Abstract
Medication non-adherence is a pressing concern among seniors, leading to a lower quality of life and higher healthcare costs. While mobile applications provide a viable medium for medication management, their utility can be limited without tackling the specific needs of seniors and facilitating the active involvement of care providers. To address these limitations, we are developing a tablet-based application designed specifically for seniors to track their medications and a web portal for their care providers to track medication adherence. In collaboration with a local Aging in Place program, we conducted a three-month study with sixteen participants from an independent living facility. Our study found that the application helped participants to effectively track their medications and improved their sense of wellbeing. Our findings highlight the importance of catering to the needs of seniors and of involving care providers in this process, with specific recommendations for the development of future medication management applications.
Introduction
Seniors take on average about seven medications per day,1 representing the highest number of prescribed medications and the most complex medical regime compared to any age group.2 While this complexity is a natural response to chronic disease conditions that are increasingly prevalent as one ages,2,3 it also brings with it a higher risk of medication non-adherence.4–6 Medication non-adherence increases from an average of approximately 20% for patients taking one medication daily to over 50% for those taking medications four times per day.7,8 It not only results in unalleviated disease conditions, but can also lead to an increased risk of comorbidities and longer hospital stays. Ultimately, it is responsible for approximately 125,000 deaths per year9 at an annual cost of roughly $100 billion.10
Mobile applications have been proposed as promising tools for mitigating some of the challenges of medication nonadherence by providing seniors with tracking, organizational, and reminder supports.11, 12 Unfortunately, there are several reasons why such applications continue to have limited impact on the aging population. The most pronounced problem is that the vast majority of these applications are designed for technologically savvy individuals, fundamentally limiting their use by a senior population that is often slow to adopt new technology.13 Further, despite the integral role that communication between patients and care providers plays in providing healthcare workers with the root causes of non-adherence,14 these applications generally have very limited ability—and often no ability—to connect the patient with care providers. These factors severally limit the practical use of these applications by seniors.
We are developing eSeniorCare, a comprehensive system targeting quality of life, comprising both a tablet application and a web portal. While the application has an extensive set of functions, in this paper we focus specifically on the application’s medication adherence component. This component assists seniors in tracking their medications by providing reminders for when medication is due and by recording the intake of medications. It also provides a communication mechanism with the care provider. The web portal helps care provider teams to communicate with seniors about missed medications, changes, and refills. By building the system around these components, eSeniorCare has been carefully designed with the features needed to empower seniors to take charge of their medication management and to enable care providers to support the medication adherence of their patients.
To investigate the impact of eSeniorCare on medication adherence, we conducted a pilot study of the system at a local independent living facility catering to a low-income senior population. The care provider team at this facility consists of a nurse and Resident Life Health Administrator (who we collectively refer to as RLHA) under the supervision of Memorial Hospital of South Bend (part of Beacon Health System). We present the design, development, and evaluation of the system’s medication management component to investigate two main research questions (RQ1 and RQ2) and an exploratory research question (RQ3):
RQ1: How do the participants use the application to track their medications?
RQ2: How does the application impact participants’ quality of life, specifically as it pertains to health?
RQ3: What influence does the application have on participants’ knowledge of their medication regimes?
Related Work
There are various methods for measuring medication adherence. Some of the methods measure adherence directly, while others attempt to infer adherence through indirect (proxy) indicators. Direct methods include measurements that determine drug metabolites, biomarkers or additionally applied marker molecules in biological fluids (e.g., plasma and urine), and direct observation therapy.15 While these methods can provide fairly accurate measurements of adherence, they are not scalable, incur high costs, and tend to be labor intensive. Indirect methods include electronic pill box cap monitoring, pill counts, self-reporting, and pharmacy refill systems.16 While these indirect methods are fairly inexpensive, their reliability depends on the individual’s responses. For example, an individual can open the electronic pillbox for a medication despite not physically taking it, thereby providing an overestimation of adherence.
The increasing popularity of smartphones has led to the development of mobile applications for medication management. These applications typically provide reminders for when a medication is due, information on medication dosage history, and medication refill alerts.17–19 While some of these applications have been developed without a focus on any particular condition, many have been developed to cater to chronic disease conditions such as hypertension, diabetes, and asthma. The potential of these mobile applications to address the challenges of medication management has been encouraging, with several studies demonstrating that they can be effective in improving medication adherence.20,21
Despite their potential, very few mobile applications have been developed for or targeted at seniors.22–25 One such application, ALICE, provides medication reminders and can send messages to the care providers in the case of nonresponse to these reminders.22 However, almost none of these applications track the medications taken as needed (PRN),26 and many provide no or non-real-time information regarding missed medications. Further, few of these applications support a direct connection between the patient and care provider. As a result, unlike eSeniorCare, these applications do not enable intervention by the care provider in the case of medication non-adherence. We have also designed eSeniorCare with several features practically useful for medication management, such as care provider follow-up in case of missed medications and PRN intake, that are missing from currently available mobile applications.
