Abstract
Involving patients in healthcare safety practices has long been an area of priority and importance. However, we still need to understand how patients perceive undesirable events during their hospital stay, and what role patients play in the prevention of these events. To address this gap, we surveyed pediatric inpatients and caregivers to understand their perspectives on undesirable events. By giving them an opportunity to use their own words to describe their experiences, we found a diverse array of undesirable events. Our qualitative analysis revealed four major types of events that patients and caregivers experienced: mismanagement, communication, policy, and lack of care coordination. We also examined the information needs that patients and caregivers experienced during these situations, and learned how they would prefer to receive this information. Based on these results, we provide recommendations for inpatient technologies that could enable patients to identify and prevent such undesirable events.
Introduction
Despite over a decade of national attention to the problem of patient safety, as described in To Err is Human and Crossing the Quality Chasm1,2, a recent study estimates that over 440,000 people die every year from preventable medical errors in U.S. hospitals3. As of 2016, preventable medical errors are considered the third leading cause of death in the United States, behind only heart disease and cancer4. Research over the past decade suggests that patients provide a distinct perspective on safety events that is not captured through staff reports and medical record review5,6. Weissman and colleagues looked at the overlap between undesirable events reported by patients and by physician review of medical records. Their work showed that 23% of 998 sampled patients reported at least one adverse event, compared to 11% of cases identified through medical record review. Moreover, only 12% of the events reported were discovered through both mechanisms6. Thus, to identify a comprehensive view of patient safety, we need to understand patients’ perspectives in addition to clinicians’ perspectives. Although several studies have solicited input from patients, these studies use closed-ended questionnaires based on categories of undesirable events that are predetermined and predefined by clinicians and medical researchers7–10. Thus, more research is needed to understand patients’ perspectives in their own words11.
Previous research has shown that patients can play a significant role in a variety of safety-related processes, such as helping healthcare providers confirm an accurate diagnosis, making appropriate treatment decisions, and choosing a good provider that aligns with the patient’s needs and values12. Patients have also been recognized as actors in identifying, preventing, and reporting medical errors. In 2007, Unruh and Pratt described five cases where oncology patients were involved in the identification, prevention, and recovery from medical errors in an outpatient setting13. Other studies in the inpatient setting have shown that patients notice errors related to their care and bring them to the attention of their providers12,14,15. However, we know little about what patients’ experiences and perspectives around patient safety are, or how to develop informatics solutions that support patients in their important safeguarding role.
In support of a strong role for patients, evidence from over 50 studies has shown a positive correlation between patient experience (e.g., respect for the preference of patients, inclusion of patients in decisionmaking, clinicians’ ability to empathize, and provision of information to enable self-care) and patient safety16. Despite this close relationship between patient experience and safety, existing technology for enhancing the patient experience is not typically designed to support and engage patients as active participants in the detection or prevention of undesirable events. To examine a related area of the role of existing technologies in supporting patient engagement within the hospital environment, Prey et al. found that technologies served a variety of purposes, including the use of entertainment to decrease anxiety and improve rehabilitation treatment, the delivery of general or tailored information to patients and caregivers, the enrichment of patient-provider communication, and the enhancement of communication and personalized decision support between patients and caregivers17. However, of the 17 articles included in the review, only two emphasized the technology’s role in improving safety18,19. Additionally, Greysen et al. conducted a pilot study using a tablet computer-based learning module to help educate patients about safety in the hospital20. Although these insights help us understand the role of patient engagement technology in the hospital setting, it remains unclear how similar tools, informed by inpatient safety experiences, can effectively support patients in identifying, preventing, and reporting undesirable events.
In this paper, we address these gaps and present the results of a survey asking pediatric inpatients and their caregivers about their prior experiences with undesirable events. Our study provides a rich understanding of these patient and caregiver experiences in their own words. We also identify information needs that participants felt could have prevented these undesirable events, as well as their preferred method for receiving this information. Based on these results, we explore the potential for technology to bridge these information gaps and assist patients and caregivers in preventing errors in the inpatient environment. These contributions have meaningful implications for the design and development of systems to increase the engagement of both patients and caregivers in hospital safety.
Methods
To account for a broad range of patient and caregiver experiences, we created a survey with open-ended questions regarding undesirable events. We defined undesirable event within the survey as something that: was a small or big concern, was unpleasant or caused harm, and could have been avoided (e.g., not being informed that a scheduled procedure was cancelled, being given the wrong medication). Although these experiences might not typically be recognized as an error by clinicians, and might not match with a clinician’s perspective of what constitutes harm, we need to understand and recognize these events from a patient’s perspective. This study was approved by the authors’ Institutional Review Board.
