Abstract
The gut microbiota is an important contributor to the worldwide prevalence of metabolic syndrome (MS), which includes obesity and diabetes. The anti-MS effects exerted by Bifidobacterium animalis ssp. lactis GCL2505 (BlaG), a highly proliferative Bifidobacterium strain in the gut, and B. longum ssp. longum JCM1217T (BloJ) were comparatively examined. BlaG treatment reduced visceral fat accumulation and improved glucose tolerance, whereas BloJ had no effect on these parameters. Gut microbial analysis revealed that BlaG exerted stronger effects on the overall bacterial structure of the gut microbiota than BloJ, including enrichment of the genus Bifidobacterium. The levels of acetate and glucagon-like peptide-1 were increased by BlaG treatment in both the gut and plasma, but not by BloJ treatment. Correlation analysis suggested that the elevation of gut acetate levels by BlaG treatment plays a pivotal role in the BlaG-induced anti-MS effects. These findings indicated that BlaG, a highly viable and proliferative probiotic, improves metabolic disorders by modulating gut microbiota, which results in the elevation of SCFAs, especially acetate.
Lifestyle changes such as the increased consumption of high-energy foods have greatly contributed to the global prevalence of metabolic syndrome (MS), which includes obesity and diabetes. Recent interest in the gut microbiota has reinforced the concept that our colonic bacteria may not simply reflect lifestyle choices such as diet, but they can also influence energy metabolism. In human and mouse studies, the gut microbiota in obese subjects was characterised by larger populations of Firmicutes and smaller populations of Bacteroidetes as well as a reduction in microbial diversity1. Moreover, a high-fat diet (HFD) in mice disrupts intestinal integrity, which exacerbates MS via adipose inflammation2,3,4. Thus, modulation of the gut microbiota is considered an emerging strategy for controlling body weight and insulin sensitivity4,5,6,7.
Indigestible carbohydrates derived from the diet are fermented by the gut microbiota and then finally converted to short-chain fatty acids (SCFAs), such as acetate, propionate and butyrate. SCFAs are absorbed via the colonic epithelium, and acetate—the most abundant SCFA—achieves concentrations of 19–160 μM in peripheral blood, whereas propionate and butyrate reach 1–13 μM and 1–12 μM8, respectively. Recently, it was revealed that SCFAs have distinct actions relevant to energy homoeostasis in addition to serving as host energy sources. Acetate activates GPR43, a G-protein-coupled receptor (GPCR), on adipocytes and suppresses insulin signalling, which inhibits fat accumulation in adipocytes and promotes the metabolism of unincorporated lipids and glucose in other tissues9. In addition, it reduces appetite through a central hypothalamic mechanism10, and pancreatic GPR43 signalling potentiates β-cell function11. Furthermore, Tolhurst et al.12 revealed that GPR43 on intestinal L-cells is stimulated by SCFAs, and induces the secretion of glucagon-like peptide-1 (GLP-1), a gut-derived peptide known to modulate satiety and glucose homoeostasis13,14.
Probiotics are defined as ‘live microorganisms that, when administered in adequate amounts, confer a health benefit on the host’15, and Bifidobacterium and Lactobacillus spp. are representative examples of such probiotic microorganisms. Several probiotics and their mixture have been reported to improve MS16,17,18,19,20. In some of these reports, several probiotics were found to improve MS by modulating the composition of the gut microbiota or its metabolites16,18. However, very few studies have comprehensively investigated the effects of probiotics on the composition of the gut microbiota, its metabolites, and host metabolic parameters. Furthermore, the properties of probiotics involved in these effects remain unclear.
Thus, the present study investigated the effects of probiotic Bifidobacterium treatment on MS and on the underlying mechanisms in order to elucidate the properties of probiotics involved in the anti-MS effects. To achieve this, we used two Bifidobacterium strains, B. animalis ssp. lactis GCL2505 (BlaG) and B. longum ssp. longum JCM1217T (BloJ), which have different properties in the gut, and intensively investigated their effects on metabolic parameters, global changes in the gut microbiota, and SCFA levels in mice. BlaG was originally isolated from the faeces of a healthy adult, and is reported to be a probiotic strain capable of proliferating in the gut21,22. BloJ is a type strain of Bifidobacterium longum that has been widely used in commercial probiotics23 and is reported to protect the host from enteropathogenic infection through the production of acetate24, but is not capable of proliferating in the gut22.
Results
B. lactis GCL2505 treatment improved glucose tolerance
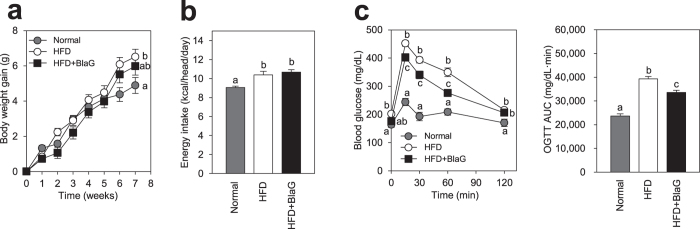
In Experiment 1, a high-fat diet (HFD) significantly increased body weight (Fig. 1a), energy intake (Fig. 1b), blood glucose (Fig. 1c), and plasma insulin levels after glucose challenge (Supplementary Fig. S2). Glucose tolerance was significantly improved by BlaG treatment in HFD-fed mice (Fig. 1c) and ob/ob mice (Experiment 3, Supplementary Fig. S1). BlaG treatment did not affect weight gain, energy intake, plasma insulin levels, or intestinal integrity-related parameters including the permeability of fluorescein-conjugated dextran or the gene expression of tight junction proteins (Fig. 1 and Supplementary Fig. S2).
