Abstract
The purpose of writing medical notes in a computer system goes beyond documentation for medical-legal purposes or billing. The structure of documentation is a checklist that serves as a cognitive aid and a potential index to retrieve information for learning from the record. For the past 50 years, one of the primary organizing structures for physicians’ clinical documentation have been the SOAP note (Subjective, Objective, Assessment, Plan). The cognitive check list is well-suited to differential diagnosis but may not support detection of changes in systems and/or learning from cases. We describe an alternative cognitive checklist called the OODA Loop (Observe, Orient, Decide, Act. Through incorporation of projections of anticipated course events with and without treatment and by making “Decisions” an explicit category of documentation in the medical record in the context of a variable temporal cycle for observations, OODA may enhance opportunities to learn from clinical care.
Introduction
Physicians and other healthcare providers write notes for a variety of purposes, including documentation of care, communication with other team members, and providing evidence of services for billing. There are a growing number of applications that help physicians write notes both for efficiency and to produce coded data as a byproduct. Whether application generated, dictated, typed or (increasingly rarely) hand written. There is a substantial question as to whom physicians are composing notes for (billers, themselves, or other providers) and many notes by medical professionals go largely unread by others. (1) There is also a growing concern about the use of cut and paste actions and templates short circuiting clinical cognition (2) and about resident practices that separate note composition from clinical workflows pre-empting thinking during note writing. (3)
We believe that when physicians compose notes, they should be thinking about the patient and the task of composition should shape both the processes of care and the ultimate conclusions they reach about diagnoses.(4) Moreover, note writing should provide an opportunity to learn from a case both as it evolves and on retrospective review. This paper reviews predominant cognitive models that shape providers’ thinking during the process of documentation, and proposes an alternative model designed to promote situational awareness and learning from experience.
Background
Larry Weed is the father of structured recording of medical information to facilitate reasoning. His theories were first expounded almost 50 years ago in the seminal paper, “Medical Records that Guide and Teach.” (4) At the core of Weed’s theories is the use of checklists for clinical cognition that encourage medical providers to think systematically about their patients. A widely adopted structural innovation described by Weed—the Subjective, Objective, Assessment and Plan (SOAP) framework—reminds clinicians of specific tasks while providing a framework for evaluation of information and provides a cognitive framework for reasoning activities.
The “Subjective” header is a cue for documentation of data that comes from patients’ experiences. By labeling this data “subjective”, it encourages clinicians to reason using an objectivist view and to divide the world into the “subjective” experiences of patients (history of illness, symptoms experienced, pain and anxiety and other features as elicited by the clinician or other healthcare providers), and the more “objective” measures of the clinician (physical examination findings, diagnostic testing and radiological examinations) that govern the processing of subjective reports of illness into medical diagnoses. Donnelly critiques this division of the world into subjective and objective based on the perspective of the physician: “The fact that we cannot know the facts becomes obscured if one accepts the subjective-objective distinction in SOAP.” (8)
The Assessment section documents the synthesis of “subjective” and “objective” evidence to arrive at a diagnosis. The Assessment section details the differential diagnosis process and may include some risk benefit tradeoffs in decision making. The Plan section details the needs for additional testing and consultation with other clinicians to address the patients’ illnesses, in addition to the steps being taken to treat the patient.
Examining this framework, what is the operational task that it supports? This author would assert that task is capture and consideration of all relevant data with a view toward differential diagnosis. SOAP is probably not the actual framework that clinicians use in diagnostic reasoning (9), but it has probably served well as a guide to to diagnostic reasoning for a variety of reasons. The framework is hypothetico-deductive one that is focused on the application of the scientific method to patient care and the disproof of competing hypotheses. This gives the approach a certain face value (that may be diminishing in light of “big data” methods of empiric assessment and treatment). In addition to being “scientific”, the approach is fundamentally Bayesian: the prior probability of different diseases is updated by elements personal history (the subjective). Physical exam findings and laboratory tests, further update the posterior probability, ruling in or out different diagnoses. The Assessment follows all this data, and thus is allows the clinician to review relevant data before reaching a conclusion. Thus, if differential diagnosis was the only task that providers performed, SOAP might be the ideal cognitive framework.
