Abstract
The U.S. Department of Veterans Affairs (VA) Veteran Health Information Exchange (VHIE, formerly Virtual Lifetime Electronic Record, or VLER) Retail Immunization Coordination Project established a partnership between VA and Walgreens to empower Veterans to elect to receive their immunizations at a local Walgreens, which might be located closer to their home than their nearest VA facility. Analysis of Veterans immunized at Walgreens between September 2014 and January 2015 showed that 64% of study Veterans now traveled <5 miles to receive their immunization, 12% of study Veterans traveled between 5 to 10 miles, and 24% of study Veterans traveled more than 10 miles. In addition, we note that 93% of Veterans traveled less than 54 miles, the average distance rural Veterans traveled to the nearest VA facility. We conclude that the VHIE Retail Immunization Coordination Project improved Veteran access to healthcare and discuss future directions of this effort.
Introduction
VA influenza immunization rates for enrolled Veterans aged 65 years or older are currently above national averages (e.g., in 2011/2012, VA immunization rate was 77% as compared to 65% for the general population according to VHA Public Health data). However, VA remains below its target objective of 90%. Many Veterans are currently already receiving immunizations through non-VA providers (e.g., employers, health outreach fairs, other clinics) and self-report their immunization history throughout the year to VA. With immunizations available at retail providers such as Rite Aid, Walgreens, CVS, etc. growing in popularity, VA is interested in determining how the convenience of retail providers, combined with automatically entered health information through interoperability, can be used to continue to improve the completeness and accuracy of the Veteran’s electronic health record and VA’s ability to accurately measure immunization rates for the target population, while boosting immunization rates of the target population overall.
VA launched the Retail Immunization Care Coordination Program (hereafter the immunization program) in October of 2013. The immunization program was structured in three phases:
Phase 1 (2013-2014): View only, query (Data was manually synched up by onsite VA staff following a clinical reminder. Data was transmitted from Walgreens, but onsite staff had to populate the patient record with immunization data.) It is also structured as a pilot program limited to Veterans Integrated Service Network (VISN) 8 throughout the state of Florida.
Phase 2 (2014+): Immunization data are automatically populating the VA patient record in CPRS. Phase 2 also extending the immunization program to a national rollout.
Phase 3 (TBD): Data will be integrated with Immunization Applications.
The immunization program allowed Veteran patients the option of choosing a Walgreens retail pharmacy to get a flu shot. Walgreens is authorized to administer the influenza vaccinations to the patients who are VA health care-enrolled and who voluntarily choose to participate in the program. In addition, many Veterans have coverage through Medicare or commercial insurance.
Immunization information of Veterans is available from Walgreens locations and retrieved for VA providers to review through VLER Health and eHealth Exchange, using the existing query and retrieve capability of VLER Health Exchange, and incorporates standard security measures to protect patient confidentiality. Participating Veterans in the VA Retail Immunization Care Coordination Program can ensure that their VA providers have complete and accurate information about the flu shot they receive, including the date, the type of vaccination, and the lot number. Once the Veteran volunteers to participate, the vaccination record is transmitted to the patient’s VA electronic health record and is available for viewing via the VLER Health Exchange. VA providers will no longer have to rely on patient self-reported immunization data or unreliable paper records.
The goals of these efforts are to improve the completeness and accuracy of the Veteran’s electronic health record and to improve VA’s ability to accurately measure immunization rates for the target population, while boosting immunization rates of the target population overall. The immunization program expects to see both administrative impacts and clinical impacts from coordinating influenza vaccination with retail pharmacies (initially Walgreens).
Administratively, the retail influenza vaccination data will improve VA clinical documentation. This will eliminate the clinical reminders shown to VA clinicians for Veterans who were already vaccinated at retail sites such as Walgreens, and reduce cognitive load and alert fatigue to clinicians. Also, this will reduce unnecessary mails and outreach to Veterans for immunization reminders and self-reports once they are immunized. There will also be administrative savings from avoiding these wasted outreach activities.
Clinically, the program will provide real time influenza vaccination data to VA, which will help focus public health efforts to target Veterans who have not been immunized, reducing reminder fatigue and waste for Veterans who were already immunized. In addition, this is expected to add a large number of influenza vaccination sites and increased convenience for Veterans.
Finally, with greater and earlier influenza vaccination, there will be healthcare utilization impacts with reduced influenza-related phone calls, outpatient visits, and admissions. Influenza laboratory testing will also be reduced.
