Abstract
[Purpose] Physical therapy is an acknowledged and frequently applied method for infantile postural asymmetry. However, there is not yet sufficient evidence for its effectiveness. [Subjects and Methods] In a randomised controlled trial, the effect of Vojta therapy versus Neurodevelopmental treatment is assessed in infants with postural asymmetry. 65 infants with postural asymmetry were recruited. 37 infants aged six to eight weeks (mean 7.38) were found to be eligible and randomly assigned to two groups, with 19 receiving Vojta and 18 Neurodevelopmental treatment. Using a standardised and blinded video-based assessment, we documented restriction in head rotation and convexity of the spine in prone and supine position before and after therapy. A reduction of at least four points (range of scale 20 points) in postural asymmetry was regarded as a clinically relevant change. [Results] On average a four-point reduction was achieved in both groups within eight weeks. A mean difference (pre-post) between the groups of −2.96 points in favour of Vojta therapy was observed. [Conclusion] While both Neurodevelopmental treatment and Vojta are effective in the treatment of infantile postural asymmetry and comparably well applied by the parents, therapeutic effectiveness is significant greater within the Vojta group.
Key words: Congenital muscular torticollis, Physiotherapy, Non-invasive therapy
INTRODUCTION
Infantile postural asymmetry (far better known as congenital muscular torticollis) is characterised predominantly by asymmetric movement patterns, such as trunk convexity and unilateral restriction in head turning1,2,3). To direct the focus on the trunk, the designation “infantile postural asymmetry” is used hereafter. The expected cause of infantile postural asymmetry is an intrauterine-acquired asymmetric fixation, possibly modified by mechanisms throughout birth4, 5). The prevalence of this idiopathic form of infantile postural asymmetry is estimated to be 15–25%6,7,8).
Since 1992 infantile postural asymmetry and plagiocephaly have become more frequent2, 4) due to the launch of the back to sleep campaign to reduce the risk of sudden infant death. An incidence of 0.4−1.3% for European countries is published3). The symptomatic form due to neuromuscular and skeletal disorders is fairly rare1, 9).
Infantile postural asymmetry occurs frequently with additional asymmetric features, such as hip dislocation, subluxation of the atlanto-axial joint, shortening of the sternocleidomastoid muscle, strabism and deformational plagiocephaly3, 5, 9, 10, 13).
To allow for unrestricted symmetric movements and to prevent a fixed torticollis, scoliosis and head deformity, most infants with postural asymmetry are treated early. There are different methods with are based largely on empirical evidence and supported by few studies; they include stretching, positioning, handling, physical, manual and microcurrent therapy8, 11,12,13,14). There is also a randomised trial which supports the therapeutic efficacy of osteopathic treatment15). In many countries Neurodevelopmental treatment (NDT) and Vojta therapy are used for the treatment of infantile asymmetry3, 5, 16). However, there have not yet been any therapeutic trials in infants with postural asymmetry for these approaches.
To evaluate the efficacy of Vojta therapy versus NDT in infants with postural asymmetry, we performed a randomised controlled trial (RCT) using a standardised video-based asymmetry scale2, 17).
SUBJECTS AND METHODS
This study was carried out from 2008 to 2012 at the Centre of Developmental Neurology, Frankfurt, Germany. All local paediatricians were asked to refer infants with postural asymmetry and a post-term age of six to eight weeks. Eligible for study participation were otherwise healthy infants who had an asymmetry score of at least 12/24 points diagnosed by a paediatrician, had not yet been treated for their asymmetry and had had a pregnancy duration of at least 32 weeks2). In addition, their parents had to provide written informed consent and had to have basic knowledge of the German language. Infants with an extreme pelvic obliquity (ICD-10 M 95.5), which does not allow evaluation of the spine in the supine position, were excluded from the study. Furthermore infants were excluded from this study if they had significant underlying diseases or a treatment before or during the study according to other concepts.