But what if the situation is more dynamic? Could hypothetico-deductive reasoning lead providers astray by anchoring them on past observations and conclusions? It is likely that more common task in medical environments than differential diagnosis of an unknown problem(s) is the active management of an evolving, known medical problem over time and the differentiation of change in a disease from acquisition of a new one. In many clinical situations, evidence changes over time, requiring providers to reconsider diagnoses and treatments or risk error. (10) The SOAP model does not explicitly integrates time into its cognitive framework and thus has an important gap.
This has not gone unnoticed. Nurse clinicians have proposed extensions to SOAP designed to address its temporal “blind spot.” For example, the SOAPE, SOAPIE, and SOAPIER models add “Intervention”, “Evaluation” and “Revision” headers) and, a result, creates categories for linking a note to overall progress on treatment of the problem. (11) The “E” and “R” are important refinements to SOAP. “E” adds an explicit reminder to asses how well has a plan worked. “R” creates explicit expectations that plans need to change over time.
Physician have also proposed changes to their SOAP notes to make it easier follow a problem over time. Proposed changes have focused frames designed to help providers look backward across prior notes may detect changes in a patient’s condition or failure of a medical plan to achieve its intended effects. To support these concepts, Meyers and Miller suggest adding an “orientation” step to SOAP (O-SOAP) based on retrospective review of records. (12, 13) Gensinger and Fowler suggest re-arrangement of SOAP as ASOP (14), focusing on Assessment at the beginning to provide more temporal orientation. An ASOP structured note would bear some similarity to a cognitive frame widely used handoffs between providers called SBAR (Situation, Background, Assessment, Recommendations) (15), with Assessments in ASOP playing a similar role to Situations in SBAR. While putting Assessment first has some advantages, it might also lead to faulty decision making, if performed in order of the acronym, by forcing conclusions prior to review of all the data, voiding the positive cognitive check list effects of SOAP.
Unfortunately, none of the proposed enhancements of the SOAP cognitive framework have gained wide acceptance as a way to document progress notes. One potential reason for the “stickiness” of the SOAP model is that it is cognitively “right-sized.” As Miller described in his seminal 1956 paper (16), there are limits on working memory capacity of the brain. Cowan revisits Miller’s work arguing that the magic number of items is four (17). It is an interesting coincidence that SOAP has four steps—as does SBAR, which is also widely adopted (18-22), and that extensions to SOAP that add additional tasks have not received as wide acceptance. Alternatively, SOAP extensions may not offer sufficient advances as to warrant their adoption based on Rogers Theory of Diffusion. (23)
Where could we look to improve upon SOAP, borrowing from other fields, while also recognizing the importance of prior authors insights into the limitations of SOAP? Electronic health records systems (EHRs) offer the potential of re interpreting the SOAP approach to focus on the evolution of problems over time. As described by Meyers’ et al. (12), the problem with the SOAP is that “it does not recognize the crucial effect that the last assessment and plan and the returned plan results have upon the next visit.” Prototypes developed by Meyers et al. (13) and Bosen (24), illustrate how EHRs could bring elements of SOAP notes related to specific problems over time together in context to improve reasoning. However, there might also be value in changing the frame all together.
An Alternative Framework for Reasoning
The discipline of human factors research provides alternative directions on how to reorganize note writing. The failure of a clinician to recognize change in manifestations of a hypothesized disease over time, or to recognize unexplained systems, might be characterized as a lack of situational awareness.(10) Endsley defines situational awareness as “the perception of the elements in the environment within a volume of time and space, the comprehension of their meaning, and the projection of their status in the near future.” (25) For example, situational awareness might require that physicians retain unexplained observations in their working memory and to document these in their notes (for example, the fever that doesn’t resolve or the serum sodium that is too low), in addition to documenting their diagnoses and their rationale. Or, situational awareness might require one discipline to be aware of the findings of another. For example, a physician might need to read a nurses note to be aware of a patient’s changes in cognition. Situational awareness might also include subtle observations of interactions between the patient and family members that give clues about how care for the patient occurs at how.