Application Design
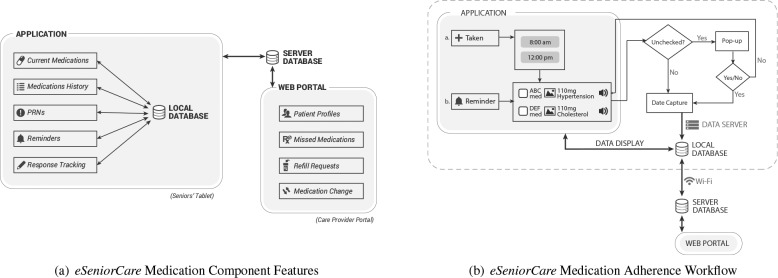
We are developing a tablet-based Android application called eSeniorCare that focuses specifically on the components of quality of life for seniors. In this section, we provide an overview of the features provided by the application’s medication management component, as illustrated in Figure 1(a).
Figure 1.
(a) Features of eSeniorCare’s medication component. (b) eSeniorCare’s medication adherence workflow. Together, these describe how patients may interact with the medication component of the application and the interactions that occur between the application, web portal, and databases to deliver care providers with up-to-date information on participants’ medication adherence.
Medication Reminders. For each participant, eSeniorCare automatically generates reminders for all prescribed medications based on the prescription data that is queried from the encrypted local database (Figure 1(b)). A reminder is scheduled five minutes before the prescribed dosage time. For each medication due at the dosage time, the reminder screen displays the following information: (a) medication name, (b) dosage information (i.e., quantity and unit), (c) associated treatment condition, (d) audio icon to speak out the medication’s name, (e) image of the medication, and (f) a checkbox that the user must check to confirm intake. If the checkbox associated with any medication is not checked, the user is asked to validate the response. The user can also view a magnified version of the image of the pill.
Medication History. For each participant, all current and previously prescribed medications are listed, along with a status—active, dosage modified, or discontinued—for each medication. This feature can help participants improve communication with their physicians.27
Current Medications. The application provides participants with comprehensive information about their current medications, along with the frequency and dosage of each medication and the corresponding treatment condition. The purpose of this feature is to empower the participants in maintaining an aggregated list of prescribed medications, which may be used as a quick reference for the patient or clinician during medical visits.
PRN. Pro re nata (PRN) medications are taken whenever the need arises. All PRNs are listed here, along with corresponding disease diagnoses, and dosage directions. Due to their potential impact on patient health, the inclusion of PRN medications is an important feature that has traditionally been absent from mobile health applications.28
Medication Taken. The participants may respond to a medication reminder even after it has disappeared by tapping the “Taken” button, as shown in Figure 1(b). The participant is then presented with a list of dosage times before the current system time for which responses have not yet been entered. If a participant selects a particular dosage time, he or she is presented with the appropriate medication reminder. This feature is typically unavailable in the mobile health applications.28
Medication Change. A participant can inform the RLHA to a change in his or her medication by clicking this button. The RLHA receives information on the medication change via the web portal. The RLHA then follows up on this information by updating the participant’s medication information.
RLHA Portal for Monitoring Adherence. A participant’s response or non-response to the reminders is reported to the RLHAs via the web portal, allowing the RLHA to follow up with the participant to resolve any issues and to provide appropriate motivation.29 To validate the participant responses for medication reminders, we implemented the “Refill Medications” button that provides a list of the refillable medications. They can pick the ones for which they require a refill. We calculate an estimate of the refill date for each refillable medication based on the initial pill count and the dosage. If the requested date does not match the estimated refill date, the RLHA is notified through the portal.
Missed medication is marked “Not Taken”; otherwise, it is marked “Taken”. In order to track the workflow of a missed medication and for ease of maintenance, we added a status field. When no action has been taken by the RLHA, the status is “Unread”. After the RLHA has followed up with the participant, the status is changed to “Resolved” and a reason is entered for the missed medication. The RLHA may use the portal to create new users, populate and maintain their medication profiles.
