Abstract
Purpose
Unicompartmental knee arthroplasty (UKA) can be a surgical treatment option for patients with high expectations regarding the post-operative level of physical activity. A systematic review was undertaken to answer three research questions: (1) is there an improvement of physical activity based on validated activity scores following UKA? (2) What are the sport disciplines and the sport patterns of UKA patients? (3) What are the pre- and post-operative sport participation rates and the return to activity rates of UKA patients?
Methods
Following the PRISMA guidelines, EMBASE, MEDLINE, ISI Web of Science and the Cochrane Central Register of Controlled Trials were searched for studies reporting the level of sport and/or physical activity before and after UKA, and/or included at least one activity score before and after UKA.
Results
Seventeen studies were identified reporting on 2972 UKAs, of which 89 % were medial UKAs and 92 % were mobile-bearing implants, respectively. Ten studies reported a statistically significant improvement of physical activity following UKA according to the UCLA activity score, the Tegner activity score or the High Activity Arthroplasty Score, respectively. Hiking, cycling and swimming are the most common activities following UKA. Sport participation before the onset of restricting symptoms ranged from 64 to 93 % and slightly decreased by 2–9 % following UKA. The return to activity rate ranged from 87 to 98 %.
Conclusion
Patients following UKA are physically active according to validated activity scores. A significant increase in low-impact activities and a decrease in high-impact activities after UKA was observed. Patients with a UKA regularly participate in sports; however, sport participation slightly decreased compared to pre-arthritic levels. This systematic review helps physicians to manage the expectations of patients regarding the level of physical activity following UKA.
Level of evidence
III.
Keywords: Unicompartmental knee arthroplasty, Sport, Physical activity, Review
Introduction
Knee osteoarthritis (OA) is a frequent cause of pain and disability in the elderly [6, 9, 39]. Epidemiologic studies suggest that almost half of the general US population may develop symptomatic knee OA by the age of 85 years, with a particularly high risk in the obese [23]. The demand for primary knee arthroplasties is, therefore, projected to grow by more than 600 % by 2030 [20].
Unicompartmental knee arthroplasty (UKA) is an effective and safe treatment option for isolated end-stage medial or lateral compartment knee OA [5, 28]. Kozinn and Scott [19] proposed indications and contraindications for fixed-bearing UKAs. The authors postulated that damage to the patellofemoral joint, obesity, youth and high activity levels should be considered a contraindication for a UKA. However, for mobile-bearing implants most of these contraindications may be neglected. The Oxford group [24] proposed to consider an Oxford UKA in all knees with bone-on-bone arthritis [11], full-thickness cartilage in the contralateral compartment [11], a fully correctible intra-articular deformity [42] and an intact anterior cruciate ligament [43, 48]. Patellofemoral arthritis is no contraindication unless deep eburnation, bone loss or patellar subluxation is observed [24]. These criteria are satisfied in a significant proportion of knees requiring arthroplasty. For fixed-bearing UKAs, the indications are less defined. Deschamps and Chol [7] suggested that for modern fixed-bearing implants, indications are slightly stricter than for mobile-bearing implants with anterior knee pain and a body mass index above 30 kg/m2 being a (relative) contraindication.
For both UKA design concepts, excellent clinical results and improved survivorship have been reported [16, 27, 31, 40, 41, 46]. Consequently, UKAs are increasingly being used in younger and more active patients [2, 3]. This particular patient cohort, however, has high expectations concerning the post-operative level of physical activity [4, 8].
Conventional outcome scores such as the American Knee Society Score [17] assess objective parameters and what a patient is capable of doing. However, these rating scales do not take into account what a patient is actually doing [51]. In times of high post-operative expectations, activity rating scales are becoming a key factor to assess the outcome of a procedure. There has been no review analysing all available studies with regard to pre- and post-operative activity scores following UKA. Therefore, the present study undertook a systematic review analysing the level of sport and physical activity following UKA. The following research questions were asked: (1) is there an improvement of physical activity based on validated activity scores following UKA? (2) What are the sport disciplines and the sport patterns of UKA patients? (3) What are the pre- and post-operative sport participation rates and the return to activity rates of UKA patients?
Materials and methods
EMBASE, MEDLINE and the ISI Web of Science for randomized controlled trials, quasi-randomized trials and controlled clinical trials as well as case series investigating the clinical outcome of UKAs with regard to physical activity and sport were searched. The inclusion criteria were defined as follows: studies reporting on the level of physical activity or sport before and after UKA using an activity score or an activity questionnaire. A combination of Medical Subject Headings (MESH) terms and free text was used to search for relevant studies. Studies in English or German language were identified (“Appendix”).
Two authors (P.K. and W.W.) reviewed all abstracts. The full text was analysed for studies meeting the inclusion criteria. The systematic review was conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [22]. The methodological index for non-randomized studies (MINORS) was used to assess the quality of all studies [34] (Table 1).
Table 1.