Figure 1. Bifidobacterium animalis ssp. lactis GCL2505 (BlaG) treatment improved glucose tolerance in mice fed a high-fat diet (Experiment 1).
(a) Body weight gain. (b) Daily energy intake. (c) Blood glucose levels and the area under the curve after oral glucose challenge (2 g/kg body weight) at 6 weeks of the BlaG treatment. Data represent the mean ± SEM. Statistical analyses were performed using the Tukey–Kramer multiple comparison test. Different letters next to bars indicate a significant difference (P < 0.05).
Bifidobacterium strain-specific effects on metabolic parameters
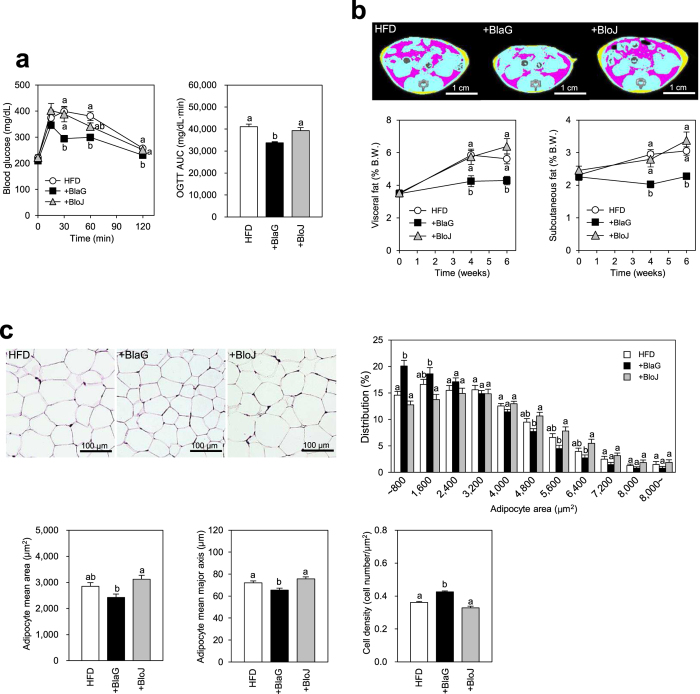
To investigate the properties of BlaG that improve glucose tolerance in the host, we compared the effect of BlaG with that of BloJ on several metabolic parameters of mice in Experiment 2. BlaG treatment significantly improved glucose tolerance compared with HFD-fed controls; however, BloJ treatment had no such effect (Fig. 2a). X-ray computed tomography (CT) analysis revealed that the accumulations of both visceral and subcutaneous fat were significantly decreased by BlaG treatment at 4 and 6 weeks after the start of treatment. However, BloJ treatment had no effect on the accumulation of either type of body fat (Fig. 2b). Histological analysis of epididymal adipocytes showed a greater proportion of smaller adipocytes in the BlaG-treated group than in the HFD-fed control group (Fig. 2c). On the other hand, no difference in adipocyte size was observed between the BloJ-treated and HFD-fed control groups. These results indicated that BlaG but not BloJ had effective anti-MS effects when administered to HFD-fed mice. Neither the plasma insulin levels after glucose challenge nor the triglyceride levels were affected by BlaG or BloJ treatment in HFD-fed mice (Supplementary Fig. S3).
Figure 2. Comparison of the BlaG treatment and Bifidobacterium longum JCM1217T (BloJ) treatment to improve glucose tolerance and body fat accumulation in HFD mice (Experiment 2).
(a) Blood glucose levels and the area under the curve after oral glucose challenge (2 g/kg body weight) after the bifidobacteria treatment for 6 weeks. (b) Representative computed tomography (CT) images after 6 weeks of probiotic treatments and serial assessment of CT-estimated proportions of visceral and subcutaneous fat weight to body weight after 0–6 weeks of probiotic treatment. The pink and yellow areas in CT images represent the visceral and subcutaneous fat, respectively. (c) Representative epididymal fat tissue staining, cell area distribution, mean area, mean major axis, and cell density of epididymal adipocytes after 7 weeks of bifidobacteria treatments. Data represent the mean ± SEM. Statistical analyses were performed using the Tukey–Kramer multiple comparison test. Different letters next to bars indicate a significant difference (P < 0.05).