The study protocol was approved by the Ethical Committee of the Martin Luther University (MLU) Halle-Wittenberg and the Hessen state chamber of physicians, Germany (approval number MC 95/2008).
A comparative study of Vojta therapy against placebo was not allowed for ethical reasons because Vojta therapy is an officially recognized treatment modality for infant asymmetry in Germany and paid by health insurance.
After written informed consent was obtained and the caregivers agreed to publication, the eligible infants were assigned to two groups using block randomisation. The sealed and sequentially numbered envelopes were not opened by the study coordinator until the family came to the first therapy session.
Infants of the first group were treated according to the Vojta method, whereas infants in the second group received elements of NDT, such as handling and positioning. Both groups were treated for 45 minutes twice a week for eight weeks at the Centre of Developmental Neurology, Frankfurt by experienced and certified Vojta and NDT physiotherapists. The parents were trained to treat their children at home. The home treatment recommended was for 20 minutes four times a day18).
Developed by Vaclav Vojta, the Vojta method is well known as reflex locomotion and can be divided into reflex crawling and reflex rolling (phases 1 and 2). By stimulating special reflex points, the physiotherapist can trigger these motor patterns. Reflex crawling is performed in a prone position, whereas reflex rolling is induced from a supine (phase 1) and side-lying (phase 2) position. During this stimulation of motor patterns, both sides of the paravertebral muscles are activated and the spine is elongated. The motor patterns can be repeated as often as needed19).
The NDT group of infants received techniques opposing their preferred posture with the aim of activating synergistic muscles. Parents were shown how to massage an infant to harmonise muscular imbalance and how to initiate special positioning during sleep, thereby antagonizing asymmetry. They were also trained to increase the prone position time during daytime (4 × 5 minutes). Further exercises in the NDT group comprised handling according to the Bobath concept, which includes recommendations for a specific positioning of the infant during everyday procedures, such as washing, feeding, picking up and laying down, in addition to the accommodation of the baby and the parental carrying20).
The primary outcome was to evaluate the therapeutic effects of the two methods and to test if Vojta therapy might be superior to NDT in reducing infant postural asymmetry.
Before and eight weeks after intervention, postural asymmetry was quantified using a standardised video-based asymmetry scale developed by Philippi et al.2, 17). Therefore a tripod with the video camera was set up at the end of treatment mat, exactly two meters above the infants. On the treatment mat, a cross was painted, in order to assess the longitudinal axis (spine) and a horizontal axis (shoulder girdle). Philippi et al. (2006:159) described: “Recording commenced with the infant’s head being held for a brief period of time in the middle supine position. A head turn was then induced by presenting noises, toys or the physiotherapist’s face, and moving them from one side to the other. After at least two turns to each side, the infant was put in the prone position with its head held for a brief time in the middle prone position, and the same procedures were repeated”2). That means, the four items of this assessment comprise convexity of the trunk and restriction in head rotation in the prone and supine position during a maximal head turn induced by optic and acoustic stimuli to the right and left side of the infants. The range of the scale is set with a maximum of 4 × 6 = 24 points for maximum asymmetry and a minimum of 4 × 1= 4 points for symmetry. For each infant, this procedure was videotaped and analysed by three experienced and trained physical therapists (Table 1), who were blinded to the therapeutic method used. The three video scorers had contact neither to the treating physical therapists nor to the parents throughout the whole study. The scorers analysed 74 videos. They did not know if the video was recorded before or after treatment and which treatment was used. The treating physical therapist and the parents were not blinded for the therapy method. The infant may be considered blinded.