Patient demographics and studies details extracted from studies included in the review (n = 17)
| Patient demographics and study details | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| References | Journal | No. of patients (knees) | Gender (per cent males) | Mean age (years) | Study type (prospective/retrospective) | Mean follow-up (months) | MINORS | Medial/lateral UKA | Type of bearing | Type of prosthesis | Type of fixation |
| Schai et al. [33] | JOA | 28 (28) | 39.2 | 52 (range 37–60) | Retrospective | 40 (range 24–72) | 9/16 | n = 25 medial, n = 3 lateral | Fixed | PFC unicompartmental knee system (Johnson & Johnson, Raynham, MA, USA) | Cemented |
| Fisher et al. [10] | The Knee | 66 (71) | 48.5 | 64 (range 49–81) | Prospective | 18 (range 4–46) | 11/16 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | Cemented |
| Walton et al. [46] | J Knee Surg. | 150 (183) | 50.7 | 71.5 (range 36–92) | Retrospective | Minimum 12 | 11/24 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | cemented |
| Naal et al. [25] | AMJSM | 83 (83) | 54.2 | 65.5 (range 47–83) | Retrospective | 18 (range 12–28) | 10/16 |
n = 77 medial n = 6 lateral |
Fixed | Preservation prosthesis (DePuy International Ltd, Leeds, UK) | Tibia cemented; femoral component not specified |
| Hopper and Leach [16] | KSSTA | 34 (41) | 58.8 | 61.3 (range 43–75) | Retrospective | 22.3 (range 12–44) | 13/24 | Not specified | not specified | Oxford (Zimmer Biomet, Bridgend, UK) | Not specified |
| Naal et al. [26] | AOTS | 77 (83) | 55.8 | 66 (range 46–84) | Retrospective | Minimum 24 | 10/16 | Medial | Fixed | Preservation prosthesis (DePuy International Ltd, Leeds, UK) | Not specified |
| Pandit et al. [28, 29] | BJJ/JBJS Br | 818 (1000) | 48 | 66 (range 32–88) | Prospective | Minimum 12 | 11/16 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | Cemented |
| Yim et al. [50] | JOA | 50 (50) | 4 | 60.3 (range 47–65) | Retrospective | 44 (rage 36–48) | 20/24 | Medial | Fixed | Miller-Galante (Zimmer, Warsaw, IN, USA) | Cemented |
| Liddle et al. [21] | KSSTA | 380 (406) | 55 | 64.8 (range 35–87) | Prospective | Minimum 12 | 14/16 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | Not specified |
| Pandit et al. [30] | JBJS | 62 (63) | 63: cemented 53: cementless |
63.8 (range 46–78) Cemented 64.7 (45–82) Cementless |
Prospective | Minimum 60 | 23/24 | Medial | Mobile | Oxford phase 3 Unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) |
n = 33 cemented n = 30 cementless |
| Pietschmann et al. [32] | Int. Orthop. | 171 (181) | 44 | 65.3 (range 44–90) | Retrospective | 50.4 (range 12–120) | 7/16 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | Cemented |
| Jahnke et al. [18] | Int. Orthop. | 159 (178) | 52.8 | 63.5 (range 36–86) | Prospective | 24 (range 1.47) | 8/16 | Medial | Mobile | Oxford (Zimmer Biomet, Bridgend, UK) | Not specified |
| Weston-Simons et al. [47] | BJJ | 258 (265) | 35.2 | 63.6 (range 32–90) | Prospective | 49.2 (range 6–99.6) | 14/16 | Lateral | Mobile | Oxford phase 3 domed unicompartmental knee prothesis (Zimmer Biomet, Bridgend, UK) | Cemented |
| Walker et al. [44] | KSSTA | 45 (45) | 42.2 | 60.1 (range 36–81) | Retrospective | 35.4 (range 24–51) | 11/16 | Lateral | Mobile | Oxford (Zimmer Biomet, Bridgend, UK) | Cemented |
| Walker et al. [45] | JOA | 93 (109) | 49.4 | 55 (range 26–60) | Prospective | 52.8 (range 27.6–100.8) | 10/16 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | Cemented |
| Hooper et al. [15] | BJJ | 126 (150) | 53.1 | 63.6 (range 39–86) | Prospective | Minimum 60 | 11/16 | Medial | Mobile | Oxford phase 3 unicompartmental knee prosthesis (Zimmer Biomet, Bridgend, UK) | Uncemented |
| Ho et al. [14] | J Knee Surg. | 36 (36) | 33 | 60.0 (range 53–64) | Retrospective | 45.6 (range 24–68.4) | 15/24 | Medial | Not specified | Not specified | Not specified |
The methodological quality of each study was evaluated using the methodological index for non-randomized studies (MINORS)
JOA Journal of Arthroplasty; AMJSM American Journal of Sports Medicine; KSSTA Knee Surgery, Sports Traumatology, Arthroscopy; AOTS Archives of Orthopaedic and Trauma Surgery; BJJ Bone and Joint Journal; JBJS Journal of Bone and Joint Surgery; J Knee Surg. Journal of Knee Surgery
Data were extracted using a standardized form, including patient demographics follow-up period, type of implant, and scores or questionnaires assessing pre- and post-operative activity levels. The same activity score had to be performed pre-operatively and at least one time post-operatively. There were no restrictions regarding type of score used. Duplicate articles and studies not reporting on the same pre- and post-operative scores were excluded. Additional information regarding physical activity or sport before and after UKA was documented, and used for further interpretation of the results.
Statistical analysis
Descriptive statistics for the included studies were presented.