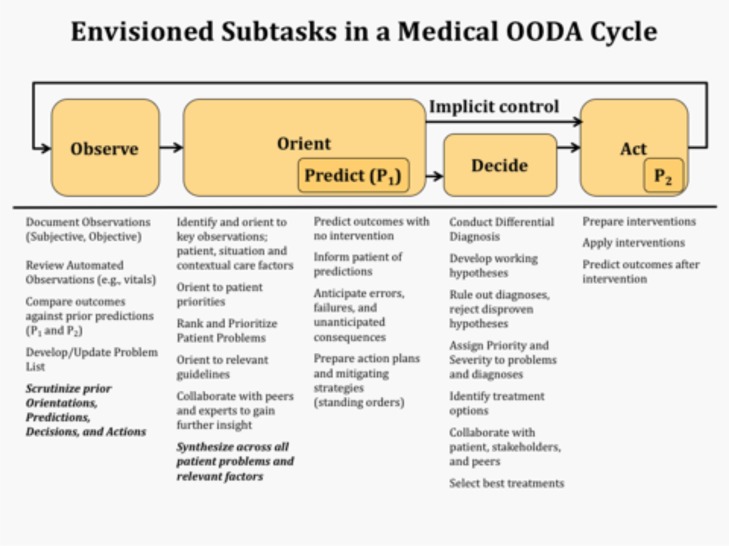
Similar to SOAP, there are cognitive models that outline steps that can help novices and experienced users maintain situational awareness and learn in rapidly changing environments. One such model, which was initially developed by Boyd to help Air Force pilots outthink their opponents in aerial combat but is now widely applied within the U.S. military, is the Observe Orient Decide Act (OODA) model.
OODA is an action-oriented decision making model is explicitly applied in a repeating loop. Completion of one cycle prompts the next. There are no fixed time intervals for OODA cycles—the rate of cycling depends on how fast circumstances are changing. The goal of the OODA Loop is “think” and “act” faster and better than the enemy (in this case the disease(s) afflicting the patient), and thereby utilize available resources to maximum effect. (26) This is an important concept that is rarely addressed in medical reasoning: unless the pace of medical assessments and interventions outpaces the disease, the patient will, at best, experience morbidity or at worst, mortality (27). Bad outcomes occur when medical treatments are not adjusted fast enough, based on current hypotheses about what the illness is, to outpace progression of the illness.
In addition, OODA loops emphasize recognition of mismatch between predictions and experiences and, also, automation of responses in specific settings, once a problem has been recognized. OODA and other models that formally integrate a predictive step enhance learning through observation. They force a projection on the learner and periodic (re) assessments to test that projection with reality.
The OODA Loop is a proven technique to speed cognitive adaptation to changing circumstances. It has been widely adopted within U.S. military doctrine and the success of operations such as the first Gulf War, attributed, at least in part, to its appropriate implementation. (26, 28) OODA loops have been successfully utilized in the field of medicine (29, 30) but not as a template for documentation or teaching reasoning. The specific elements of the OODA framework will be discussed in turn in following paragraphs.
The Observation step encompasses both subjective and objective elements found in the SOAP note avoiding the subjective-fallacy. The decision maker notes what facts are available at a particular time. Observations might be general or specific to a designated problem. They might come from more than one observer; for example, a nurse or a caretaker. Observations may reflect patient history or be abstracted from other elements of a clinical record such as laboratory and radiological tests. Observations are time stamped, reflecting the state of the world at the time of its examination by the reasoner. This is critical, because in retrospective review of decision making, for the purposes of learning, a learner would need to distinguish an error due to a lack of availability of key information (a failure of observation) from a failure to integrate that information into a decision process.