Site and Eligibility
This study was conducted at Seattle Children’s Hospital, which manages over 300 beds, 5,000 hospital employees, and approximately 15,000 annual inpatient admissions. Patients were considered eligible if they were at least 7 years old, spent at least one night in the hospital during their current visit, and spoke English as their primary language. Caregivers were considered eligible if they were caring for a patient who had currently spent at least one night in the hospital, and if English was their primary language. Patients who were not well enough to give informed consent were not approached to complete the survey. We recruited participants from the acute care and intensive care units, and excluded those on the rehabilitation and inpatient psychiatric units due to the potential of our intervention to negatively affect safety, security, and patient care processes.
Procedure
We approached patients and caregivers after they spent at least one night in the hospital. A member of the research team described the study, defined the term undesirable event, and asked whether they had previously experienced such an event. If potential participants stated they had not experienced an undesirable event, they were deemed ineligible and thanked for their time. Those individuals who did experience an undesirable event were given further information about the survey instrument, and at that point either declined or consented to participate in this study. The consented participants were administered the survey instrument on an iPad, which was thoroughly wiped down with sanitizing cloths after each use to prevent the spread of infection within the hospital21. A research team member was available to answer questions or help the participant take the survey if necessary. Because we focus on patients’ perceptions, comparing the events that respondents mentioned in the survey with provider perspectives or official medical record reports was outside the scope of this study.
Survey Instrument
Our survey instrument was hosted by SurveyGizmo (www.surveygizmo.com) and went through several iterations of content validity and testing to ensure that the questions were clear, thorough, and understandable for all eligible participants, including children as young as 7 years old. The survey questions related to the participant’s undesirable event were a combination of closed- and open-ended questions asking them: (1) what was the undesirable event that they experienced, (2) what they believed caused this event, (3) what was the outcome of this event, (4) what they believe could have kept this event from happening, (5) what information the respondent thought they needed during this event, and (6) in what format they would prefer to receive this information. The participant could answer these questions about any previous undesirable event, not necessarily related to their current hospital stay. For example, caregivers could respond to the survey about an event in a different hospital that occurred several years ago with a family member other than their current pediatric patient. This flexibility helped to broaden the types of events we were interested in capturing.
Data Analysis
We analyzed the demographic and closed-ended survey question results using the analytical tools within SurveyGizmo. We conducted an inductive thematic content analysis on the responses to the four open-ended survey questions related to the respondent’s undesirable event22. The research team met regularly during data collection to read new survey responses and revise the codebook based on emerging themes observed in the data set. Three members served as coders, assigning each survey response one or more codes that represented these themes. Data analysis concluded when themes in the codebook reached saturation and each completed open-ended survey response was assigned at least one code.
Results
Our qualitative analysis found four major types of undesirable events that patients and caregivers discussed in their survey responses: Mismanagement, Communication, Policy, and Lack of Care Coordination. For each of these categories, we provide explanations with quotes and anecdotes from our participants below, as well as summarize the outcomes associated with these events (Figure 1). We also examine what information participants thought would have been helpful in preventing or reducing the impact of these events (Figure 2), and how they prefer to receive this information. Patient and caregiver responses are designated with ‘P#’ and ‘C#’ identifiers, respectively.
Figure 1.