B. lactis GCL2505 treatment altered the overall structure of gut microbiota
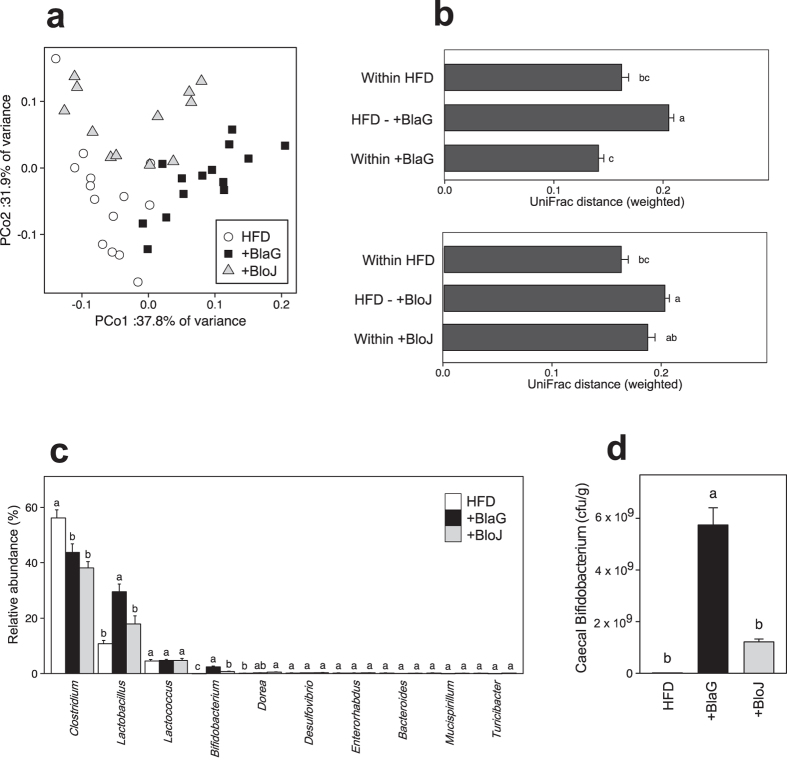
We compared the overall bacterial community structure of the gut microbiota by using 16 S rRNA gene pyrosequencing in Experiment 2. A principal coordinate analysis based on the weighted UniFrac metric revealed that the BlaG-treated group formed a distinct cluster clearly set apart from the HFD-fed control group (Fig. 3a). In addition, the mean distance in the mixture of HFD-fed control and the BlaG-treated groups was significantly higher than in the HFD or BlaG groups (Fig. 3b). However, the distance in the mixture of HFD-fed control and BloJ-treated groups was no different to that of the BloJ groups. Moreover, cluster analysis against the weighted UniFrac metric also revealed a clear separation of the HFD-fed control group from the BlaG-treated group in accordance with the bar chart (Supplementary Fig. 4b). These results indicated that BlaG treatment exerted a significantly greater influence on the overall bacterial community structure of gut microbiota compared with BloJ treatment in HFD-fed mice.
Figure 3. Analysis of the microbiota in the contents of the caecum.
(a) Principal coordinate analysis plot generated using a weighted UniFrac metric. The two components explained 69.7% of the variance. (b) Weighted UniFrac distance metric in the HFD-fed control, the BlaG-treated, and the BloJ-treated groups. (c) Bacterial composition at the genus level in the samples. For genus-level assignment of 16 S reads (16 S rRNA gene V1–V2 region), a 94% sequence identity threshold was applied. The vertical axis represents the relative abundance (%) of each genus in the microbiota. (d) The number of Bifidobacterium in caecal samples quantified by quantitative polymerase chain reaction. Data represent the mean ± SEM. Tukey–Kramer multiple comparison test was used. Different letters next to bars indicate a significant difference (P < 0.05).
Composition of gut microbiota
In bacterial composition analysis at the genus level, the abundance of both Lactobacillus and Bifidobacterium was significantly greater in the BlaG-treated group than in the HFD-fed controls or the BloJ-treated group (Fig. 3c). Quantitative polymerase chain reaction (qPCR) also demonstrated that the number of Bifidobacterium cells was significantly greater in the BlaG-treated group than in the BloJ-treated group (Fig. 3d). Species-level analysis revealed that both L. johnsonii and B. animalis were more abundant in the BlaG-treated group than in the control group (Supplementary Fig. S4e). The number of administered Bifidobacterium strains in the gut was quantified by qPCR using species-specific primers, namely, B. lactis-specific primers for the BlaG-treated group and B. longum-specific primers for the BloJ group. In the BlaG-treated group, the number of B. lactis was 2.6 ± 0.3 × 109 cfu/g, whereas the number of B. longum in the BloJ-treated group was far less at 0.46 ± 0.17 × 109 cfu/g.
