Abstract
[Purpose] This study aimed to investigate Japanese physical therapists’ attitudes of evidence-based practice and clinical practice guidelines. [Subjects and Methods] In 2014, a cross-sectional postal mail survey using a self-administered questionnaire was conducted. Of 2,982 physical therapists belonging to the Chiba Prefecture Physical Therapist Association, 1,000 were randomly selected. The questionnaire comprised 42 items pertaining to the attitudes of and behavior toward evidence-based practice and clinical practice guidelines. It was investigated to reveal the relationship between clinical practice guidelines/evidence-based practice and therapist characteristics. [Results] The response rate was 39.6%, and 384 questionnaires were available. The main results were as follows: 83.3% participants agreed to the importance of evidence-based practice, 77.1% agree to that evidence-based practice supports clinical decision of physical therapists, and about 11% agreed to have been educated about evidence-based practice. Then, 29.2% used, 54.9% agreed to the importance of, and 13.3% agreed to the utility of clinical practice guidelines. An important factor related mostly to a positive attitude, knowledge and behavior of evidence-based practice and clinical practice guidelines was participating in research activities. [Conclusion] Many of physical therapists do not use and understand the importance of clinical practice guidelines. Participating in research activities may partially contribute to improving these conditions.
Key words: Evidence-based medicine, Clinical practice guidelines, Medical education
INTRODUCTION
Clinical practice guidelines (CPG) are defined as follows in Japan: “A clinical practice guideline is a document that presents appropriate recommendations to assist patients and practitioners in making decisions regarding clinical practice of high importance, based on the body of evidence evaluated and integrated by systematic reviews and the balance between benefits and harms.”1). Using CPG improves some clinical outcomes and process such as taking the evidence into practice2). In physical therapy, because CPG are useful as a means to facilitate evidence-based practice (EBP)3,4,5), they are expected to be increasingly used in clinical settings, improving the attitudes of EBP as a spillover effect. It therefore seems important to know the tendencies that physical therapists take attitudes of EBP and CPG, and some modifiable basic attributes of physical therapists related to attitudes of EBP and CPG.
According to the results of a survey targeting physical therapists in Sweden, the local attitudes of EBP were found to be high6,7,8), with most therapists using CPG. A similar tendency was observed among physical therapists in the U.S. in a study showing that physical therapists highly take attitudes of EBP and CPG9). Moreover, EBP knowledge and behaviors among physical therapists in various countries10) and EBP barriers, enablers and interventions11) have been studied in systematic review. These results also indicate that most of physical therapists in foreign countries make feel EBP to be facilitated and educated.
These characteristics and work environments related to attitude or behavior of implementing EBP have been more reported in previous studies. In detail, foreign physical therapists, who have insufficient time and organizational barriers, lack of computer and search skills, appraisal and application of research findings, feel barriers to implement EBP and using CPG12, 13). About basic attributes of physical therapists, individual characteristic, which includes highest degree, age, and number of years licensed, or work place environment such as number of physical therapists working at the same place and recommendation to facilitate EBP and use CPG, are related to implementing EBP14, 15) and using CPG13).
Some educational barriers have been also reported about EBP education. For example, skills of reading literatures and continuing EBP education course influences their EBP practice16). The percentage of physical therapists learning or being educated about EBP such as searching strategy, EBP training, and appraising searches is approximately 50%17). It seems for implementing EBP that academic or clinical education has important roles.
On the other hand, no data have been published for Japanese physical therapists. In Japan, continuing medical education, including both under-graduation and post-graduation, on EBP and CPG is still developing compared with that in the U.S. and European countries18). Therefore, it is worth examining and reporting the current status of Japanese physical therapists with regard to EBP and CPG to make the focus and goals of the medical education system clear.
Here we aimed to clarify the attitudes and behavior of Japanese physical therapists with regard to EBP and CPG, and basic attributes related to them.
SUBJECTS AND METHODS
A cross-sectional postal mail survey was conducted using an anonymous self-administered questionnaire.