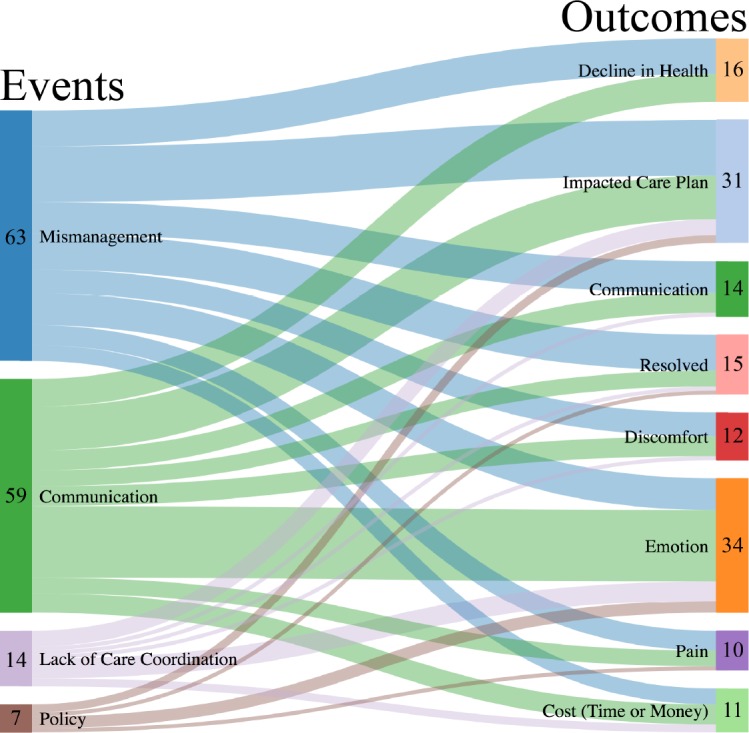
Relationship between reported events and outcomes. We identified 143 unique relationships when coding the undesirable events. Mismanagement and Communication events account for most of the self-reported events. While there was more consistency between the different amount of outcomes, impacted care plans and emotions were mentioned more frequently than other outcomes.
Figure 2.
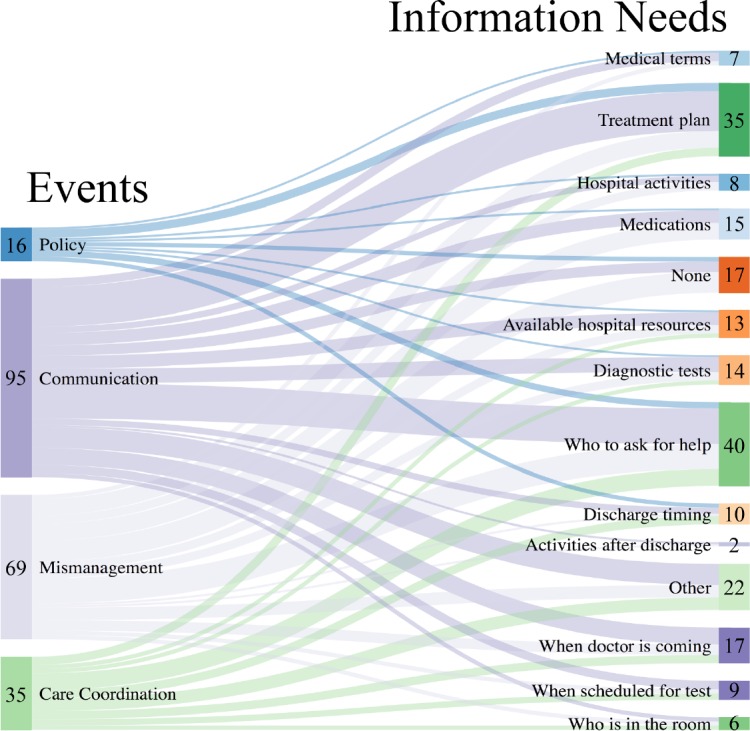
Information Needs. We asked patients to report if one or more of 16 information needs would have been beneficial during their undesirable event. We identified 215 unique relationships between the undesirable events and the information needs expressed in the survey. The most identified gaps in information were knowing who to ask for help and knowing the treatment plan.
Because we also assigned identifiers to 10 blank and 13 incomplete survey responses that were excluded from our analysis, some identifier numbers are greater than the number of complete responses.
Participants
Our research team approached 173 individuals in the hospital, of which 83 (47.98%) were considered ineligible because they had not experienced an undesirable event, 22 (12.72%) declined, and 68 (39.31%) completed the survey. Participant demographics are summarized in Table 1. Three of our participants expressed their desire to answer questions about more than one personal experience with undesirable events. Therefore, 68 individuals completed 71 survey responses describing 71 undesirable events, of which 16 (22.5%) identified being a patient, and 55 (77.5%) identified being a caregiver at the time of the undesirable event.
Table 1.