B. lactis GCL2505 treatment elevated both acetate and GLP-1 levels, which are associated with metabolism parameters
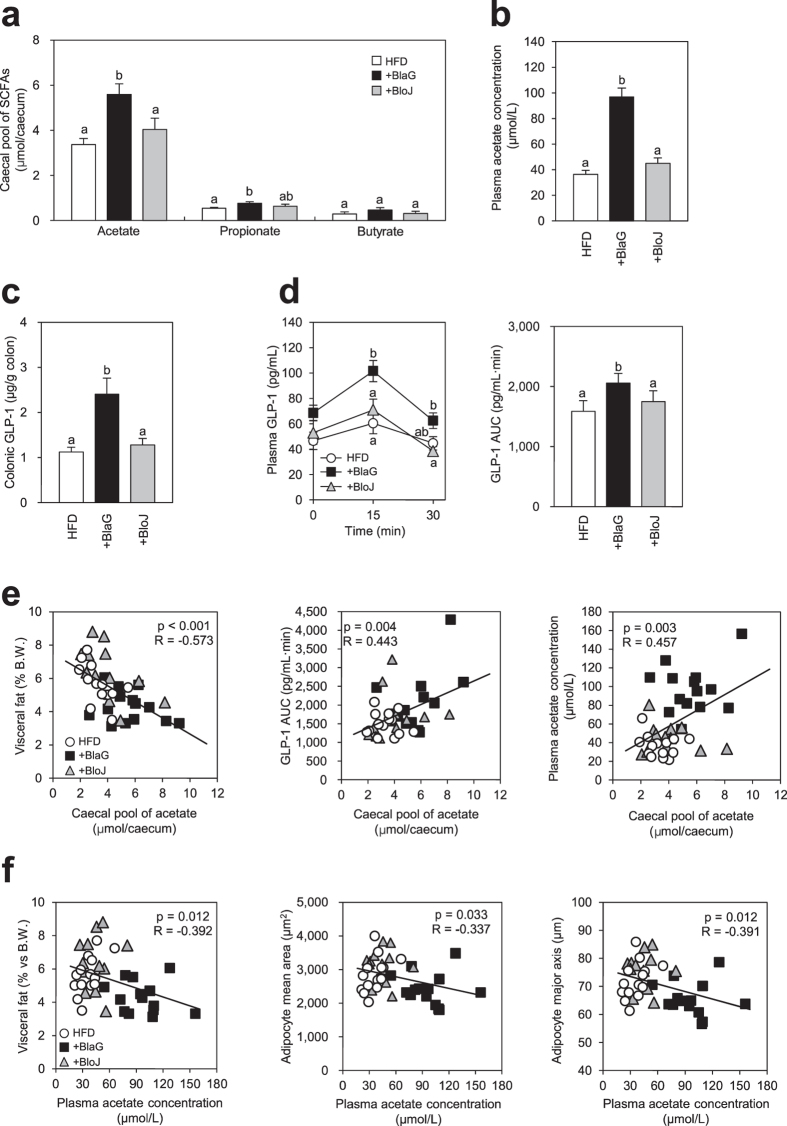
We measured the amount of SCFAs in the gut. The caecal pools of acetate and propionate were significantly higher in the BlaG-treated group than in the HFD-fed control group (Fig. 4a). Similar elevation of caecal acetate by BlaG treatment was also observed in the preliminary ob/ob mice model (Experiment 3, Supplementary Fig. S1e). However, these SCFAs were not markedly elevated by BloJ treatment in the HFD-fed mice. The plasma acetate concentration was also significantly higher in the BlaG-treated group than in the HFD-fed control or BloJ-treated groups (Fig. 4b). Compared with the HFD-fed control group, a significant elevation of colonic GLP-1 secretion was observed in the BlaG-treated group, but not in the BloJ-treated group (Fig. 4c). In addition, plasma GLP-1 levels after glucose challenge were significantly elevated only by BlaG treatment (Fig. 4d). We performed correlation analyses to investigate whether the caecal SCFAs affect metabolic parameters and/or GLP-1 secretion. The level of caecal acetate correlated negatively with the amount of visceral fat but positively with plasma GLP-1 levels (Fig. 4e). Moreover, the concentration of plasma acetate correlated positively with the caecal pool of acetate, but negatively with both the amount of visceral fat and adipocyte size (Fig. 4e,f).
Figure 4. Effect of bifidobacteria treatment on short-chain fatty acid (SCFA) levels, glucagon-like peptide-1 (GLP-1) secretion, and the correlation between the two variables.
(a) SCFA levels in the caecum after 7 weeks of probiotic treatments. (b) Plasma acetate concentration. (c) Colonic GLP-1 levels measured using enzyme-linked immunosorbent assay. (d) Plasma GLP-1 levels and the area under the curve 0–30 min after oral glucose challenge in mice fed a high-fat diet with 6 weeks of probiotic treatments. (e) Correlation analysis between caecal acetate levels and visceral fat accumulation, plasma acetate levels and GLP-1 levels. (f) Correlation analysis between plasma acetate levels and visceral fat accumulation and adipocyte size. Pearson’s R correlation and corresponding P value are presented. Data represent the mean ± SEM. Tukey–Kramer multiple comparison test was used to assess the differences between the groups. Different letters next to bars indicate a significant difference (P < 0.05).
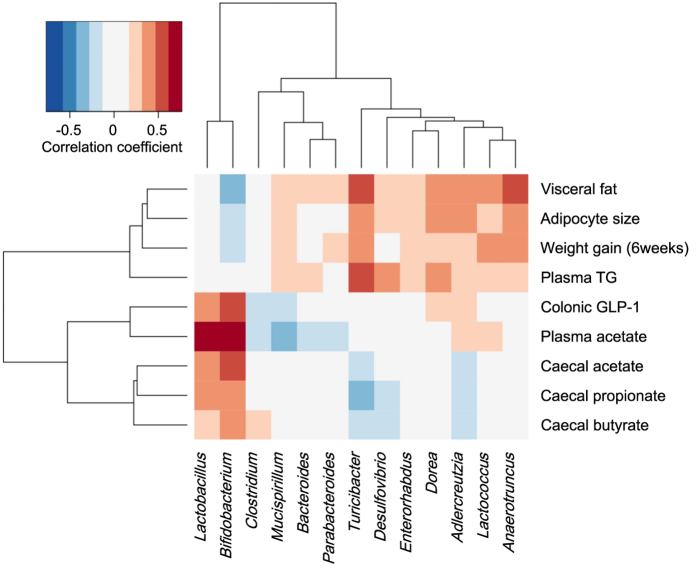
Relationship between gut microbiota composition and SCFA/MS-related parameters
We next assessed the correlation between the relative abundance of dominant bacterial genera and SCFAs/ MS-related parameters to identify the genera that might contribute to the production of SCFA or the anti-MS effects (Fig. 5). At the genus level, the relative abundance of Bifidobacterium correlated positively with caecal acetate, plasma acetate and colonic GLP-1 levels (r = 0.54, 0.76 and 0.60, respectively, all P < 0.001), and negatively with the amount of visceral fat (r = −0.31, P < 0.05). The abundance of Lactobacillus also correlated with caecal acetate, plasma acetate and colonic GLP-1 levels (r = 0.67, 0.42 and 0.43, respectively, all P < 0.01). The other genera showed no correlation with SCFA levels. At the species level, correlation and network analyses revealed that the abundance of B. animalis, L. johnsonii and L. reuteri correlated positively with caecal SCFA, plasma acetate level and GLP-1 (Supplementary Figs S5 and 6).