Results
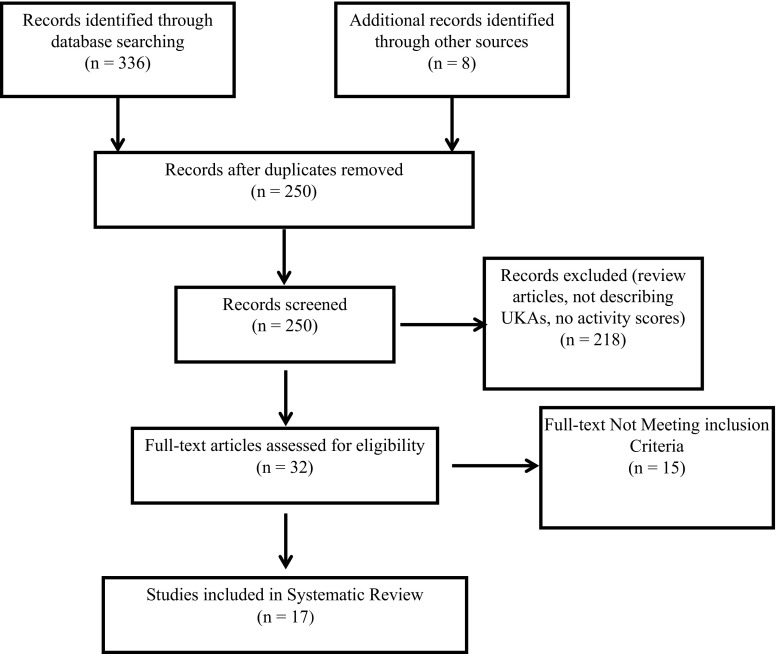
Three hundred and thirty-six studies were identified in the search. Additional eight studies were identified through cross-referencing. After exclusion of duplicates, a total of 250 papers were screened for applicability (Fig. 1). One study by Streit et al. [37] in 2012 reported on the same cohort as Walker et al. [44] in 2015; the study of Streit et al. [37] was therefore excluded from this review. Another study by Streit et al. [36] was not considered as it analysed the same cohort as Walker et al. [45]. Ultimately, 17 studies were included in the final analysis. These 17 studies reported on 2972 UKAs in 2636 patients. The patients’ age ranged from 25 to 92 years (Table 1). The majority of cases (89 %, 2653 of 2972) were medial UKAs; 11 % (319 of 2972) were lateral UKAs. One study analysing 41 UKAs did not specify whether a medial or lateral UKA was performed [16]. The mean MINORS score was of 11/16 points for single-arm studies (n = 12) and 16/24 points for comparative studies (n = 5) (Table 2).
Fig. 1.
Flow chart of study protocol following the PRISMA guidelines. The systematic review included 17 studies
Table 2.
Methodological index for non-randomized studies (MINORS)
| References | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | TOT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schai et al. [33] | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | – | – | – | – | 9/16 |
| Fisher et al. [10] | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 0 | – | – | – | – | 11/16 |
| Walton et al. [46] | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 2 | 1 | 11/24 |
| Naal et al. [25] | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | – | – | – | – | 10/16 |
| Hopper and Leach [16] | 2 | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 13/24 |
| Naal et al. [26] | 2 | 2 | 1 | 2 | 0 | 1 | 2 | 0 | – | – | – | – | 10/16 |
| Pandit et al. [28, 29] | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 0 | – | – | – | – | 11/16 |
| Yim et al. [50] | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 20/24 |
| Liddle et al. [21] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | – | – | – | – | 14/16 |
| Pandit et al. [30] | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 23/24 |
| Pietschmann et al. [32] | 1 | 2 | 1 | 1 | 0 | 2 | 0 | 0 | – | – | – | – | 7/16 |
| Jahnke et al. [18] | 2 | 0 | 2 | 2 | 0 | 1 | 1 | 0 | – | – | – | – | 8/16 |
| Weston-Simons et al. [47] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | – | – | – | – | 14/16 |
| Walker et al. [44] | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | – | – | – | – | 11/16 |
| Walker et al. [45] | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | – | – | – | – | 10/16 |
| Hooper et al. [15] | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 0 | – | – | – | – | 11/16 |
| Ho et al. [14] | 2 | 0 | 1 | 2 | 0 | 2 | 1 | 0 | 1 | 2 | 2 | 2 | 15/24 |
The methodological index for non-randomized studies (MINORS) applied to all studies assessing the level physical activity before and after implantation of a unicompartmental knee arthroplasty. The items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate)
Activity scores
Thirteen of seventeen studies used validated activity scores to evaluate the pre- and post-operative level of physical activity. Ten of these studies reported a statistically significant improvement following UKA according to the UCLA activity score [51], the Tegner activity score [38] or the High Activity Arthroplasty Score [1, 10, 15, 18, 21, 26, 30, 44, 45, 47] (Table 3).
Table 3.