Survey Response Rates and Demographics
| n | % | |
|---|---|---|
| Survey respondents* | 68 | |
| Surveys completed | 71 | |
| Patients/caregivers approached | 173 | |
| Patients, caregivers ineligible | 83 | 48 |
| Patients/caregivers declined | 22 | 12.7 |
| Caregiver responses | 55 | 77.5 |
| Patient responses | 16 | 22.5 |
| Age | ||
| 18 or over | 62 | 87.3 |
| 14-17 | 7 | 9.9 |
| 7-13 | 2 | 2.8 |
| Gender | ||
| Male | 13 | 18.3 |
| Female | 57 | 80.3 |
| I prefer not to answer | 0 | 0 |
| Other - write in | 0 | 0 |
| No answer | 1 | 1.4 |
| Race/Ethnicity** | ||
| White or Caucasian | 51 | 71.8 |
| Hispanic or Latino | 7 | 9.9 |
| Black or African American | 1 | 1.4 |
| Asian | 7 | 9.9 |
| Native American/American Indian | 4 | 5.6 |
| Pacific Islander | 0 | 0 |
| Other - write in | 1 | 1.4 |
| I prefer not to answer | 7 | 9.9 |
| No answer | 1 | 1.4 |
3 respondents completed multiple surveys about different undesirable events
Participants could choose multiple categories
Mismanagement
‘Mismanagement’ is a term we use to characterize undesirable events that consisted of clinicians’ errors in judgement or decision-making, and problems with the execution of a task or completion of a process. The strongest themes within this category dealt with medication and equipment errors.
Medications
Patients and caregivers reported a variety of medication errors, including not receiving needed medications, receiving the wrong dosage, and receiving the wrong medication. One caregiver discussed her son not getting a medication for urinary retention for five days, resulting in the patient holding urine for over 12 hours at a time and the need to put in a catheter (C53). Regarding medication administration, another caregiver wrote about an event that happened to her daughter right before undergoing a major procedure: “She was given 5 times to [sic] much morphine and she was hardly breathing” (C47). In other cases, patients received the wrong medication intended for another patient. A pediatric patient recalled a mix-up while sharing a hospital room with his sister: “Someone did not look at the label close enough” (P12).
Equipment
Participants also mentioned the misconfiguration or mishandling of medical devices. One NICU caregiver noticed that the nurse did not use a board to secure her son’s IV. She later woke in the middle of the night to find the patient’s IV detached and his hospital gown “soaked in blood.” She recalled: “I didn’t know what had happened… but it looked pretty scary, and made me wonder when he had last been checked on by staff” (C45). In another example, C63 woke suddenly for early morning rounds at 6:00 am. As the examination began, this caregiver noticed the patient’s External Ventricular Drain was not clamped off, and brought this oversight to the attention of the providers in the room. “At that point they realized they had the incorrect patient. They were looking for the baby in the next bed. Her parents were not with her…I’m thankful I came to my senses in time to interrupt them.” Because C63 noticed the problem and shared this information with the providers, she stopped a treatment from being given to the wrong patient.
Outcomes
Many of the undesirable events were successfully resolved. For example, C53’s son eventually received the necessary medication, while C47 noted her daughter’s mistake in morphine administration was reversed, and the patient was able to wake up. Other situations, however, lead to a decline in the patient’s health, which required additional care. For example, one patient was told she needed to remain flat after a procedure, but was walked back to her hospital room instead. Severe headaches and vomiting developed as a result. “My hospital stay was lengthened due to this and has caused lower back pain for several years” (P94). As a result of these experiences, patients and caregivers reported feeling angry, scared, and worried.
Communication
Many undesirable events discussed by survey respondents involved communication problems that manifested in different ways: between providers, in receiving information, and in providing information.
Between Providers
Participants identified conflicts and a lack of communication among their providers as a type of undesirable event. Regarding his diagnosis, a pediatric patient said that “the doctors were disagreeing amongst themselves” and, in this patient’s opinion, this disagreement caused them to overlook the data and miss “the real problem” (P30). In another example, a caregiver described an event where disagreements between different teams of providers actually distracted them from the patient’s increasingly urgent medical situation: “[my son] turned blue and was gasping for air. The nurse my son had that day took charge and called the charged [sic] nurse for help. As we moved my son to the ICU floor, both team[s] were still arguing” (C91).
Not Receiving Information
Participants described difficulty in dealing with the lack of information. One parent mentioned, “A doctor I had never met before discussed worst case scenario treatment options in a very casual fashion…He was not a doctor in charge of making treatment decisions but more of a consult however didn’t identify himself that way” (C78). Because this caregiver did not receive more information about the provider, including why he was in the room, it influenced C78’s interpretation of treatment options that were discussed. Another caregiver remembered a time when the IV team was called to repair her son’s leaking line, but took over 2 hours to arrive. When asked about what she thought caused this event, C90 responded, “unwillingness of IV team to give updates despite repeated requests from [hospital department]”. This caregiver felt “caught off guard” because this delay also prevented the patient’s family from receiving critical information about his treatment side effects.