The eligible group comprised 2,982 of 3,465 physical therapists belonging to the Chiba Prefecture Physical Therapist Association as of June 2014, excluding those belonging to an educational institution, at-home members, members of this project, and the participants of the preliminary investigation (preliminary investigation has been done in order to confirm the accuracy of questionnaires). Among the eligible participants, 1,000 were randomly selected using a table of random numbers. In addition, it was confirmed that the attributes of the members of the Chiba Prefecture Physical Therapist Association were not largely biased compared with the national average.
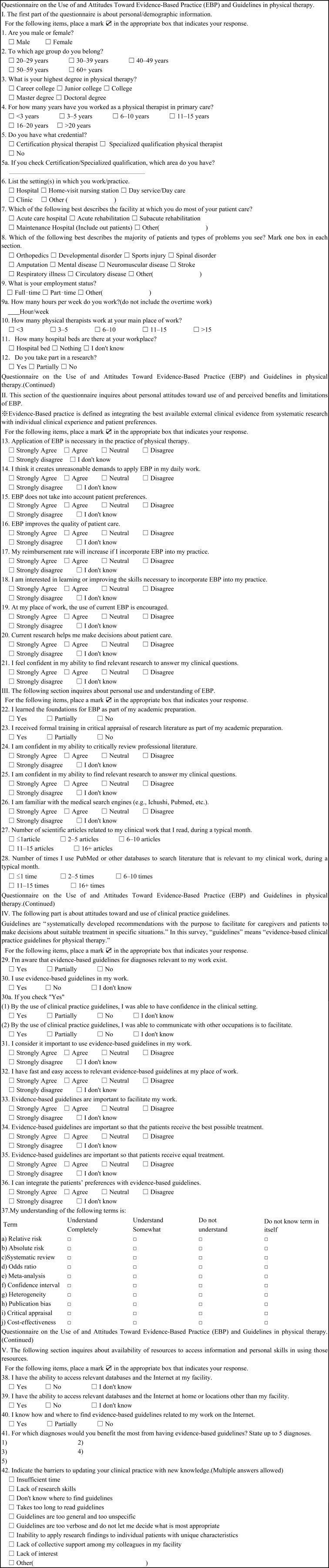
The collection time limit was set as 2 weeks after distribution, and reminders were sent 1 week after the distribution. We included questions used in previous studies6,7,8,9) (Appendix Table 1) that its validation and reliability was confirmed, according to the following process: forward translation by the authors into Japanese, backward translation by an experienced translator, and discussion and modification as appropriate to maintain compatibility and adopt cross-cultural factors (e.g certification, available database in Japan). Average time was about 30 min to fill out the questionnaire. The reliabilities were examined preliminary for ten Japanese participants before the survey, revealing an interclass correlation coefficient of 0.89–0.92 for 2 weeks and 0.91–0.96 for 1 month, which confirmed adequate reproducibility for items 13–42.
The questionnaire comprised 42 items: basic attributes of the respondent (items 1–12), attitudes of EBP (items 13–21), EBP education (items 22–23), EBP-related behavior (items 24–28), attitudes of CPG (items 29–36), knowledge of EBP and CPG (item 37; a–j), CPG-related behavior (items 38–41), and obstacles in using CPG (item 42). Some questions were also included in addition to the previous studies because following questions seem to be related to attitudes and behavior of EBP16, 17) and CPG: “whether you are engaged in research activities,” “whether your confidence in clinical decision making has increased by the use of CPG of the treatment,” and “whether communication with other health care professionals has increased/improved by using CPGs”.
The Likert scale (3-point scale for “Yes,” “Partially,” and “No” and 5-point scale for answers ranging from “Strongly agree” to “Strongly disagree”) was used. As for answers involving frequency numbers, scales were set in reference to previous studies.
Data analysis was done with the statistics software JMP.Pro11 (SAS Institute Inc., Cary, NC, USA). Descriptive statistics was used to analyze the frequency and distribution of questionnaire answers. Univariate logistic regression analysis was used to clarify the relevance of related items between EBP/CPG and basic attributes and to identify. Answers were dichotomized according to previous studies6, 9, 16) prior to performing the logistic regression analysis. With regard to the analysis of the results of the 5-point Likert scale, the answers “Strongly agree” and “Agree” were classified into an “Agree group,” whereas the answers “Neutral,” “Disagree,” and “Strongly disagree” were classified into a “Disagree group”; with regard to the analysis of the results of the 3-point Likert scale, answers were divided into “Yes” and “Other.” As for the basic attributes, an educational background of “master” or “doctor” was unified as “master or doctor.” As for years of experience, “16–20 years” and “21 years or more” were grouped as “16 years or more.” The answer “I don’t know” or missing values (not noted) were excluded from the examination.
