Abstract
Gay and bisexual men (GBM) report high rates of sexual compulsivity (SC), yet no empirically based treatments exist. An intervention based on the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders was pilot tested in a sample of 13 HIV-positive GBM with SC. Participants completed a baseline interview, and were offered up to ten intervention sessions. Of those, 11 completed a 3-month follow-up assessment. Despite problems with session attendance (only 4 men completed all 10 sessions), improvements were observed in all psychological outcomes, including SC, depression, and anxiety. Decreases were observed in drug use and HIV risk. The Unified Protocol may be useful in improving the health of HIV-positive GBM, however challenges with session attendance must be addressed. Future work should consider if fewer sessions produce similar results, whether barriers to attending all sessions could be alleviated, and how the intervention would perform compared to treatments.
Keywords: Gay and bisexual men, HIV-positive, Sexual compulsivity, Mental health, Cognitive behavioral therapy
Resumen
Hombres gays y bisexuales (HGB) declaran un indice alto de comportamientos sexuales compulsivos (CSC), pero igual no hay ningún tratamiento que existe para poder ayudar. Una intervención basada en el Protocolo Unido para el Tratamiento Transdiagnostico de Desordenes Emocionales fue probado con una muestra de 13 HGB que son positivo con el VIH y con CSC. Los participantes completaron una entrevista de referencia y se les ofreció hasta 10 sesiones de intervención. De ese grupo, 11 completaron una evaluación de seguimiento después de tres meses. Aunque hubieron problemas con la asistencia de las sesiones (solo 4 hombres completaron las 10 sesiones), mejoramientos se observaron en todos los resultados psicologicos, incluyendo CSC, depresion y la ansiedad. Se observaron reducciones en uso de drogas y riesgos para contraer el VIH. El Protocolo Unido puede ser útil en mejorar la salud de HGB con el VIH, pero igual los retos con la asistencia de las sesiones tienen que ser dirigidos. Trabajando con este tratamiento en el futuro se debe considerar si al tener menos sesiones, se produce los mismos resultados, si las barreras para la asistencia de sesiones pueden ser aliviadas y como la intervención se desarollaría comparada con otros tratamientos.
Introduction
Sexual compulsivity (SC) is characterized by sexual fantasies and behaviors that increase in frequency and intensity to a level that they are personally considered out-of-control, serve as a significant source of distress, and interfere with personal, interpersonal, and vocational pursuits [1–4]. Some estimates have suggested a prevalence of SC between 3 and 6 % in the general U.S. population, with higher prevalence among men [5, 6], with the greatest prevalence among gay and bisexual men (GBM) [7, 8]. Higher rates of SC have been also observed among HIV-positive GBM compared to HIV-negative GBM [9]. Among HIV-positive GBM, SC has been associated with increased HIV transmission risk behavior (TRB), which includes a greater number of condomless anal sex acts (CAS), more concurrent CAS sexual partners, engaging in so-called sexual marathons, and greater incidence of STIs, as well as lower condom self-efficacy and HIV status disclosure [10–16]. As such, treating the symptoms of SC among HIV-positive GBM may serve several purposes, including the reduction in psychological distress [17, 18] and improvement in health as well as a reduction in the risk of HIV transmission. Such a treatment should be considered a high public health priority given that GBM represent an overwhelming majority of new HIV infections in the U.S. [19].
Among GBM, high levels of mental health comorbidity have been observed, particularly with anxiety, depression and substance use disorders [20, 21]. Evidence suggests that when such problems co-occur they create a synergistic epidemic (i.e., syndemic) of problems that act in an additive fashion to increase TRB [22–29]. SC has been found to be associated with known syndemic factors [22, 30–33], and recent evidence suggests that SC might best be considered a syndemic factor itself among GBM [18, 26]. One possible explanation for the disproportionate experience of SC as well as other syndemic factors among GBM is their exposure to sexual minority stress. Minority stress theory posits that GBM experience disproportionate amount of stress due to the stigmatized status of their sexual orientation [34, 35]. In addition to sexual minority stressors, HIV-related stigma is an additional stressor for HIV-positive GBM and likely drives increased burden of psychological distress observed among these men [36]. We have previously found that, for HIV-positive GBM, the internalization of HIV-related stigma predicts experiences of SC over and above the influence of sexual minority stigma [18]. These findings suggest that treatments for SC that are sensitive to these experiences and tailored to address them may be most effective.
Two universal processes that have been shown to underlie the experience of SC for GBM are emotion dysregulation and maladaptive cognitions. The association between both sexual minority and HIV-related stressors and mental health outcomes—including anxiety, depression, and SC—has been shown to be mediated over time by decreased emotion regulation [17, 37]. In addition to these underlying difficulties with regulating emotion, the association between sexual minority and HIV-related stressors and negative health outcomes may also be explained in part by maladaptive coping strategies [38]. As such, in addition to a tailored focus on minority and HIV-related stress processes, treatments for SC should target these core underlying mechanisms of emotion dysregulation and maladaptive cognitions.
Despite evidence linking SC with a range of problems for GBM, no empirically-based treatments for SC exist. A review of current treatment approaches for SC suggests clinicians rely on various behavioral treatment modalities [39], none of which have been empirically supported through RCTs [40]. Among these approaches, cognitive behavioral therapy (CBT) has been suggested as a potential approach to promote regulation of compulsive sexual behavior [41–43]. For years, there have been calls for parsimonious and pragmatic treatments that address common factors underlying frequently co-occurring psychosocial conditions [44, 45]. As such, transdiagnostic treatments have been developed for the treatment of emotional disorders using empirically supported principles of CBT [46]. Ellard et al. [46] developed a Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (UP) that expanded on common principles of CBT to include a greater focus on the interactions between emotions and cognitions. The UP was recently adapted for use with HIV-negative GBM to reduce TRB and the disproportionate experience of mental health problems rooted in minority stress, and compared to a waitlist condition, this intervention (Project ESTEEM) resulted in significant reductions for depression, alcohol use problems, SC, and TRB [47].