Figure 5. Correlation between the relative abundance of genera and metabolic parameters in mice.
Pearson’s correlation coefficients are represented by colour ranging from blue (negative correlation, −1) to red (positive correlation, 1). Data on genus reads used for the analysis represented 73.7% of the total reads of microbiota.
Discussion
Although numerous reports indicate that several probiotics improve MS16,17,18,19,20, the properties of probiotics that are involved in these anti-MS effects remain unclear. In the present study, BlaG treatment improved glucose tolerance in HFD-fed mice as well as in ob/ob mice (Fig. 1 and Supplementary Fig. S1). We conducted a comparative analysis using both BlaG and BloJ to investigate the mechanism(s) underlying the anti-MS effect by BlaG. The results showed that only BlaG improved glucose metabolism, concomitantly suppressing the accumulation of body fat and adipocyte hypertrophy (Fig. 2).
Several studies have reported that the anti-obesity effect of probiotics is related to changes in the gut microbiota16,18,25. We thus hypothesised that BlaG exerts an influence on the gut microbiota that differs from that exerted by BloJ because it has a greater proliferative activity in the gut than BloJ22. Interestingly, 16 S rRNA pyrosequencing analysis of caecal contents revealed that BlaG exerted a significantly greater influence on the overall bacterial structure of gut microbiota than BloJ (Fig. 3b and Supplementary Fig. S4b). Analysis of the bacterial composition at genus-level revealed that the relative abundances of the genera Bifidobacterium and Lactobacillus were remarkably enriched in the gut microbiota of the BlaG-treated mice (Fig. 3c). Indeed, qPCR analysis demonstrated that the number of B. lactis in the BlaG-treated group was more than five-fold greater than that of B. longum in the BloJ-treated group following treatment with the same cell numbers of each probiotic strain (see results). Consequently, BlaG treatment resulted in approximately a four-fold increase in the number of Bifidobacterium compared with BloJ treatment (Fig. 3d). These results demonstrated that BlaG proliferated effectively in the gut in HFD-fed mice because there were a greater number of Bifidobacterium cells present in BlaG-treated group, which agrees with previous reports21,22. Therefore, the highly proliferative probiotic strain BlaG altered the overall bacterial structure of the gut microbiota, probably through efficient proliferation, resulting in the improvement of MS, whereas the low numbers of Bifidobacterium strain BloJ had little influence on the microbiota or host metabolism.
The dominant metabolites of Bifidobacterium and Lactobacillus are acetate/lactate and lactate, respectively. Lactate is eventually metabolised to other organic acids including SCFAs by gut microbes26. Hence, we next focused on the changes in levels of SCFAs in the gut and plasma following probiotic treatment. Caecal and plasma acetate levels were significantly elevated by BlaG treatment, whereas the levels were unchanged by BloJ treatment (Fig. 4a,b). Similar elevation of caecal acetate by BlaG treatment was also observed in the ob/ob mice model (Supplementary Fig. S1e). Correlation analysis between the abundances of the gut microbiome and SCFAs revealed that genus Bifidobacterium and genus Lactobacillus correlated positively with SCFAs levels (Fig. 5). These data suggested that the enrichment of Bifidobacterium and Lactobacillus in the BlaG-treated mice might play a major role in accelerating the production of SCFAs in the gut. Because Lactobacillus mostly produces lactate as an end product of carbohydrate metabolism, the increase in Bifidobacterium appeared to have mainly contributed to the elevation of acetate in the BlaG-treated mice.
It has been recently demonstrated that SCFAs regulate energy homoeostasis via GPCRs9,27. GPR41 is activated equally by propionate and butyrate, whereas GPR43 is more responsive to acetate and propionate than to butyrate28,29. In the intestinal epithelium, SCFAs were found to stimulate GPR43, which resulted in the secretion of GLP-1, a gut-derived hormone that plays a significant role in energy metabolism9. In the present study, BlaG treatment significantly enhanced GLP-1 levels in both the colon and plasma, whereas no such effect was observed in the BloJ-treated mice (Fig. 4c,d). In addition, colonic GLP-1 levels correlated positively with luminal acetate levels (Fig. 4e) but not with propionate or butyrate levels (data not shown). These results implied that enhanced luminal acetate levels following BlaG treatment stimulated GLP-1 secretion in the colon, possibly via GPR43.
