Abstract
[Purpose] The aim of the present study was to investigate the association between sleep duration, quality and obesity in the medical students of Saudi population. [Subjects and Methods] This is a cross-sectional study carried out in 408 medical students from King Khalid University Hospitals, Riyadh, Saudi Arabia, based on well-designed questionnaire study and consent form. [Results] The results of this study revealed 39.9% of subjects perform the exercise on regular basis and 61.5% of them reduced their weight, which may be due to diet plan (52.9%) also. Only 68.6% of the subjects were affected with the weight. The maximum number of subjects was lying down after the lunch (88.2%), sitting and reading (80.1%) are prone to develop obesity in future. [Conclusion] Our study confirms sleep disturbance has affected the weight gain and the maximum number of subjects was lying down after the lunch and sitting and reading will be prone to develop obesity in future.
Key words: Sleep, Weight gain, Obesity
INTRODUCTION
The notion that inadequate of short or long sleep is a sufficient cause for overweight/obesity has been the subject of much controversy which was spurred by mixed epidemiologic evidence, with cross-sectional and longitudinal studies showing independent associations of inadequate sleep with overweight/obesity1). Both short and long sleep durations have been associated with increased risk of coronary heart disease, type 2 diabetes mellitus (T2DM) and with daytime sleepiness and waking unrefreshed. Short but not long sleep duration has been identified as a risk factor for hypertension2). Earlier studies demonstrate the association between existence overweight or obese and sleep, specifically with shortened sleep duration, poor sleep quality, later bedtimes, and variable sleep times day-to-day3,4,5,6). The purported association between obesity and sleep is not still clear7). The association between sleep duration and weight gain has been well established, although the different variables were observed in gender. The relation in men appears to be linear and negative, while in women, the relation between sleep duration and obesity risk seems to be high8).
Medical students are a unique group of young adults whose academic commitments and lifestyle can impact their sleep habits and result in sleep deprivation9). Physical activity, sleep, screen time i.e. TV viewing and eating habits are four key modifiable lifestyle behaviours that can influence body weight. Insufficient lack of sleep, viewing the TV and consumption of high calorie (sweetened) beverages are the major potential risk factors for prone of obesity10). The relationship between race, ethnicity and obesity has been shown to exist after accounting for differences in socioeconomic status11). Short sleep is the common most frequent sleep behavior inspected and associated with obesity, hyperglycemia, and adverse changes in metabolic factors. Insufficient sleep is associated with poor impulse control, risk-taking behaviors, and other cognitive and psychological deficits that may contribute to weight gain. Other reports, however, suggest that short sleep may not independently influence obesity12, 13). In general, the relationship between sleep/wake habits and the academic performance of medical students is insufficiently addressed in the literature9).
Therefore, we designed this study to investigate the association with sleep duration, quality and obesity in the medical students of Saudi population.
SUBJECTS AND METHODS
This is a cross-sectional study carried out in King Khalid University Hospitals, capital city of Saudi Arabia. The recruitment of the subjects began with the clearance of ethical approval and based on the design of the study subjects were selected from College of Medicine. Based on the questionnaire and sign of consent form, we have selected 408 students based on the sample size concluded from the earlier pilot study [Unpublished data]. The current study was explained to the students and assured that all their information will not be revealed and maintained confidentiality to all except for the publication.
We have used a standardized formula to estimate the sample size of this current study through the pilot study, which was carried out earlier by our group [Unpublished data].
The sample size was calculated based on a pilot study that was conducted among 13 medical students in College of medicine, KKUH, Riyadh.
54% of had normal values concerning their sleeping pattern, while 46% didn’t.
p=0.54
Confidence level=95%
- d (width of confidence interval)=5%
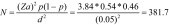
We will be collecting 400 (males and females) for better accuracy of the data.