The significance level was set at 5%. For models identified as significant in the logistic regression analysis, statistical significance was tested using the 95% confidence interval (CI) of the odds ratio.
The study was approved by Kyoto University Graduate School and Faculty of Medicine, Ethics Committee (No. E2266). We explained the study using cover letter sentences, and it was considered to agree if the participants anonymously responded.
The study was subsidized by the Health, Labour and Welfare-supported “study on clinical practice guidelines forming the base of medical care to fulfill social responsibilities” and the general, incorporated association Chiba Prefecture Physical Therapist Society.
RESULTS
Among the 1,000 people included, 396 responded to the questionnaire (response rate, 39.6%), and 384 questionnaires were available for analysis. Table 1 shows the attributes and work environments of the respondents. The percentages of certified physical therapists and specialized qualified physical therapists are interpreted to be general in Japanese physical therapists, which averages are 1% and 2% each in the whole country.
Table 1. Demographics and workplace characteristic (N=384).
| Item | Value |
|---|---|
| Gender | Male: 64%, Female: 36% |
| Age | 20–29 years: 43%, 30–39 years: 38%, 40–49 years: 16%, 50–59 years: 3%, 60+ years: 0% |
| Highest degree | Career college: 68%, College: 29%, Master degree: 2%, Doctoral degree: 1% |
| Primary care experience | <3 years: 17%, 3–5 years: 26%, 6–10 years: 31%, 11–15 years: 15%, 16+ years: 10% |
| Certification/Specialized qualification | *Certification physical therapist: 3%, Specialized qualification physical therapist: 1% |
| Work practice (Total number) | Hospital: 256, Home-visit nursing station: 9, Day service/Day care: 56, Clinic: 74, Other: 30 |
| Patient care (Total number) | Acute care hospital: 165, Acute rehabilitation: 82, Subacute rehabilitation: 141, Maintenance Hospital: 216, Other: 11 |
| Number of people at workplace | <3: 23, 3–5: 65, 6–10: 85, 11−15: 54, 15+: 160 |
| Hospital bed (Av ± SD) | 220 ± 172 hospital beds |
Av: average, SD: standard deviation. *Physical therapists can be certification physical therapists by clinical experiences and paper-tests in Japan. Moreover, certification physical therapists can be specialized qualification physical therapist by earning points of paper productions etc.
Table 2 shows attitudes and behavior toward EBP. Regarding the question about attitudes and behavior toward EBP, proportion of respondents answering “Strongly agree” or “Agree” on EBP is indicated for more than 83.3% about importance of EBP, 77.1% about decision support, and 83.3% about necessity of knowledge acquisition. On the other hand, less than 50% answered “Strongly agree” or “Agree” to the questions such as “Is introducing EBP patients’ preference?” (39.0%), “Is available papers enough to support a clinical question?” (13.2%) and “Will EBP improve cost-effectiveness?” (43.0%). As for the question regarding EBP education, 10.4% respondents answered “Yes” to the question “I learned the foundations for EBP as part of my academic preparation.”, and 11.2% respondents answered “Yes” to the question “I received formal training in critical appraisal of research literature as part of my academic preparation.” In addition, with regard to the question concerning their own confidence in EBP behavior, such as taking the view that performing literature searches and reviews is important for EBP, approximately 10–25% answered “Agree.”
Table 2. The percentage of EBP items (N=384).
| Item No. | Agree or Yes group (%) | Disagree or Other group (%) |
|---|---|---|
| 13 | 83.3 | 12.2 |
| 14 | 77.1 | 15.6 |
| 15 | 39.1 | 51.6 |
| 16 | 74.5 | 20.6 |
| 17 | 43.0 | 45.8 |
| 18 | 83.3 | 13.5 |
| 19 | 26.0 | 65.4 |
| 20 | 13.3 | 78.9 |
| 21 | 22.9 | 71.9 |
| 22 | 10.4 | 89.6 |
| 23 | 11.2 | 88.8 |
| 24 | 9.6 | 87.5 |
| 25 | 24.2 | 73.7 |
| 26 | 13.5 | 84.9 |
| 27 | 79.2 | 20.8 |
| 28 | 80.2 | 19.8 |
Agree group: “Strongly agree” and “Agree” Disagree group: “Strongly disagree”, “Disagree”, and “Neutral” Yes group: “Yes”, Other group: “No” and “Neutral” Item No. refers to Appendix.