Objective
This paper covers the initial analyses of phase 2 of the immunization project, as the scope expanded nationally. Goals for the immunization pilot include the following: increased access to vaccinations by Veterans, enhanced vaccination rates, and improved data collection. Internal analysis of the Phase 1 results suggested that the immunization project is improving Veteran access and reaching a new population of Veterans. Therefore, Phase 2 analyses focused on confirming, identifying, and quantifying the impact on Veteran access. Phase 2 analyses leveraged Geographic Information System (GIS) to analyze geographic distribution of Walgreen sites providing immunization services, existing VA facilities, and residence of affected Veteran populations. The goal is to assist VA leaders and stakeholders to visualize how the immunization project is expanding Veteran Access.
Methods
We considered all Walgreens claims submitted to VA for the months of September 2014 through March 2015. The claims were matched against VA’s master patient index to confirm Veteran eligibility using patient matching algorithms and criteria according to established VA practices. Only claims with a confirmed “match” were considered in this analysis.
For each confirmed claim, travel distance was calculated between the Veteran’s home and the Walgreens store administering the immunization. The street addresses of the Walgreens stores were provided by the Walgreens national office. Due to Veteran privacy concerns, only the Veteran’s home zip code reported on the Walgreens claim was available for analysis. Therefore, travel distances were calculated from the centroid of the Veteran’s home zip code.1 The ArcGIS Desktop program2 from the Environmental Systems Research Institute (ESRI) was used to calculate the straight-line distance from the centroid of the Veteran’s home zip code to the Walgreens location where they received their immunization. Straight-line, or Euclidean distance is the minimum distance between points.
In addition, we also retrieved the location of the VA facility the Veteran frequents, based on the Veteran’s VA records and site ID, and calculated the corresponding travel distance using the same methodology as above. For Veterans who frequents more than one VA facility, the distances to each VA were calculated, and then averaged travel distance was used for the comparison.
To estimate the travel distances saved by Veterans, we only considered situations where the choice of being immunized at Walgreens led to a reduction in travel. Since these Veterans were eligible for free immunization at VA and had already received care at VA in the past (as shown by the presence of their medical records), any Veteran who traveled further than their usual VA facility to visit a Walgreens store further away were clearly not motivated to reduce travel distances, and had elected to visit Walgreens for a different reason. We also examined each Veteran’s VA visit records to determine whether they had VA visits during the influenza season before and after their Walgreens immunization.
Results
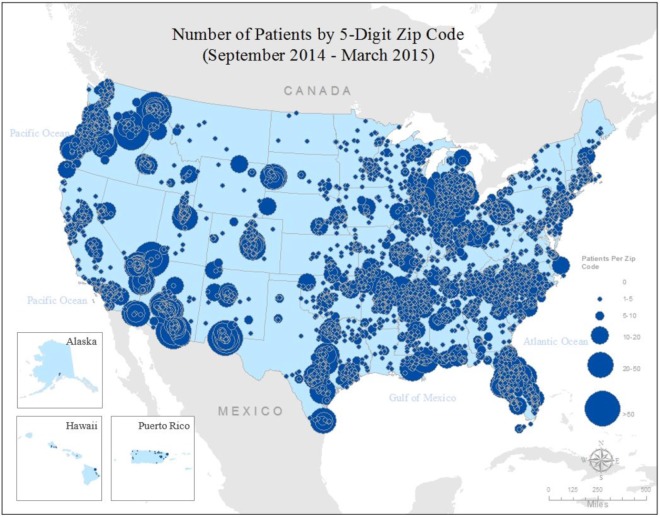
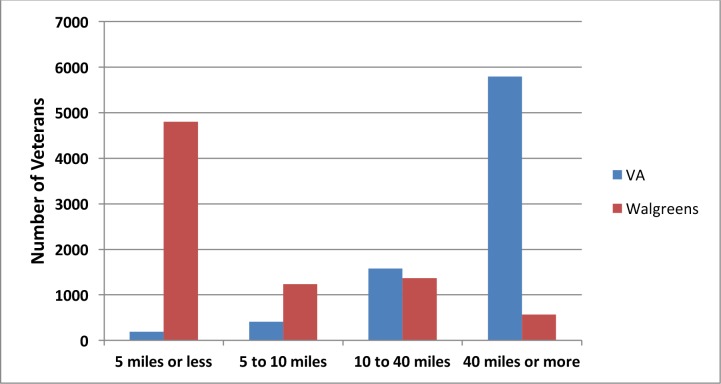
For the seven-month period between September 2014 and March 2015, there were 8,809 confirmed claims submitted by Walgreens for immunizing Veterans. Of these 8,809 claims, 827 (9.4%) had poorly formatted zip codes (neither 5 nor 9 digits), unused zip codes, or unused Walgreens store numbers. The remaining 7,982 claims were mapped to the Veteran’s home zip code (Figure 1) and used for the following travel distance analysis. Straight-line distances were calculated for each validated claim from the centroid of the Veteran’s zip code to the specific Walgreens location and the VA facilities the Veteran frequents. A further 473 (5.3%) claims where the Walgreens site visited was further away than the Veteran’s usual VA site of care. The results are shown in Figure 2. As can be seen from Figure 2, travel distances to Walgreens for these Veterans are usually 5 miles or less, whereas travel distances to VA facilities are usually 40 miles or more. After excluding Veterans who traveled to distant Walgreens for immunizations, who were presumably not motivated by reductions in travel distances, we found that during the 2014-2015 influenza season, these Veterans avoided a total of 2,055,240 miles by traveling to a near-by Walgreens store as opposed to their usual VA facility.