HIV-positive GBM are disproportionally affected by symptoms of SC [9, 48], and often report increased rates of TRB [49, 50] and substance use [51–53]. As such, an empirically-based unified approach that addresses associations between sexual minority and HIV-related stressors, SC, substance use, and HIV TRB is warranted. As a result, we pilot tested the ESTEEM intervention with a sample of HIV-positive GBM with high levels of SC (ESTEEM-SC). We sought to examine the feasibility and acceptability of the intervention, and preliminary estimates of its impact on SC as well as the general problems it was designed to impact (e.g., depression, anxiety, emotion regulation) among HIV-positive GBM.
Methods
Participants
Between May and July of 2014, we recruited HIV-positive GBM through advertisements posted on social and sexual networking websites and mobile applications (e.g., Facebook, sex party listservs, a popular mobile sex-seeking app) and through active and passive recruitment methods implemented in diverse geographic areas of NYC using techniques previously effective in the recruitment of GBM [54–57]. In addition, we contacted former participants of a study focused on SC among GBM in New York City who had agreed to be notified about future studies. We enrolled 13 men; slightly less than half (n = 6, 46.2 %) were recruited from a former observational study focused on SC, the same number (n = 6, 46.2 %) were recruited via Facebook, and one was recruited via an email blast to a nightlife listserv.
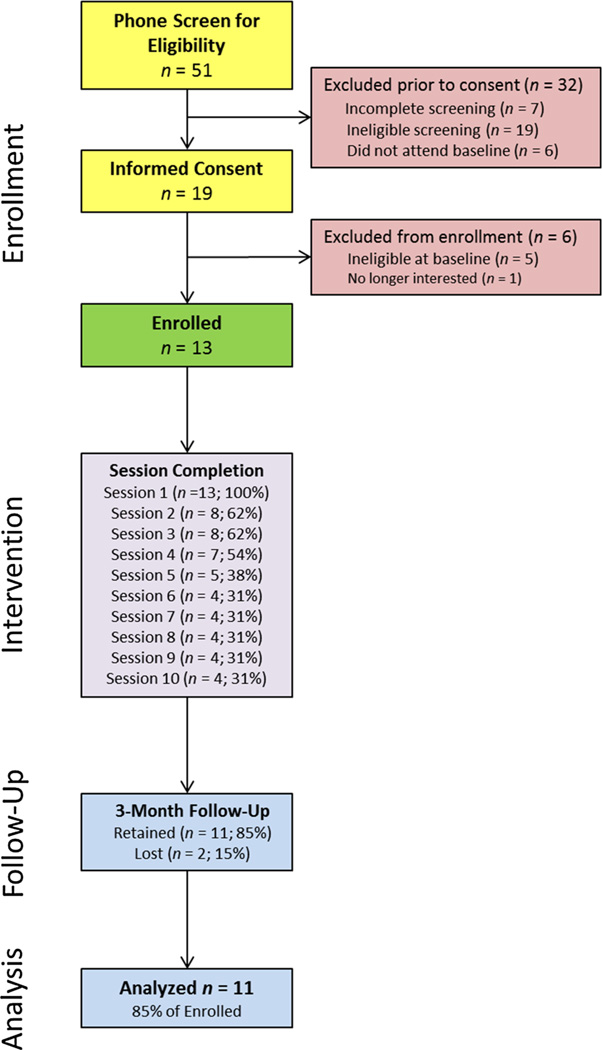
All potential participants completed a brief screening questionnaire over the phone to confirm eligibility. These eligibility criteria were defined as: (1) being born male and currently identifying as male; (2) identifying as gay or bisexual; (3) being aged 18 or older; (4) being fluent in English; (5) residing in the New York City area; (6) being HIV-positive; (7) reporting recent (past 90 days)TRB(i.e., at least one instance of CAS with any casual male partner or with an HIV-negative or status-unknown main male partner); (8) reporting symptoms of SC; and (9) not currently receiving regular mental health services. SC symptomology was assessed during the phone screener using the 10-item Sexual Compulsivity Scale [2, 58] and, consistent with prior research, a cutoff of 24 or higher was considered indicative of high symptomology [10, 18, 48, 59]. Figure 1 displays the CONSORT model for the present non-randomized pilot trial, including data on attendance at each intervention session. We enrolled 13 men, of whom two were unable to be retained at follow-up assessment, resulting in an analytic sample of 11 men for pre-post analyses.
Fig. 1.
This figure displays the CONSORT model for the non-randomized ESTEEM-SC intervention pilot trial. As can be seen, of the 13 men who were enrolled and initiated treatment, 11 (84.6 %) were retained at follow-up and examined for pre-post analyses in the present manuscript
Procedures
Upon reviewing an online study advertisement or receiving an invitation to participate in the research study, interested individuals contacted the research office to complete an eligibility screening by phone. During the call, a research assistant assessed consent for phone screening, described the study, and asked questions to assess eligibility. Eligible participants were sent a link leading to a survey containing measures to be completed from home and scheduled for an in-office appointment to complete the remaining baseline measures and to confirm final eligibility. After completing the at-home survey and the in-office portion of the baseline assessment and confirming eligibility, all participants completed their first ESTEEM-SC treatment session. Treatment occurred over the course of 3 months between the baseline and 3-month assessment. During the 3-month assessment, participants were asked to provide brief, qualitative feedback on the intervention, including barriers to attending sessions. All procedures were reviewed and approved by the Institutional Review Board of the City University of New York.
