Abstract
To assess the associations of obesity with newly diagnosed and previously known atopic disorders in Chinese adults. 4,629 adults aged 18 years or older were recruited in Harbin, China. Among them, 1,114 were previously diagnosed atopic cases, 1,298 were newly diagnosed cases, and 2,217 non-atopic controls. Obesity and overweight are defined according to the criteria established by the Working Group on Obesity in China. The associations of obesity with known and newly diagnosed atopic disorders were assessed using logistic regressions. Obesity was significantly associated with known atopic disorders (adjusted OR = 2.41 (95% CI: 1.81, 3.22)). The association of obesity with newly diagnosed atopic cases was not as strong as that with known cases, and was not statistically significant (adjusted OR = 1.27 (95% CI: 0.94, 1.72)). The similar pattern was observed in different allergic diseases, gender and age stratifications. The association between overweight and atopic diseases were not significant. Obesity is strongly associated with previously diagnosed atopic cases but not so with newly diagnosed atopic cases in Chinese adults. It is likely that people with atopic disorders have a higher risk of developing obesity. Our findings are important for the management of atopic disorders and chronic disease prevention among atopic disease patients.
There is a current debate on the association between obesity and atopic diseases in adults. It is still not clear if the recent epidemic of obesity has contributed to the rise in the incidence of individuals with atopic diseases or the rising incidence of atopic diseases has contributed to the increase in obesity. Some studies showed a positive association1,2,3,4 while others showed no association between obesity and atopic diseases in adults5,6. To understand the associations of obesity with those atopic diseases has important public health implications to elucidate the causal link and the importance of weight control in preventing atopic diseases. Previous studies often mixed newly diagnosed atopic cases with previously existing symptomatic cases. It is critical to separate the association of obesity with newly diagnosed atopic diseases from that with previously diagnosed atopic disease to understand the time sequence of the two events. The prevalence of obesity has been increased rapidly worldwide, particularly in low and middle income countries like China7. The incidence of atopic diseases, including atopic dermatitis, allergic rhinitis and allergic asthma, has also increased in China recently8. Therefore, understanding the association between obesity and atopic disease is particularly important for preventing and managing those conditions for this population. In this study, we assessed the associations of obesity with newly atopic disease and with previously diagnosed atopic disorders in Chinese adults.
Results
Characteristics of cases and controls
Table 1 shows the characteristics of controls, new and known atopic cases. In males, new cases and controls were different in family history while known cases were different from controls in age, weight, marital status, alcohol drinking, exercise, education, family history and the prevalence of obesity. In females, new cases and controls were different in age, residential region and cigarette smoking while known cases were different from controls in age, BMI, residential region, marital status, alcohol drinking, education, family history and the prevalence of obesity.