The relationships between EBP items and basic attributes were seen as follow. Either “Taking part in a study”, “Number of people at workplace”, “Primary care experience”, “Certification/Specialized qualification”, “Highest degree”, or “Sex” was positively associated with almost all questions. Table 3 shows the relationships between attitudes and behavior of EBP and whether participating in research activities, which is more basic attributes related to attitudes and behavior of EBP than others. Physical therapists engaged in research activities were more prone to answering “Yes” to questions on education and behavior of EBP compared with those not engaged in research: The recommendation of EBP in the workplace (OR=6.50, 95% CI=3.16–13.57), education using EBP (OR=6.36, 95% CI=2.62–15.19), education using critical appraisal of academic literature (OR=5.29, 95% CI=2.30–11.93), confidence in terms of extracting a meaning of a treatise (OR=8.53, 95% CI=3.70–19.73), ability to perform a literature search on a clinical question (OR=5.23, 95% CI=2.60–10.71), and familiarity using a medicine search site (OR=7.08, 95% CI=3.31–15.14).
Table 3. Attitudes and behavior of evidence-based practice (EBP) related to participating in research activities.
| Item | Level | Odds Ratio (95% CI) | N |
|---|---|---|---|
| 17. My reimbursement rate will increase if I incorporate EBP into my practice. | Yes | 1.47 (0.70–3.17) | 341 |
| Partially | 0.5 (0.3–0.9)* | ||
| No | Reference | ||
| 19. At my place of work, the use of current EBP is encouraged. | Yes | 6.50 (3.16–13.57)* | 351 |
| Partially | 6.45 (3.69–11.44)* | ||
| No | Reference | ||
| 21. I feel confident in my ability to find relevant research to answer my clinical questions. | Yes | 1.43 (0.67–2.91) | 364 |
| Partially | 0.51 (0.25–0.96)* | ||
| No | Reference | ||
| 22. I learned the foundations for EBP as part of my academic preparation. | Yes | 6.36 (2.62–15.19)* | 384 |
| Partially | 3.11 (1.42–6.77)* | ||
| No | Reference | ||
| 23. I received formal training in critical appraisal of research literature as part of my academic preparation. | Yes | 5.29 (2.30–11.93)* | 384 |
| Partially | 1.72 (0.77–3.70) | ||
| No | Reference | ||
| 24. I am confident in my ability to critically review professional literature. | Yes | 8.53 (3.70–19.73)* | 373 |
| Partially | 1.31 (0.49–3.20) | ||
| No | Reference | ||
| 25. I am confident in my ability to find relevant research to answer my clinical questions. | Yes | 5.23 (2.60–10.71)* | 376 |
| Partially | 1.33 (0.73–2.35) | ||
| No | Reference | ||
| 26. I am familiar with the medical search engines (e.g., Ichushi, PubMed, etc.) | Yes | 7.08 (3.31–15.14)* | 378 |
| Partially | 1.22 (0.54–2.59) | ||
| No | Reference | ||
| 27. Number of scientific articles related to my clinical work that I read, during a typical month. | Yes | 11.77 (5.66–25.43)* | 384 |
| Partially | 2.10 (1.13–3.84)* | ||
| No | Reference | ||
| 28. Number of times I use PubMed or other databases to search literature that is relevant to my clinical work, during a typical month. | Yes | 17.10 (8.02–38.50)* | 384 |
| Partially | 2.12 (1.11–4.00)* | ||
| No | Reference |
* p<0.05. 95%CI: 95% confidence interval, N: number of respondents
Furthermore, as modifiable basic attributes, a higher number of people in the workplace and higher educational background were positively associated with the items pertaining to the attitudes of and behavior toward EBP. As not modifiable variables, sex was related to them.