Table 1. Characteristics of the physical therapists.
| PT 1 | PT 2 | PT 3 | |
|---|---|---|---|
| Gender | female | female | female |
| Age (years) | 43 | 35 | 53 |
| Experience from getting the physio license | 20 years | 12 years | 22 years |
| Receive Vojta certification | 2001 | --- | 1999 |
| Receive NDT certification | 1997 | 2008 | 1995 |
| Other certification | Castillo Morales | Systemic family therapy |
The secondary outcome was the compliance of the parents, which was ensured through two appointments a week at the treatment centre and supervision of their manual therapy skills. The parents had to be present at 12 of the 16 possible appointments at the treatment centre to avoid elimination from the study. In addition, the frequency of therapy at home and the behaviour of the infants during these treatments were evaluated with a structured parent questionnaire. The questionnaire was completed by the parents every 14 days. With this questionnaire parents were ask if the crying of their infants affected the duration and frequency of their exercises at home and if crying and behaviour changed over time.
The statistical analysis was performed with SPSS© 18.0 and an intention-to-treat-model used for the evaluation. The main thesis is tested on a statistical significance of 0.05 using a multivariate analysis of variance (MANOVA) within all three scorers over all four items. An increase or decrease of four points (out of 24) was determined to be the minimum for clinical relevance.
The changes in an infant’s behaviour were evaluated with the questionnaire through a four-point Likert scale every two weeks. A correlation analysis between therapy and screaming behaviour was performed using a contingency table and Pearson’s χ2 distribution.
The intraclass correlation coefficient for the three blinded scorers was 0.77. The estimation of the number of subjects needed for this therapy study was performed with the software nQuery Advisor and SAS/IML.
A previous study about osteopathy and infantile postural asymmetry was used as the reference for the estimation15). The group difference in the asymmetry reduction before and after treatment should be at least four points on the asymmetry scale. Based on a power of 80, a significance level of 5%, an estimated treatment effect of 4 points and a standard deviation (SD) of 3.5 points, 15 infants were needed for each group. A list of block randomisation was created with a computer-based random number generator at the Institute of Medical Epidemiology, Biometry and Informatics at MLU. An independent person sent the order of allocation in closed, opaque and numbered envelopes to the investigator, who opened them after receipt of parental consent. Because the envelopes were kept in a locked cabinet until opening, confidentiality was ensured.
RESULTS
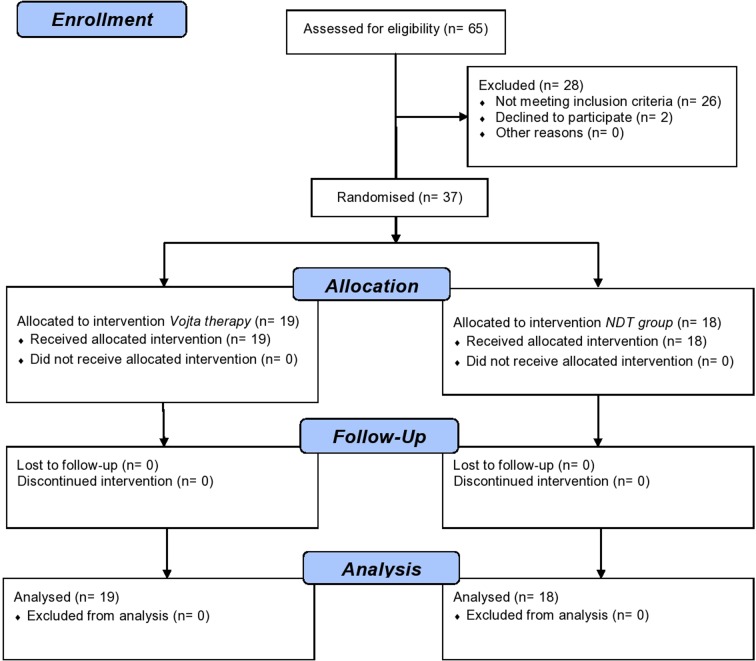
Sixty-five infants were recruited and 28 did not meet the inclusion criteria. Two parents refused to participate. Twenty-six infants exceeded maximal age of eight weeks during the referral and decision process. Thirty-seven infants were found to be eligible and randomly assigned to the two groups, 19 receiving Vojta therapy and 18 receiving NDT (Fig. 1).