Challenges in Providing Information
Many caregivers felt that their voiced concerns about potential or ongoing problems were not acknowledged. For example, one NICU caregiver kept waking in the middle of the night due to the continuous alarm from the isolette. According to this caregiver, the nurse would come into the room and attempt to shut off the alarm every few minutes. “We were familiar with the isolette… and so could tell she had it on the wrong mode. We continued voicing our concern and the machine kept beeping…finally they had a NICU nurse come down and show her that she didn’t have the temperature probe on the baby’s body…” (C69). Although this caregiver expressed her concern to the nurse, she had to wait for a different provider to intervene and turn off the alarm. In another example, one adolescent patient described his unwillingness to give his providers information because he felt he was not receiving the care he needed: “the docters [sic] didn’t give me anything to help the pain. It basically felt like they gave up on me and said suck it up… I soon didn’t even want to talk to the docters [sic] at all because they were being horribly rude to me” (P18).
Outcomes
As a result of these communication errors, patients and caregivers experienced a range of negative emotions (e.g., frustration, stress, unhappiness, distrust, fear), health outcomes, delays in care or discharge, and need for additional care. Some respondents indicated that their undesirable events were successfully resolved. For example, C90’s son eventually had his IV line repaired. A few caregivers explicitly mentioned speaking up and requesting different providers to care for their child (C20, C65). Caregivers also expressed a desire to be more involved in the care process.
Policy
Patients and caregivers found themselves at odds with policies that seemed unreasonable or inconvenient. During a previous admission at a different hospital, P21 made a request for manual chest physiotherapy (CPT), a request that was not fulfilled due to “liability concerns”. The patient described, “I have had manual CPT at every other hospital I have ever been admitted to without any problem and found their policies to be ridiculous” (P21). One caregiver mentioned that hospital policy made it difficult to keep her family physically together: “After we had been asleep a while they came and told us hospital policy that our son cannot stay here but they were trying to approve it. So approve it! It’s been a long day and I don’t see how telling me that when we’re already in bed can help anyone” (C38).
Adverse effects of contact isolation protocols were also mentioned. A patient described her frustration with being placed under isolation when she did not believe she met its criteria. The patient’s siblings were not allowed to visit, and she was unable to receive the emotional support she wanted (P89). C62 was not allowed to store perishable food in the patient’s room according to contact isolation rules. Their room was far from the cafeteria or nutrition room, and an increased financial cost was associated with obtaining a room closer to food storage. As a result, both the caregiver and patient were unable to eat properly during their hospital stay.
Outcomes
Respondents cited negative health outcomes and negative emotions as a result of undesirable events related to policy. Because P21’s preferences were not accommodated, there was “barely any improvement in lung function, followed by another hospital stay for the same lung issues just a few months later.” Due to C62’s lack of food access, she was unable to eat regularly, resulting in poorer general health. Negative emotions were also mentioned. P89 reported that contact isolation made her feel trapped in her room. “I felt as though [the doctors] didn’t understand how much it affected me as a patient.”
Lack of Care Coordination
The term ‘Lack of Care Coordination’ includes problems with scheduling, logistics, or coordination among providers, families, and patients. One participant described: “Care was not clustered and woke baby up repeatedly through the night, often just 30 minutes apart from one another” (C43). Two other caregivers mentioned missed opportunities to speak with providers about their child’s care (C57, C49). For C49, this prevented the patient’s parents from discussing their concerns about the patient’s care. “Further attempts were made by caregiver to state concerns. Hospitalist involved but damage was done.”
A lack of planning caused inconvenient delays in discharge for some patients. P39 stated, “I got discharged on Monday when my doctor said it could have been on Sunday” due to both a lack of coordination and communication. P16, an adolescent patient, experienced a discharge delay “for about a week” because both the patient and hospital staff had difficulty contacting the appropriate caregiver to sign the discharge paperwork. There was no plan in place to accommodate for this situation, and despite being healthy enough for discharge, the patient remained in the hospital until someone was available to provide a signature for her release.