Intervention
ESTEEM-SC is a 10-session intervention based on ESTEEM, which was based on the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders [60]. Modules were adapted to help participants identify minority stress experiences; track and address cognitive, affective, and behavioral reactions to minority stress, with a focus on avoidance reactions, including substance use and CAS; attribute distress to minority stress rather than to personal failure; and assertively confront minority stress related situations in safe contexts. Adaptations were infused throughout the Unified Protocol Therapist Work-book [60]; this adaptation served as the therapist manual for each session. Module content is described in detail elsewhere [47]. ESTEEM-SC was delivered by advanced clinical psychology doctoral students.
Outcome Measures
Given the literature reviewed previously, we sought to examine the effect of ESTEEM-SC on several primary outcomes. Given that the intervention directly targets difficulties with emotion regulation and symptoms of SC, we examined these as the primary outcomes. Moreover, because depression and anxiety have been found to be strongly associated with SC and because the UP is used to treat both, we examined both the symptom severity of and functional impairment from depression and anxiety. Because SC is often considered to be a problem resulting from compulsive thoughts and behaviors, we also sought to examine any impact on general obsessive–compulsive symptomatology. Finally, we sought to examine the extent to which the intervention would reduce TRB and substance use, both of which have been found to be associated with SC. The following measures were administered at the baseline enrollment and at 3 months follow-up.
Difficulties of Emotion Regulation Scale (DERS)
The 36-item DERS [61] was used to assess symptoms of emotion dysregulation. Participants indicated how much each statement applied to them from 1 (almost never [0– 10 %]) to 5 (almost always [91– 100 %]). We utilized the full scale score, calculated as the summed response across the 36 items, as an indicator of overall emotion dysregulation (BL α = 0.89, 3M α = 0.92).
Sexual Compulsivity Scale (SCS)
The SCS [58] was used to measure symptoms of sexual compulsivity. The SCS contains 10 items rated on a scale from 1 (not at all like me) to 4 (very much like me) and responses were summed to derive an overall score (BL α = 0.90, 3M α = 0.98).
Center for Epidemiological Studies Depression Scale (CESD)
The CESD [62] was utilized to measure depressive symptomology. The scale consists of 20 items that ask individuals to rate how often they have experienced symptoms of depression in the past week with responses ranging from 1 (rarely or none of the time [less than 1 day]) to 4 (most or all of the time [5–7 days]). Responses were summed to form an overall score (BL α = 0.88, 3M α = 0.88).
Penn State Worry Questionnaire (PSWQ)
The 16-item PSWQ [63] was used to measure symptoms of generalized anxiety. Response options ranged from 1 (Not at all typical of me) to 5 (Very typical of me) and were summed to form an overall index of generalized anxiety symptomology (BL α = 0.82, 3M α = 0.75).
Overall Depression Severity and Impairment Scale (ODSIS)
The 5-item ODSIS [64] was used to assess past-week depressive symptom severity and functional impairment. Response options ranged from 0 (None) to 4 (Extreme) with additional qualitative responses appended to each item’s response option. Responses were summed to form an index of functional impairment related to depressive symptomology (BL α = 0.93, 3M α = 0.89).
Overall Anxiety Severity and Impairment Scale (OASIS)
The 5-item OASIS [65] was used to assesses severity and functional impairment associated with any anxiety disorder over the past week. Like the ODSIS, responses ranged from 0 (Little or none) to 4 (Extreme) with more detailed qualitative responses appended to each item’s response option. Responses were summed to form an overall index of functional impairment related to anxious symptomology (BL α = 0.80, 3M α = 0.94).
Yale-Brown Obsessive Compulsive Scale (YBOCS)
The 10-item YBOCS [66] was used to assess obsessive–compulsive symptomology characterized by loss of control, salience, distress, interference, and resistance against obsessive and compulsive thoughts. Responses ranged from 0 to 4 with response options tailored to each question (e.g., 0 = none, 4 = extreme interference, incapacitating) and choices were summed to form an overall index of obsessive– compulsive symptomology (BL α = 0.81, 3M α = 0.69).
Short Inventory of Problems for Drug Use (SIP-DU)
The 15-item SIP-DU [67] was used to assess the frequency of negative consequences of drug use in the past 90 days. Responses ranged from 0 (Never) to 3 (Daily or almost daily) and were summed to form an index of the amount of problems participants faced as a result of their drug use (BL α = 0.97, 3M α = 0.97).
90-Day Time Line Follow Back (TLFB)
Past 90-day sexual behaviour and substance use were assessed with the TLFB [68]. The TLFB demonstrates strong reliability and validity, including agreement with real-time interviews and collateral reports of alcohol use [69] and sex risk [70], and has previously been utilized with HIV-positive GBM [71–73] and GBM with SC [9, 26, 74, 75]. From the TLFB we calculated: (1) the total number of new (i.e., first-time) male partners men had as an indicator of frequency of sexual partnering; (2) the total number of CAS acts with any non-main (i.e., casual) male partners as an indicator of TRB; and (3) the total number of days on which club drugs (i.e., cocaine/crack, crystal methamphetamine, ecstasy/MDMA, ketamine, and GHB) were used as an indicator of substance use frequency.
Data Analyses
To better understand any changes resulting from the ESTEEM-SC intervention, we calculated pre-post changes (from baseline enrollment to 3-month follow-up) in the primary outcome measures using paired samples t-tests, using data from the 11 men retained at follow-up. We did this both for psychological outcomes as well as sexual risk and substance use. In doing so, we utilized the results of the t-tests to calculate Cohen’s dz as a measure of effect size, and interpreted effects as small (dz = 0.2), medium (dz = 0.5) and large (dz = 0.8) following published guidelines [76, 77].