The four-page questionnaire consist of multiple information and the students were just to click Yes or no and need to click the correct answer if the option exceed more than 4 [For example: 0, 1, 2, 3, 4 and 5]. The details of the questionnaire were as follows (i) personal information, (ii) family histories of different diseases i.e., the subjects with advanced obesity for Diabetes Mellitus, Iron deficiency anemia, Vitamin D deficiency, Hypothyroidism, Depression, Polycystic ovary syndrome, Heart disease or Stroke, Musculoskeletal disorder (osteoarthritis/joint disease), Connective tissue disease (SLE or myositis), hypogonadism, (iii) habit of smoking, caffeine (iv) exercise/diet/lose weight and (v) sleep assessment and dozing i.e. Sleep assessment was categorized (a) sleep duration (b) pattern (Quality). The duration was assessed by obtaining the average total sleeping hours in 24 hours. Quality assessed “Epworth Sleepiness Scale” (ESS) in which the subject choose how they doze off/fall asleep in different situations on daily basis time (example: sitting, reading, driving…etc.]. However, in the initial page, we have explained about the study and participant details and signature in the consent form.
The age of students has been calculated with Years and weight was measured with kilograms (kgs) and height was measured with centimeters or meter square (cms/m2). Body mass Index (BMI) was calculated with formula BMI=weight (kg)/height (cms/m2)14). The below normal weight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), obese (30.0–39.9 kg/m2), and extremely obese (40 kg/m2) was opted as per the World Health Organization criteria for BMI in our study. The BMI measurements were performed with trained women in health care centers. Height and body weight were measured without shoes and with light cloths. Height was measured to the nearest 0.5 cm and weight to the nearest 0.1 kg15).
Statistical Package for Social Sciences software was performed to carry the statistical analysis (SPSS 21.0 SPSS Inc., Chicago, IL, USA). We have performed Anova analysis to calculate the variable between 3 different groups.
RESULTS
In this cross-sectional study, we have recruited the total subjects about 408 medical students and among them 54.9% (224) participants are males and 45.1% (184) were females. The mean age of the total subjects was 20.7 ± 2.3, among this the mean age of the males and females are 20.7 ± 2.3 and 20.7 ± 2.3 respectively. The anthropometric measurements of the students were described in Table 1. The weight, height and BMI of the total students were 69.4 ± 19.1 kgs, 167.4 ± 13.4 cms and 28.52 ± 14.2. All the students were not in the underweight. The mean BMI of the male subjects are 25.3 ± 5.92 and females were 23.0 ± 4.9. When we performed the Anova analysis with the 3 variants i.e. (i) total subjects (ii) male and (iii) females we find the BMI and weight as significant association and this indicates that male subjects were more prone to proliferate the weight as well as BMI.
Table 1. Anthropometric measurements of medical students.
| S.No | Anthropometrics | Total subjects | Males | Females |
|---|---|---|---|---|
| N (%) | n=408 | n=224 | n=184 | |
| 1 | Age (years) | 20.7 ± 2.33 | 20.7 ± 2.88 | 20.8 ± 1.43 |
| 2 | Gender (male: female) | 54.9%: 45.1% | 100%: 0% | 100%: 0% |
| 3 | Weight (kg) | 69.1 ± 19.1 | 70.7 ± 18.4 | 59.4 ± 13.43 |
| 4 | Height (m2) | 167.7 ± 13.4 | 174.3 ± 6.85 | 160.5 ± 6.58 |
| 5 | BMI (kg/m2) | 28.52 ± 14.2 | 25.3 ± 5.92 | 23.0 ± 4.9 |
| 6 | Family history of DM | 07 (1.7%) | 03 (1.3%) | 04 (2.1%) |
Table 2 represents the elaborate details about exercise and diet plan. In this study, 37.2% of the participants were on regular exercise with a mean age of 5days/week for up to 2 hours. However, 56.1% of them had lost weight with exercise (37.2%) and diet (48%). The remaining 62.8% of the participants skipped the exercise due to busy schedule with college 43.6% (178) and 78 (19.1%) of them were not interested to perform the exercise. The main reason for avoiding the exercise was most of the subjects were females. However, 56.1% (229) subjects lost their weight due to exercise and diet patterns. The diet pattern was followed by 48.1% (196) subjects with the help of dietician (12.2%) and family medicine (35.9%) and remaining 51.9% (212) subjects have avoided the diet pattern to lose the weight.