Outcomes
In addition to discharge delays, C57’s daughter experienced a delay in care because he was not present for his child’s procedure. Negative emotions were also identified as outcomes of events related to lack of care coordination. C43’s child was “sad” and “cranky” the following day due to lack of sleep, while P16 struggled with unwanted feelings of being alone in the hospital. Respondents felt that proper planning and communication would have prevented these events from occurring. “Coordinate with each other… make sure you know what needs to be done in advance” (C43). C49 expressed a desire for “an agreed upon round time that met [the] schedule of all parties involved.”
Information Needs and Preferences
After describing their undesirable event, respondents were provided a list of 16 information needs, and asked if one or more of these items would have been helpful for them to know. The results of this question are shown in Figure 2. Differences in information needs were found across the types of events and between patients and caregivers. For example, patients who experienced mismanagement, communication, or policy errors were most interested in having information about their tests, procedures, and treatment plans. Patients who experienced care coordination problems wanted to know about discharge, while caregivers more interested in the timing of clinician visits. However, across all types of undesirable events that emerged from our analysis, caregivers most frequently indicated their desire to know ‘who to contact for help or questions’.
Respondents were then asked how they prefer to receive these information needs. They selected one or more modes of information delivery, from a list of 9 non-technology based (e.g., paper handouts, written on the whiteboard, talking with doctors and nurses) and existing electronic (e.g., patient portal, text message, email) methods. Of the 80 total choices that our 16 patient respondents made, 68 (85.0%) fell into the non-technology based category, while 12 (15.0%) fell into the electronic category. Our 55 caregiver respondents made a total of 263 choices, of which 183 (69.6%) indicated non-electronic and 80 (30.4%) were electronic preferences for information delivery.
Discussion
Our participants provided informative data about the context and consequences of patient and caregiver experiences with undesirable events. Our results highlight the value of these perspectives in informing the design, development, and improvement of patient engagement technologies that can support error prevention within the hospital environment.
Undesirable Events from the Patient Perspective
Our findings extend previous definitions of undesirable events by accounting for patient and caregiver experiences. In addition to confirming previous concepts of undesirable events, participants also discussed mismanagement of situations regarding medications and medical equipment, disagreements with hospital policies, and challenges with communication and coordination. In related work, patients were usually asked to provide a binary response (yes or no) as to whether they encountered specific instances of clinician-defined undesirable events7–10. These studies rarely allowed patients to provide further details. Our survey gave patients and caregivers the opportunity to share their knowledge in an unrestricted, open-ended way. This patient-focused approached revealed previously unidentified types of errors, and explored patient-perceived causal relationships between an undesirable event and its impact on the patient and caregiver (Figure 1). This knowledge permits future systems to better align with the needs of patients and caregivers.
Implications for Health IT and Inpatient Engagement Systems
Our results yield three major implications for inpatient information systems designed to increase patient engagement in the prevention of undesirable events. These systems should: (1) accommodate different information needs and preferences, (2) provide real-time information about the patient’s care, and (3) supplement face-to-face communication with clinicians.
Accommodate Different Information Needs and Preferences
Our findings indicate that information needs differed across types of events as well as between patients and caregivers. It is extremely important for patient-facing solutions to provide this range of information, due to current challenges in anticipating the nature of an undesirable event during a patient’s hospital stay. Future work in this area could further explore patterns of information needs associated with types of events, which would assist in the prediction or delivery of this tailored information to the patient and caregiver.
When asked about how they prefer to receive the information above, respondents favored more traditional communication options (e.g., paper handout, written on the patient’s whiteboard, talking with clinicians,) rather than modern solutions (e.g., patient portal, email, text message). This focus on non-technology based solutions could be explained by current hospital practices that tend to rely on such traditional solutions for distributing information, and the barriers patients and caregivers encounter when attempting to capture this information using technology23. Despite our respondents’ strong preference for paper, handwritten, and verbal communication, recent work involving pediatric inpatient portals found that 89% of parents thought the use of such a portal helped reduce errors in the patient’s care24. More research is needed to understand how the availability and enhancement of similar tools can impact patient and caregiver preferences for information delivery.
Provide Real-Time Information
Patient-facing information systems for the inpatient environment need to provide patients and caregivers with real-time information about the patient’s care. One respondent, a caregiver, described a situation where she did not receive updates about changes made to the patient’s medication plan: “[there were] too many people involved and too many changes made and parents not aware of them” (C15). In this case, not receiving updates about changes to the patient’s medication was the primary reason for the caregiver’s undesirable event. Because undesirable events can arise at any point during a hospital stay, we strongly recommend that systems provide patients and their caregivers with information about their care without any built-in time delay, providing capture and access functionality that supports retrieval and review at a patient or caregiver’s convenience. These tools have the potential to share information with other family members and caregivers who make critical decisions about the patient’s care. Also, providing additional information (e.g., explaining what a lab result means) allows patients and caregivers to better understand treatments and ultimately strengthen their ability to act as their own advocate.