Results
As can be seen in Table 1, the retained sample consisted predominantly of men of color, with only 18.2 % of men identifying as White and nearly half (45.5 %) as Black. A majority of the sample was gay-identified, had less than a bachelor’s degree, and was single. The sample was split nearly evenly with regard to employment, with 54.5 % being unemployed at the time of enrollment. The men were 34 years of age, on average. The CONSORT model in Fig. 1 displays information on completion of each session. Of the 13 participants enrolled, four (30.7 %) completed all 10 sessions, and 5 men (38.5 %) completed only the first session that occurred immediately after the baseline assessment. The two men not retained at follow-up were two of the five who completed only the first session. As can be seen at the bottom of Table 1, the average number of sessions completed was 5.4.
Table 1.
Demographic Characteristics of the ESTEEM-SC Sample (n = 11)
| n | % | |
|---|---|---|
| Race/ethnicity | ||
| Black | 5 | 45.5 |
| Latino | 3 | 27.3 |
| White | 2 | 18.2 |
| Other/multiracial | 1 | 9.1 |
| Sexual orientation | ||
| Gay | 10 | 90.9 |
| Bisexual | 1 | 9.1 |
| Employment status | ||
| Employed | 5 | 45.5 |
| Unemployed | 6 | 54.5 |
| Highest educational attainment | ||
| Less than bachelor’s degree | 10 | 90.9 |
| Bachelor’s degree or higher | 1 | 9.1 |
| Relationship status | ||
| Single | 9 | 81.8 |
| Partnered | 2 | 18.2 |
| M | SD | |
| Age (range 27–51; Mdn. = 30.0) | 34.4 | 9.6 |
| Sessions attended (range 1–10; Mdn. = 4.0) | 5.4 | 3.9 |
Table 2 presents the results for the change from baseline to follow-up in the psychological outcomes of emotion dysregulation, SC, depressive symptomatology, generalized anxiety symptomatology, depression-related functional impairment, anxiety-related functional impairment, and obsessive–compulsive symptoms for the 11 men retained. Three of the seven outcomes reached a statistically significance decline, demonstrating improvement over time in depressive symptomatology as measured by the CESD, generalized anxiety symptomatology as measured by the PSWQ, and obsessive–compulsive symptomatology as measured by the YBOCS. We also observed a marginally significant reduction in anxiety-related functional impairment as measured by the OASIS. Moreover, all psychological outcomes showed reductions, with effect sizes ranging from small-to-moderate for SC and depression-related functional impairment to large for those three variables that reached statistical significance.
Table 2.
Pre-post changes in psychological outcomes (n = 11)
| BL | 3M | BL vs. 3M | |||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | t(10) | p | dz | |
| Emotion dysregulation (DERS) | 109.36 | 20.99 | 98.36 | 19.55 | 1.76 | 0.11 | 0.53 |
| Sexual compulsivity (SCS) | 27.82 | 6.35 | 24.27 | 10.03 | 1.35 | 0.21 | 0.41 |
| Depressive symptomatology (CESD) | 1.29 | 0.48 | 0.90 | 0.42 | 2.76 | 0.02 | 0.83 |
| Generalized anxiety symptomatology (PSWQ) | 57.45 | 8.09 | 50.00 | 11.64 | 5.57 | <0.001 | 1.68 |
| Depression-related functional impairment (ODSIS) | 7.82 | 5.02 | 6.18 | 3.76 | 1.20 | 0.26 | 0.36 |
| Anxiety-related functional impairment (OASIS) | 8.82 | 4.00 | 6.27 | 4.67 | 2.03 | 0.07 | 0.61 |
| Obsessive–compulsive symptomatology (YBOCS) | 17.18 | 5.23 | 13.55 | 3.88 | 3.01 | 0.01 | 0.91 |
Table 3 presents the results regarding changes from baseline to follow-up in sexual risk and substance use for the 11 men retained. As can be seen, we did not observe any statistically significant changes in drug-related problems, frequency of drug use, or TRB. Effect sizes, however, demonstrated small-to-moderate decreases in both drug use problems and frequency of drug use. Importantly, though not significant, we observed medium effect sizes for reductions in number of new male sexual partners—reducing by nearly nine partners, on average—as well as number of CAS acts with casual male partners, which were reduced by nearly 14 instances.
Table 3.
Pre-post changes in sexual risk outcomes and substance use (n = 11)
| BL | 3M | BL vs. 3M | |||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | t(10) | p | dz | |
| New male partners | 16.36 | 24.10 | 7.72 | 9.53 | 1.63 | 0.14 | 0.49 |
| CAS acts with casual male partners (TRB) | 21.09 | 30.71 | 7.72 | 9.50 | 1.66 | 0.13 | 0.50 |
| Drug use problems (SIP-DU) | 16.18 | 14.50 | 10.91 | 11.28 | 1.24 | 0.24 | 0.37 |
| Club drug use days | 3.91 | 6.07 | 3.45 | 4.66 | 0.39 | 0.70 | 0.21 |
Ten of the 11 retained participants provided qualitative data on their experience in ESTEEM-SC. The four participants who completed all ten sessions reported enjoying their therapist, homework assignments, and the topics covered in the sessions. These participants expressed an awareness of their TRB and problematic SC symptoms, and reported that they “wanted help.” Participants who completed 3–5 of the ten sessions reported that work, family, and other obligations prevented them from attending all the sessions. Although some sessions missed were able to be rescheduled, others were not due to logistics and scheduling challenges. Participants who attended only the first session (the session that occurred right after the baseline appointment) identified several barriers to coming back for the remaining sessions, including transportation barriers and problems with the availability of therapists for scheduling (e.g., the participant was available during the morning, but the assigned therapist was only available later in the day). One participant indicated that a family emergency prevented him from coming back for any sessions, and another reported that he felt uncomfortable with a female therapist.