Table 2. Exercise and diet details of the selected students.
| S.No | n=408 | |
|---|---|---|
| 1 | Exercise | 152 (37.2%) |
| 2 | Lose weight | 229 (56.1%) |
| 3 | Diet plan | 196 (48.0%) |
| 4 | Average sleep | 7.1 ± 1.8 |
| 5 | Day: Night | 194 (47.6%): 214 (52.4%) |
| 6 | Affected weight | 280 (68.6%) |
The mean of the sleeping time of all the subjects were 7.1 ± 1.8 and among this 52.4% sleep during night and rest of them (47.6%) sleeps during the day. However, 68.6% subjects were effected with the weight gain and rest of them i.e. 9.3% of the subjects were not affected and 22.1% of them are not sure whether they have or not affected with the weight. We have recorded the sleeping pattern assessments with the selected subjects in Table 3. The maximum number of subjects were lying down after the lunch (88.3%; p<0.05), sitting and reading (81.2%; p<0.05) are prone to develop obesity in future. The other disturbances such as sleeping in the car, besides the driver (74.8%; p<0.05), watching televisions (72.3%; p<0.05), Sitting quietly after the lunch (69.2%; p<0.05), sitting in the inactive places such as in the public places like theatre or meeting spots (64%; p<0.05), sleeping in the car for short duration of time i.e. red signal (48.3%; p<0.05) and sitting and chitchatting with others (31.4%; p<0.05).
Table 3. Sleep pattern assessments in the medical students.
| S.No | Sleep disorders | n=408 |
|---|---|---|
| 1 | Sitting and Reading | 327 (81.2%) |
| 2 | Watching Television | 295 (72.3%) |
| 3 | Sitting in the inactive places | 261 (64%) |
| 4 | Sleeping in the car (non-driver) | 305 (74.8%) |
| 5 | Lying down after lunch | 360 (88.3%) |
| 6 | Sitting and talking to others | 128 (31.4%) |
| 7 | Sitting quietly after lunch without drinks | 282 (69.2%) |
| 8 | Sleeping in the car, when signal is red | 197 (48.3%) |
The details of the family histories of recorded diseases have been characterized in Table 5. In this study, we have recorded the 14 variables of which consists of family history of the diseases as well as the common and routine habits that were prone to develop the diseases. The family history of diabetes was found to be 1.7% and the heart disease/stroke was found to be 0.7%. This data represents the lowest percentage of effecting the metabolic diseases. The maximum number of family histories in Iron deficiency anemia (12.9%), Vitamin D deficiency (38.3%) and hypothyroidism (2.2%) was found in the female subjects. Although, the family history of polycystic ovarian syndrome (8.7%) was purely recorded from the female subjects. The 8.1% of the family history was recorded as depression. The musculoskeletal and pulmonary disorders family histories were recorded as 1.9% and 12.9% respectively. The family histories of connective tissue diseases were found to be 0.2% and we could not find any family history in the hypogonadism i.e. 0%. In our study, we could find the history of caffeine as the largest family history among the studied group, which was recorded as 73.7%. The smoking history was found to be 10.5% and medication history to be 18.1%.
Table 5. Students carrying the variable family histories.
| S.No | Different family histories | Percentages |
|---|---|---|
| 1 | Medication | 18.1% |
| 2 | Caffeine | 73.7% |
| 3 | Smoking | 10.5% |
| 4 | Pulmonary disorder | 12.9% |
| 5 | Hypogonadism | 0 |
| 6 | Connective tissue disease | 0.2% |
| 7 | Musculoskeletal disorder | 1.9% |
| 8 | Heart disease/stroke | 0.7% |
| 9 | Polycystic ovarian syndrome | 8.7% |
| 10 | Depression | 8.1% |
| 11 | Hypothyroidism | 2.2% |
| 12 | Vitamin D deficiency | 38.3% |
| 13 | Iron deficiency anemia | 12.9% |
| 14 | Diabetes | 1.7% |
DISCUSSION
At present, there is no maximum information around the sleep disorders and weight gain which leads to obesity in medical students. Therefore, we carried out a cross-sectional study in KKUH with 408 medical students. The result of our study have carried out this study in medical students of KKUH and our results have revealed the positive association between lack of sleep leads to weight gain and then to obesity. The present study is in agreement with the prior studies supporting the relation between short sleep and lack of sleep with weight gain, leads to obesity8, 16,17,18). Steptoe et al.2) studied have been carried out in 17,465 university students (young adults) in 27 countries and reported that short sleep duration (<7 hours) increased the adjusted odds of poor health in both men and women, whereas no relationship was found between long sleep duration (>8 hours) and health outcomes19). Alotair et al.20) has been carried out a study differentiating between the genders in the Saudi population with obstructive sleep apnea. We found that controlling for energy balance, depression, and demographic variables did not mitigate the relationship between sleep and weight8).