Table 1. Characteristics of new and known atopic cases and controls in Chinese adults.
| Control | New cases | P1 | Known cases | P1 | |
|---|---|---|---|---|---|
| Male | |||||
| Number | 613 | 433 | 390 | ||
| Age, years | 35.84 (16.91) | 34.34 (17.31) | 0.1611 | 31.96 (14.91) | 0.0002 |
| Height, cm | 167.40 (16.69) | 168.10 (17.21) | 0.4853 | 169.30 (15.57) | 0.0616 |
| Weight, kg | 66.33 (17.93) | 66.99 (19.72) | 0.5766 | 69.18 (18.67) | 0.0160 |
| BMI, kg/m2 | 23.18 (4.38) | 23.11 (4.56) | 0.8166 | 23.66 (4.54) | 0.0953 |
| Rural, n (%) | 203 (33.12) | 154 (35.57) | 0.4104 | 118 (30.26) | 0.3440 |
| Married, n (%) | 377 (61.50) | 255 (58.89) | 0.3953 | 210 (53.85) | 0.0165 |
| Cigarette smoking, n (%) | 223 (36.38) | 175 (40.42) | 0.1853 | 126 (32.31) | 0.1870 |
| Alcohol drinking, n (%) | 216 (35.24) | 149 (34.41) | 0.7826 | 104 (26.67) | 0.0045 |
| Physical exercise, n (%) | 240 (39.15) | 172 (39.72) | 0.8523 | 184 (47.18) | 0.0121 |
| Education | |||||
| Junior high school or lower | 287 (46.82) | 208 (48.04) | 0.9250 | 151 (38.72) | 0.0412 |
| Senior high school | 141 (23.00) | 98 (22.63) | 102 (26.15) | ||
| University or higher | 185 (30.18) | 127 (29.33) | 137 (35.13) | ||
| Family history, n (%) | 72 (11.75) | 70 (16.17) | 0.0398 | 176 (45.13) | <0.0001 |
| Obese, n (%) | 45 (7.34) | 38 (8.78) | 0.3977 | 58 (14.87) | 0.0001 |
| Female | |||||
| Number | 1,604 | 865 | 724 | ||
| Age, years | 38.18 (13.64) | 36.26 (14.02) | 0.0010 | 36.80 (14.52) | 0.0305 |
| Height, cm | 160.80 (7.77) | 160.20 (10.23) | 0.1360 | 160.40 (9.67) | 0.2405 |
| Weight, kg | 57.53 (10.34) | 57.04 (11.67) | 0.3051 | 58.18 (11.67) | 0.1957 |
| BMI, kg/m2 | 22.16 (3.57) | 22.04 (3.62) | 0.4136 | 22.53 (3.91) | 0.0319 |
| Rural, n (%) | 565 (35.22) | 257 (29.71) | 0.0055 | 200 (27.62) | 0.0003 |
| Married, n (%) | 1,254 (78.18) | 652 (75.38) | 0.1132 | 522 (72.10) | 0.0014 |
| Cigarette smoking, n (%) | 138 (8.60) | 53 (6.13) | 0.0280 | 50 (6.91) | 0.1641 |
| Alcohol drinking, n (%) | 93 (5.80) | 58 (6.71) | 0.3695 | 15 (2.07) | <0.0001 |
| Physical exercise, n (%) | 446 (27.81) | 258 (29.83) | 0.2886 | 206 (28.45) | 0.7474 |
| Education | |||||
| Junior high school or lower | 679 (42.33) | 348 (40.23) | 0.1698 | 270 (37.29) | 0.0022 |
| Senior high school | 448 (27.93) | 228 (26.36) | 186 (25.69) | ||
| University or higher | 477 (29.74) | 289 (33.41) | 268 (37.02) | ||
| Family history, n (%) | 223 (13.90) | 135 (15.61) | 0.2512 | 312 (43.09) | <0.0001 |
| Obese, n (%) | 62 (3.87) | 40 (4.62) | 0.3660 | 69 (9.53) | <0.0001 |
1P values comparing cases with controls.
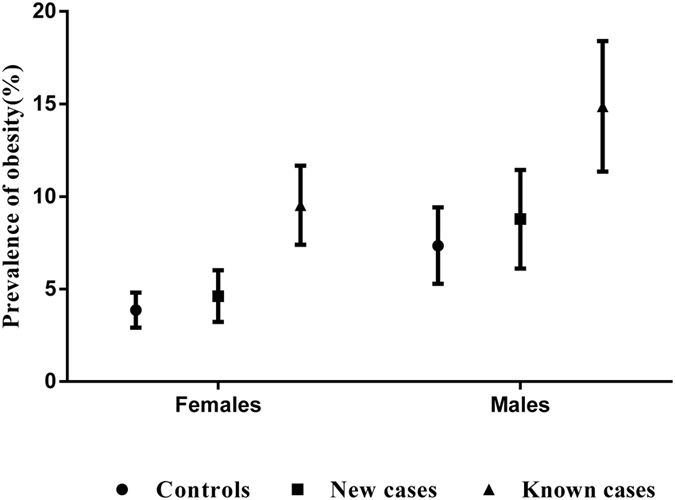
Prevalence of obesity among new and known cases and controls
Although the prevalence was lower in females than in males, the patterns of the relationships between obesity and atopic cases were the same in both genders. Both case groups had a higher prevalence of obesity than the control group. The previously known cases had a higher prevalence than the newly diagnosed case group, as shown in Fig. 1.
Figure 1. Prevalence of obesity among non-atopic controls, newly diagnosed and previously known atopic cases in Chinese adults.