Offline Usage. Our study site has Wi-Fi connectivity that is limited to the core of the building and community areas. As a result, the majority of the participants did not have Wi-Fi connectivity in their apartments. To account for the intermittent connectivity, the tablet application has a local database—located in the tablet’s encrypted internal memory—that enables the desired offline functioning of the application. The application is only required to connect to Wi-Fi once a day for synchronization with the remote server.
Methods
We conducted a study of eSeniorCare in collaboration with the Aging in Place (AiP) program designed by the Community Health Enhancement (CHE) vision of the Memorial Hospital of South Bend. The program operates in several local independent living facilities with a mixed-income senior population, and aims to positively impact wellness and quality of life for its participants while they are living in their current home settings. As part of this aim, AiP is actively interested in the development of a low-cost solution to help its participants improve adherence to their medication regimens.
Overview. We held an interest meeting with residents at the facility to introduce the purpose of the study and requirements of participation. We only accepted residents who were cognitively intact, determined by the St. Louis University Mental Status Exam (SLUMS), a 30-point screening questionnaire that tests for orientation, memory, attention, and executive functions;30 fluent in English; and had good vision. Finally, participation was restricted to individuals with at least one chronic condition and one actively prescribed medication.
Each resident who qualified for the study, based on the selection criteria described above, was given an encrypted, password-protected 7-inch Samsung Galaxy Tab 2 tablet device. Participants were expected to carry the device with them at all times and to manage their medications as reasonably directed by the device. Those who participated for the full duration of the study were permitted to keep the tablet.
Participants. We recruited sixteen participants with an average age of 66 years (SD = 9.2). Five participants were male and eleven were female. Twelve participants identified themselves as African American/Black, three as non-Hispanic White, and one as other. One participant was married, six were divorced, two were widowed, two were separated, and five never married. One participant was employed, one was looking for work, seven were retired, and four indicated that they could not work. Two participants had between 9th and 11th grade education, four had completed high school, eight had 1-3 years of technical school, one was a college graduate, and one had an advanced degree. The number of medications per participant ranged from 1 to 13, with an average of 6-7 medications.
Study Design. We conducted the study over a period three months to evaluate the RQ1, RQ2, and RQ3. The participants were required to respond to the medication reminders, report PRN intake, and report changes in medication. To familiarize participants with the application, one-on-one training with the application was provided at the beginning of the study. The RLHA were instructed to access the web portal on alternate days to track the medication responses. In the case of missed medication, a registered nurse followed up with the participant and took appropriate action.
Evaluation Metrics. To answer our research questions, we used the following information:
Medication Usage Logs (MUL): Participant responses to medication reminders, reported changes to prescribed medication, and incidences of PRN were recorded in a database.
Medication Adherence Questionnaire (MAQ): A questionnaire designed based on the Brief Medical Questionnaire (BMQ)31 for measuring medication adherence. Studies have shown that if a patient is better aware of her or his medications and diseases, then he or she will have an improved adherence to his or her medication regime.15 We administered a paper-based MAQ both at the beginning and at the end of the study. Table 1 provides an outline of the questionnaire. The questions in MAQ are tailored to the prescription information provided by the participants. The response(s) for each question are matched with the prescription information.
Final Feedback Questionnaire (FFQ): A 38-point post-study feedback questionnaire for evaluating the usability of the application and the effectiveness of the study. Sample questions are included in Table 2. The questionnaire was administered both on paper and online at the end of the study.
SF12v2: A 12-item health survey provided by Quality Metric to measure the general health (physical and mental) of an individual and health-related quality of life, and well-validated for the aging population.32 It measures the health status in eight functional domains: bodily pain, physical function, role physical, role emotional, mental health, vitality, social function, and general health. These domains are further collapsed into a physical component summary (PCS) and a mental component summary (MCS). The survey was administered on paper at the beginning and end of the study.
Table 1.
Medication Adherence Questionnaire (MAQ) provided to participants.
| Description | Options |
|---|---|
| Match the diseases diagnosed and medications taken. | • List of diagnoses |
| • List of medications | |
| Fill out the following details [options] for 2 medications. | • Diagnosis |
| • Dosage information (quantity per intake and number of times per day) | |
| • Identification (color, name, size, pill bottle / container for daily use) | |
| How many pills do you take per day? | No options provided |
| How do you remind yourself of the medications to be taken? | No options provided |
Table 2.