Discussion
SC disproportionately affects GBM, particularly HIV-positive GBM, and is associated with increased HIV TRB. With no empirically supported treatments for SC, the present findings represent an effort to adapt and pilot test an empirically-driven intervention designed for HIV-negative GBM with mental health difficulties to be used with HIV-positive GBM with high levels of SC symptomology. The ESTEEM-SC intervention resulted in large effects on psychological distress, with significant reductions observed in anxiety, depression, and obsessive compulsive symptoms, despite a very small sample size. Reductions were also observed for SC as well as sexual risk and substance use, with the effect sizes ranging from small to moderate. These findings are consistent with a randomized waitlist-controlled trial of the original ESTEEM intervention in a sample of HIV-negative GBM with anxiety or depression [47]. Further, the effects of this intervention were observed in a racially and ethnically diverse sample of HIV-positive men, addressing a significant gap in research and treatment with men of color, for whom HIV transmission rates are disproportionately high [78].
Intensive interventions that target more than one syndemic condition have generally been shown to be more effective in reducing sexual risk behaviors compared to interventions that target only one condition [79]. A meta-analysis of 12 interventions aimed at reducing HIV TRB among HIV-positive persons found significant reductions in five of the 12 studies [80]. Two features that distinguished these five studies from the others were that they were intensive and they addressed a myriad of factors associated with HIV. Research suggests that interventions that narrowly focus on one syndemic factor result in less durable effects [79]. ESTEEM-SC addressed and reduced symptoms of several known syndemic conditions affecting HIV-positive GBM, including SC, depression, sexual risk, and substance use. Even with the use of highly trained therapists, these types of intensive interventions have been shown to be cost-effective in comparison to the cost associated with treating someone who is affected with HIV. Safren et al. [79] estimated that treating as many as 100 HIV-positive persons with a 20-session intervention using the highest trained therapists costs significantly less than the health care costs associated with treating one new HIV infection.
The present study tested such an intervention in a sample of HIV-positive GBM with high levels of SC. SC operates as one of several syndemic factors that compound the risk for HIV transmission [18, 26]. In fact, we found that ESTEEM-SC produced improvements in SC symptoms while also improving two additional syndemic factors, depression and substance use. Currently, interventions that address syndemics as a whole have not been tested and given the high incidence of HIV among GBM the development of treatments targeting syndemic conditions is a high priority [26, 79]. The findings from the present study suggest that by targeting core deficits in emotion regulation and tailoring content to the unique issues faced by HIV-positive GBM with SC, the effects of ESTEEM-SC may generalize to comorbid anxiety and mood conditions. The associated effects on depression are particularly noteworthy given that both SC and depression have been implicated in syndemic processes which accelerate HIV incidence in MSM populations [18, 26].
However, the intensive nature of the intervention also posed challenges, with less than ideal retention across the ten sessions of ESTEEM-SC. On average, men completed between five and six sessions; over a third of men enrolled only attended the first session and approximately another third completed all 10. In the original ESTEEM study, rates of session attendance were also problematic, with nearly a third completing only one session and only 44 % completing all 10 session. The UP (the basis for both ESTEEM and ESTEEM-SC) is structured to have as many as 18 sessions [60] and, by comparison, the 10 session ESTEEM-SC intervention is modest and comparable to three of the most successful behavioral interventions that have targeted HIV-positive populations—the Healthy Living Project (15 90-min sessions) [81], PLUS (8 sessions) [82], and CBT-AD (10–12 sessions) [83, 84]. However, these other more intensive interventions had better session attendance than we found for ESTEEM-SC, suggesting that it would be helpful to reduce the number of sessions and/or modify logistical factors that participants cited as barriers to attendance. We combined the first intervention session with the baseline, and as such 38 % of participants completed only the first ESTEEM-SC session. It is possible these participants were motivated more by the financial incentive of participation in a research project than by the opportunity for treatment. Men who attended all or most of their intervention sessions talked about being very motivated to work on their SC symptoms and reported enjoying the session content and homework. A delayed onset randomization that occurs after attendance at baseline could help in future studies to enroll only those with motivation to receive treatment for SC.
It is also possible that some of the barriers cited by the men—logistical issues related to scheduling, transportation challenges, and therapist characteristics—were of greater concern for those with less initial motivation to work on their SC associated problems. Some of these barriers could be addressed through more flexible scheduling, offering intervention sessions by phone or video-chat, and providing options regarding important therapist characteristics such as gender. Additional limitations include the small sample size, the fact that all participants were recruited in a large urban area, limited follow-up period, and the use of only a pre- and post-test design thus capitalizing on assessment effects and regression to the mean.
Conclusions
It is noteworthy that, despite retention challenges and other limitations, significant effects were observed in this pilot sample. This suggests that even small doses of CBT tailored for HIV-positive GBM can have a meaningful effect and further suggests the possibility that addressing retention challenges may enhance such effects. One of the most significant findings is that this intervention resulted in significant reduction in SC and other mental health problems. The next step is to examine whether or not the same effects could be observed with an intervention with fewer sessions, so as to increase treatment retention. Following further piloting of the study in order to improve accessibility and reduce burden of the sessions, the next step is to test ESTEEM-SC in a randomized control trial. Doing so should involve examining its efficacy compared to a time- and attention-matched control condition consisting of an existing HIV behavioral intervention that is not designed to simultaneously address SC and mental health issues for HIV-positive GBM. Finally, this study relied on 10 sessions of individualized therapy and studies should examine the cost-effectiveness of such an approach. As mentioned, the cost of treating HIV as well as other health problems among GBM remains significant and an intensive intervention is potentially justified [79]. There is the potential for great long-term benefit in targeting limited resources for treatment to the GBM who are in the most need.