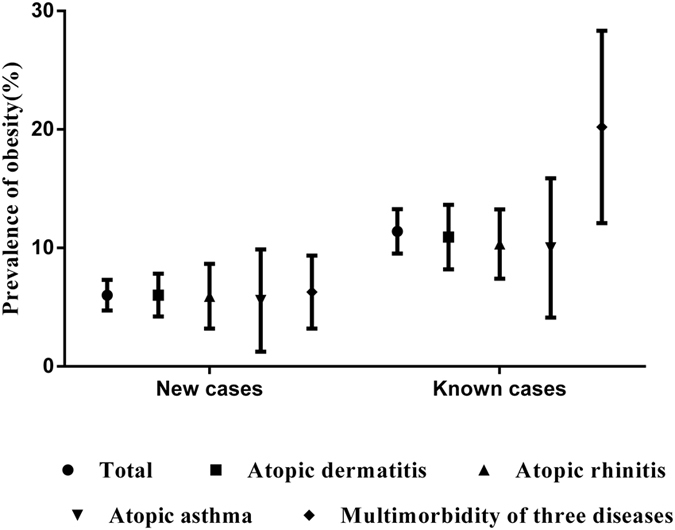
Prevalence of obesity among atopic dermatitis, atopic rhinitis, atopic asthma, and multimorbidity of three atopic diseases
Patients with different atopic diseases had different prevalence of obesity. Those with multimorbidity of three atopic diseases had a higher prevalence than the others, as shown in Fig. 2.
Figure 2. Prevalence of obesity among atopic dermatitis, atopic rhinitis, atopic asthma, and multimorbidity of three atopic diseases in Chinese adults.
Associations of obesity with newly diagnosed and previously known atopic diseases
Obesity was significantly associated with known atopic disease (crude OR = 2.54, 95% CI: 1.94, 3.32), as shown in Table 2. The association between obesity and newly diagnosed atopic disease was not significant (crude OR = 1.26, 95% CI: 0.93, 1.70). Adjusted for age, sex, education, cigarette smoking, alcohol drinking, marital status, family history of atopic diseases and physical exercise, the associations between obesity and known atopic cases remained strong and significant, adjusted OR = 2.41 (95% CI: 1.81, 3.22). The association between obesity and newly diagnosed atopic cases was weaker than that of obesity with known atopic cases, and remained non-significant, adjusted OR = 1.27 (95% CI: 0.94, 1.72). The similar patterns were observed in different allergic diseases, gender stratifications and age stratifications.
Table 2. Association of obesity with newly diagnosed and previously known atopic cases in Chinese adults.
| Cases | Obesity N (%)a | Crude | P | Adjustedb | P | |
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||||
| Newly diagnosed | Male | 433 (8.78) | 1.21 (0.77–1.91) | 0.3983 | 1.25 (0.79–1.97) | 0.3339 |
| Female | 865 (4.62) | 1.21 (0.80–1.81) | 0.3666 | 1.29 (0.85–1.94) | 0.2270 | |
| 18–39 | 775 (4.90) | 1.32 (0.85–2.05) | 0.2223 | 1.33 (0.85–2.07) | 0.2192 | |
| 40–59 | 466 (7.51) | 1.30 (0.84–2.02) | 0.2460 | 1.26 (0.81–1.97) | 0.3120 | |
| ≥60 | 57 (8.77) | 1.21 (0.39–3.78) | 0.7464 | 1.38 (0.42–4.50) | 0.5930 | |
| Atopic dermatitis | 664 (6.02) | 1.26 (0.87–1.84) | 0.2194 | 1.33 (0.91–1.95) | 0.1356 | |
| Atopic rhinitis | 287 (5.92) | 1.24 (0.73–2.10) | 0.4208 | 1.27 (0.74–2.18) | 0.3907 | |
| Atopic asthma | 108 (5.56) | 1.16 (0.50–2.70) | 0.7309 | 1.08 (0.46–2.54) | 0.8587 | |
| Multimorbidity of three atopic diseases | 239 (6.28) | 1.32 (0.76–2.31) | 0.3279 | 1.24 (0.71–2.18) | 0.4524 | |
| Total | 1,298 (6.01) | 1.26 (0.93–1.70) | 0.1303 | 1.27 (0.94–1.72) | 0.1238 | |
| Previously known | Male | 390 (14.87) | 2.21 (1.46–3.33) | 0.0002 | 2.06 (1.32–3.21) | 0.0016 |
| Female | 724 (9.53) | 2.62 (1.84–3.74) | <0.0001 | 2.64 (1.80–3.86) | <0.0001 | |
| 18–39 | 690 (10.58) | 3.02 (2.06–4.43) | <0.0001 | 2.70 (1.79–4.09) | <0.0001 | |
| 40–59 | 374 (10.96) | 1.97 (1.29–3.02) | 0.0018 | 1.89 (1.19–3.02) | 0.0073 | |
| ≥ 60 | 50 (26) | 4.41 (1.75–11.15) | 0.0017 | 5.03 (1.94–12.99) | 0.0009 | |
| Atopic dermatitis | 504 (10.91) | 2.42 (1.72–3.40) | <0.0001 | 2.29 (1.59–3.29) | <0.0001 | |
| Atopic rhinitis | 416 (10.34) | 2.27 (1.57–3.29) | <0.0001 | 2.37 (1.59–3.54) | <0.0001 | |
| Atopic asthma | 100 (10.00) | 2.19 (1.11–4.33) | 0.0240 | 2.32 (1.13–4.78) | 0.0224 | |
| Multimorbidity of three atopic diseases | 94 (20.21) | 5.00 (2.91–8.57) | <0.0001 | 5.24 (2.98–9.24) | <0.0001 | |
| Total | 1,114 (11.40) | 2.54 (1.94–3.32) | <0.0001 | 2.41 (1.81–3.22) | <0.0001 |
aN, number of cases; percentage, prevalence of obesity among atopic cases.
