | p | B (95 % CI) | p | B (95 % CI) | p | B (95 % CI) | p | |
| Direct effect | ||||||||
| Foster family | 2.41 (−1.03, 5.85) | .17 | .08 (−.002, .16) | .06 | −.05 (−.16, .05) | .33 | .07 (−.03, .17) | .17 |
| Indirect effect | ||||||||
| Positive parenting | 1.79 (.50, 3.07) | .007 | .05 (.02, .09) | .005 | .07 (.02, .11) | .004 | .06 (.02, .11) | .005 |
| Psychological aggression | .05 (−.41, .51) | .82 | .003 (−.008, .02) | .51 | .01 (−.003, .03) | .10 | .02 (−.0002, .04) | .052 |
| Physical punishment | .13 (−.38, .65) | .60 | .002 (−.006, .01) | .64 | .0005 (−.005, .006) | .86 | .001 (−.007, .01) | .66 |
| Daily hardships | .13 (−.72, .97) | .77 | .003 (−.02, .02) | .77 | .002 (−.01, .01) | .79 | .004 (−.02, .03) | .77 |
| Total indirect effect | 2.10 (.20, 4.00) | .03 | .06 (.01, .11) | .02 | .08 (.03, .14) | .003 | .09 (.02, .16) | .007 |
All models control for sex, age, SES, and HIV-positive and HIV-affected status
Fig. 2.
Graphical depiction of mediation for depression
Note. All analyses control for child sex, age, HIV status, and family wealth
Discussion
Prior research has indicated increased vulnerability facing children affected by HIV or living with HIV [41–45], especially in resource-poor settings. However, while the research to date has given a great deal of attention to documenting the experiences and vulnerability of AIDS orphans [46, 47], there has been little fine-grained attention to questions of fostering and other family configurations that are common for supporting children affected by HIV in SSA. In this manner, the present study helps to advance insights into the situation of children—many affected by HIV—who are in fostering situations in Rwanda, and it points to important topics for future research in many resource-poor settings.
Of importance, our findings indicate that HIV-positive children are significantly more likely to live in foster homes compared to HIV-affected and unaffected children; however, living with HIV was not significantly predictive of greater symptoms of mental distress after accounting for foster family status. However, HIV-positive status remains an important contributor to greater symptoms of distress since children who are HIV-positive are much more likely to live in a foster family. HIV-affected children were not more likely to live in foster families. One potential explanation for the lower number of HIV-affected children in foster families is the lower number of reported caregiver deaths among HIV-affected (22.8 %) compared to HIV-positive (50.5 %) children; the HIV-affected sample in this study is predominantly children currently living with an HIV-positive caregiver. However being HIV-affected was significantly predictive of depression and irritability after accounting for other family and household factors.
In Rwanda, universal access to treatment and specialized services for HIV-positive children [3, 48] may be one explanation for better mental health outcomes in HIV-positive children compared to the elevated levels of mental health distress in HIV-affected children who often do not receive additional services. Without access to the same services as HIV-positive children, HIV-affected children may lack needed support to cope with a caregiver’s HIV. Further, the higher levels of mental health problems in HIV-affected children after accounting for living in a foster family and other parent and family factors highlights the vulnerability of these children which has been demonstrated in research among HIV-affected children in other settings [49, 50]. Providing family-focused parenting and mental health services linked to HIV care may be an important opportunity to promote mental health in children living with HIV themselves as well as children whose caregivers are living with HIV.