Acknowledgments
This pilot project was conducted by the Hunter College Center for HIV/AIDS Educational Studies and Training (CHEST), under the direction of Jeffrey T. Parsons. The authors acknowledge the contributions of other members of the ESTEEM-SC Research Team involved in this project: Evie Arroyo, Demetria Cain, Chris Hietikko, Ruben Jimenez, Douglas Keeler, Alexa Michl, Brett Millar, Chloe Mirzayi, Chris Murphy, Luis Nobrega, Carlos Ponton, Rachel Proujanksy, Brian Salfas, Laurie Spacek, Jonathan Warren, and Thomas Whitfield.
Funding This study was funded by the Hunter College Center for HIV/AIDS Educational Studies and Training (CHEST), under the direction of Jeffrey T. Parsons. H. Jonathon Rendina’s contribution to this project was supported by a career development award from the National Institute on Drug Abuse (K01-DA039030). Raymond L. Moody’s contribution to the project was supported, in part, by a supplement to a grant from the National Institute on Drug Abuse (R01-DA036466 S2). John Pachankis was supported, in part, by a grant from the National Institute on Mental Health (R34-MH096607). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Compliance with Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflicts of interest The authors declare they have no conflict of interest.
References
- 1.Kafka MP. Hypersexual disorder: a proposed diagnosis for DSMV. Arch Sex Behav. 2010;39(2):377–400. doi: 10.1007/s10508-009-9574-7. [DOI] [PubMed] [Google Scholar]
- 2.Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: validity, and predicting HIV risk behavior. J Personal Assess. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 3.Muench F, Parsons JT. Sexual compulsivity and HIV: identification and treatment. Focus. 2004;19(6):1–5. [PubMed] [Google Scholar]
- 4.Parsons JT, Kelly BC, Bimbi DS, Muench F, Morgenstern J. Accounting for the social triggers of sexual compulsivity. J Addict Dis. 2007;26(3):5–16. doi: 10.1300/J069v26n03_02. [DOI] [PubMed] [Google Scholar]
- 5.Black DW. Compulsive sexual behavior: a review. J Psychiatr Pract. 1998;4(4):219–229. [Google Scholar]
- 6.Kuzma JM, Black DW. Epidemiology, prevalence, and natural history of compulsive sexual behavior. Psychiatr Clin N Am. 2008;31(4):603–611. doi: 10.1016/j.psc.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Baum MD, Fishman JM. AIDS, sexual compulsivity, and gay men: a group treatment approach. In: Cadwell SA, Burnham RA Jr, editors. Therapists on the front line: psychotherapy with gay men in the age of AIDS. Washington, DC: American Psychiatric Press Inc; 1994. pp. 255–274. [Google Scholar]
- 8.Missildine W, Feldstein G, Punzalan JC, Parsons JT. S/he loves me s/he loves me not: questioning heterosexist assumptions of gender differences for romantic and sexually motivated behaviors. Sex Addict Compulsivity. 2005;12(1):65–74. [Google Scholar]
- 9.Parsons JT, Rendina HJ, Ventuneac A, Moody RL, Grov C. Hypersexual, sexually compulsive, or just highly sexually active? Investigating three distinct groups of gay and bisexual men and their profiles of HIV-related sexual risk. AIDS Behav. 2015;20(2):1903–1913. doi: 10.1007/s10461-015-1029-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in HIV seropositive men who have sex with men: prevalence and predictors of high-risk behaviors. Addict Behav. 1999;24(6):857–868. doi: 10.1016/s0306-4603(99)00056-8. [DOI] [PubMed] [Google Scholar]
- 11.Shuper PA, Joharchi N, Rehm J. Personality as a predictor of unprotected sexual behavior among people living with HIV/AIDS: a systematic review. AIDS Behav. 2014;18(2):398–410. doi: 10.1007/s10461-013-0554-5. [DOI] [PubMed] [Google Scholar]
- 12.Kalichman SC, Greenberg J, Abel GG. HIV-seropositive men who engage in high risk sexual behavior: psychological characteristics and implications for prevention. AIDS Care. 1997;9(4):441–540. doi: 10.1080/09540129750124984. [DOI] [PubMed] [Google Scholar]
- 13.O’Leary A, Wolitski RJ, Remien RH, et al. Psychosocial correlates of transmission risk behavior among HIV-seropositive gay and bisexual men. AIDS. 2005;19:S67–S75. doi: 10.1097/01.aids.0000167353.02289.b9. [DOI] [PubMed] [Google Scholar]
- 14.Reece M. Sexual compulsivity and HIV serostatus disclosure among men who have sex with men. Sex Addict Compulsivity. 2003;10:1–11. [Google Scholar]
- 15.Lacefield K, Negy C, Schrader RM, Kuhlman C. Comparing psychosocial correlates of condomless anal sex in HIV-diagnosed and HIV-nondiagnosed men who have sex with men: a series of meta-analyses of studies from 1993–2013. LGBT Health. 2015;2(3):200–220. doi: 10.1089/lgbt.2014.0069. [DOI] [PubMed] [Google Scholar]
- 16.Semple SJ, Zians J, Grant I, Patterson TL. Sexual compulsivity in a sample of HIV-positive methamphetamine-using gay and bisexual men. AIDS Behav. 2006;10(5):587–598. doi: 10.1007/s10461-006-9127-1. [DOI] [PubMed] [Google Scholar]
- 17.Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, Parsons JT. Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: a longitudinal examination of mental health and sexual risk behavior. Ann Behav Med. 2016 doi: 10.1007/s12160-016-9822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and sexual compulsivity in a community-based sample of HIV-positive gay and bisexual men. AIDS Behav. 2012;16(3):741–750. doi: 10.1007/s10461-011-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson AS, Hall HI, Hu X, Lansky A, Holtgrave DR, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA. 2014;312(4):432–434. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cochran SD, Sullivan JG, Mays VM. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003;71(1):53–61. doi: 10.1037//0022-006x.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee JH, Gamarel KE, Kahler CW, et al. Co-occurring psychiatric and drug use disorders among sexual minority men with lifetime alcohol use disorders. Drug Alcohol Depend. 2015;151:167–172. doi: 10.1016/j.drugalcdep.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dyer TP, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012;89(4):697–708. doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. 