Fig. 1.
CONSORT − flow diagram: order of study
Randomisation was successfully performed as shown by similar baseline criteria in both groups (Table 2). The study was conducted according to the CONSORT criteria for RCTs. There were no protocol violations, such as dropouts or change of group affiliation.
Table 2. Baseline demographic and clinical characteristics.
| Characteristics | Vojta therapy (n=19) |
NDT (n=18) |
|---|---|---|
| Mean (SD) age, weeks | 7.16 (0.77) | 7.61 (0.61) |
| Gender, male / female, n | 16 / 3 | 10 / 8 |
| Mean (SD) growth, cm | 51.50 (3.4) | 50.38 (3.3) |
| Posture awake, n | ||
| All positions | 5 | 4 |
| No prone position | 14 | 14 |
| Posture asleep, n | ||
| Supine | 17 | 12 |
| Supine, side | 2 | 4 |
| Prone | 0 | 2 |
| Parental carrying, n | ||
| <1 h / week | 2 | 1 |
| 2–6 h / week | 2 | 2 |
| 1 h / day | 15 | 12 |
| 2–4 h / day | 0 | 3 |
| Plagiocephaly, n | 16 | 9 |
| Twin birth, n | 1 | 3 |
| Mean birthweight, g (range) | 3,321 (2,360–4,390) | 3,101 (1,530–4,310) |
| Mean asymmetry score points (SD) | 18.47 (1.72) | 18.35 (2.06) |
n: subjects; SD: standard deviation; h: hours; cm: centimeter; g: gram
Within an eight-week treatment either with Vojta therapy or NDT, an average four-point reduction of postural asymmetry was achieved. The mean difference (pre-post) between both groups was −2.96 points (95% CI [−5.01; −0.91]), a statistically significant improvement in favour of Vojta therapy (p=0.025) (Fig. 2).
Fig. 2.
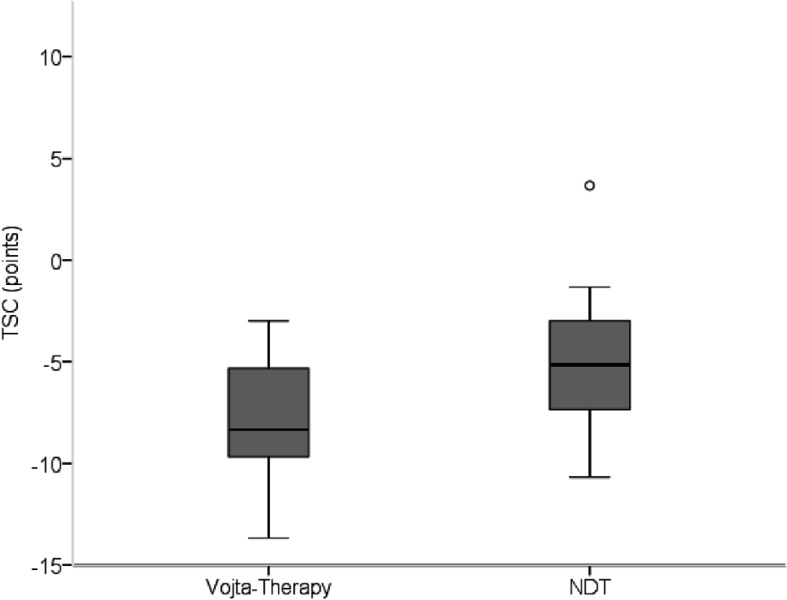
Total score difference (TSC) in the Vojta and NDT group represented as box plots. A negative TSC represents an improvement, while a positive TSC indicates deterioration. A discordant value is marked by a circle
In the Vojta group, the asymmetry score dropped from 18.47 points (SD 1.72) to 10.72 points (SD 2.77) (−7.75 points 95%CI [−6.43; −9.08]) and in the NDT group from 18.35 points (SD 2.06) to 13.56 points (SD 3.53) (−4.79 points 95%CI [−3.12; −6.47]) (Fig. 3).