Questions and response trends for the Final Feedback Questionnaire.
| Num. | Question Text | Feedback Trend |
|---|---|---|
| Q1 | eSeniorCare made me more aware of my health. |  |
| Q2 | I felt an improvement in my health/well-being as a result of eSeniorCare |  |
| Q3 | eSeniorCarehelped me to know my medications: dosage, purpose for medication etc. | 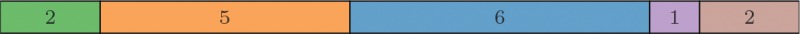 |
| Q4 | Overall,eSeniorCarehelped me manage my medications. |  |
| Q5 | I showedeSeniorCare to my physician. |  |
| Q6 | eSeniorCare showed my correct medication information. |  |
| Q7 | I would like to enter my own medications. |  |
Note: The bar segments from left to right correspond to the responses “Strongly Agree” (green), “Agree” (orange), “Neither Disagree Nor Agree” (blue), “Disagree” (purple), and “Strongly Disagree” (brown). For each segment, the value denotes the number of participants with the response, while its length denotes the proportion.
Results
In this section, we provide details of the results from our study of eSeniorCare. Our results come from information gathered by tracking how participants used the application over the course of the study, as well as from questionnaires, administered at the beginning of the study and at its conclusion.
RQ1: How do participants use eSeniorCare to track their medications?
A majority of the participants (n = 12) initially faced difficulties in maneuvering the touch screen (sensitivity, pointing, and dragging)33 and with the tablet itself due to a lack of technological fluency and unfamiliarity with the tablet. Several hour-long group workshops and one-on-one training sessions helped familiarize participants with the technology and application. To help overcome usability challenges with the touchscreen, we provided each participant with a stylus. We also provided printed manuals for eSeniorCare application. These activities were substantial in helping to foster user engagement, with participants expressing a strong desire for the study to continue as it approached its conclusion.
The FFQ included several questions to assess how participants used the application to track their medications. All but one of the participants reported that the application showed the correct medications (Table 2: Q6). We note that one participant also made a considerable number of changes to his or her medication list, so it could be a function of that artifact. Around 50% of the participants reported that they showed the application to their physician (Table 2: Q5). More than 65% of the participants reported that they felt the application helped them to manage their medications (Table 2: Q4), and about 50% of the participants reported that they felt the application made them more aware of their health (Table 2: Q1).
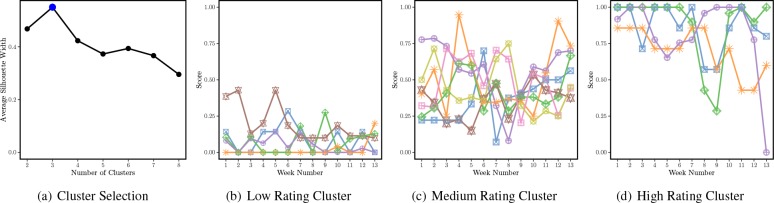
Medication Reminders. We used the MUL to define a rating system for tracking the frequency of medication responses for each participant. A rating of 1 was given if the participant acknowledged a medication reminder. The maximum possible daily rating for the participant is then equal to the number of times per day that a medication is due to be taken. We calculated the weekly rating as the sum of the participant’s daily ratings for a week divided by the sum of the participant’s maximum possible daily rating for a week (thus taking into account the variation in the number of daily reminders among the participants). We averaged the weekly rating to obtain the average weekly rating (AWR). To identify similar usage patterns among participants, we performed k-medoids clustering34 on the participants’ weekly ratings, using the measure of silhouette width35 to evaluate the number of clusters. Based on the maximum average silhouette width, we discovered three distinguishable clusters of participants, illustrated in Figure 2(a). The majority of the participants (n = 7) had moderate usage, shown in Figure 2(b), with AWR ranging from 0.52 to 0.73. The remaining participants were split between low-usage ratings (n = 5), shown in Figure 2(c), with AWR less than 0.28, and high-usage ratings (n = 4), shown in Figure 2(d), with AWR greater than 0.93.
Figure 2.
Cluster analysis based on participants’ weekly ratings. (a) Illustrates the average silhouette width (Y-axis)35 as a function of the number of clusters (X-axis); the blue point (n = 3) represents the natural number of clusters determined by the silhouette width. Based on the usage patterns, we call these clusters: low-, medium-, and high-usage clusters. (b)(c)(d) Illustrate the weekly ratings for participants of the low-, medium-, and high-usage clusters, respectively; for each plot, the X-axis is the week and the Y-axis is the weekly rating for each of the cluster’s participants, with each line representing a participant.