Results indicate that children living in foster homes are more likely to develop symptoms of depression, anxiety and irritability due to less positive and supportive parenting practices, which are important protective factors against mental health symptoms. These studies complement existing research highlighting the increased risk of distress and maltreatment among orphaned and abandoned children [11, 12, 16, 17]. By accounting for parenting practices, this study provides additional context as to the mechanisms by which orphaned children and children living in foster families in Rwanda may exhibit greater levels of mental health distress and requires further research, both quantitative and qualitative, in other settings in SSA [16]. Lower SES, larger family sizes, and greater daily hardships are additional negative factors that are associated with increased mental distress in the literature [6, 7, 51], but were not present in our sample of foster children. A higher SES associated with fostering children in this sample may contribute to protecting foster children from worse outcomes. These findings contribute to the ongoing discussion regarding foster homes in Rwanda, where national policy has called for de-institutionalization and reintegration of children back into extended families rather than housing them in institutions [52]. As the Rwandan government advances this policy of encouraging formal fostering instead of orphanages, further studies are needed to understand how to promote mental health, family functioning and supportive parenting of children in foster care during and after reintegration into families. Such analyses, with a focus on the mechanisms that may be in operation, can suggest supports and services that may help strengthen families that are expanding and adjusting to a fostering arrangement. Similar movements are underway across SSA and other low-resource settings making mixed methods research of this nature increasingly critical.
Limitations of this study must be noted. Logistically we were unable to collect biomarkers of HIV-status for the children recruited in the sample. However, due to the robust system of CHWs in Rwanda and additional support in the study districts by PIH/IMB which provides directly observed therapy to HIV-positive patients, we have confidence that our methods overall contributed to correct categorization of children by HIV-status for those who tested positive through the Rwandan health system. Also, any miscategorization, which is likely present, but rare given the strength of the HIV-testing and CHW system in Rwanda, would have occurred equally among the three groups. Given the focus on children’s outcomes, data related to caregiver HIV clinical outcomes, disclosure to children, and current illness were not collected which could have strengthened the analyses. However, we relied on the categorization of HIV-care service providers at the community level. Additionally, we did not gather information on when or why children entered a foster family or how they may have acquired HIV, which also could be an important factor in children’s wellbeing. Given the potential bias in reporting of biological parents compared to foster caregivers, we chose to rely on child self-reports of main outcomes. The strengths of this study include the use of validated measures of mental health, protective factors and family processes in Rwandan children and a sample allowing for comparisons across children affected and unaffected by HIV.
Conclusions
Our findings demonstrate that family support and positive parenting practices play important roles in shaping the mental health of children and can mitigate risks such as those observed among children living in a foster families. In our study, children living with HIV were much more likely to live in a foster family than their peers who were unaffected by HIV. Children who are in foster homes may be less likely to have the protective factors of family support and supportive parenting. Individual mental health interventions as well as family-based preventative interventions may be warranted to promote these protective factors and prevent child mental health symptoms [53]. Healthcare providers and social service programs should endeavor to provide such support to foster parents to ensure they are adequately empowered and supported to care for fostered children. In our study, we also observed that HIV-affected children also had higher levels of mental health distress compared to HIV-positive and HIV-unaffected children. Interventions that specifically target this population are warranted in Rwanda and such dynamics should be explored in other parts of SSA as well. Further, children in foster families and HIV-affected children should be connected to healthcare and social service providers and institutions to support their mental well-being. Theory and evidence-based interventions to support foster families that focus on empowering and developing positive parenting skills in foster parents and providing information on promoting children’s mental health in the context of adversity such as parental loss and parental HIV are advised. Providing family-focused parenting and mental health services in HIV clinics may also improve mental health outcomes of children living with, and affected by, HIV.
Acknowledgments
This work was made possible by the collaboration and dedication of the Rwandan Ministry of Health and Partners In Health/Inshuti Mu Buzima. We are endlessly grateful to the local research team who carried out these interviews and to the study participants and their families who shared their experiences with us. We also wish to express our deep gratitude to the Honorable Minister of Health, Dr. Agnes Binagwaho and Dr. Yvonne Kayiteshonga, Mental Health Division Manager at the Rwandan Biomedical Center. This study was funded by the Harvard University Center for AIDS Research (CFAR) Grant numbers P30 AI060354, 1K01MH07724601 A2, R34MH084679 03S1, and 5T32MH093310 from the National Institute of Mental Health, the François-Xavier Bagnoud Center for Health and Human Rights, the Peter C. Alderman Foundation, the Harvard Center for the Developing Child, the Harvard School of Public Health Career Incubator Fund, and the Julie Henry Family Development Fund. The funders had no role in study design, data collection, analysis or interpretation, manuscript writing, or the decision to publish.