Overview of pre- and post-operative activity scores and sport questionnaires of all studies analysed
| Activity scores and sport questionnaires | ||||||
|---|---|---|---|---|---|---|
| References | Journal | Outcome score(s) | Pre-operative assessment (time) | Pre-operative values | Post-operative values | Significance |
| Schai et al. [33] | JOA | Tegner | Before surgery | 2.3 | 2.7 | Not calculated |
| Fisher et al. [10] | The Knee | UCLA | Before surgery | 4.2 (range 3–6) | 6.5 (range 3–9) | p < 0.01 |
| Walton et al. [46] | J Knee Surg. | Simple sport questionnaire (no. of disciplines) | Before surgery | N/A | N/A | Not calculated |
| Naal et al. [25] | AMJSM | Sport questionnaire (no. of disciplines/frequency/session length) | Before onset of restricting symptoms | 5/2.9/66 min | 3.1/2.8/55 min | p < 0.01/0.329/0.08 |
| Hopper and Leach [16] | KSSTA | Sport questionnaire (no. of disciplines/frequency per week/minimum session length) | Before surgery | 1.5/3.2/85 min | 1.4/3.4/92.1 min | p = 0.083/p = 0.727/p = 0.487 |
| Naal et al. [26] | AOTS | UCLA | Before surgery | 4.7 ± 2.4 | 7.1 ± 1.9 | p < 0.01 |
| Pandit et al. [28, 29] | BJJ/JBJS Br | Tegner | Before surgery | 2.3 ± 1.1 | 1 year follow-up: 2.9 ± 0.9 10 years follow-up: 2 ± 0.8 |
Not calculated |
| Yim et al. [50] | JOA | Tegner, sport questionnaire (no. of disciplines) | Before surgery | 3.2 ± 0.9 2.2 ± 1.6 |
2.6 ± 0.9 1.6 ± 1.7 |
Not calculated |
| Liddle et al. [21] | KSSTA | Tegner | Before surgery | 2.0 (1–5) | 3.0 (1–6) | p < 0.01 |
| Pandit et al. [30] | JBJS | Tegner | Before surgery | Cemented: 1.9 ± 0.8 Cementless: 1.9 ± 0.7 |
2.6 ± 0.8 2.9 ± 0.6 |
p < 0.05 p < 0.05 |
| Pietschmann et al. [32] | Int. Orthop. | Sport questionnaire (no. of disciplines/frequency per week/minimum session length) | Before surgery | 1.73/–/– | 1.74/–/– | Not calculated |
| Jahnke et al. [18] | Int. Orthop. | UCLA, Tegner, Heidelberg Sports Activity Score | Before surgery | 6.2 ± 1.3 4.1 ± 1.4 23.8 ± 18.5 |
6.3 ± 1.1 4.0 ± 1.0 29.3 ± 18.5 |
p < 0.01 p = 0.27 p < 0.01 |
| Weston-Simons et al. [17] | BJJ | Tegner | Before surgery | 2.2 ± 1.2 | 2.9 ± 1.2 | p < 0.01 |
| Walker et al. [44] | KSSTA | UCLA, Tegner, Schulthess Clinic Activity Score | Before surgery Before surgery Before onset of restricting symptoms |
5.3 ± 2.3 2.9 ± 1.6 N/A |
6.7 ± 1.5 3.5 ± 0.8 N/A |
p < 0.01 p < 0.01 N/A |
| Walker et al. [45] | JOA | UCLA, Tegner, Schulthess Clinic Activity Score | Before surgery Before surgery Before onset of restricting symptoms |
3.3 ± 1.5 2.0 ± 1.1 N/A |
6.8 ± 1.5 3.8 ± 1.1 N/A |
p < 0.001 p < 0.001 N/A |
| Hooper et al. [15] | BJJ | High Activity Arthroplasty Score | Before surgery | 4.33 ± 2.5 | 10.55 ± 1.93 | p < 0.001 |
| Ho et al. [14] | J Knee Surg. | UCLA | Before onset of restricting symptoms | 8.1 ± 1.5 | 7.4 ± 1.6 | Not calculated |
JOA Journal of Arthroplasty; AMJSM American Journal of Sports Medicine; KSSTA Knee Surgery, Sports Traumatology, Arthroscopy; AOTS Archives of Orthopaedic and Trauma Surgery; BJJ Bone and Joint Journal; JBJS Journal of Bone and Joint Surgery; J Knee Surg. Journal of Knee Surgery
Five studies described the UCLA activity score directly before surgery, and all these studies were able to demonstrate a significant improvement after UKA implantation [10, 18, 26, 44, 45]. Only one study assessed the UCLA activity score before the onset of knee symptoms [14]. In comparison with pre-arthritic activity levels, the UCLA activity score slightly decreased from 8.1 to 7.4 points following UKA. Despite the slight decrease in activity levels, patients still had the highest UCLA activity score of all studies analysed [14] (Table 3).
Overall, nine studies used the Tegner activity score to describe the pre- and post-operative level of physical activity. Five studies reported a statistically significant improvement following UKA [21, 30, 44, 45, 47]. The remaining four studies did either show no statistical difference [18] or did not calculate a significance level, respectively [29, 33, 50]. Jahnke et al. [18] described no statistically significant difference (n.s.) in the Tegner activity score comparing pre- and post-operative levels. The mean pre-operative Tegner activity score in Jahnkes’ study was considerably higher (4.1) compared to the remaining studies using this score (Table 3). Patient demographics did not differ compared to the other studies. The reason for the high pre-operative Tegner score, therefore, cannot be explained. Schai et al. [33] reported a relative improvement from 2.3 to 2.7 points according to the Tegner activity score, without calculating a significance level. Pandit et al. [29] also described the Tegner activity score in their study of 1000 consecutive Oxford UKAs with a minimum follow-up of 10 years. There was an improvement of the pre-operative Tegner activity score up to 7 years post-operatively; however, the score decreased below pre-operative levels at 10 years. Pandit et al. [29] did not calculate any significance level. Only Yim et al. [50] described a decrease in the Tegner activity score following UKA. However, a significance level was not calculated. Yim et al. [50] described a cohort of 96 % (48 of 50) female patients (Table 3).