Figure 1.
Number of Veterans by 5-Digit Zip Code, September 2014 to March 2015
Figure 2.
Veteran travel distances to VA versus Walgreens
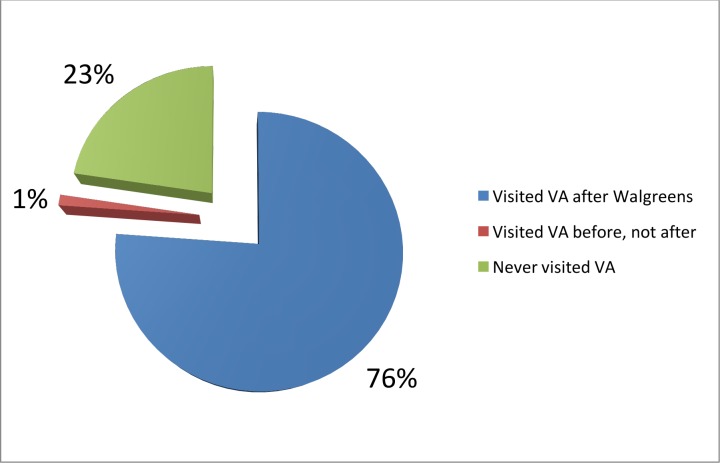
When these Veterans’ VA visit records were review, 55% of the Veterans had one or more visits to VA facilities between the start of the influenza season on September 1, 2014 and the day when they were immunized at Walgreens. These were missed opportunities to vaccinate Veterans earlier. Further comparison of the Walgreen visits and VA visits were graphed below in Figure 3. Seventy-six percent (76%) of Veterans immunized at Walgreens visited a VA facility after their Walgreens immunization during the 2014-2015 influenza season. However, there was an average of 45 calendar days between their Walgreens immunization and the following VA visit; this represented days of extra protection against influenza and related illnesses even when compared to the ideal case that all Veterans were immunized at their next VA visit. Of the other 24% of Veterans who did not visit a VA facility during the influenza season after their Walgreens immunization, one percent (1%, the red slice in Figure 3) did visit VA prior to their Walgreens immunization; these were lost opportunities that VA never had a chance to correct. The remaining 23% never visited a VA facility during the entire 2014-2015 influenza season. It is quite possible that these 23% of Veterans would never have been immunized without this Retail Immunization Care Coordination program. At the very least, it is certain that VA would never receive the immunization records of these Veterans without the Retail Immunization Care Coordination program, and they will erroneously remain on the unimmunized list for VA’s population health programs.
Figure 3.
Proportions of Veterans who visited VA before or after Walgreens
Discussion
This study applied GIS analysis techniques to the immunization claims submitted by Walgreens to VA in two ways: graphic visualization of geospatial distribution, and quantitative analysis of travel distances. Each claim used for this analysis represented a confirmed Veteran whose demographic information matched closely to the records in VA’s Master Veteran Index (MVI) database. In addition, the Veterans’ VA visit records were compared against their Walgreen immunization records to examine their chronological relationships. While the study is limited by the use of the Veteran’s home zip centroid and straight-line distance, these limitations applied equally to both Walgreens and VA facilities, so the impact on the travel distances compared should be minimal, and if anything, probably resulted in a conservative, lower-bound estimates of distance traveled.
Whereas Phase 1 of the immunization program was limited to VISN 8 in the State of Florida, the claims analyzed were from Phase 2 during national deployment. Visual inspection of Figure 1 confirmed the national nature of phase 2 of the immunization program, with activities shown in every state, including Alaska and Hawaii. In addition, it should be observed that several sites appeared to have higher activities than Florida, the original pilot sites. This confirmed the success of the Phase 1 pilot, and the resulting decision to deploy the immunization program nationally.