Number of people in the workplace significantly contributes attitudes and behavior for EBP as follows: less than 3 physical therapists in workplace was more prone to disagree “Number of scientific articles related to my clinical work that I read, during a typical month.” (OR=0.01, 95%CI=0.00–0.28), and “Number of times I use PubMed or other databases to search literature that is relevant to my clinical work, during a typical month.” (OR=0.01, 95%CI=0.00–0.32). From three to five physical therapists in workplace was more prone to disagree “EBP improves the quality of patient care.” (OR=0.26, 95%CI=0.13–0.51), and “Number of scientific articles related to my clinical work that I read, during a typical month.” (OR=0.35, 95%CI=0.14–0.77). From three to five and from six to ten physical therapists in workplace were more prone than more than 15 physical therapists to disagree “At my place of work, the use of current EBP is encouraged” (3–5 physical therapists: OR=0.20, 95%CI=0.07–0.45, 6–10 physical therapists: OR=0.40, 95%CI=0.21–0.76), “I learned the foundations for EBP as part of my academic preparation.” (3–5 physical therapists: OR=0.08, 95%CI=0.00–0.36, 6–10 physical therapists: OR=0.17, 95%CI=0.04–0.51), and “I received formal training in critical appraisal of research literature as part of my academic preparation.” (3–5 physical therapists: OR=0.01, 95%CI=0.05–0.15, 6–10 physical therapists: OR=0.42, 95%CI=0.16–0.97). From six to ten physical therapists in workplace were more prone than more than 15 physical therapists to disagree “I am familiar with the medical search engines (e.g., Ichushi, Pubmed, etc.)”.
Similarly, a higher educational background such as whether what last degree is and what sort of school participants graduated is significantly associated with attitudes and behavior for EBP as follows (all p<0.05): “I received formal training in critical appraisal of research literature as part of my academic preparation.”, “Current research helps me make decisions about patient care.”, “At my place of work, the use of current EBP is encouraged.”, “I am confident in my ability to critically review professional literature.”, “I am confident in my ability to find relevant research to answer my clinical questions.”, “I am familiar with the medical search engines (e.g., Ichushi, Pubmed, etc.)”, “Number of scientific articles related to my clinical work that I read, during a typical month.”, and “Number of times I use PubMed or other databases to search literature that is relevant to my clinical work, during a typical month.”.
Then, attitude and behavior toward CPG and obstacles in using it was resulted below. 29.2% respondents used CPG and 54.9% of them agreed to the answer that “CPG is important”. Moreover, 13.3% respondents agreed to the clinical usefulness of CPG (Table 4).
Table 4. The percentage of CPG items (N=381).
| Item No. | Agree or Yes group (%) | Disagree or Other group (%) | Item No | Agree or Yes group (%) |
|---|---|---|---|---|
| 29 | 40.1 | 59.1 | 42a | 38.8 |
| 30 | 29.2 | 70.1 | 42b | 45.3 |
| 30 (1) | 26.3 | 72.9 | 42c | 23.4 |
| 30 (2) | 18.8 | 80.5 | 42d | 43.8 |
| 31 | 54.9 | 35.4 | 42e | 41.7 |
| 32 | 76.3 | 15.1 | 42f | 38.3 |
| 33 | 13.3 | 72.9 | 42g | 39.8 |
| 34 | 45.3 | 44.3 | 42h | 16.1 |
| 35 | 56.0 | 33.1 | 42i | 15.6 |
| 36 | 15.1 | 64.8 | 42j | 11.2 |
| 37a | 5.2 | 70.8 | ||
| 37b | 7.6 | 69.3 | ||
| 37c | 8.6 | 66.1 | ||
| 37d | 4.2 | 72.7 | ||
| 37e | 6.8 | 60.4 | ||
| 37f | 6.3 | 65.6 | ||
| 37g | 0.3 | 54.7 | ||
| 37h | 3.1 | 56.3 | ||
| 37i | 6.8 | 70.3 | ||
| 37j | 11.7 | 69.8 | ||
| 38 | 70.1 | 29.7 | ||
| 39 | 62.8 | 37.0 | ||
| 40 | 22.1 | 77.3 | ||
Agree group: “Strongly agree”and “Agree” Disagree group: “Strongly disagree”, “Disagree”, and “Neutral”. Yes group: “Yes”, Other group: “No” and “Neutral” Item No. refers to Appendix.