In a recent study on 150 consecutive cementless UKAs, Hooper et al. [15] were able to demonstrate a significant improvement according to the High Activity Arthroplasty Score following UKA (Table 3).
Sport disciplines, length and frequency
Seven out of 17 studies described the level of physical activity in more detail, using either standardized [18, 44, 45] or non-standardized questionnaires [10, 25, 32, 50].
Using the Heidelberg Sports Activity Score, Jahnke et al. [18] reported that hiking, cycling and swimming were the three most practiced sports after surgery. Swimming, hiking and ‘other sports’ increased significantly. High-impact sports such as skiing, cross-country skiing and ball sports decreased significantly compared to pre-operatively practiced sports. Walker et al. [44] showed that biking, hiking and long walks were the most common activities after surgery according to the Schulthess Clinic Activity Score. Similar to Jahnke et al., a significant decrease in more intense activities such as tennis, soccer, jogging or skiing was observed after UKA implantation. In a further analysis of patients younger than 60 years, Walker et al. [45] reported a significant decrease in high-impact activities and a significant increase in low-impact activities after surgery, respectively.
Five studies reported physical activities based on individually developed scores. Naal et al. [25] described the physical activity using an individual score which recorded the number of activities, its frequency and the session length. The authors report an unchanged activity frequency after surgery with similar session length and a slight, although significant, decrease in the number of different sport disciplines (Table 3). The most common activities after surgery were hiking, cycling and swimming. Hopper et al. [16] analysed the participation in the following disciplines: golf, swimming, dancing (line/ballroom), bowls and cycling. The authors showed that the number of activities, its frequency and the session length remained unchanged with a UKA (Table 3). Yim et al. [50] assessed the participation in cycling, swimming, exercise walking, dancing, jogging and mountain climbing, and described a return to 1.6 activities after surgery compared to 2.2 activities before surgery, respectively. Fisher et al. [10] showed that most patients (93 %) following UKA resumed the same physical activity they performed before becoming symptomatic with knee pain. The top three activities were swimming, golf and dancing in Fishers’ study. Pietschmann et al. [32] described the percentage of patients who performed sports activities before (60 %) and after (53 %) surgery. The authors, furthermore, reported on an increase in the weekly sport frequency after UKA and a shift from high-impact sports towards low-impact sports, respectively.
Sport participation and return to activity
The pre-operative and post-operative sport participation was described in ten studies [10, 14, 16, 18, 25, 32, 44–46, 50]. The sport participation before the onset of restricting symptoms of the knee was reported in five studies, and ranged from 64 to 93 %, respectively [10, 14, 25, 44, 45]. In all five studies, patients stayed active; however, sport participation decreased up to 9 % compared to pre-arthritic conditions (Table 4). Seven studies described the return to activity rate which ranged from 80 to 98 % [10, 14, 16, 25, 32, 44, 45] (Table 4).
Table 4.
Summary of the reported pre- and post-operative sport participation rate and the return to activity rate of all studies analysed
| Pre-operative and post-operative sport participation | ||||
|---|---|---|---|---|
| References | Time of pre-operative assessment | Pre-operative sport participation | Post-operative sport participation | Return to activity rate |
| Fisher et al. [10] | Before onset of knee pain | 64 % (42 of 66) | 59 % (39 of 66) | 93 % |
| Walton et al. [46] | Directly before surgery | 79 % (121 of 150) | 86 % (131 of 131) | Not described |
| Naal et al. [25] | Before onset of knee pain | 93 % (77 of 83) | 88 % (73 of 83) | 95 % |
| Hopper and Leach [16] | Directly before surgery | 88 % (30 of 34) | 85 % (29 of 34) | 97 % |
| Yim et al. [50] | Directly before surgery | 84 % (42 of 50) | 60 % (30 of 50) | Not described |
| Pietschmann et al. [32] | Directly before surgery | 60 % (78 of 131) | 53 % (69 of 131) | 80 % |
| Jahnke et al. (2014) | Directly before surgery | 90 % | 93 % | Not described |
| Walker et al. [44] | Before onset of knee pain | 93 % (42 of 45) | 91 % (43 of 45) | 98 % |
| Walker et al. [45] | Before onset of knee pain | 93 % (86 of 93) | 91 % (85 of 93) | 93 % |
| Ho et al. [14] | Before onset of knee pain | 83 % (30 of 36) | 72 % (26 of 36) | 87 % |
Patients with a unicompartmental knee arthroplasty participate regularly in sports
Discussion
The most important findings of the present study were that the level of physical activity improves following UKA implantation according to established activity scores. A shift from high-impact to low-impact activities was observed. The number of different sport activities decreased, whereas the session length und frequency remained overall unchanged.
The UCLA activity score is validated activity assessment tool for patients with joint arthroplasties of the lower extremities [1, 51]. The present review demonstrates that in all but one study (n = 5) the UCLA activity score significantly improved following UKA implantation. The mean post-operative UCLA activity score ranged from 6.3 to 7.4 points. An UCLA activity score of 7 corresponds with the regular participation in active events such as bicycling. One study assessing the UCLA activity score before the onset of first restricting symptoms reported a slight decrease in the activity level compared to pre-arthritic conditions [14]. The study, however, still demonstrated the highest UCLA activity score of all studies analysed [14]. Overall, patients following UKA remain active according to the UCLA activity score.