To determine whether the ratings (usage patterns) given by participants grouped into different clusters is statistically significantly different, we performed a one-way ANOVA test on the AWR for the clusters. The extremely low p- value for the AWR of different clusters (Table 3: AWR) indicates that the ratings are statistically significant different. There is also a statistically significant difference in the AWR for different clusters when all of the demographic factors (gender, race, education, employment status, and marital status) are considered as variables in the model (Table 3: DWR). To identify differences between specific groups, we use the post-hoc Tukey-Kramer method (Table 3: AWR right side), which shows that there is a statistically significant difference in the AWR between several pairs of groups.
Table 3.
One-way ANOVA results for participants clustered according to response type.
| Post-hoc Tukey-Kramer Test Results‡ | |||||
|---|---|---|---|---|---|
| Type | F-test† | p-value | Low-Medium | Medium-High | High-Low |
| AWR | 101.730 (2) | 1.15 × 10−8* | 5.15(4.7 × 10−6)* | 5.17 (4.5 × 10−6)* | 10.32 (0.00)* |
| DWR | 79.179 (2) | 5.35 × 10−6* | — | — | — |
| MAQ | 0.084 (1) | 0.777 | — | — | — |
| PCS | 6.647 (1) | 0.0257* | — | — | — |
| MCS | 11.381 (1) | 0.00621* | — | — | — |
| PCSWR | 0.329 (1) | 0.5778 | — | — | — |
| MCSWR | 1.872(1) | 0.1985 | — | — | — |
Note: AWR: Medication Average Weekly Rating; DWR: Medication Average Weekly Rating by Demographics; MAQ: Medication Adherence Questionnaire. Low, Medium, and High refer to the groups shown in Figure 2. *Significant at a 95% confidence level. †Formatted as: score (degrees of freedom). ‡Formatted as: mean difference (p-value).
RLHA Interaction. Table 4 shows the percentage of medication alerts to which each participant responded, and the number of days over which these responses occurred. A low response percentage was observed for two participants, namely 1 and 13. Participant 1 had only one medication listed as a daily medication, but was advised by his or her physician to take it as needed. Participant 13 had a considerable number of changes to his or her medication list, making it difficult to finalize the list. Table 4 shows the count of medications that were reported “Taken” and “Not Taken” for each participant over the study span. The most common reason cited for missed medications was “did not want to take” (28%), followed by “took but didn’t enter” (17%) and “discontinued” (15%). The RLHA followed up with the participants in case of any missed medications, and medication change. Only 37.5% of the participants would prefer to enter their own medications (Table 2: Q7). All of the participants appreciated this follow-up and felt that their best interest is being looked after.
Table 4.
A summary of the frequency, duration, and content of participant responses to medication alerts.
| Participant ID | Number of days | Response Percent* | Taken | Not Taken |
|---|---|---|---|---|
| 1 | 8 | 8.99 | 6 | 1 |
| 2 | 74 | 83.15 | 819 | 6 |
| 3 | 17 | 19.10 | 45 | 3 |
| 4 | 73 | 82.02 | 186 | 23 |
| 5 | 74 | 83.15 | 672 | 19 |
| 6 | 79 | 88.76 | 581 | 0 |
| 7 | 58 | 65.17 | 121 | 34 |
| 8 | 18 | 20.22 | 94 | 5 |
| 9 | 78 | 87.64 | 532 | 8 |
| 10 | 76 | 85.39 | 168 | 0 |
| 11 | 83 | 93.26 | 436 | 0 |
| 12 | 81 | 91.01 | 513 | 0 |
| 13 | 4 | 4.49 | 9 | 0 |
| 14 | 11 | 12.36 | 66 | 14 |
| 17 | 52 | 58.43 | 138 | 94 |
| 19 | 62 | 69.66 | 61 | 2 |
Calculated based on the number of days in the second phase (89 days).
PRN Intake. We found that eight participants had at least one PRN medication listed during the study phase. For those with at least one PRN medication, the number of PRN medications ranged from 1 to 5, with a median of 5. We also found that five participants tracked their PRN medications at least once over the study period; two of these participants tracked their PRN medications exactly 1 time, two tracked 5 times, and one tracked 69 times. Of the participants who did not track even once during the study phase, one had only a single medication listed and did not receive any confirmation from the physician regarding medication intake.
RQ2: How does eSeniorCare impact participants’ health-related quality of life?