Kimura et al.9 reported that GPR43 signalling in adipocytes inhibits insulin signalling, and results in the suppression of fat accumulation in adipose tissue and an improvement in systemic insulin resistance. In the present study, BlaG treatment resulted in the elevation of both plasma and caecal acetate levels (Fig. 4a,b) in conjunction with improved glucose tolerance and less body fat accumulation. On the other hand, acetate levels showed a significant negative correlation with the amount of visceral fat and adipocyte size (Fig. 4e,f). These results suggested that the elevation in plasma acetate following BlaG treatment was associated with a reduction in the size of adipocytes, probably through enhanced insulin sensitivity via GPR43 signalling, which resulted in improved glucose tolerance and less fat accumulation. Together with the elevation in GLP-1 expression following BlaG treatment, our findings suggest that the enhanced production of gut acetate probably played a pivotal role in the anti-MS effects observed.
It has been reported that GLP-1 and GPR43 signalling potentiates insulin secretion by beta cells in the pancreas13. In addition, GLP-1 and acetate are reported to control appetite via the central nervous system10,30. However, bifidobacteria treatment did not affect either insulin secretion or food intake in this study (Fig. 1 and Supplementary Figs S2 and 3). Further research is therefore required to investigate why the elevation of both GLP-1 secretion and plasma acetate in this study did not lead to increased insulin secretion or appetite suppression.
Several possible relationships between metabolic parameters and intestine-related parameters, such as intestinal integrity, and between the diversity of the gut microbiota and the Bacteroidetes/Firmicutes ratio have been reported3,31. Some reports have indicated that increases in the number of bifidobacteria following probiotic or prebiotic treatment might restore impaired intestinal integrity4,5. In the present study, there were no changes in intestinal integrity-related parameters (Supplementary Fig. S2c and d) or microbial diversity (Supplementary Fig. S4a). Moreover, phylum-level analysis of the gut microbiota in this study demonstrated that BlaG treatment significantly elevated the abundance of phylum Actinobacteria but did not affect the Bacteroidetes/Firmicutes ratio (Supplementary Fig. S4d). It appears unlikely that intestinal integrity, microbial diversity, or the Bacteroidetes/Firmicutes ratio is involved in the anti-MS effects mediated by BlaG treatment.
In conclusion, B. lactis GCL2505, a highly viable and proliferative probiotic, exerted anti-MS effects, such as improved glucose tolerance and the suppression of visceral fat accumulation, via changes in the overall bacterial structure of the gut microbiota and elevations in the levels of SCFAs, especially acetate.
Methods
Preparation of Bifidobacterium strains
BlaG was obtained from Ezaki Glico Co., Ltd. and cultured in Gifu anaerobic medium broth (Nissui) supplemented with up to 1% glucose. BloJ was obtained from the Japan Collection of Microorganisms (RIKEN BioResource Center) and cultured in MRS broth (Merck). To prepare the probiotic treatments, these strains were cultured daily under anaerobic conditions using the AnaeroPack Kenki (Mitsubishi Gas Chemical Co.). Cultures were washed and suspended in phosphate-buffered saline (PBS) or saline for the duration of the treatments.
Ethics of animal treatments
All experimental procedures were approved by the Tokai University Animal Experimentation Committee and the Institutional Animal Care and Use Committee of Ezaki Glico Co., and were performed in accordance with either the Guidelines for the Care and Use of Animals for Scientific Purposes at Tokai University or the Guidelines for Proper Conduct of Animal Experiments (Science Council of Japan).
Experiment 1
Five-week-old male C57BL/6 J mice (SLC Inc.) were housed in a controlled environment (12-h/12-h light-dark cycle). Mice were fed a normal diet (10% of calories from fat; D12450B, Research Diet Inc.) (Normal group, n = 12) or a HFD (45% of calories from fat; D12451, Research Diets Inc.). After 2 weeks, the HFD-fed mice were divided into HFD-fed control (n = 12) and BlaG-treated (n = 12) groups based on their body weights. Mice in the BlaG-treated groups received oral administration of the appropriate BlaG strain (1 × 109 colony forming units/day) daily for 7 weeks. Mice in the normal or HFD-fed control groups were given PBS daily. OGTT was performed 6 weeks after BlaG treatment (see below). After a further week, intestinal permeability testing was performed (see Supplementary methods) and all mice were sacrificed as described below. The experimental design is shown in Supplementary Fig. S7a.
Experiment 2
Five-week-old male C57BL/6 J mice (SLC Inc.) were housed in a controlled environment (12-h/12-h light-dark cycle). All mice were fed a HFD (D12451). After 2 weeks, the mice were divided into HFD-fed control (n = 12–14), BlaG (n = 12–14) and BloJ (n = 11–12) -treated groups based on their body weights and fat composition measured by X-ray CT (see below). Mice in the BlaG- or BloJ-treated groups received oral administration of the appropriate Bifidobacterium strain (1 × 109 colony forming units/day) daily for 7 weeks. Mice in the HFD-fed control group were given saline daily. At 0, 4, and 6 weeks after probiotics treatment started, body fat composition was analysed using X-ray CT (see below). OGTTs were performed 6 weeks after probiotics treatment commenced (see below). All mice were sacrificed at the end of the trial as described below. This experiment was performed in duplicate and the experimental design is shown in Supplementary Fig. S7b.
Oral glucose tolerance tests
Oral glucose tolerance tests were performed as follows. Mice were fasted for 6 h and then injected with glucose by gavage (2 g/kg glucose). Blood glucose content was determined with a glucose meter (Glucose Pilot, Aventir Biotech) using blood collected from the tip of the tail vein. In addition, plasma samples were collected after the glucose challenge to assess glucose-stimulated GLP-1 and insulin expression.