The Tegner activity rating system was initially developed to evaluate activity after knee ligament injuries [38]. The Tegner and the UCLA activity scores both have a scale of 1–10 points. The Tegner score, however, is usually used for more active patient populations like ACL reconstruction patients. A Tegner score of 10, for instance, corresponds with competitive sports such as soccer on a national or international level. The mean post-operative Tegner activity score of all studies analysed in this review was 3.1 points which corresponds with competitive and recreational sports such as swimming. The fact that in some studies the Tegner score did not show statistically significant improvements following surgery is partly explained by the larger bandwidth of activities described in the Tegner activity score. The practiced activities have the change a lot to move from a Tegner activity score of 3 to a score of 4, while an improvement from level 3 to level 4 is easy on UCLA activity rating scale, respectively.
Eight out of 17 studies described the level of physical activity in more detail. All studies, irrespective of the questionnaire utilized, showed a significant decrease in high-impact activities and a significant increase in low-impact activities. The most popular activities after surgery were hiking, cycling and swimming. Almost all activities were in line with recommendations for the return to recreational and athletic activity after TKA presented by the Knee Society [12]. Naal et al. [25] reported on an active Swiss patient population of which 22 % performed downhill skiing following surgery. The Knee Society has not come to a conclusion whether downhill skiing should be recommended [13].
Although patients took up lower-impact activities, its frequency per week and the minimum session length even increased [16] or remained unchanged [25, 32]. The only study describing a decrease in activities was published by Yim et al. [50]. Interestingly, this study described an Asian cohort with 96 % (48 of 50) female patients. However, the reason for a decrease in physical activities according to the Tegner score and a sport questionnaire remains unknown.
There has been a lot of debate whether mobile-bearing designs offer a clinical advantage over fixed-bearing designs because of decreased wear rates and reduced shear stress at the interfaces [35]. However, a recent meta-analysis showed that there are no differences in the clinical outcome; and in experienced hands, revision rates are comparable [31]. The current review included four studies with fixed-bearing UKAs, and no differences in the level of post-operative physical activities were observed [25, 26, 33, 50].
Two studies reported on the level of sport and physical activity following lateral UKA [44, 47]. Both studies demonstrated a highly significant improvement of post-operative physical activity according to the UCLA and Tegner activity score, respectively.
Witjes et al. [49] recently published a literature review describing pre- and/or post-operative participation in specific types of sports and/or the time to return to sport after TKA and/or UKA. The authors concluded that participation in sports seems more likely after UKA than after TKA, and patients tend to return to lower-impact types of sport. This review is in line with these observations. However, the current review provides additional information as it included all available studies that described the level of activity utilizing scores commonly used in clinical practice.
There are a number of limitations that warrant acknowledgment. Firstly, only 8 of the 17 studies included were prospectively designed; hence, the level of evidence currently available is not particularly high. It cannot be ignored that retrospective studies may be influenced by various bias-inducing factors. Second, 12 out of 17 studies (2398 of 2636 patients) reported on the Oxford phase 3 unicompartmental knee implant. Therefore, the conclusions of this review are primarily valid for this particular type of implant. Third, most studies, with exception of Pandit et al. [29], were quite small in terms of patient numbers. Finally, the minimum follow-up was <2 years in eight studies. However, in an attempt to increase the number of studies, these studies were not excluded.
In clinical practice, this systematic review may help physicians to manage the expectations of patients regarding the level of physical activity following UKA. Eleven out of thirteen studies described a post-operative increase in physical activity according to validated activity scores. Almost all activities were in line with Knee Society recommendations for the return to recreational and athletic activity. Even though patients have increasing demands, this report suggests that patients do not participate in high-level sports following UKA. The reason for a limitation of sport activities remained unclear in most studies. Only Walker et al. [44] described that the preservation of the implant was the main reason for a limitation of activities.
Additionally, this study allows surgeons performing UKAs to compare their results with the results published in the literature.
Conclusion
Patients following UKA are active according to validated activity scores. A significant increase in low-impact activities and a decrease in high-impact activities after UKA was observed. The number of different sport activities decreased, whereas the session length und frequency remained overall unchanged. Patients with a UKA regularly participate in sport, however, sport participation slightly decreased compared to pre-arthritic levels.
Acknowledgments
Open access funding provided by Medical University of Vienna.
Authors’ contributions
WW drafted the study, directly supervised the systematic review and finalized the manuscript. PK performed the systematic review and drafted the manuscript. UK revised the manuscript and supported the review process. FB provided suggestions on the review process and wrote substantial parts of the manuscript. RW analysed the data and contributed to the manuscript. All authors read and approved the final manuscript.
Appendix
The following search terms were used on MEDLINE:
UKA.
(activity, physical[MeSH Terms] OR activity, motor[MeSH Terms] OR sports[MeSH Terms] OR sports OR sport OR (motor AND activity) OR motor activity OR physical activity OR activity).
1. AND 2.
Compliance with ethical standards
Competing interests
The authors declare that they have no competing interests.