This is the first study carried out in Saudi Arabia on Medical students. The correlation was connected between obesity and disturbance of sleep. Haghighatdoost et al.21) has concluded from their study that short sleepers had significantly lower diet quality indices and higher values of BMI and waist circumferences, as well as a higher percentage of obesity and abdominal adiposity compared to longer sleepers, without any significant differences in physical activity levels. Table 4 explains about the variable characters associated to develop the weight and which leads to obesity. In this table, we have shown the difference between underweight (BMI; <24.9 kg/m2), overweight (BMI; 25.0–29.9 kg/m2) and obesity (BMI; 30.0 kg/m2) with the selected parameters and compare in the 3 groups to see the difference for the development of weight gain, leads to obesity. The selected variables showed positive associations for BMI, exercise and diet pattern to lose weight, effect of watching television (p<0.05) and negative associations such as age, average sleep, effected weight, lying down after lunch and sitting in the inactive places (p>0.05). the underweight subjects have the high frequency percentage in losing the weight (30.6%) by performing the exercise (25.7%) and diet (27%) on the regular basis compare with the overweight and obese. The duration of sleeping between 5–6 hours are prone to weight gain. The obese subjects have the less activity in exercise and diet for losing the weight and the average sleep duration was found to be less and this leads to the weight gain and we can find the relation between obesity and lack of sleep in the medical students. The subjects who are failed to reduce the weight loss can follow the Melam et al.15) studies for brisk walking and aerobics. This is a king of physical therapy exercise required to carry out for minimum 10–12 weeks to reduce the weight loss.
Table 4. Association of variable forms of BMI in the medical students.
| S.No | Variables | Normal weight (n=259) |
Over weight (n=95) |
Obese (n=54) |
|---|---|---|---|---|
| 1 | Age | 20.8 ± 1.97 | 20.50 ± 3.38 | 21.14 ± 1.56 |
| 2 | Gender (M:F) | 127 (31.1): 132 (32.4) | 55 (13.5): 40 (9.8) | 42 (10.3): 12 (22.2) |
| 3 | BMI (kg/m2) | 21.08 ± 2.51 | 27.21 ± 1.42 | 34.77 ± 4.83 |
| 4 | Exercise | 105 (25.7%) | 43 (10.5%) | 15 (3.7%) |
| 5 | Lose weight | 125 (30.6%) | 76 (18.6%) | 50 (12.3%) |
| 6 | Diet plan | 70 (27) | 47 (11.5) | 27 (6.6) |
| 7 | Average sleep | 7.13 ± 2.02 | 7.11 ± 1.69 | 6.90 ± 1.55 |
| 8 | Effected weight | 1.57 ± 1.77 | 1.40 ± 0.61 | 1.87 ± 0.94 |
| 9 | Watching television | 1.05 ± 0.96 | 1.13 ± 1.78 | 1.22 ± 2.17 |
| 10 | Lying down after lunch | 1.87 ± 0.93 | 1.90 ± 2.03 | 1.94 ± 2.45 |
| 11 | Sitting in the inactive places | 0.97 ± 1.37 | 1.09 ± 1.85 | 1.05 ± 1.19 |
The current study is in agreement with the Roane et al.22) studies suggesting the future research should be studied in depth with the roles of sleep duration, sleep timing, and sleep variability and gender in weight gain (obesity). Sleep behaviors may be underlying, modifiable mechanisms that promote weight gain in different ways for men and women. Thus, more rigorous exploration into the independent, additive, and moderating roles of these modifiable mechanisms would provide valuable information to develop practical interventions for reducing weight gain, and potentially, obesity rates. The limitations of current study could be the neglecting nutritional details and we could have measure the hypertension in the medical students and this could fulfill in the future studies from our sample population. Our study concludes, sleep disturbance has affected the weight gain and the maximum number of subjects was lying down after the lunch and sitting and reading will be prone to develop obesity in future.