Footnotes
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest Theresa S. Betancourt has received funding from Harvard University Center for AIDS Research (Grant number P30 AI060354) and the National Institutes of Mental Health (Grant numbers 1K01MH07724601 A2, R34MH084679 03S1), and Lauren C. Ng’s time was supported by NIMH Grant #5T32MH093310).
References
- 1.UNICEF. Children and AIDS: Fifth Stocktaking Report. New York: UNICEF, UNAIDS, World Health Organization, UNFPA, UNESCO; 2010. [Google Scholar]
- 2.UN High Commissioner for Refugees (UNHCR) UNHCR CDR Background Paper on Refugees and Asylum Seekers from Rwanda. Geneva: UNHCR; 1998. [Google Scholar]
- 3.Binagwaho A, Fuller A, Kerry V, et al. Adolescents and the right to health: eliminating age-related barriers to HIV/AIDS services in Rwanda. AIDS Care. 2012;24(7):936–42. doi: 10.1080/09540121.2011.648159. [DOI] [PubMed] [Google Scholar]
- 4.UNAIDS. HIV and AIDS estimates. 2014 Available from: http://www.unaids.org/en/regionscountries/countries/rwanda.
- 5.Ji G, Li L, Lin C, Sun S. The impact of HIV/AIDS on families and children—a study in China. AIDS. 2007;21(Suppl 8):S157–61. doi: 10.1097/01.aids.0000304712.87164.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monasch R, Boerma JT. Orphanhood and childcare patterns in sub-Saharan Africa: an analysis of national surveys from 40 countries. AIDS. 2004;18(Suppl 2):S55–65. doi: 10.1097/00002030-200406002-00007. [DOI] [PubMed] [Google Scholar]
- 7.Heymann J, Earle A, Rajaraman D, Miller C, Bogen K. Extended family caring for children orphaned by AIDS: balancing essential work and caregiving in a high HIV prevalence nations. AIDS Care. 2007;19(3):337–45. doi: 10.1080/09540120600763225. [DOI] [PubMed] [Google Scholar]
- 8.Wakhweya A, Dirks R, Yeboah K. Children thrive in families: family centered models of care and support for orphans and other vulnerable children affected by HIV and AIDS. Joint Learning Initiative on Children and HIV/AIDS. 2008 [Google Scholar]
- 9.Stover J, Bollinger L, Walker N, Monasch R. Resource needs to support orphans and vulnerable children in sub-Saharan Africa. Health Policy Plan. 2007;22:21–7. doi: 10.1093/heapol/czl033. [DOI] [PubMed] [Google Scholar]
- 10.Cluver L, Gardner F, Operario D. Poverty and psychological health among AIDS-orphaned children in Cape Town, South Africa. AIDS Care. 2009;21:732–41. doi: 10.1080/09540120802511885. [DOI] [PubMed] [Google Scholar]
- 11.Abebe T, Aase A. Children, AIDS and the politics of orphan care in Ethiopia: the extended family revisited. Soc Sci Med. 2007;64(10):2058–69. doi: 10.1016/j.socscimed.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Gray CL, Pence BW, Ostermann J, et al. Prevalence and incidence of traumatic experiences among orphans in institutional and family-based settings in 5 low- and middle-income countries: a longitudinal study. Glob Health Sci Pract. 2015;3(3):395–404. doi: 10.9745/GHSP-D-15-00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster G. The capacity of the extended family safety net for orphans in Africa. Psychol Health Med. 2000;5(1):55–62. [Google Scholar]
- 14.Bicego G, Rutstein S, Johnson K. Dimensions of the emerging orphan crisis in sub-Saharan Africa. Soc Sci Med. 2003;56(6):1235–47. doi: 10.1016/s0277-9536(02)00125-9. [DOI] [PubMed] [Google Scholar]
- 15.Ardington C, Leibbrandt M. Orphanhood and Schooling in South Africa: trends in the vulnerability of orphans between 1993 and 2005. Econ Dev Cult Change. 2010;58(3):503–36. doi: 10.1086/650414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cluver L, Gardner F. The mental health of children orphaned by AIDS: a review of international and southern African research. J Child Adolesc Mental Health. 2007;19(1):1–17. doi: 10.2989/17280580709486631. [DOI] [PubMed] [Google Scholar]