In addition, the distances traveled by these Veterans to receive immunization at Walgreens were estimated and detailed in Figure 2. It can be seen that the great majority of Veterans (73%) traveled more than 40 miles to their usual VA facilities, the distance under which the Veteran Access, Choice, and Accountability Act of 2014 (VACAA) used to define excess travel. While this is not a strict determination of VACAA eligibility, since VACAA used nearest VA facility whereas this study used the VA facilities the Veterans frequent, it nonetheless illustrated the significant travel burden for this group of Veterans. While this study did not include a direct comparison against the distances these Veterans would travel to the nearest VA medical facilities, comparison against published literature presented a very favorable picture. In 2006, Probst and her colleagues analyzed the 2001 National Household Travel Survey (NHTS) data collected by the US Department of Transportation, and found that national average distance traveled for medical and dental care was 10.2 miles.1 In 2010, Jeremy Mattson reported that the median distanced traveled for healthcare services is 5 miles for routine health checkups, 9 miles for chronic healthcare visits, and 5 miles for emergency care.2 In contrast to the travel distance to VA facilities, only 7% of Veterans traveled more than 40 miles to Walgreens, seventeen percent (17%) traveled between 10 to 40 miles, fifteen percent (15%) traveled between 5 to 10 miles, and 60% traveled less than 5 miles. Using standard IRS mileage rates of 55 cents per mile for the estimated 2,055,240 miles saved by Veterans from travelling to a near-by Walgreens store for influenza vaccination, this is a savings of $1,182,000 ($0.55/mile x 2,055,240 miles) for Veterans. This study did not attempt to determine or estimate proportion of Veterans for whom VA provided transportation, travel assistance or reimbursements, which would further increase total travel cost and VA-specific costs.
As illustrated in Figure 3, 2,051 Veterans who never visited VA during the 2014-2015 influenza season were immunized at Walgreens, in addition, 6,908 Veterans were immunized earlier than their next VA appointment, gaining 323,328 days of protection against influenza and related illnesses. Based on the estimates reported by Duncan et al. in their cost benefits model3, we estimated societal savings of $663.56 and $125.24 respectively for senior vs. adult Veterans who would not have been immunized otherwise. Using the same data set from the Duncan model, we also estimated the marginal benefit of earlier immunization at $3.16/day and $0.60/day respectively for senior vs. adult Veterans. Applying these estimated for the 2,051 Veterans (759 seniors, 1292 adults) who never visited VA during the 2014-2015 influenza season resulted in estimated societal savings of $665,452 (759 x $663.56 + 1292 x $125.24) and the 323,328 day of earlier influenza protection resulted in $499,492 (119,631 senior days x $3.16/day + 203,697 adult-days x $0.60/day) estimated savings.
Tallying the three sources of Veteran, VA, and societal savings from the Retail Immunization Care Coordination program during the 2014-2015 influenza season, we found a total estimated saving of $2,346,000. This compares quite favorable to the total VA expenditure for the 2014-2015 Retail Immunization Care Coordination program of $250,000, a mere 10.6% of the estimated savings.
Conclusion
By applying GIS analysis techniques, we were able to show how Phase 2 of VA’s Retail Immunization Coordination Program with Walgreens is improving Veteran access and furthering Veteran health. We first demonstrated how Phase 2 of the immunization program had improved Veteran access by expanding the coverage beyond Florida to cover every state in the nation. We then estimated savings of $1,182,000 for Veterans from reducing more than 2 million miles in travel. We also estimated more than $1 million savings from earlier immunization and reaching unserved Veterans. We conclude that Phase 2 of the immunization program had improved Veteran access to healthcare, and VA should continue to expand the program with other private sector partners and additional services.
References
- 1.Probst JC, Laditka SB, Wang JY, et al. Columbus, SC: South Carolina Rural Health Research Center; 2006. Mode of travel and actual distance traveled for medical or dental care by rural and urban residents. [Google Scholar]
- 2.Mattson J. Fargo, ND: Small Urban & Rural Transit Center, Upper Great Plains Transportation Institute, North Dakota State University; 2010. Transportation, distance, and health care utilization for older adults in rural and small urban areas. [Google Scholar]
- 3.Duncan IG, Taitel MS, Zhang J, et al. Planning influenza vaccination programs: a cost benefit model. Cost Eff Resour Alloc. 2012;10(1):10. doi: 10.1186/1478-7547-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]