Conflict of Interest
None.
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research at King Saud University for its support.
REFERENCES
- 1.Jean-Louis G, Youngstedt S, Grandner M, et al. : Unequal burden of sleep-related obesity among black and white Americans. Sleep Health, 2015, 1: 169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steptoe A, Peacey V, Wardle J: Sleep duration and health in young adults. Arch Intern Med, 2006, 166: 1689–1692. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, D’Elia L, Strazzullo P, et al. : Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care, 2010, 33: 414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaput JP, Sjödin AM, Astrup A, et al. : Risk factors for adult overweight and obesity: the importance of looking beyond the ‘big two’. Obes Facts, 2010, 3: 320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hart CN, Larose JG, Fava JL, et al. : The association between time in bed and obesity risk in young adults. Behav Sleep Med, 2013, 11: 321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore M, Kirchner HL, Drotar D, et al. : Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics. Sleep Med, 2011, 12: 239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lakerveld J, Mackenbach JD, Horvath E, et al. : The relation between sleep duration and sedentary behaviours in European adults. Obes Rev, 2016, 17: 62–67. [DOI] [PubMed] [Google Scholar]
- 8.Lytle LA, Pasch KE, Farbakhsh K: The relationship between sleep and weight in a sample of adolescents. Obesity (Silver Spring), 2011, 19: 324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bahammam AS, Alaseem AM, Alzakri AA, et al. : The relationship between sleep and wake habits and academic performance in medical students: a cross-sectional study. BMC Med Educ, 2012, 12: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilkie HJ, Standage M, Gillison FB, et al. : Multiple lifestyle behaviours and overweight and obesity among children aged 9–11 years: results from the UK site of the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open, 2016, 6: e010677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boles RE, Halbower AC, Daniels S, et al. : Family chaos and child functioning in relation to sleep problems among children at risk for obesity. Behav Sleep Med, 2016, 8: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olds T, Maher CA, Ridley K: The place of physical activity in the time budgets of 10- to 13-year-old Australian children. J Phys Act Health, 2011, 8: 548–557. [DOI] [PubMed] [Google Scholar]
- 13.Sung V, Beebe DW, Vandyke R, et al. : Does sleep duration predict metabolic risk in obese adolescents attending tertiary services? A cross-sectional study. Sleep, 2011, 34: 891–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan IA, Vattam KK, Jahan P, et al. : Importance of glucokinase −258G/A polymorphism in Asian Indians with post-transplant and type 2 diabetes mellitus. Intractable Rare Dis Res, 2016, 5: 25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melam GR, Alhusaini AA, Buragadda S, et al. : Impact of brisk walking and aerobics in overweight women. J Phys Ther Sci, 2016, 28: 293–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel SR, Malhotra A, White DP, et al. : Association between reduced sleep and weight gain in women. Am J Epidemiol, 2006, 164: 947–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gangwisch JE, Malaspina D, Boden-Albala B, et al. : Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep, 2005, 28: 1289–1296. [DOI] [PubMed] [Google Scholar]
- 18.Hasler G, Buysse DJ, Klaghofer R, et al. : The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep, 2004, 27: 661–666. [DOI] [PubMed] [Google Scholar]
- 19.Pikovsky O, Oron M, Shiyovich A, et al. : The impact of sleep deprivation on sleepiness, risk factors and professional performance in medical residents. Isr Med Assoc J, 2013, 15: 739–744. [PubMed] [Google Scholar]
- 20.Alotair H, Bahammam A: Gender differences in Saudi patients with obstructive sleep apnea. Sleep Breath, 2008, 12: 323–329. [DOI] [PubMed] [Google Scholar]
- 21.Haghighatdoost F, Karimi G, Esmaillzadeh A, et al. : Sleep deprivation is associated with lower diet quality indices and higher rate of general and central obesity among young female students in Iran. Nutrition, 2012, 28: 1146–1150. [DOI] [PubMed] [Google Scholar]
- 22.Roane BM, Seifer R, Sharkey KM, et al. : What role does sleep play in weight gain in the first semester of university? Behav Sleep Med, 2015, 13: 491–505. [DOI] [PMC free article] [PubMed] [Google Scholar]