Supplement Face-to-Face Communication
Inpatient systems also have the potential to offer patients and caregivers alternative communication routes when face-to-face communication fails. Many respondents described different ways in which these failures occurred. For example, one caregiver mentioned a conflict with a nutritionist regarding her son’s diet. The nutritionist “did not listen to what I had to say”, and ultimately the caregiver “got irritated and took matter[s] into my own hands” (C91). In this case, when in-person communication broke down, an electronic system could have allowed C91 to non-confrontationally request support or opinions from another clinician. Another caregiver discussed a time where face-to-face communication with her son’s providers actually caused increased worry and concern: “The resident came in [and] was asking questions that were causing me alarm. It was making me worried about my son and if there was something going on that they weren’t telling me…” (C51). In situations like this, when there is increased potential for miscommunication, or when there is an evident lack of information, inpatient tools can serve as a mechanism for patients or caregivers to request further details and ask follow-up questions when needed.
Limitations and Future Work
Individuals who were not eligible, not well enough to provide consent or answer survey questions, or declined participation were not given the survey. Because of this constraint, other types of undesirable events could have been missed. Three participants responded to our survey more than once, because they expressed a desire to answer questions about multiple undesirable events. Although this introduced a demographic redundancy in our data set, we independently tracked the number of unique individuals we approached during this study, and have reported the differences in these values. A selection bias could influence our results, as respondents were not offered compensation for their participation, and those who were frustrated with their situation might have had increased motivation to participate. Our sample size and single hospital location also limits the generalizability of our results. Pediatric patients were less likely to complete our survey due to illness or ineligibility. Despite their reduced involvement in our study, the diverse experiences of this population indicates an area of further exploration. A better understanding of the perceived usefulness of existing inpatient technologies, and their current or potential role in preventing medical errors is also needed.
Conclusion
In this paper, we presented the results of a survey asking pediatric inpatients and their caregivers about their prior experiences with undesirable events. We categorized the perceived types of events and illustrated their relationship with outcomes that patients and caregivers described. Our findings demonstrate that patients and caregivers have a broad definition of undesirable events, have many unmet information needs that they feel might help prevent such events, and have specific preferences for receiving this information. Based on these results, we made recommendations for future iterations of patient engagement technology, which has the potential to increase support for patients and caregivers in becoming active participants in their healthcare, and help reduce the tragic toll of medical errors.
Acknowledgements
We would like to thank each of our participants for taking time during their hospital stay to take part in this study, the Patients as Safeguards research team, Kathryn Nickel, and members of the Outcomes Assessment Program at Seattle Children’s Hospital (Stephanie Hillman, Emily Dehmer, Jessica Kowalchuck, Kristine Lee, Neil Panlasigui, and Breanna Dolan) for their partnership and support. This research study was primarily funded by the Agency for Healthcare Research and Quality (AHRQ) grant #1R01HS022894, with additional support from the National Library of Medicine Biomedical and Health Informatics Training Grant #T15LM007442.