SF12v2 was completed by nine participants. The majority of these participants belonged to the medium-usage group, as defined above. We used the missing data estimation supplied by the SF12v2 scoring software36 to estimate scores for the remaining participants. A majority of the participants (56.25%) had a post-study physical health score (PCS) score greater than or equal to that at the beginning of the study. We also observed a decrease in mental health score (MCS) for the same proportion of participants at the end of the study. We note, however, that about 50% of the participants reported PCS higher than the U.S. norm for their age category, both at the beginning and end of the study. To examine the relationship between post-study scores and medication component usage (WR), we developed a linear regression model with the post-study SF12v2 component score as the dependent variable and the pre-study SF12v2 scores and cluster number (high, medium and low rating groups) as independent variables, while controlling for demographic variables (age, education and race), other components of the application, and tablet use. We observed a strong relationship between the post-study and pre-study scores (Table 3: PCS and MCS). However, we did not observe a notable relationship between post-study scores and WR (Table 3: PCSWR and MCSWR). This may be due to the short duration of the study, the weather conditions (winter), and the small sample size. Further, we did not take into account the impact of chronic conditions on the scores.
RQ3: What influence does eSeniorCare have on participants’ knowledge of their medication regimes?
To explore the influence of eSeniorCare on a participant’s knowledge of their medications, we examined each participant’s responses to the questions in the MAQ. For each correct response to a question, we gave the participant 1 point. We then calculated each participant’s MAQ score as the total number of points he or she earned divided by the maximum possible points for that participant.
There was an increase in MAQ scores for 50% of the participants, while 19% showed a decrease. The remaining 31% of the participants showed no change in their scores because they obtained maximum or nearly maximum scores for both pre- and post-study questionnaires. To determine whether the difference between the pre- and post-study MAQ scores is statistical significantly different, we performed a paired t-test (t-statistic: -1.03; p-value: 0.317). We did not find any statistically significant difference. We further examined the relationship between MAQ scores and the clusters assigned based on weekly ratings via a one-way ANOVA test (Table 3: MAQ). We did not observe any statistically significant relationship between the change in MAQ scores and weekly ratings.
Discussion
The main objective of our study was to evaluate the design and impact of the medication adherence component of eSeniorCare on the participant’s health-related quality of life and explore the impact on their knowledge of medications. As a part of three-month-long study, the participants (seniors aged 55 years or older) used a tablet-based application to record their medication intake. The RLHA used a web-portal to track missed medications, changes in medications, and refill alerts reported by the participants through the application. All of the participants completed the study.
From our clustering illustrated in Figure 2, we found that the majority of participants (n = 11) used the medication component to track their medications, with most of the participants (n = 13) reporting higher (or maximum) MAQ scores at the end of the study than at the beginning. The majority of participants (n = 10) also reported higher physical health SF12v2 scores. However we found that, after controlling for demographic factors, the medication component usage (technology) did not have an impact on these scores. This accords with prior studies that have investigated the impact of computer use on quality of life.37,38 That said, we did observe a significant change in the post-study scores compared to the pre-study scores, even after controlling for age, gender, education and race.
From our ANOVA tests shown in Table 3, we found that the majority of the participants had an increase in MAQ scores at the end of the study, though the improvement in the MAQ scores for the participants at the end of the study was not statistically significant. We note, however, that the majority of the participants already had almost perfect scores at the beginning of the study, resulting in a very small margin of potential improvement for most of the participants.
For tracking medication adherence, we relied on each participant’s self-reported responses. As there is no gold standard in tracking adherence, a combination of methods is instead recommended.14 We thus implemented a secondary method of tracking medication adherence via a “Refill Medications” function. During the study phase, however, most of the participants did not use this functionality. This may be because most of the participants had already obtained 90-day refills for their medications, thus obviating the need to use the refill functionality throughout the duration of the study.
Recommendations for future work. We believe that our study provides a foundation for further development of integrated technological solutions for seniors. We also believe that the benefits of these solutions can and should go beyond the seniors themselves, as they can also help care providers and clinicians by providing them with a direct connection for monitoring medication adherence and connecting with their patient pool on health and wellness. Based on our findings, we provide the following recommendations for the development of mobile applications for medication management, and particularly for those oriented to low-income aging populations:
The application should function appropriately with intermittent Internet connectivity. We found that limited access to Wi-Fi was a major obstacle for the deployment of our application. To use the available connectivity efficiently, we specifically recommend periodically synchronizing locally stored data with a remote server. The care provider should be able to track the last synchronization date for each participant for tracking medication adherence to overcome the challenges with limited to no internet connectivity in a low-income, independent living facility.
The application should be accompanied by a companion web portal, accessible to a care provider. The portal should provide information on missed medications, refill alerts, and medication changes so that the care provider can take appropriate action. We found that participants were grateful for follow-ups by their care provider team.