2012;102(1):156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parsons JT, Rendina HJ, Moody RL, Ventuneac A, Grov C. Syndemic production and sexual compulsivity/hypersexuality in highly sexually active gay and bisexual men: further evidence for a three group conceptualization. Arch Sex Behav. 2015;44(7):1903–1913. doi: 10.1007/s10508-015-0574-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Leary A, Jemmott JB, III, Stevens R, Rutledge SE, Icard LD. Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS Behav. 2014;18(11):2080–2088. doi: 10.1007/s10461-014-0708-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singer MC. AIDS and the health crisis of the US urban poor: the perspective of critical medical anthropology. Soc Sci Med. 1994;39(7):931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- 29.Singer MC, Erickson PI, Badiane L, et al. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63(8):2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carrico AW, Pollack LM, Stall RD, et al. Psychological processes and stimulant use among men who have sex with men. Drug Alcohol Depend. 2012;123(1):79–83. doi: 10.1016/j.drugalcdep.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herrick AL, Lim SH, Plankey MW, et al. Adversity and syndemic production among men participating in the multicenter AIDS cohort study: a life-course approach. Am J Public Health. 2013;103(1):79–85. doi: 10.2105/AJPH.2012.300810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raymond NC, Coleman E, Miner MH. Psychiatric comorbidity and compulsive/impulsive traits in compulsive sexual behavior. Compr Psychiatry. 2003;44:370–380. doi: 10.1016/S0010-440X(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 33.Black DW, Kehrberg LLD, Flumerfelt DL, Schlosser SS. Characteristics of 36 subjects reporting compulsive sexual behavior. Am J Psychiatry. 1997;154(2):243–249. doi: 10.1176/ajp.154.2.243. [DOI] [PubMed] [Google Scholar]
- 34.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hatzenbuehler ML, O’Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–234. doi: 10.1007/s12160-011-9275-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pachankis JE, Rendina HJ, Restar A, Ventuneac A, Grov C, Parsons JT. A minority stress—emotion regulation model of sexual compulsivity among highly sexually active gay and bisexual men. Health Psychol. 2015;34(8):829–840. doi: 10.1037/hea0000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pachankis JE, Rendina HJ, Ventuneac A, Grov C, Parsons JT. The role of maladaptive cognitions in hypersexuality among highly sexually active gay and bisexual men. Arch Sex Behav. 2014;43(4):669–683. doi: 10.1007/s10508-014-0261-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cooper M, Lebo RA. Assessment and treatment of sexual compulsivity: a multi-modal perspective. J Soc Work Pract Addict. 2001;1(2):61–74. [Google Scholar]
- 40.Krueger RB, Kaplan MS. The paraphilic and hypersexual disorders: an overview. J Psychiatr Pract. 2001;7(6):391–403. doi: 10.1097/00131746-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Kaplan MS, Krueger RB. Diagnosis, assessment, and treatment of hypersexuality. J Sex Res. 2010;47(2–3):181–198. doi: 10.1080/00224491003592863. [DOI] [PubMed] [Google Scholar]
- 42.McConaghy N, Armstrong MS, Blaszczynski A. Expectancy, covert sensitization and imaginal desensitization in compulsive sexuality. Acta Psychiatr Scand. 1985;72(2):176–187. doi: 10.1111/j.1600-0447.1985.tb02592.x. [DOI] [PubMed] [Google Scholar]
- 43.Sbraga TP, O’Donohue WT. The sex addiction workbook: proven strategies to help you regain control of your life. Oakland: New Harbinger Publications; 2004. [Google Scholar]
- 44.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther. 2004;35(2):205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 45.Goldfried MR. Toward the delineation of therapeutic change principles. Am Psychol. 1980;35(11):991–999. doi: 10.1037//0003-066x.35.11.991. [DOI] [PubMed] [Google Scholar]
- 46.Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified protocol for the transdiagnostic treatment of emotional disorders: protocol development and initial outcome data. Cogn Behav Pract. 2010;17(1):88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: a randomized controlled trial of a transdiagnostic minority stress approach. J Consult Clin Psychol. 2015;83(5):875–889. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Arch Sex Behav. 2010;39(4):940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Forney JC, Miller RL The City Project Study T. Risk and protective factors related to HIV-risk behavior: a comparison between HIV-positive and HIV-negative young men who have sex with men. AIDS Care. 2012;24(5):544–552. doi: 10.1080/09540121.2011.630341. [DOI] [PubMed] [Google Scholar]
- 50.van Kesteren NMC, Hospers HJ, Kok G. Sexual risk behavior among HIV-positive men who have sex with men: a literature review. Patient Educ Couns. 2007;65(1):5–20. doi: 10.1016/j.pec.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 51.Pantalone DW, Bimbi DS, Holder CA, Golub SA, Parsons JT. Consistency and change in club drug use by sexual minority men in New York City, 2002 to 2007. Am J Public Health. 2010;100(10):1892–1895. doi: 10.2105/AJPH.2009.175232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rhodes SD, Hergenrather KC, Yee LJ, Knipper E, Wilkin AM, Omli MR. Characteristics of a sample of men who have sex with men, recruited from gay bars and Internet chat rooms, who report methamphetamine use. AIDS Patient Care STDS. 2007;21(8):575–583. doi: 10.1089/apc.2007.0002. [DOI] [PubMed] [Google Scholar]