bAdjusted for age, sex, education, cigarette smoking, alcohol drinking, marital status, family history of atopic diseases and physical exercise.
ORs and 95% CIs for different atopic diseases in relation to BMI category
Table 3 presents the ORs and 95% CIs for different atopic diseases in relation to BMI category stratified by sex. Obesity was significantly associated with known atopic disease in both males (crude OR = 2.17, 95% CI: 1.42, 3.32) and in females (crude OR = 2.57, 95% CI: 1.80, 3.68). The association between obesity and newly diagnosed atopic disease was not significant (crude OR = 1.21, 95% CI: 0.76, 1.92 in males and OR = 1.17, 95% CI: 0.78, 1.76 in females). The associations between overweight and the two kinds of atopic diseases in both males were all not significant. Adjusted for age, sex, education, cigarette smoking, alcohol drinking, marital status, family history of atopic diseases and physical exercise, the associations between obesity and known atopic cases remained strong and significant, adjusted OR = 2.20 (95% CI: 1.38, 3.50) in males and adjusted OR = 2.67 (95% CI: 1.81, 3.91) in females. The association between obesity and newly diagnosed atopic cases was weaker than that of obesity with known atopic cases, and remained non-significant, adjusted OR = 1.29 (95% CI: 0.81, 2.06) in males and adjusted OR = 1.28 (95% CI: 0.84, 1.93) in females. The associations between overweight and the two kinds of atopic diseases in both males were still not significant.
Table 3. ORs and 95% CIs for atopic diseases in relation to BMI.
| Control N (%) | Newly diagnosed N (%) | cOR1 (95% CI) | aOR1 (95% CI) | Previously known N (%) | cOR1 (95% CI) | aOR1 (95% CI) | |
|---|---|---|---|---|---|---|---|
| Male | |||||||
| Normal | 357 (58.24) | 249 (57.51) | 1.00 (ref) | 1.00 (ref) | 212 (54.36) | 1.00 (ref) | 1.00 (ref) |
| Overweight | 211 (34.42) | 146 (33.72) | 0.99 (0.76–1.29) | 1.07 (0.81–1.42) | 120 (30.77) | 0.96 (0.72–1.27) | 1.18 (0.86–1.62) |
| Obesity | 45 (7.34) | 38 (8.78) | 1.21 (0.76–1.92) | 1.29 (0.81–2.06) | 58 (14.87) | 2.17 (1.42–3.32) | 2.20 (1.38–3.50) |
| Female | |||||||
| Normal | 1,179 (73.50) | 649 (75.03) | 1.00 (ref) | 1.00 (ref) | 510 (70.44) | 1.00 (ref) | 1.00 (ref) |
| Overweight | 363 (22.63) | 176 (20.35) | 0.88 (0.72–1.08) | 0.97 (0.78–1.20) | 145 (20.03) | 0.92 (0.74–1.15) | 1.04 (0.83–1.32) |
| Obesity | 62 (3.87) | 40 (4.62) | 1.17 (0.78–1.76) | 1.28 (0.84–1.93) | 69 (9.53) | 2.57 (1.80–3.68) | 2.67 (1.81–3.91) |
c OR, crude odds ratio; CI, confidence interval. a OR, adjusted odds ratio, adjusted for age, sex, education, cigarette smoking, alcohol drinking, marital status, family history of atopic diseases and physical exercise. 1OR values comparing cases with controls.