The companion web portal should have functionality for the creation and maintenance of medication profiles for the users. We found that the complex medical regimen maintained by many seniors frequently makes medication entry directly via the application difficult. Further, to expedite this process, the application could be integrated with health information exchanges (HIEs) with necessary safety and privacy measures.
The participants should be able send to and receive messages from RLHA using the application as we found this communication to be a key factor for using eSeniorCare.
Limitations. While our current study was informative in impact as well as needs assessment, we do believe that having a larger sample pool over a longer time period can help strengthen the findings and conclusions drawn from the study. However, this is an important first step in developing an application that is integrative of the senior participants and their care provider team, demonstrating its strengths and weaknesses, and laying the foundation for partnering with independent living facilities for longer-duration studies. A further limitation is that we only address unintentional medication non-adherence, as our medication tracking relied on self-reporting; this is an area of ongoing research. It should be further noted that other features of the application aside from those actively investigated may have also contributed to the positive findings of our study.
Conclusion
We presented eSeniorCare, a health and wellness system focused specifically on improving senior care and quality of life. By analyzing participant information collected both through this system and through surveys, we found that eSeniorCare provides an intersection of technology and relationship building that can help seniors to effectively track their medications. We observed that the participants became more aware of their medications and were more likely to use them as prescribed. We also discovered that the role of RLHAs—providing personal support and medication tracking—is crucial to this improvement. Based on our findings, we also provide a series of suggestions for future developers to improve the design of their own medical management applications. Through an easy-to-use application and web portal, eSeniorCare empowers seniors to take charge of their medication management and places them in the center of a system of support, representing an important step toward improving senior care and quality of life.
References
- 1.aPlaceforMom. Importance of Taking Medications Correctly; 2015. Accessed 9th March 2016. Available at: http://www.aplaceformom.com/senior-care-resources/articles/importance-of-taking-medications.
- 2.Latif S, McNicoll L. Medication and non-adherence in the older adult. Geriatrics for the Practising Physician. 2009;92(12):418–419. http://rimed.org/medhealthri/2009-12/2009-12-418.pdf. [PubMed] [Google Scholar]
- 3.Ward BW. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010.; Preventing Chronic Disease.; 2013. 10 pp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balkrishnan R. Predictors of medication adherence in the elderly. Clinical Therapeutics. 1998;20(4):764–771. doi: 10.1016/s0149-2918(98)80139-2. [DOI] [PubMed] [Google Scholar]
- 5.Brown MT, Bussell JK. In: Mayo Clinic Proceedings. Vol. 86. Elsevier: 2011. Medication adherence: WHO cares? pp. 304–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jackevicius C, Mamdani M, Tu J. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. Journal of the American Medical Association (JAMA). 2002;288(4):462–467. doi: 10.1001/jama.288.4.462. [DOI] [PubMed] [Google Scholar]
- 7.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clinical Therapeutics. 2001;23(8):1296–1310. doi: 10.1016/s0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- 8.Salzman C. Medication compliance in the elderly. Journal of Clinical Psychiatry. 1995;56(Suppl 1):18–23. [PubMed] [Google Scholar]
- 9.Atreja A, Bellam N, Levy SR. Strategies to enhance patient adherence: making it simple. Medscape General Medicine. 2005;7(1):4. [PMC free article] [PubMed] [Google Scholar]
- 10.DiMatteo MR. Variations in patients adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care. 2004;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 11.Reach G. Can technology improve adherence to long-term therapies? Journal of Diabetes Science and Technology. 2009;3(3):492–499. doi: 10.1177/193229680900300313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horowitz BT. Mobile Phone App Helps Patients Take Medication More Consistently: Study; 2011. Accessed September 18, 2015. Available at: http://www.eweek.com/c/a/Health-Care-IT/Mobile-Phone-App-Helps-Patients-Take-Medication-More-Consistently-Study-295220.
- 13.Grindrod KA, Li M, Gates A. Evaluating user perceptions of mobile medication management applications with older adults: a usability study. JMIR mHealth and uHealth. 2014;2(1) doi: 10.2196/mhealth.3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stegemann S, Baeyens J, Cerreta F, et al. Adherence measurement systems and technology for medications in older patient populations. European Geriatric Medicine. 2012;3(4):254–260. [Google Scholar]
- 15.Osterberg L, Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 16.Lee ML, Dey AK. Reflecting on pills and phone use: supporting awareness of functional abilities for older adults.. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems.; ACM;; 2011. pp. p. 2095–2104. [Google Scholar]
- 17.Hayakawa M, Uchimura Y, Omae K, et al. A smartphone-based medication self-management system with realtime medication monitoring. Applied Clinical Informatics. 2013;4(1):37–52. doi: 10.4338/ACI-2012-10-RA-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinclair J. Pillboxie; 2011. Available from: http://pillboxie.tumblr.com/.