The relationship between the questions on CPG and basic attributes of the respondents has been shown about almost items. Table 5 shows the relationships between attitudes and behavior of EBP and whether participating in research activities, which is related to many of attitudes and behavior of EBP. Physical therapists engaged in research activities were more prone to answering “Yes” to the items related to the attitudes of and behavior toward CPG than those not engaged in research: Being aware of CPG (OR=2.34, 95% CI=1.19–4.72), using CGP (OR=3.02, 95% CI=1.47–6.32), integrating patients’ preferences with CPG (OR=2.93, 95% CI=1.31–6.43), being able to access clinical databases at their workplace (OR=3.22, 95% CI=1.22–11.11), and knowing how to search for CPG on the internet (OR=2.75, 95% CI=1.32–5.61).
Table 5. Attitudes and behavior of clinical practice guidelines (CPG) related to participating in research activities.
| Item | Level | Odds Ratio (95% CI) | N |
|---|---|---|---|
| 29. I am aware that evidence-based guidelines for diagnoses relevant to my work exist. | Yes | 2.34 (1.19–4.72)* | 381 |
| Partially | 1.04 (0.63–1.72) | ||
| No | Reference | ||
| 30. I use evidence-based guidelines in my work. | Yes | 3.02 (1.47–6.32)* | 335 |
| Partially | 1.68 (0.96–2.91) | ||
| No | Reference | ||
| 36. I can integrate the patients’ preferences with evidence-based guidelines. | Yes | 2.93 (1.31–6.43)* | 307 |
| Partially | 0.45 (0.18–1.00) | ||
| No | Reference | ||
| 38. I have the ability to access relevant databases and the internet at my facility. | Yes | 1.33 (0.60–3.27) | 347 |
| Partially | 2.68 (1.35–5.83)* | ||
| No | Reference | ||
| 39. I have the ability to access relevant databases and the internet at home or locations other than my facility. | Yes | 3.22 (1.22–11.11)* | 335 |
| Partially | 0.62 (0.36–1.10) | ||
| No | Reference | ||
| 40. I know how and where to find evidence-based guidelines related to my work on the internet. | Yes | 2.75 (1.32–5.61)* | 380 |
| Partially | 1.58 (0.88–2.78) | ||
| No | Reference |
* p<0.05. 95%CI: 95% confidence interval, N: number of respondents
In addition, a higher number of people at the workplace and a higher educational background were positively related with the attitudes of and behavior toward CPG as modifiable variables, and sex and years of experiences as not modifiable variables.
Number of people in the workplace significantly contributes attitudes and behavior for EBP as follows: less than 3 physical therapists in workplace was more prone to disagree “I have the ability to access relevant databases and the internet at my facility.” (OR=0.20, 95%CI=0.07–0.54). From three to five physical therapists in workplace was more prone to disagree “I am aware that evidence-based guidelines for diagnoses relevant to my work exist.” (OR=0.50, 95%CI=0.27–0.91), “I use evidence-based guidelines in my work.” (OR=0.49, 95%CI=0.24–0.97), “I have the ability to access relevant databases and the internet at my facility.” (OR=0.23, 95%CI=0.11–0.47), and “I know how and where to find evidence-based guidelines related to my work on the internet.” (OR=0.32, 95%CI=0.12–0.76). From six to ten physical therapists in workplace were more prone than more than 15 physical therapists to disagree “I am aware that evidence-based guidelines for diagnoses relevant to my work exist.” (OR=0.38, 95%CI=0.21–0.66), and “Evidence-based guidelines are important so that patients receive equal treatment.” (OR=0.32, 95%CI=0.18–0.57).
A higher educational background such as whether what last degree is and what sort of school participants graduated is significantly associated with attitudes and behavior for EBP as follows (all p<0.05): “I am aware that evidence-based guidelines for diagnoses relevant to my work exist.”, “I use evidence-based guidelines in my work.”, and “I know how and where to find evidence-based guidelines related to my work on the internet.”