Discussion
In this study, we found that obesity was strongly and significantly associated with previously diagnosed atopic cases, and this association was different from that of obesity with newly diagnosed atopic cases in Chinese adults. The association of obesity with previously diagnosed existing atopic cases was much stronger than that with newly diagnosed cases, which implies it is likely that people with atopic disorders have higher risk of obesity.
In the current debate on the association between obesity and atopic diseases in adults, some studies support the presence of a positive association while others found no association between obesity and atopic diseases in adults1,2,3,4,5,6,9,10,11,12. In a study of 1,997 Canadian adults, Chen et al. found a significant association between obesity and atopic diseases with an adjusted odds ratio 1.33 (1.04, 1.71). In another study of 2,090 American adults, Silverberg et al. reported positive associations of obesity with atopic dermatitis and atopic asthma2. On the other hand, the data from Germany suggest no association between obesity and atopic diseases. The data from Australian adults showed no association between BMI and atopic diseases13. A multicentre cross-sectional survey of young adults in Europe showed that a positive association between high BMI and the risk of asthma attacks in women but there was no association between BMI and sensitization to any of allergens tested in the study6. Leung et al. showed that obesity was not associated with atopic diseases in Chinese children14. Little data are available from Chinese adults. In this study, we found that a significant association between obesity and the presence of a previously diagnosed atopic disease while a not significant association between obesity and newly diagnosed atopic diseases. Our findings are somewhat consistent with those of some previous studies of US adults2,10. Ma et al. reported no association between obesity and atopic diseases but an independent association of previously diagnosed asthma10. Silverberg et al. also found no association between obesity and atopic diseases but a significant association between obesity and symptomatic atopic dermatitis2. In this study, the atopic dermatitis, atopic rhinitis, atopic asthma, and multimorbidity of three atopic diseases were all significantly associated with obesity.
Having two sets of atopic case groups, newly diagnosed and previously diagnosed, is a unique feature in this study. A stronger association of obesity with previously diagnosed atopic cases than that with newly diagnosed atopic cases suggested that the duration of atopic cases might have played a role in the increased risk of obesity among the patients with atopic disorders. Although it is possible that the causal relationship could have existed in both directions: the presence of obesity increased the risk of atopic diseases and the presence of atopic diseases increased the risk of obesity, our data strongly support the latter. It is still not clear about why people with atopic diseases have a higher risk of obesity, but there are several possible explanations. Patients with previously diagnosed atopic diseases may be less physically active to avoid contact with allergens, and they are likely to store more energy than those without the condition. Also, some medications for treating atopic disorders may cause the patients to gain weight. Although we do not have evidence to support any of those explanations in the study population, our findings stress the importance of weight management and obesity prevention among atopic patients. Clinical guidelines for managing and treating atopic conditions should include the obesity prevention as a priority. We should also develop strategies, with appropriate choices of medications and advice on physical exercise and diet, specifically aiming to efficiently prevent obesity related chronic diseases among patient atopic disorders.
There are several strengths in this study. First, all cases and controls were confirmed by allergen-specific tests to sixteen common allergens in the region to minimise potential misclassification. Second, with two sets of different types of cases, we were able to obtain some evidence on time sequence between obesity and atopic diseases in Chinese adults.
However, there are some limitations in this study. As a case-control study, we were not able to identify exact times when either obesity or atopic diseases first occurred. Some newly diagnosed atopic cases might have had the condition for a quite a while but remained undiagnosed. Therefore, in the observed association between obesity and newly diagnosed atopic cases, obesity could have been either the cause or effect or both. Further cohort studies are needed to assess the detailed associations between obesity and atopic disorders, specifically aiming to assess if obesity increases the risk of atopic diseases in Chinese adults.
In conclusion, obesity is strongly associated with previously diagnosed atopic diseases but not so with newly diagnosed atopic disorders. Our data suggest that it is more likely that people with atopic disorders have a higher risk of obesity than that people with obesity have a higher risk of developing atopic disorders. Our findings are important for the management of atopic disorders and chronic disease prevention among atopic disease patients.