- 19.myCommunity Pillbox; 2009. Available from: http://pillboxapp.com/
- 20.Quinn C, Clough S, Minor J, et al. WellDocTM mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes technology & therapeutics. 2008;10(3):160–168. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 21.Patel S, Jacobu-Kantor L, Marshall L, et al. Mobilizing your medications: an automated medication reminder application for mobile phones and hypertension medication adherence in a high-risk urban population. Journal of diabetes science and technology. 2013;7(3):630–639. doi: 10.1177/193229681300700307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mira J, Navarro I, Botella F, et al. A Spanish pillbox app for elderly patients taking multiple medications: randomized controlled trial. Journal of medical Internet research. 2014;16(4):e99. doi: 10.2196/jmir.3269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferreira F, Almeida N, Rosa A, et al. Elderly centered design for interaction–the case of the S4S medication assistant. Procedia Computer Science. 2014;27:398–408. [Google Scholar]
- 24.Dalgaard LG, Gronvall E, Verdezoto N. MediFrame: A Tablet Application to Plan, Inform, Remind and Sustain Older Adults’ Medication Intake.. In: Proceedings of the IEEE International Conference on Healthcare Informatics (ICHI).; IEEE; 2013. pp. 36–45. [Google Scholar]
- 25.Silva J, Mouttham A, El Saddik A. UbiMeds: a mobile application to improve accessibility and support medication adherence.; In: Proceedings of the 1st ACM SIGMM International Workshop on Media Studies and Implementations that Help Improving Access to Disabled Users.; ACM; 2009. pp. 71–78. [Google Scholar]
- 26.Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: potential benefits to patients and providers. Journal of the American Pharmacists Association (JAPhA). 2013;53(2):172. doi: 10.1331/JAPhA.2013.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown S. Overcoming the pitfalls of medication reconciliation. Nursing Management. 2012;43(1):15–17. doi: 10.1097/01.NUMA.0000409932.77213.9b. [DOI] [PubMed] [Google Scholar]
- 28.Stawarz K, Cox AL, Blandford A. Don’t forget your pill!: designing effective medication reminder apps that support users’ daily routines.; In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems.; ACM; 2014. pp. 2269–2278. [Google Scholar]
- 29.Dalgaard LG, Grönvall E, Verdezoto N. Accounting for medication particularities: Designing for everyday medication management.; In: Proceedings of the 7th International Conference on Pervasive Computing Technologies for Healthcare. Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering (ICST);; 2013. pp. 137–144. [Google Scholar]
- 30.Tariq SH, Tumosa N, Chibnall JT, Perry MH, Morley JE. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder?a pilot study. American Journal of Geriatric Psychiatry. 2006;14(11):900–910. doi: 10.1097/01.JGP.0000221510.33817.86. [DOI] [PubMed] [Google Scholar]
- 31.Svarstad BL, Chewning BA, Sleath BL, Claesson C. The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Education and Counseling. 1999;37(2):113–124. doi: 10.1016/s0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 32.Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Quality of Life Research. 2009;18(6):727–735. doi: 10.1007/s11136-009-9483-1. [DOI] [PubMed] [Google Scholar]
- 33.Findlater L, Froehlich JE, Fattal K, Wobbrock JO, Dastyar T. Age-related differences in performance with touchscreens compared to traditional mouse input.; In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems.; ACM; 2013. pp. 343–346. [Google Scholar]
- 34.Park HS, Jun CH. A simple and fast algorithm for K-medoids clustering. Expert Systems with Applications. 2009;36(2):3336–3341. [Google Scholar]
- 35.Rousseeuw P. Silhouettes: a graphical aid to the interpretation and validation of cluster analysis. Journal of computational and applied mathematics. 1987;20:53–65. [Google Scholar]
- 36.Maruish M. User’s manual for the SF-12v2 Health Survey; 2012.
- 37.Choi M, Kong S, Jung D. Computer and internet interventions for loneliness and depression in older adults: a meta-analysis. Healthcare Informatics Research. 2012;18(3):191–198. doi: 10.4258/hir.2012.18.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elliot AJ, Mooney CJ, Douthit KZ, Lynch MF. Predictors of older adults’ technology use and its relationship to depressive symptoms and well-being. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69(5):667–677. doi: 10.1093/geronb/gbt109. [DOI] [PMC free article] [PubMed] [Google Scholar]