Fig. 3.
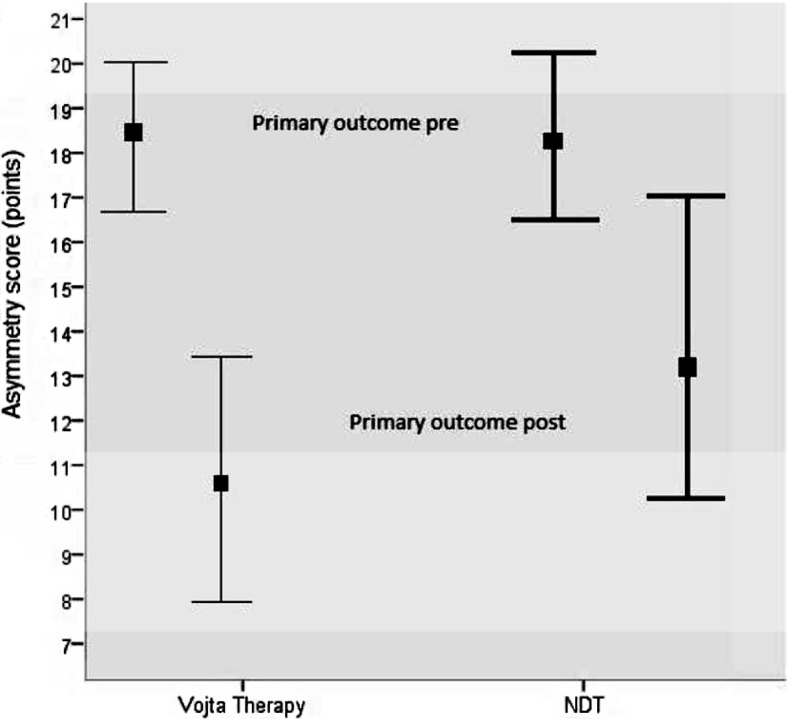
MANOVA regarding the difference in the primary outcome criteria before and after treatment (pre-post)
The changes of the supine position contributed more to the results than those of the prone position.
The mean changes were −1.18 points (p<0.001; 95% CI [−0.082; −0.840]) in head rotation supine, −0.81 points (p=0.011; 95% CI [−0.105; −0.921]) in spinal convexity supine, −0.47 points (p=0.094; 95% CI [−0.107; −0.744]) in head rotation prone and −0.50 points (p=0.230; 95% CI [−0.105; −0.610]) spinal convexity prone.
Despite the recommendations of the physical therapists to treat their infants four times a day, parents in the Vojta group treated their infants on average 2.21 times/day for 10.5 minutes. They attended on average 15.63 from 16 possible appointments with their children at the treatment centre. Parents in the NDT group treated their infants on average 2.44 times/day for 10.9 minutes. They attended on average 14.94 from 16 possible appointments at the treatment centre. Thirty-four of 37 parents (91.9%) reported similar or less frequent crying of their infant after eight-week treatment, whereas three parents (8.1%) noticed more frequent crying (one of the NDT group, two of the Vojta group).
DISCUSSION
Infantile postural asymmetry in seven-week-old infants both in the NDT group and the Vojta group showed clinically relevant improvement after an eight-week treatment interval consisting both of home treatment carried out by the parents twice a day for 10 minutes on average and the therapy at the treatment centre, which was performed twice a week for 30 minutes on average. With the same duration and frequency of treatment, there was statistically significant improvement in the Vojta group.
This study is the first RCT to show the effects of Vojta therapy and NDT on infantile postural asymmetry. The significant effect achieved through Vojta therapy compared to NDT may be explained by its more intensive muscle activation due to relatively precisely guided movement responses to triggered reflexes. In contrast, NDT allows for more variation of muscle activation; as a result, muscles which need activation may be missed because stronger muscles take over the work of weaker ones.