- 53.Yu G, Wall MM, Chiasson MA, Hirshfield S. Complex drug use patterns and associated HIV transmission risk behaviors in an internet sample of U.S. men who have sex with men. Arch Sex Behav. 2014;44(2):421–428. doi: 10.1007/s10508-014-0337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grov C, Bux D, Parsons JT, Morgenstern J. Recruiting hard-to-reach drug-using men who have sex with men into an intervention study: lessons learned and implications for applied research. Subst Use Misuse. 2009;44(13):1855–1871. doi: 10.3109/10826080802501570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vial AC, Starks TJ, Parsons JT. Finding and recruiting the highest risk HIV-negative men who have sex with men. AIDS Educ Prev. 2014;26(1):56–67. doi: 10.1521/aeap.2014.26.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vial AC, Starks TJ, Parsons JT. Relative efficiency of field and online strategies in the recruitment of HIV-positive men who have sex with men. AIDS Educ Prev. 2015;27(2):103–111. doi: 10.1521/aeap.2015.27.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Parsons JT, Vial AC, Starks TJ, Golub SA. Recruiting drug using men who have sex with men in behavioral intervention trials: a comparison of internet and field-based strategies. AIDS Behav. 2013;17(2):688–699. doi: 10.1007/s10461-012-0231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalichman SC, Rompa D. The sexual compulsivity scale: further development and use with HIV-positive persons. J Personal Assess. 2001;76:379–395. doi: 10.1207/S15327752JPA7603_02. [DOI] [PubMed] [Google Scholar]
- 59.Grov C, Golub SA, Mustanski B, Parsons JT. Sexual compulsivity, state affect, and sexual risk behavior in a daily diary study of gay and bisexual men. Psychol Addict Behav. 2010;24(3):487. doi: 10.1037/a0020527. [DOI] [PubMed] [Google Scholar]
- 60.Barlow DH, Farchione TJ, Fairholme CP, et al. Unified protocol for transdiagnostic treatment of emotional disorders: therapist guide. New York: Oxford University Press; 2011. [Google Scholar]
- 61.Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2004;26(1):41–54. [Google Scholar]
- 62.Radloff LS. The CES-D scale. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 63.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State worry questionnaire. Behav Res Ther. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 64.Bentley KH, Gallagher MW, Carl JR, Barlow DH. Development and validation of the Overall Depression Severity and Impairment Scale. Psychol Assess. 2014;26(3):815–830. doi: 10.1037/a0036216. [DOI] [PubMed] [Google Scholar]
- 65.Norman SB, Hami Cissell S, Means-Christensen AJ, Stein MB. Development and validation of an overall anxiety severity and impairment scale (OASIS) Depress Anxiety. 2006;23(4):245–249. doi: 10.1002/da.20182. [DOI] [PubMed] [Google Scholar]
- 66.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 67.Allensworth-Davies D, Cheng DM, Smith PC, Samet JH, Saitz R. The short inventory of problems—modified for drug use (SIPDU): validity in a primary care sample. Am J Addict. 2012;21(3):257–262. doi: 10.1111/j.1521-0391.2012.00223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported ethanol consumption. In: Allen J, Litten RZ, editors. Measuring alcohol consumption: psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 69.Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68(1):134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 70.Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the timeline followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDS. 2001;12(6):365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Velasquez MM, von Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: a randomized clinical trial. J Consult Clin Psychol. 2009;77(4):657. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Parsons JT, Kowalczyk WJ, Botsko M, Tomassilli J, Golub SA. Aggregate versus day level association between methamphetamine use and HIV medication non-adherence among gay and bisexual men. AIDS Behav. 2013;17(4):1478–1487. doi: 10.1007/s10461-013-0463-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Grov C, Rendina HJ, Ventuneac A, Parsons JT. Brief report: partners met via sex parties present significantly greater odds for condomless anal sex among MSM: an event-level analysis of venues where male partners are met. JAIDS. 2014;67(5):564–568. doi: 10.1097/QAI.0000000000000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rendina HJ, Moody RL, Ventuneac A, Grov C, Parsons JT. Aggregate and event-level associations between substance use and sexual behavior among gay and bisexual men: comparing retrospective and prospective data. Drug Alcohol Depend. 2015;154:199–207. doi: 10.1016/j.drugalcdep.2015.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Grov C, Rendina HJ, Moody RL, Ventuneac A, Parsons JT. HIV serosorting, status disclosure, and strategic positioning among highly sexually active gay and bisexual men. AIDS Patient Care STDS. 2015;29(10):559–568. doi: 10.1089/apc.2015.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rosenthal R. Meta-analytic procedures for social research. Vol. 6. Newbury Park: SAGE Publications, Incorporated; 1991. [Google Scholar]
- 77.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.CDC. Trends IN U.S. HIV Diagnoses, 2005–2014. CDC Fact Sheet. 2015 http://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-data-trends-fact-sheet-508.pdf.
- 79.Safren SA, Perry N, Blashill A, O’Cleirigh C, Ribaudo H, Mayer K. The cost and intensity of behavioral interventions to promote HIV self-care for high-risk HIV-positive MSM compared to the cost and intensity of standard HIV treatment. Arch Sex Behav. 2015;44:1833–1841. doi: 10.1007/s10508-014-0455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Crepaz N, Lyles CM, Wolitski RJ, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20(2):143–157. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- 81.The Healthy Living Project Team. Effects of a behavioral intervention to reduce risk of transmission among people living with HIV: the Healthy Living Project Randomized Controlled Study. JAIDS. 2007;44(2):213–221. doi: 10.1097/QAI.0b013e31802c0cae. [DOI] [PubMed] [Google Scholar]
- 82.Parsons JT, Golub SA, Rosof E, Holder C. Motivational interviewing and cognitive-behavioral intervention to improve HIV medication adherence among hazardous drinkers: a randomized controlled trial. JAIDS. 2007;46(4):443. doi: 10.1097/qai.0b013e318158a461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Safren SA, O’Cleirigh C, Tan JY, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28(1):1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psychol. 2012;80(3):404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]