The next step in the OODA model is Orientation, which puts Observations in context and presents integrative hypotheses for causation or explanation (e.g., diagnoses and social contexts). To quote Boyd, “orientation is an interactive process of many-sided implicit cross-referencing projections, empathies, correlations, and rejections that is shaped by and shapes the interplay of genetic heritage (!), cultural tradition, previous experiences, and unfolding circumstances.” A frequent cause of decision-making error in complex, evolving environments is cognitive tunneling, which is a form of “expectancy-driven” thinking bias. (31) An explicit goal of the orientation step is the prevention of this mental tunnel vision and the mitigation of confirmation bias—that is, an excessive, self-convincing focus on a few details thought to be pertinent. Orientation includes noting which observations are missing and which are unexplained.
Boyd stressed iterative re-orientation as an essential means to correct oneself from perceptual “mismatches” with reality, as it “unfold[s] in an irregular, disorderly, unpredictable manner.” (32) This effortful act of sense making (33) would call upon the physician to apply the wholeness of his or her being, including his or her previous experience and innate talents, medico-ethical heritage, a holistic contextual view of his patient, and even his or her feelings in addition relevant guidelines and resources available in the environment in order to integrate across observations and problems to create a synthesis on the current patient state. Orientation might include updating probabilities of different potential diseases in the differential diagnosis. It could also include an assessment of the effects of treatment, but should always include the non-medical context of care. Problem list generation and, perhaps more importantly, problem list maintenance, are part of the Orientation step.
Endsley (a contemporary of Boyd, whose work includes best practices for safety in aircraft cockpit environments and has been adopted by medical safety researchers) expanded the initial concepts underlying the OODA Loop by proposing that situational awareness should include projection (prediction) of the effects of both action and inaction. (25, 34) In current documentation practices, providers rarely predict what will happen if they do nothing or expected the effects of a prescribed treatment. This is critical for subsequent comparison to observed effects to ascertain if the cognitive model of the provider is correct. For example, predicting the effect of prescription of a blood pressure medicine (e.g., drop in systolic blood pressure of 10 mm/hg by the next visit, a decrease in potassium of 0.2 ug/mL after infusion, or an increase in uric acid concentration of 0.5 ug/mL). Documentation of the expected effect of actions (and non-actions) is important in assessing the correctness of decisions and the adequacy of actions. Understanding of the gap between predictions and observations is critical to learning from experience. To echo Boyd, who also made projection a major theme of his work, if your predictions were incorrect, your earlier observations (perceptions) or orientation (integration of information) were mismatched with reality. One must –(re) observe and (re) orient, quickly until predictions match reality. Or, in other words, one must learn.
The third step in the OODA model is to make and record decisions. Decisions include both interpretations of observations through the lens of orientating (e.g., diagnoses) and risk-benefit trade-offs that underlie Actions. Decisions, like Observations and Orienting hypotheses, should be time stamped. (3) Analyzing the effect of decisions provides the opportunity to assess and refine decision-making skills—to allow trainees to learn from their experiences and to see, potentially, what others decided to do in similar circumstances. Quality control efforts could benefit from individual and team performance reviews of decisions made during episodes of care. Tracing longitudinal decision pathways permits individual and team reflection and learning. It may also facilitate the identification of novel approaches, which could be leveraged across a healthcare organization in pertinent care settings, or inform guideline improvement efforts. For example, natural language process approaches might be applied to identify all the decision points in a case and bring those together for review. In SOAP formatted notes, medical decisions are often implicit in documentation, embedded in Assessments and Plans; there is no easy way to call these out of a health record and re examine a provider’s reasoning vis-à-vis the state of evidence at any particular time and his or her rationale for decision making.
Advanced versions of OODA include implicit guidance and control operations as an alternative to explicit decision-making. In note writing and clinical care, this might take the form of instructions for “what if” cases that are expected. For example, a standing order for use of acetaminophen with a fever over 39 C, followed by obtaining a blood culture. These bits of “compiled” knowledge of how to respond to a patient’s illness shorten the time to implementation of orientating insights and potential enable quicker control of progression of disease.