A further strength of our study is that outcome was measured objectively by a standardised video-based score evaluated by independent raters, who were blinded for treatment and clinical data.
Although infants cry during Vojta treatment, the acceptance of the parents in this study was good and did not influence compliance. It is assumed that crying during Vojta therapy is more likely an expression of the infant’s unwillingness to activate weak muscles rather than an expression of pain. This assumption is supported by the fact that crying stops as soon as the training ceases and by the report of parents that crying caused by pain sounds different. Parents who cannot bear the baby’s crying under Vojta therapy obtained with NDT a second, effective method but during the study period reached slightly less symmetry. Compared with other measures8, 10, 11, 14, 15) both methods show very good results.
In physical therapy, there is an ongoing discussion about the appropriate treatment intensity at home. Usually parents do less home therapy than recommended; this was also the case in our study. Nevertheless, in our study physical therapy performed twice a day for ten minutes by the parents was sufficient in order to be effective. Parents also have to perform home therapy if they apply other recommended approaches for torticollis like stretching8, 10, 11). However, stretching is sometimes a difficult experience for both parents and infants as it is often rather painful. A novel therapy, kinesiology tape14), seems to be a promising treatment option according to a first pre-post study. This approach is soft and needs no home therapy.
A limitation of our study was the restricted intervention period. It cannot be proven in the end that the natural course would not have achieved the same effect over time. A further limitation is the missing placebo group, which could not be implemented for ethical reasons. From two historical study groups (n=12 and n=16) of infants with postural asymmetry who were not be treated for 4 weeks at the age of 6–12 weeks, we know that there was a minimal change of their postural asymmetry score (± 1 point on average)15). This may indicate that initiating physical therapy is more beneficial than waiting. In the treat-or-not-to-treat debate, there are two further important clinical aspects which might offer a good argument to treat those infants early. Infants with fixed movement restriction in cervical rotation are limited in their age-related participation because they cannot explore the environment as they would like to and need to.
In untreated infants, torticollis and spine convexity may become more fixed over time and the risk of scoliosis and headaches increases. With early treatment we have the chance to relax the asymmetrically tensed-up spine muscles more easily and quickly; later on, however, the treatment of fixed torticollis, scoliosis and headache will be more extensive.
Our study supports the beneficial effect of physical therapy on infants with infantile postural asymmetry and indicates that physical therapy may be a good complement to stretching and other treatments. Our data suggest that effectiveness can be attained by ten minutes of home therapy twice a day and one 30-minute-treatment per week by the physical therapist. Our results show that therapy compliance was comparable in NDT and Vojta therapy; however, the total effect was greater in the Vojta group.
This good result of physiotherapy measures in the treatment of infantile postural asymmetry should now be examined with a greater numbers of participants, maybe in multicentre studies.
Funding
This study was partially funded by Physio Germany (German Association of Physical Therapy − ZVK e. V.).