Body fat composition analysis
Body fat composition was analysed by the method described by Lubura et al.32 with some modifications. In brief, mice were anaesthetised by inhalation of isoflurane and scanned using a LaTheta (LCT-100) experimental animal X-ray CT system (Aloka). Contiguous 1-mm slice images between the proximal end of lumbar vertebra L1 and the distal end of L6 were used for quantitative assessment using LaTheta software (version 2.10, Aloka). Subcutaneous and visceral fat levels were evaluated quantitatively.
Sample collection
Mice were killed in a CO2 atmosphere after a 4-h fast, and blood samples and tissues were harvested for further analysis. Blood samples were collected into tubes containing heparin (Ajinomoto Co.) following cardiac puncture, and plasma was stored at −80°C after centrifugation at 3,000 × g for 15 min at 4 °C. Caecal contents and the colon segments were precisely dissected and stored at −80°C for further analysis. Colon segments were stored in RNAlater (Sigma-Aldrich) at −80°C until mRNA expression analysis. The epididymal fat was stored in 10% neutral formalin for histological analysis.
Biochemical analysis
For plasma GLP-1 quantification, blood samples were collected in test tubes containing a dipeptidyl peptidase IV inhibitor (Millipore). Colonic GLP-1 was extracted according to the method described by Cani et al.33. The homogenate was centrifuged at 2000 × g for 20 min at 4 °C, and the supernatant fraction was decanted and diluted 1000-fold in assay buffer. The active GLP-1 concentration was determined using an enzyme-linked immunosorbent assay (ELISA) method (Active GLP-1 ELISA Kit, Shibayagi). Plasma and caecal acetate levels were enzymatically measured in duplicate using a commercial kit (Acetate Colorimetric Assay Kit, Sigma-Aldrich). The analysis of other caecal SCFAs was performed as follows: Caecal samples were suspended in 5% (w/v) metaphosphate-PBS (49 mL/g sample). Suspensions were subsequently filtered using a 3-kDa MWCO spin column (Pall Corporation) and analysed on a gas chromatography-flame ionisation detector system (Shimadzu GC2014, Shimadzu, Kyoto, Japan) equipped with a glass column packed with 60/80 SHINCARBON A coated with Themon-3000 (Shinwa-kakou). Plasma triglyceride (Wako) and insulin (Ultrasensitive Mouse Insulin ELISA, Mercodia) levels were determined using the corresponding commercial kits.
Adipose tissue histology
Epididymal fat was fixed in 10% neutral formalin, processed in paraffin blocks, sectioned to a thickness of 4 μm, and stained with haematoxylin and eosin. Slides were scanned using a BIOREVO BZ-9000-Generation-II microscope (KEYENCE Co.), and the sizes of 700–1500 adipocytes were measured using BZ-II-Analyzer software (version 2.2, KEYENCE Co.). The number of adipocytes per total area of counted adipocytes was determined as the cell density.
16 S rRNA metagenomic analysis
The extraction of bacterial DNA from the samples of caecal contents was performed as described previously34. The hypervariable V1–V2 region of the 16 S gene was amplified by PCR with barcoded 27Fmod (5′-AGRGTTTGATYMTGGCTCAG-3′) and reverse primer 338R35 (5′-TGCTGCCTCCCGTAGGAGT-3′) and then sequenced using the 454 GS FLX Titanium or 454 GS Junior system (Roche Applied Science). Operational taxonomic unit (OTU) clustering, taxonomy assignment and UniFrac analysis were performed as described previously36.
Quantitative PCR analysis of the microbiota in the caecum
Bacterial DNA was extracted from the contents in the caecum as described previously21. The bacterial strains used as standard curves as well as the primers and amplification programs are listed in Supplementary Table 1. Quantitation of specific bacterial counts, the bacterial strains used as standard curves, primers and amplification programs are also listed in Supplementary Table 1.
Statistical analysis
Results are presented as means ± SEM. Statistical evaluation of multiple groups was performed using one-way ANOVA with posthoc Tukey Kramer multiple comparison testing. Statistical evaluation of two groups was performed using the Student t-test. Correlation analyses were conducted using Pearson linear regression. A value of P < 0.05 was considered statistically significant. All statistical analyses were conducted using the open-source software program R, Version 3.1.1 (http://cran.r-project/org).
Additional Information
How to cite this article: Aoki, R. et al. A proliferative probiotic Bifidobacterium strain in the gut ameliorates progression of metabolic disorders via microbiota modulation and acetate elevation. Sci. Rep. 7, 43522; doi: 10.1038/srep43522 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Footnotes
The authors declare no competing financial interests.
Author Contributions R.A. and K.K. designed the study, performed research, analysed data and drafted the manuscript. W.S. and M.H. performed metagenomic informatics and reviewed/edited the manuscript. H.T., Y.M. and N.S. performed research and analysed data. Y.K. designed the study and reviewed/edited the manuscript.