The final element in an OODA cycle is to specify Actions. The OODA framework specifies Actions rather than the SOAP note’s Plans: this is because it is one thing to plan and another to act. While the difference is semantics to some degree (Webster’s defines a “plan” as “a detailed formulation of a program of action”), specifying actions removes ambiguity. For example, a list of actions might clarify which team members have responsibility for execution of the different actions that comprise “the plan” (including the patient). Action specifications should include predictions of their effects, potentially aided by predictive analytics models. Observations in subsequent cycles should address the effectiveness of implementation of proposed actions.
The OODA Loop has the advantage of being applied in a cyclic fashion, clarifying thinking over time, with the most recent Observations challenging Predictions and Actions from the previous period. Iterative diagnostic reasoning helps prevent errors by encouraging the review of assumptions of prior decisions and aiding to assess the degree to which the operational model fits observed effects. (35) A failure to reconsider initial diagnosis in the face of mounting evidence supporting an alternative is a frequent cause of error. (36) The Decide step, in a temporal frame, allows revisiting of the choice, model, and actions, and a reconsideration of assumptions. In contrast to SOAP, OODA prompts the documenter to refine his or her thinking based on how prior actions correspond to current observations. (See Figure 1.) It prompts the note writer to contemplate, “What was I thinking yesterday and was it correct? How should I think differently today? What is important to focus on at this juncture? What is relevant? What warrants action? What will happen if I do nothing?” (37) While the OODA cycle includes prediction in two of the steps, we would argue that prediction is not an independent action. Rather one cannot/should not complete the tasks of Orientation or Action selection without the context provided by a prediction of the outcomes of inaction and action.
Figure 1.
Medical OODA Cycle.
As clinicians increasingly “cut and paste” content from prior patient encounters into notes, (38) the decision support opportunities provided by note writing are in jeopardy. It is time we (once again) recognize note writing as a cognitive task that helps clinicians think better and thereby avoid errors. But, in order to better reflect what we know about clinical cognition after 50 years, perhaps it is time to advance the mindset that guides notes. There is probably not a single cognitive frame that is valid for all types of notes. The cognitive frame of note writing should match the predominant task in management of the patient. The POMR/SOAP format is well adapted to the initial medical encounter. In an initial evaluation of a patient, the sequential evaluation of symptoms, signs and evidence to formulate a differential diagnosis may be the most important task. Further, a reductionist approach, focused on identifying specific problems and solutions, may be highly adaptive. But, in the subsequent management of patients, particularly in dynamic environments or the ongoing management of patient conditions, it may be more important for the cognitive frame of the note to aid the author in maintaining situational awareness, and in detecting change and errors in diagnosis. In this setting, integrating lessons from OODA-style thinking may be preferable. An OODA-style note would also improve communications by explicitly documenting a clinician’s reasoning and decisions, much of which is not transparent in SOAP notes.
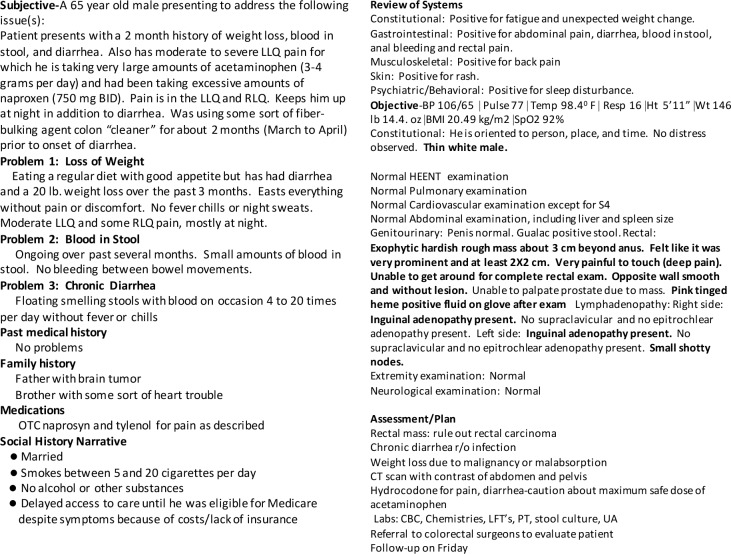