- 17.Onuoha FN, Munakata T, Serumaga-Zake PA, Nyonyintono RM, Bogere SM. Negative mental health factors in children orphaned by AIDS: natural mentoring as a palliative care. AIDS Behav. 2009;13(5):980–8. doi: 10.1007/s10461-008-9459-0. [DOI] [PubMed] [Google Scholar]
- 18.Betancourt T, Scorza P, Kanyanganzi F, et al. HIV and child mental health: a case-control study in Rwanda. Pediatrics. 2014;134(2):e464–72. doi: 10.1542/peds.2013-2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adna RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences: a convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2005;256:174–86. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schilling EA, Alseltine RH, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7(30):1–10. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jewkes RK, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HS2 incident infections in rural South African youth. Child Abuse Negl. 2010;34:833–41. doi: 10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shonkoff JP, Garner AS, Siegel BS, et al. the lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 23.Kaggwa EB, Hindin MJ. The psychological effect of orphanhood in a matured HIV epidemic: an analysis of young people in Mukono, Uganda. Soc Sci Med. 2010;70:1002–10. doi: 10.1016/j.socscimed.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Betancourt TS, Meyers-Ohki S, Stulac SN, et al. Nothing can defeat combined hands (Abashize hamwe ntakibananira): protective processes and resilience in Rwandan children and families affected by HIV/AIDS. Soc Sci Med. 2011;73(5):693–701. doi: 10.1016/j.socscimed.2011.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Betancourt TS, Rubin-Smith JE, Beardslee WR, et al. Understanding locally, culturally, and contextually relevant mental health problems among Rwandan children and adolescents affected by HIV/AIDS. AIDS Care. 2011;23(4):401–12. doi: 10.1080/09540121.2010.516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Betancourt T, Scorza P, Meyers-Ohki S, et al. Validating the center for epidemiological studies depression scale for children in Rwanda. J Am Acad Child Adolesc Psychiatry. 2012;51(12):1284–92. doi: 10.1016/j.jaac.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scorza P, Stevenson A, Canino G, et al. Validation of the “World Health Organization Disability Assessment Schedule for Children, WHODAS-Child” in Rwanda. PLoS One. 2013;8(3):e57725. doi: 10.1371/journal.pone.0057725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ng LC, Kanyanganzi F, Munyanah M, Mushashi C, Betancourt TS. Developing and validating the youth conduct problems scale-rwanda: a mixed methods approach. PLoS One. 2014;9(6):e100549. doi: 10.1371/journal.pone.0100549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Betancourt TS, Rubin-Smith J, Beardslee WR, et al. Understanding locally, culturally, and contextually relevant mental health problems among Rwandan children and adolescents affected by HIV/AIDS. AIDS Care. 2012;23(4):401–12. doi: 10.1080/09540121.2010.516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radloff LS. The use of the center for epidemiological studies depression scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149–66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan DV, Shytle D, Milo K, Janavs J, Lecrubier Y. MINI International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) J Clin Psychiatry. 2010;71(3):313–26. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 32.Achenbach TM. Manual for the Youth Self-Report and 1991 profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 33.Craig KJ, Hietanan H, Markova IS, Berrios GE. The Irritability Questionnaire: a new scale for the measurement of irritability. Psychiatr Res. 2008;159:367–75. doi: 10.1016/j.psychres.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Rohner RP. Parental Acceptance-Rejection Questionnaire (PARQ) Test Manual. In: Rohner RP, Khaleque A, editors. Handbook for the study of parental acceptance and rejection. Vol. 4. Sorrs: Rohner Research Publications; 2005. pp. 43–105. [Google Scholar]