References
- 1.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66(2):228–241. doi: 10.2106/00004623-198466020-00010. [DOI] [PubMed] [Google Scholar]
- 2.Biswas D, Van Thiel GS, Wetters NG, Pack BJ, Berger RA, Della Valle CJ. Medial unicompartmental knee arthroplasty in patients less than 55 years old: minimum of two years of follow-up. J Arthroplasty. 2014;29(1):101–105. doi: 10.1016/j.arth.2013.04.046. [DOI] [PubMed] [Google Scholar]
- 3.Bruni D, Akkawi I, Iacono F, Raspugli GF, Gagliardi M, Nitri M, Grassi A, Zaffagnini S, Bignozzi S, Marcacci M. Minimum thickness of all-poly tibial component unicompartmental knee arthroplasty in patients younger than 60 years does not increase revision rate for aseptic loosening. Knee Surg Sports Traumatol Arthrosc. 2013;11:2462–2467. doi: 10.1007/s00167-013-2578-9. [DOI] [PubMed] [Google Scholar]
- 4.Callaghan JJ. Unicompartmental knee replacement: introduction: where have we been? Where are we now? Where are we going? Clin Orthop Relat Res. 2005;430:272–273. doi: 10.1097/01.blo.0000151844.03672.0b. [DOI] [PubMed] [Google Scholar]
- 5.Cartier P, Khefacha A, Sanouiller JL, Frederick K. Unicondylar knee arthroplasty in middle-aged patients: a minimum 5-year follow-up. Orthopedics. 2007;30(8 Suppl.):62–65. [PubMed] [Google Scholar]
- 6.Davis MA, Ettinger WH, Neuhaus JM, Mallon KP. Knee osteoarthritis and physical functioning: evidence from the NHANES I Epidemiologic Followup Study. J Rheumatol. 1991;18(4):591–598. [PubMed] [Google Scholar]
- 7.Deschamps G, Chol C. Fixed-bearing unicompartmental knee arthroplasty. Patients’ selection and operative technique. Orthop Traumatol Surg Res. 2011;97(6):648–661. doi: 10.1016/j.otsr.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty for younger patients: an alternative view. Clin Orthop Relat Res. 2002;404:108–112. doi: 10.1097/00003086-200211000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Ettinger WH, Jr, Fried LP, Harris T, Shemanski L, Schulz R, Robbins J. Self-reported causes of physical disability in older people: the Cardiovascular Health Study. CHS Collaborative Research Group. J Am Geriatr Soc. 1994;42(10):1035–1044. doi: 10.1111/j.1532-5415.1994.tb06206.x. [DOI] [PubMed] [Google Scholar]
- 10.Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG. Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee. 2006;13(4):296–300. doi: 10.1016/j.knee.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Goodfellow JW, O’Connor J, Dodd CA, Murray DW. Unicompartmental arthroplasty with the Oxford knee. Oxford: Oxford University Press; 2006. [Google Scholar]
- 12.Healy WL, Iorio R, Lemos MJ. Athletic activity after total knee arthroplasty. Clin Orthop Relat Res. 2000;380:65–71. doi: 10.1097/00003086-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377–388. doi: 10.1177/03635465010290032301. [DOI] [PubMed] [Google Scholar]
- 14.Ho JC, Stitzlein RN, Green CJ, Stoner T, Froimson MI. Return to sports activity following UKA and TKA. J Knee Surg. 2016;29(3):254–259. doi: 10.1055/s-0035-1551835. [DOI] [PubMed] [Google Scholar]
- 15.Hooper N, Snell D, Hooper G, Maxwell R, Frampton C. The five-year radiological results of the uncemented Oxford medial compartment knee arthroplasty. Bone Joint J. 2015;97-B(10):1358–1363. doi: 10.1302/0301-620X.97B10.35668. [DOI] [PubMed] [Google Scholar]
- 16.Hopper GP, Leach WJ. Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc. 2008;16(10):973–979. doi: 10.1007/s00167-008-0596-9. [DOI] [PubMed] [Google Scholar]
- 17.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 18.Jahnke A, Mende JK, Maier GS, Ahmed GA, Ishaque BA, Schmitt H, Rickert M, Clarius M, Seeger JB. Sports activities before and after medial unicompartmental knee arthroplasty using the new Heidelberg Sports Activity Score. Int Orthop. 2015;39(3):449–454. doi: 10.1007/s00264-014-2524-6. [DOI] [PubMed] [Google Scholar]
- 19.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71(1):145–150. doi: 10.2106/00004623-198971010-00023. [DOI] [PubMed] [Google Scholar]
- 20.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 21.Liddle AD, Pandit H, Jenkins C, Price AJ, Dodd CA, Gill HS, Murray DW. Preoperative pain location is a poor predictor of outcome after Oxford unicompartmental knee arthroplasty at 1 and 5 years. Knee Surg Sports Traumatol Arthrosc. 2013;21(11):2421–2426. doi: 10.1007/s00167-012-2211-3. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, Dragomir A, Kalsbeek WD, Luta G, Jordan JM. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray DW, Liddle A, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint J. 2015;97-B(10 Suppl. A):3–8. doi: 10.1302/0301-620X.97B10.36542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S, Munzinger U, Drobny T. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35(10):1688–1695. doi: 10.1177/0363546507303562. [DOI] [PubMed] [Google Scholar]
- 26.Naal FD, Neuerburg C, Salzmann GM, Kriner M, von Knoch F, Preiss S, Drobny T, Munzinger U. Association of body mass index and clinical outcome 2 years after unicompartmental knee arthroplasty. Arch Orthop Trauma Surg. 2009;129(4):463–468. doi: 10.1007/s00402-008-0633-7. [DOI] [PubMed] [Google Scholar]