DISCUSSION
This is the first survey on the attitudes and behavior toward EBP and CPG of Japanese physical therapists. We found that thoughts on EBP are partially shared, but appropriate use of CPG is not shared among these therapists and that only few of the study individuals received EBP education.
The attitudes of EBP and CPG among Japanese physical therapists are low compared with that among foreign therapists6,7,8,9). This may be because EBP education systems have not been developed in Japan. In fact, the results of the present study indicate that physical therapists that have mastered or doctoral degree and certified/specialized qualification (Japanese physical therapists first graduate school and qualified. After that, they proceed to gradable certified system, certified physical therapists, and specialized physical therapist.). At only bachelor degree, students are not almost taught what is evidence or how to use guideline. Moreover, there are not physical therapists in clinical setting who can teach what EBP is or spend time to teach it. In order to spend time to teach, number of people in workplace needs to be increased, that is indicated by the present study which less number of people in workplace do not facilitate attitudes and behavior toward EBP or CPG. Also, previous studies have reported that postgraduate EBP education improves the conviction and attitudes of EBP9, 16, 19). Therefore, postgraduate EBP education is important for physical therapists to be able to implement EBP. However, the present study showed that only 10% of the respondents received EBP education.
It is especially interesting in the present study that “being engaged in research” was related to most questions on EBP and CPG. To put research evidence into practice, we need to know the existing evidence and how to use it in reality13, 20, 21). Because the educational systems of physical therapists in Japan are not established, the one way to know and use the evidence may be to take part in research activities, which may improve practice in turn. This study revealed that approximately 10% of the respondents engaged in research activities, a figure increasing to approximately 30% if those who are only partly engaged in are included. This suggests that that patients have been provided the quality of physical therapy becomes uniform unless 70% of physical therapists who are not engaged in research activities do not raise their attitudes of EBP and CPG. Thus, education that includes research activities appears critical to raising attitudes toward EBP and CPG.
This study has some limitations. First, there may be bias due to the nature of the self-administered questionnaire survey. Therefore, the attitudes of EBP and CPG may have been overestimated. Second, comparison of the present results with those from other countries should be performed with caution because the validation of the questionnaire has not been completed; validation is important, despite the careful translation process. Third, any causality of the relation between research experience and a positive attitude toward EBP cannot be determined because our findings are based on a cross-sectional survey, and high motivation of the clinicians may confound the relationship between attitude toward EBP and research experience. However, the hypothesis generated by this study should be pursued further. Fourth, the present findings are not likely to be seriously biased because the respondents were randomly sampled in a single prefecture; however, generalizability needs attention across other prefectures. Fifth, low response rate should be considered as limitation. This study gain approximately 40% response, and this rate is less than other countries (e.g. 73% in American physical therapists15) and 81% in Canadian physical therapists16)). It may influence the present results at the point that participants who have already been aware of EBP or using CPG respond to these questionnaires.
From the above, these findings implicate three policies as follows. First, in order to facilitate EBP and using CPG, work environment needs to be established such as increasing number of physical therapists in the workplace, recommending EBP, and making times to spend searching relevant research evidences. Of course, establishing these environments is hard to implement, organizations need to consider for physical therapists. Second, physical therapists need to participate in research activities. Engaging research activities may make physical therapists be aware of necessity to have attitudes toward EBP and using CPG. Third, educational systems need to be more improved as soon as possible. Education guideline from Japanese physical therapy association indicated that we need to teach EBP and how to adjust CPG for patients in clinical settings or academic preparation, but these statements are not implemented. We expect that these three policies are developed.
As for the future problems to be tackled, it can be pointed out that an intervention program should be developed to improve the attitudes, behavior, and education of EBP and CPG and that EBP promotion and CPG expansion are necessary.
Appendix
Table 1.