- 35.UNICEF. Multiple Indicator Cluster Surveys - Round 4. New York, NY: UNICEF; 2009. Available from: http://www.childinfo.org/mics4_background.html. [Google Scholar]
- 36.Layne CM, Stuvland R, Saltzman W, Djapo N, Pynoos RS. Adolescent Post War Adversities Scale. Unpublished instrument. 1999 [Google Scholar]
- 37.Rutstein SO, Johnson K. The DHS Wealth Index. Calverton: ORC Macro; 2004. [Google Scholar]
- 38.Bolton P. Cross-cultural validity and reliability testing of a standard psychiatric assessment instrument without a gold standard. J Nerv Mental Dis. 2001;189(4):238–42. doi: 10.1097/00005053-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 40.StataCorp. Stata Statistical Software: Release 120. College Station: StataCorp LP; 2011. [Google Scholar]
- 41.Betancourt TS, Meyers-Ohki SE, Charrow A, Hansen N. Annual Research Review: mental health and resilience in HIV/AIDS-affected children—a review of the literature and recommendations for future research. J Child Psychol Psychiatry. 2013;54(4):423–44. doi: 10.1111/j.1469-7610.2012.02613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. J Child Psychol Psychiatry. 2012;53(4):363–70. doi: 10.1111/j.1469-7610.2011.02459.x. [DOI] [PubMed] [Google Scholar]
- 43.Cluver L, Orkin M. Cumulative risk and AIDS-orphanhood: interactions of stigma, bullying and poverty on child mental health in South Africa. Soc Sci Med. 2009;69(8):1186–93. doi: 10.1016/j.socscimed.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 44.Heymann J, Earle A, Rajaraman D, Miller C, Bogen K. Extended family caring for children orphaned by AIDS: balancing essential work and caregiving in a high HIV prevalence nations. AIDS Care. 2007;19:337–45. doi: 10.1080/09540120600763225. [DOI] [PubMed] [Google Scholar]
- 45.Whetten K, Whetten RA, Ostermann J, Itemba D. Trauma, anxiety and reported health among HIV-positive persons in Tanzania and the US Deep South. AIDS Care. 2008;20(10):1233–41. doi: 10.1080/09540120801918636. [DOI] [PubMed] [Google Scholar]
- 46.Ssewamala FM, Nabunya P, Ilic V, Mukasa MN, Ddamulira C. Relationship between family economic resources, psychosocial well-being, and educational preferences of AIDS-orphaned children in Southern Uganda: baseline findings. Glob Soc Welfare. 2015;2(2):75–86. doi: 10.1007/s40609-015-0027-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Block E. Flexible kinship: caring for AIDS orphans in rural Lesotho. J R Anthropol Inst. 2014;20(4):711–27. doi: 10.1111/1467-9655.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Merkel E, Gupta N, Nyirimana A, et al. Clinical outcomes among HIV-positive adolescents attending an integrated and comprehensive adolescent-focused HIV Care Program in Rural Rwanda. J HIV AIDS Soc Serv. 2013;12(3–4):437–50. [Google Scholar]
- 49.Doku P. Parental HIV/AIDS status and death, and children’s psychological wellbeing. Int J Mental Health Syst. 2009;3(1):26. doi: 10.1186/1752-4458-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lester P, Rotheram-Borus MJ, Lee SJ, et al. Rates and predictors of anxiety and depressive disorders in adolescents of parents with HIV. Vulnerable Child Youth Stud. 2006;1(1):81–101. [Google Scholar]
- 51.Foster G, Williamson J. A review of current literature of the impact of HIV/AIDS on children in sub-Saharan Africa. AIDS. 2000;14(suppl 3):S275–84. [PubMed] [Google Scholar]
- 52.Ministry of Gender and Family Promotion. Strategy for National Child Care Reform. Kigali: Government of Rwanda; 2010. [Google Scholar]
- 53.Betancourt TS, Ng L, Kirk CM, et al. Family-based prevention of mental health problems in children affected by HIV and AIDS: an open trial. AIDS. 2014;28(Suppl 3):S359–68. doi: 10.1097/QAD.0000000000000336. [DOI] [PMC free article] [PubMed] [Google Scholar]