References
- 1.To Err Is Human: Building a Safer Health System. Natl Acad Press; 2000. Mar, pp. 1–287. [PubMed] [Google Scholar]
- 2.Crossing the Quality Chasm: A New Health System for the 21st Century. Natl Acad Press; 2001. Mar, pp. 1–8. [PubMed] [Google Scholar]
- 3.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013 Sep;9(3):122–8. doi: 10.1097/PTS.0b013e3182948a69. [DOI] [PubMed] [Google Scholar]
- 4.Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016 May 3;353:i2139. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 5.Carlesso LC, Cairney J, Dolovich L, Hoogenes J. Defining adverse events in manual therapy: An exploratory qualitative analysis of the patient perspective. Man Ther. 2011;16(5):440–6. doi: 10.1016/j.math.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Weissman JS, Schneider EC, Weingart SN, Epstein AM, David-Kasdan J, Feibelmann S, et al. Comparing Patient-Reported Hospital Adverse Events with Medical Record Review: Do Patients Know Something That Hospitals Do Not? Ann Intern Med. American College of Physicians. 2008 Jul;149(2):100. doi: 10.7326/0003-4819-149-2-200807150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Agoritsas T, Bovier P a, Perneger T V. Patient reports of undesirable events during hospitalization. J Gen Intern Med. 2005;20(10):922–8. doi: 10.1111/j.1525-1497.2005.0225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis RE, Sevdalis N, Neale G, Massey R, Vincent C a. Hospital patients’ reports of medical errors and undesirable events in their health care. J Eval Clin Pract. 2013;19(5):875–81. doi: 10.1111/j.1365-2753.2012.01867.x. [DOI] [PubMed] [Google Scholar]
- 9.Schwappach DLB. “Against the silence”: development and first results of a patient survey to assess experiences of safety-related events in hospital. BMC Health Serv Res. 2008;8:59. doi: 10.1186/1472-6963-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solberg LI, Asche SE, Averbeck BM, Hayek AM, Schmitt KG, Lindquist TC, et al. Can patient safety be measured by surveys of patient experiences? Jt Comm J Qual Patient Saf. 2008;34(5):266–74. doi: 10.1016/s1553-7250(08)34033-1. [DOI] [PubMed] [Google Scholar]
- 11.Harrison R, Walton M, Manias E, Smith–Merry J, Kelly P, Iedema R, et al. The missing evidence: a systematic review of patients’ experiences of adverse events in health care. Int J Qual Heal Care. 2015:1–19. doi: 10.1093/intqhc/mzv075. [DOI] [PubMed] [Google Scholar]
- 12.Vincent CA, Coulter A. Patient safety: what about the patient? Qual Saf Heal Care. BMJ Publishing Group Ltd. 2002 Mar;11(1):76–80. doi: 10.1136/qhc.11.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Unruh KT, Pratt W. Patients as actors: the patient’s role in detecting, preventing, and recovering from medical errors. Int J Med Inform. 2007 Jun;76(1):S236–44. doi: 10.1016/j.ijmedinf.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 14.van den Bemt PMLA, Egberts ACG, Lenderink AW, Verzijl JM, Simons KA, van der Pol WSCJM, et al. Adverse drug events in hospitalized patients. Eur J Clin Pharmacol. Springer-Verlag. 1999 Apr;55(2):155–8. doi: 10.1007/s002280050611. [DOI] [PubMed] [Google Scholar]
- 15.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The Incidence and Severity of Adverse Events Affecting Patients after Discharge from the Hospital. Ann Intern Med. American College of Physicians. 2003 Feb 4;138(3) doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 16.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. British Medical Journal Publishing Group. 2013;3(1):1–18. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prey JE, Woollen J, Wilcox L, Sackeim AD, Hripcsak G, Bakken S, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc. 2014;21(4):742–50. doi: 10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bers MU, Gonzalez-Heydrich J, DeMaso DR. Use of a Computer-Based Application in a Pediatric Hemodialysis Unit: A Pilot Study. J Am Acad Child Adolesc Psychiatry. 2003;42(4):493–6. doi: 10.1097/01.CHI.0000046810.95464.68. [DOI] [PubMed] [Google Scholar]
- 19.Anthony R, Ritter M, Davis R, Hitchings K, Capuano TA, Mawji Z. Lehigh Valley Hospital: engaging patients and families. Jt Comm J Qual patient Saf. 2005 Oct;31(10):566–72. doi: 10.1016/s1553-7250(05)31074-9. [DOI] [PubMed] [Google Scholar]
- 20.Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD. Tablet computers for hospitalized patients: A pilot study to improve inpatient engagement. J Hosp Med. 2014;9(6):396–9. doi: 10.1002/jhm.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dykes PC, Stade D, Dalal A, Clements M, Collins S, Mse FC, et al. Strategies for Managing Mobile Devices for Use by Hospitalized Inpatients. AMIA Annu Symp Proc; American Medical Informatics Association; 2015. pp. 522–31. [PMC free article] [PubMed] [Google Scholar]
- 22.Strauss Anselm L, Corbin JM. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 1998:431. [Google Scholar]
- 23.Kendall L, Mishra SR, Pollack A, Aaronson B, Pratt W. Making background work visible: opportunities to address patient information needs in the hospital. AMIA Annu Symp Proc. 2015;201(5):1957–66. [PMC free article] [PubMed] [Google Scholar]
- 24.Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Informatics Assoc. 2016:1–9. doi: 10.1093/jamia/ocw070. [DOI] [PMC free article] [PubMed] [Google Scholar]