References
- Ley R. E., Turnbaugh P. J., Klein S. & Gordon J. I. Microbial ecology: Human gut microbes associated with obesity. Nature 444, 1022–1023 (2006). [DOI] [PubMed] [Google Scholar]
- Cani P. D. et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56, 1761–1772 (2007). [DOI] [PubMed] [Google Scholar]
- Cani P. D. et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57, 1470–1481 (2008). [DOI] [PubMed] [Google Scholar]
- Cani P. D. et al. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut 58, 1091–1103 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neyrinck A. M. et al. Wheat-derived arabinoxylan oligosaccharides with prebiotic effect increase satietogenic gut peptides and reduce metabolic endotoxemia in diet-induced obese mice. Nutr. Diabetes 2, e28 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everard A. et al. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes 60, 2775–2786 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X. et al. Modulation of gut microbiota by berberine and metformin during the treatment of high-fat diet-induced obesity in rats. Sci. Rep. 5 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canfora E. E., Jocken J. W. & Blaak E. E. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat. Rev. Endocrinol. 11, 577–591 (2015). [DOI] [PubMed] [Google Scholar]
- Kimura I. et al. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43. Nat. Commun. 4, 1829 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost G. et al. The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat. Commun. 5, 3611 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNelis J. C. et al. GPR43 potentiates β-cell function in obesity. Diabetes 64, 3203–3217 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolhurst G. et al. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61, 364–371 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjems L. L., Holst J. J., Volund A. & Madsbad S. The influence of GLP-1 on glucose-stimulated insulin secretion: effects on cell sensitivity in type 2 and nondiabetic subjects. Diabetes 52, 380–386 (2003). [DOI] [PubMed] [Google Scholar]
- Zander M., Madsbad S., Madsen J. L. & Holst J. J. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and β-cell function in type 2 diabetes: a parallel-group study. Lancet 359, 824–830 (2002). [DOI] [PubMed] [Google Scholar]
- Report of a Joint FAO/WHO Working Group on Drafting Guidelines for the Evaluation of Probiotics in Food. London, Ontario, Canada: 2002. April, May. Guidelines for evaluation of probiotics in food. Available at: http://www.fda.gov/ohrms/dockets/dockets/95s0316/95s-0316-rpt0282-tab-03-ref-19-joint-faowho-vol219.pdf. (Accessed: 19/07/2016) (2008).
- Yadav H., Lee J. H., Lloyd J., Walter P. & Rane S. G. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J. Biol. Chem. 288, 25088–25097 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin Y. N. Effects of four Bifidobacteria on obesity in high-fat diet induced rats. World J. Gastroenterol. 16, 3394 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. et al. Modulation of gut microbiota during probiotic-mediated attenuation of metabolic syndrome in high fat diet-fed mice. ISME J. 9, 1–15 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- An H. et al. Antiobesity and lipid-lowering effects of Bifidobacterium spp. in high fat diet-induced obese rats. Lipids Health Dis. 10, 116 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo S. et al. Antiobesity effects of Bifidobacterium breve strain B-3 supplementation in a mouse model with high-fat diet-induced obesity. Biosci. Biotechnol. Biochem. 74, 1656–1661 (2010). [DOI] [PubMed] [Google Scholar]
- Ishizuka A. et al. Effects of administration of Bifidobacterium animalis subsp. lactis GCL2505 on defecation frequency and bifidobacterial microbiota composition in humans. J. Biosci. Bioeng. 113, 587–591 (2012). [DOI] [PubMed] [Google Scholar]
- Aoki R. et al. Effect of Bifidobacterium animalis subsp. lactis GCL2505 on the physiological function of intestine in a rat model. Food Sci. Nutr. 4, 782–790 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soccol C. R. et al. The potential of probiotics: A review. Food Technol. Biotechnol. 48, 413–434 (2010). [Google Scholar]
- Fukuda S. et al. Bifidobacteria can protect from enteropathogenic infection through production of acetate. Nature 469, 543–547 (2011). [DOI] [PubMed] [Google Scholar]
- Falcinelli S. et al. Probiotic treatment reduces appetite and glucose level in the zebrafish model. Sci. Rep. 6, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flint H. J., Scott K. P., Louis P. & Duncan S. H. The role of the gut microbiota in nutrition and health. Nat. Rev. Gastroenterol. Hepatol. 9, 577–589 (2012). [DOI] [PubMed] [Google Scholar]
- Kimura I. et al. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41). Proc. Natl. Acad. Sci. 108, 8030–8035 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue D., Tsujimoto G. & Kimura I. Regulation of energy homeostasis by GPR41. Front. Endocrinol. (Lausanne). 5, 5–7 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura I., Inoue D., Hirano K. & Tsujimoto G. The SCFA receptor GPR43 and energy metabolism. Front. Endocrinol. (Lausanne). 5, 3–5 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutzwiller J. P. et al. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am. J. Physiol. 276, R1541–1544 (1999). [DOI] [PubMed] [Google Scholar]
- Turnbaugh P. J. et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444, 1027–131 (2006). [DOI] [PubMed] [Google Scholar]
- Lubura M. et al. Non-invasive quantification of white and brown adipose tissues and liver fat content by computed tomography in mice. PLoS One 7, e37026 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cani P. D., Dewever C. & Delzenne N. M. Inulin-type fructans modulate gastrointestinal peptides involved in appetite regulation (glucagon-like peptide-1 and ghrelin) in rats. Br. J. Nutr. 92, 521 (2004). [DOI] [PubMed] [Google Scholar]
- Said H. S. et al. Dysbiosis of salivary microbiota in inflammatory bowel disease and its association with oral immunological biomarkers. DNA Res. 21, 15–25 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. W. et al. Robustness of gut microbiota of healthy adults in response to probiotic intervention revealed by high-throughput pyrosequencing. DNA Res. 20, 241–253 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuda A. et al. Influence of proton-pump inhibitors on the luminal microbiota in the gastrointestinal tract. Clin. Transl. Gastroenterol. 6, e89 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.