REFERENCES
- 1.Fukui T, Yamaguchi N: Minds handbook for clinical practice guideline development. Tokyo: Igakushoin, 2014. [Google Scholar]
- 2.Grimshaw JM, Russell IT: Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet, 1993, 342: 1317–1322. [DOI] [PubMed] [Google Scholar]
- 3.Fritz JM, Cleland JA, Brennan GP: Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Med Care, 2007, 45: 973–980. [DOI] [PubMed] [Google Scholar]
- 4.Liddle SD, David Baxter G, Gracey JH: Physiotherapists’ use of advice and exercise for the management of chronic low back pain: a national survey. Man Ther, 2009, 14: 189–196. [DOI] [PubMed] [Google Scholar]
- 5.Rutten GM, Degen S, Hendriks EJ, et al. : Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit? Phys Ther, 2010, 90: 1111–1122. [DOI] [PubMed] [Google Scholar]
- 6.Bernhardsson S, Johansson K, Nilsen P, et al. : Determinants of guideline use in primary care physical therapy: a cross-sectional survey of attitudes, knowledge, and behavior. Phys Ther, 2014, 94: 343–354. [DOI] [PubMed] [Google Scholar]
- 7.Salbach NM, Guilcher SJ, Jaglal SB, et al. : Determinants of research use in clinical decision making among physical therapists providing services post-stroke: a cross-sectional study. Implement Sci, 2010, 5: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salbach NM, Veinot P, Jaglal SB, et al. : From continuing education to personal digital assistants: what do physical therapists need to support evidence-based practice in stroke management? J Eval Clin Pract, 2011, 17: 786–793. [DOI] [PubMed] [Google Scholar]
- 9.Jette DU, Bacon K, Batty C, et al. : Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther, 2003, 83: 786–805. [PubMed] [Google Scholar]
- 10.da Silva TM, Costa LC, Garcia AN, et al. : What do physical therapists think about evidence-based practice? A systematic review. Man Ther, 2015, 20: 388–401. [DOI] [PubMed] [Google Scholar]
- 11.Scurlock-Evans L, Upton P, Upton D: Evidence-based practice in physiotherapy: a systematic review of barriers, enablers and interventions. Physiotherapy, 2014, 100: 208–219. [DOI] [PubMed] [Google Scholar]
- 12.Salbach NM, Veinot P, Rappolt S, et al. : Physical therapists’ experiences updating the clinical management of walking rehabilitation after stroke: a qualitative study. Phys Ther, 2009, 89: 556–568. [DOI] [PubMed] [Google Scholar]
- 13.Bernhardsson S, Larsson ME, Eggertsen R, et al. : Evaluation of a tailored, multi-component intervention for implementation of evidence-based clinical practice guidelines in primary care physical therapy: a non-randomized controlled trial. BMC Health Serv Res, 2014, 14: 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mikhail C, Korner-Bitensky N, Rossignol M, et al. : Physical therapists’ use of interventions with high evidence of effectiveness in the management of a hypothetical typical patient with acute low back pain. Phys Ther, 2005, 85: 1151–1167. [PubMed] [Google Scholar]
- 15.Bridges PH, Bierema LL, Valentine T: The propensity to adopt evidence-based practice among physical therapists. BMC Health Serv Res, 2007, 7: 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salbach NM, Jaglal SB, Korner-Bitensky N, et al. : Practitioner and organizational barriers to evidence-based practice of physical therapists for people with stroke. Phys Ther, 2007, 87: 1284–1303. [DOI] [PubMed] [Google Scholar]
- 17.Carter RE, Stoecker J: Descriptors of American Physical Therapy Association physical therapist members’ reading of professional publications. Physiother Theory Pract, 2006, 22: 263–278. [DOI] [PubMed] [Google Scholar]
- 18.Japanese Physical Therapy Association: http://www.japanpt.or.jp/00_jptahp/wp-content/uploads/2013/10/International_report_comparison2.pdf (Accessed Jun. 21, 2014)
- 19.Pollock AS, Legg L, Langhorne P, et al. : Barriers to achieving evidence-based stroke rehabilitation. Clin Rehabil, 2000, 14: 611–617. [DOI] [PubMed] [Google Scholar]
- 20.Menon A, Korner-Bitensky N, Kastner M, et al. : Strategies for rehabilitation professionals to move evidence-based knowledge into practice: a systematic review. J Rehabil Med, 2009, 41: 1024–1032. [DOI] [PubMed] [Google Scholar]
- 21.Tilson JK, Mickan S: Promoting physical therapists’ of research evidence to inform clinical practice: part 1—theoretical foundation, evidence, and description of the PEAK program. BMC Med Educ, 2014, 14: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]