Methods
Study participants
In this case-control study, all atopic cases and controls were recruited from Harbin City in Heilongjiang Province of Northeast China. During March 2009 and December 2014, adult patients, aged 18 years or older, who visited the Department of Allergy of the First Affiliated Hospital of Harbin Medical University, were eligible for this study as potential cases. Potential controls were healthy adults who visited the same hospital for a health check-up during the same period. Potential cases and controls underwent allergen-specific IgE tests to sixteen allergens. We focused on the most common three atopic diseases, atopic dermatitis, asthma and rhinitis in this study. The current guidelines for allergic dermatitis15, rhinitis16 and asthma17 were used to diagnose them. The previously diagnosed atopic cases must meet the following criteria:
Had persistent positive IgE to at least one of the sixteen allergens in previous tests and in current test;
Had been diagnosed with at least one kind of atopic diseases mentioned above for more than one year and had also been diagnosed at this time.
Those meeting the following criteria were defined as newly diagnosed atopic cases:
Had positive IgE to at least one of the sixteen allergens in current test;
Diagnosed for the first time with at least one kind of atopic diseases mentioned above.
Multiple atopic cases were defined as those who had more than one kind of allergic diseases. Controls were those who had no previous history of atopic disease and were negative in all IgE concentrations. We conducted a questionnaire interview among 4,000 potential cases and 3,000 potential controls recruited. With the questionnaires with missing information or anomalous data excluded, we had 1,512 newly diagnosed cases, 1,297 previously diagnosed cases and 2,577 non-atopic controls. Questionnaires with logic errors and of specific populations (athletes and pregnant or breastfeeding women) were also excluded. Finally, our study included 1,298 newly diagnosed cases (664 atopic dermatitis, 287 atopic rhinitis, 108 atopic asthma, and 239 multimorbidity of three atopic diseases included), 1,114 previously diagnosed cases (504 atopic dermatitis, 416 atopic rhinitis, 100 atopic asthma, and 94 multimorbidity of three atopic diseases included) and 2,217 non-atopic controls.
Measurements
Allergen-specific IgE testing
Allergen-specific IgE in serum concentrations to sixteen most common allergens in the region were measured using the AllergyScreen system (Mediwise Analytic GmbH, Germany) in all potential cases and controls. A positive atopic sensitisation was defined if the concentration of at least one of the allergen specific IgE was 0.35 kU/l or greater. The sixteen allergens were showed in Supplementary Table S1.
Anthropometric measurements and obese
Body weight was measured to the nearest 0.1 kg using a calibrated standard scale with participants wearing light dress without shoes. Height was measured to the nearest 0.1 cm using a stadiometer. The physician who performed the anthropometric measurements did not know the nature of this study and the grouping of the study participants. Body mass index (BMI) was calculated as body weight (kg) divided by height (m) squared (kg/m2). All subjects were grouped into one of the following three groups, normal weight (BMI < 24), overweight (BMI ≥ 24 and BMI < 28) and obesity (BMI ≥ 28) according to the criteria established in 2003 by the Working Group on Obesity in China18.
Demographic, family history and lifestyle factors
A structured questionnaire interview was conducted to collect data on the characteristics of study participants. Demographic factors included sex, age, education level, residential region and marital status. Lifestyle variables included cigarette smoking, alcohol drinking and physical exercise. The data on family history of related diseases such as atopic dermatitis, atopic rhinitis and atopic asthma were also collected. Age was calculated as the difference between the year of birth and the year of interview. Educational status was categorized into three levels: junior high school or lower, senior high school, and university or higher. Residential region was categorized into two groups: urban and rural. Marital status was also categorized into two groups: unmarried and married. Current smokers were defined on the basis of the World Health Organization criteria, as those who self-reported smoking every day for at least 6 months19. Regular alcohol drinkers were defined as drinking more than twice per week for at least one year. Classification of physical exercise was defined according to the criteria which take exercise intensity, time and frequency into consideration. The details are contained in the Supplementary Method. All subjects provided written informed consent to participate in this study. This project was approved by Harbin Medical University’s Ethical Review Committee. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Data analysis
The prevalence of obesity was calculated and compared among the three groups: controls, new cases and known cases. To assess the associations of obesity with new and known atopic disorders, we estimated odds ratios (OR) and their 95% confidence intervals using logistic regressions to adjust for potential confounding factors. We used stratification analysis to assess the associations of obesity with different types of known cases. Analyses were conducted for males and females separately, and all analyses were performed using SAS 9.1 (SAS Institute Inc., Cary, NC, USA)20.