REFERENCES
- 1.von Aufschnaiter D: Physiotherapie bei so genannter Säuglingsskoliose. In: Hüter-Becker A, Dölken M (eds.), Physiotherapie in der Pädiatrie, 2nd ed. Stuttgart: Thieme, 2010, pp 451–456. [Google Scholar]
- 2.Philippi H, Faldum A, Jung T, et al. : Patterns of postural asymmetry in infants: a standardized video-based analysis. Eur J Pediatr, 2006, 165: 158–164. [DOI] [PubMed] [Google Scholar]
- 3.Tatli B, Aydinli N, Caliskan M, et al. : Congenital muscular torticollis: evaluation and classification. Pediatr Neurol, 2006, 34: 41–44. [DOI] [PubMed] [Google Scholar]
- 4.Lessard S, Gagnon I, Trottier N: Exploring the impact of osteopathic treatment on cranial asymmetries associated with nonsynostotic plagiocephaly in infants. Complement Ther Clin Pract, 2011, 17: 193–198. [DOI] [PubMed] [Google Scholar]
- 5.Rubio AS, Griffet JR, Caci H, et al. : The moulded baby syndrome: incidence and risk factors regarding 1,001 neonates. Eur J Pediatr, 2009, 168: 605–611. [DOI] [PubMed] [Google Scholar]
- 6.Lee YT, Yoon K, Kim YB, et al. : Clinical features and outcome of physiotherapy in early presenting congenital muscular torticollis with severe fibrosis on ultrasonography: a prospective study. J Pediatr Surg, 2011, 46: 1526–1531. [DOI] [PubMed] [Google Scholar]
- 7.Petronic I, Brdar R, Cirovic D, et al. : Congenital muscular torticollis in children: distribution, treatment duration and out come. Eur J Phys Rehabil Med, 2010, 46: 153–157. [PubMed] [Google Scholar]
- 8. Öhman A, Nilsson S, Beckung E: Stretching treatment for infants with congenital muscular torticollis: physiotherapist or parents? A randomized pilot study. PM R, 2010, 2: 1073–1079. [DOI] [PubMed] [Google Scholar]
- 9.Lampe R, Mitternacht J, Gradinger R: Der angeborene muskuläre Schiefhals. 2003. Found: http://www.paediatrie-in-bildern.de/article.php?sid=12 (Accessed Dec. 30, 2012)
- 10.Cheng JC, Au AW: Infantile torticollis: a review of 624 cases. J Pediatr Orthop, 1994, 14: 802–808. [PubMed] [Google Scholar]
- 11.Kim MY, Kwon DR, Lee HI: Therapeutic effect of microcurrent therapy in infants with congenital muscular torticollis. PM R, 2009, 1: 736–739. [DOI] [PubMed] [Google Scholar]
- 12.van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, et al. : Effect of pediatric physical therapy on deformational plagiocephaly in children with positional preference: a randomized controlled trial. Arch Pediatr Adolesc Med, 2008, 162: 712–718. [DOI] [PubMed] [Google Scholar]
- 13.Bullinger HM, Sacher R, Wuttke M: Die manualmedizinische Behandlung von Haltungs- und Bewegungsasymmetrien im Säuglingsalter. Manuelle Med, 2012, 50: 401–404. [Google Scholar]
- 14.Öhman AM: The immediate effect of kinesiology taping on muscular imbalance for infants with congenital muscular torticollis. PM R, 2012, 4: 504–508. [DOI] [PubMed] [Google Scholar]
- 15.Philippi H, Faldum A, Schleupen A, et al. : Infantile postural asymmetry and osteopathic treatment: a randomized therapeutic trial. Dev Med Child Neurol, 2006, 48: 5–9, discussion 4. [DOI] [PubMed] [Google Scholar]
- 16.von Aufschnaiter D: Physiotherapie bei Torticollis am Beispiel des muskulären Schiefhalses (frühkindliche Form). In: Hüter-Becker A, Dölken M (eds.), Physiotherapie in der Pädiatrie, 2nd ed. Stuttgart: Thieme, 2010, pp 441–450. [Google Scholar]
- 17.Philippi H, Faldum A, Bergmann H, et al. : Idiopathic infantile asymmetry, proposal of a measurement scale. Early Hum Dev, 2004, 80: 79–90. [DOI] [PubMed] [Google Scholar]
- 18.Orth H: Das Kind in der Vojta-Therapie. A companion book for the practice. München: Urban & Fischer, 2005. [Google Scholar]
- 19.Vojta V, Peters A: Das Vojta Prinzip, 3rd ed. Heidelberg: Springer, 2007. [Google Scholar]
- 20.Lommel E: Handling und Behandlung auf dem Schoß: In Anlehnung an das Bobath-Konzept, 3rd ed. München: Pflaum, 2002. [Google Scholar]