- 27.O’Rourke MR, Gardner JJ, Callaghan JJ, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC. The John Insall Award: unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27–37. doi: 10.1097/01.blo.0000185451.96987.aa. [DOI] [PubMed] [Google Scholar]
- 28.Pandit H, Gulati A, Jenkins C, Barker K, Price AJ, Dodd CA, Murray DW. Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee. 2011;18(3):168–171. doi: 10.1016/j.knee.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93(2):198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 30.Pandit H, Liddle AD, Kendrick BJ, Jenkins C, Price AJ, Gill HS, Dodd CA, Murray DW. Improved fixation in cementless unicompartmental knee replacement: five-year results of a randomized controlled trial. J Bone Joint Surg Am. 2013;95(15):1365–1372. doi: 10.2106/JBJS.L.01005. [DOI] [PubMed] [Google Scholar]
- 31.Peersman G, Stuyts B, Vandenlangenbergh T, Cartier P, Fennema P. Fixed- versus mobile-bearing UKA: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3296–3305. doi: 10.1007/s00167-014-3131-1. [DOI] [PubMed] [Google Scholar]
- 32.Pietschmann MF, Wohlleb L, Weber P, Schmidutz F, Ficklscherer A, Gulecyuz MF, Safi E, Niethammer TR, Jansson V, Muller PE. Sports activities after medial unicompartmental knee arthroplasty Oxford III—what can we expect? Int Orthop. 2013;37(1):31–37. doi: 10.1007/s00264-012-1710-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schai PA, Suh JT, Thornhill TS, Scott RD. Unicompartmental knee arthroplasty in middle-aged patients: a 2- to 6-year follow-up evaluation. J Arthroplasty. 1998;13(4):365–372. doi: 10.1016/S0883-5403(98)90000-6. [DOI] [PubMed] [Google Scholar]
- 34.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 35.Smith TO, Hing CB, Davies L, Donell ST. Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res. 2009;95(8):599–605. doi: 10.1016/j.otsr.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 36.Streit MR, Streit J, Walker T, Bruckner T, Philippe Kretzer J, Ewerbeck V, Merle C, Aldinger PR, Gotterbarm T. Minimally invasive Oxford medial unicompartmental knee arthroplasty in young patients. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3620-x. [DOI] [PubMed] [Google Scholar]
- 37.Streit MR, Walker T, Bruckner T, Merle C, Kretzer JP, Clarius M, Aldinger PR, Gotterbarm T. Mobile-bearing lateral unicompartmental knee replacement with the Oxford domed tibial component: an independent series. J Bone Joint Surg Br. 2012;94(10):1356–1361. doi: 10.1302/0301-620X.94B10.29119. [DOI] [PubMed] [Google Scholar]
- 38.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 39.Verbrugge LM, Lepkowski JM, Konkol LL. Levels of disability among U.S. adults with arthritis. J Gerontol. 1991;46(2):S71–S83. doi: 10.1093/geronj/46.2.S71. [DOI] [PubMed] [Google Scholar]
- 40.Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee. 2014;21(1):180–184. doi: 10.1016/j.knee.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 41.Vorlat P, Putzeys G, Cottenie D, Van Isacker T, Pouliart N, Handelberg F, Casteleyn PP, Gheysen F, Verdonk R. The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):40–45. doi: 10.1007/s00167-005-0621-1. [DOI] [PubMed] [Google Scholar]
- 42.Waldstein W, Bou Monsef J, Buckup J, Boettner F. The value of valgus stress radiographs in the workup for medial unicompartmental arthritis. Clin Orthop Relat Res. 2013;471(12):3998–4003. doi: 10.1007/s11999-013-3212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Waldstein W, Merle C, Bou Monsef J, Boettner F. Varus knee osteoarthritis: how can we identify ACL insufficiency? Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2178–2184. doi: 10.1007/s00167-014-2994-5. [DOI] [PubMed] [Google Scholar]
- 44.Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR. Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3281–3287. doi: 10.1007/s00167-014-3111-5. [DOI] [PubMed] [Google Scholar]
- 45.Walker T, Streit J, Gotterbarm T, Bruckner T, Merle C, Streit MR. Sports, physical activity and patient-reported outcomes after medial unicompartmental knee arthroplasty in young patients. J Arthroplasty. 2015;30(11):1911–1916. doi: 10.1016/j.arth.2015.05.031. [DOI] [PubMed] [Google Scholar]
- 46.Walton NP, Jahromi I, Lewis PL, Dobson PJ, Angel KR, Campbell DG. Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg. 2006;19(2):112–116. doi: 10.1055/s-0030-1248089. [DOI] [PubMed] [Google Scholar]
- 47.Weston-Simons JS, Pandit H, Kendrick BJ, Jenkins C, Barker K, Dodd CA, Murray DW. The mid-term outcomes of the Oxford domed lateral unicompartmental knee replacement. Bone Joint J. 2014;96-B(1):59–64. doi: 10.1302/0301-620X.96B1.31630. [DOI] [PubMed] [Google Scholar]
- 48.White SH, Ludkowski PF, Goodfellow JW. Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br. 1991;73(4):582–586. doi: 10.1302/0301-620X.73B4.2071640. [DOI] [PubMed] [Google Scholar]
- 49.Witjes S, Gouttebarge V, Kuijer PP, van Geenen RC, Poolman RW, Kerkhoffs GM. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46(2):269–292. doi: 10.1007/s40279-015-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yim JH, Song EK, Seo HY, Kim MS, Seon JK. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow-up of 3 years. J Arthroplasty. 2013;28(2):243–247. doi: 10.1016/j.arth.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 51.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]