Additional Information
How to cite this article: Xie, B. et al. Associations of obesity with newly diagnosed and previously known atopic diseases in Chinese adults: a case-control study. Sci. Rep. 7, 43672; doi: 10.1038/srep43672 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
This study was funded by the National Science and Technology Major Project of the Ministry of Science and Technology of China (2016ZX08011004008).
Footnotes
The authors declare no competing financial interests.
Author Contributions M.L. and Z.W. conceived of the study and participated in its design. B.X., Y.W. and M.L. participated in the study design and conduct of data collection. B.X. and Y.W. carried out quantitative statistical analysis. All authors contributed to the writing of the manuscript and critically reviewed the final version submitted for publication. All authors read and approved the final manuscript.
References
- Chen Y., Rennie D., Cormier Y. & Dosman J. Association between obesity and atopy in adults. Int. Arch. Allergy Imm. 153, 372–377 (2010). [DOI] [PubMed] [Google Scholar]
- Silverberg J. I., Silverberg N. B. & Lee-Wong M. Association between atopic dermatitis and obesity in adulthood. Br. J. Dermatol. 166, 498–504 (2012). [DOI] [PubMed] [Google Scholar]
- Fitzpatrick S., Joks R. & Silverberg J. I. Obesity is associated with increased asthma severity and exacerbations, and increased serum immunoglobulin E in inner-city adults. Clin. Exp. Allergy 42, 747–759 (2012). [DOI] [PubMed] [Google Scholar]
- Husemoen L. L. et al. Association of obesity and insulin resistance with asthma and aeroallergen sensitization. Allergy 63, 575–582 (2008). [DOI] [PubMed] [Google Scholar]
- Flexeder C., Bruske I., Magnussen H. & Heinrich J. Association between obesity and atopy in adults? Int. Arch. Allergy Imm. 156, 117–118 (2011). [DOI] [PubMed] [Google Scholar]
- Jarvis D., Chinn S., Potts J. & Burney P. Association of body mass index with respiratory symptoms and atopy: results from the European Community Respiratory Health Survey. Clin. Exp. Allergy 32, 831–837 (2002). [DOI] [PubMed] [Google Scholar]
- Wu Y. Overweight and obesity in China. B. m. j. 333, 362–363 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asher M. I. et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 368, 733–743 (2006). [DOI] [PubMed] [Google Scholar]
- Chen Y., Rennie D., Cormier Y. & Dosman J. Atopy, obesity, and asthma in adults: the Humboldt study. J. Agromedicine 14, 222–227 (2009). [DOI] [PubMed] [Google Scholar]
- Ma J., Xiao L. & Knowles S. B. Obesity, insulin resistance and the prevalence of atopy and asthma in US adults. Allergy 65, 1455–1463 (2010). [DOI] [PubMed] [Google Scholar]
- Luo X. et al. Effect modification by gender and smoking status on the association between obesity and atopic sensitization in Chinese adults: a hospital-based case–control study. BMC Public Health 14, 1–8 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X. et al. Association between obesity and atopic disorders in Chinese adults: an individually matched case–control study. BMC Public Health 13, 1–5 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter L. M., Salome C. M., Peat J. K. & Woolcock A. J. Obesity is a risk for asthma and wheeze but not airway hyperresponsiveness. Thorax 56, 4–8 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung T. F. et al. Association between obesity and atopy in Chinese schoolchildren. Int. Arch. Allergy Imm. 149, 133–140 (2009). [DOI] [PubMed] [Google Scholar]
- Schram M. E. et al. Validation and refinement of the Millennium Criteria for atopic dermatitis. J. Dermatol. 38, 850–858 (2011). [DOI] [PubMed] [Google Scholar]
- Branch CMAoOHaNS. Guidelines for diagnosis and treatment of atopic rhinitis. Chin. J. Clin. 38, 67–68 (2010). [Google Scholar]
- Blumberg M. Z. & Jeffrey S. Frequency of Objective Criteria for the Diagnosis of Asthma in an Outpatient Allergy Practice. J. Allergy Clin. Immu. 125, AB124 (2010). [Google Scholar]
- Zhou B. F. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases—report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed. Environ. Sci. 15, 245–252 (2002). [PubMed] [Google Scholar]
- WHO. Guidelines for the Conduct of Tobacco Smoking Surveys for the General Population. In Geneva, Switzerland: World Health Organization Document WHO/SMO/83 (1983).
- StataCorp. Stata Statistical Software: Release 12. College Station, Texas: StataCorp LP (2011).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