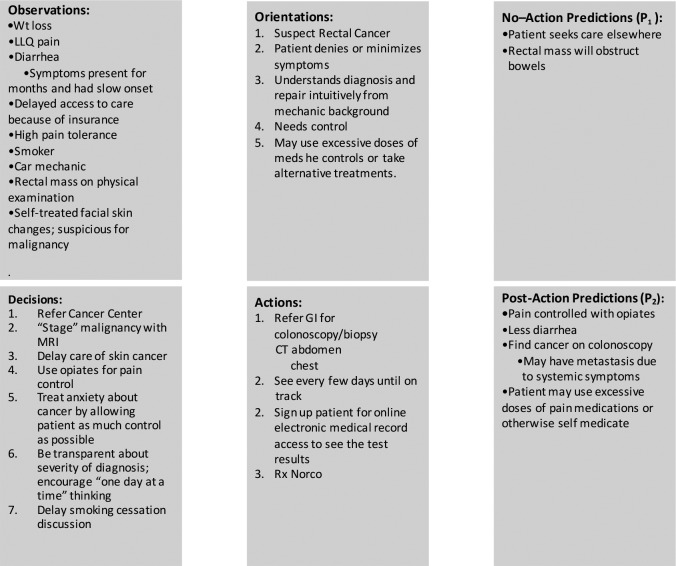
What would an OODA note look like in an electronic medical records system? To better understand this, working with a student in my laboratory, we adapted from the initial visit of a patient with colorectal cancer to the OODA format. In Figure 2a is the description of the patient visit in a more traditional SOAP and problem oriented format. Figure 2b is the description in the OODA format. The OODA note is not comprehensive in order to illustrate its differences.
Figure 2a.
Description of an initial visit of a patient with colorectal cancer in the traditional format.
Figure 2b.
Same note in OODA format.
While the first note focused on the process of coming to the diagnosis of colorectal cancer and the evidence for an against this diagnosis, the OODA equivalent focused more on developing an action plan that both executable and acceptable to that patient. The consequences of inaction are also made explicit. The OODA note is more conceptual and combines subjective and objective data elements in one category and orientating information that places the patient in a human context. The explicit predictions with and without treatment help assess both the correctness of the diagnosis and the impact of care. In a SOAP note, it is relatively easy for the note to focus the note on the disease (colorectal cancer) rather than the patient. The note, a documentation of the findings of the physician, goes into great detail on the history suggestive of cancer, the findings that confirmed it, and emphasized the amount of time it took for the physician to perform the careful history and examination required to make the diagnosis. It is an excellent logbook entry (15) of the care of this patient. But, beyond careful documentation, what did does the log do? In this case, the diagnosis was virtually certain (and would be absolutely certain with obvious diagnostic tests.) What was uncertain that needed to be managed? It was the patient’s response to learning the diagnosis and the plan for controlling his symptoms. OODA may help focus documentation and as a result clinical thinking on the uncertain—on the parts of care that are not obvious—that need attention and future care. The differences are illustrative and should not be considered the target for OODA implementation rather than the definitive instance.
Other Medical Applications of OODA documentation
In addition to using OODA as a documentation template, there are many other potential applications that could take data from an OODA framework and make it more available to clinicians. If data in OODA format were coded and if appropriate meta data were available, then it might be possible to re-present notes created in the OODA format in the more traditional SOAP format. In fact, there is probably not a strong reason to align note creation frameworks supporting cognition with the framework used for display for a viewer. Informatics tools could allow readers to view notes in the templates most aligned to their own thinking using metadata to order and organize the display.
OODA may be an important tool in medical education. Notes labeled in an OODA format allows a different type of chart review of a case more akin to “replay” of the clinical state of thinking. At each point where a decision was recorded, the learner could review the observed data, the orientations of the decision maker, the projects and the decisions. In current EHRs, review of a case occurs primarily through the retrospective lens of the discharge summary. While many authors write discharge summaries as historical records or “captain’s logs”, this is probably not the highest use of these documents, which should be focused on care coordination post discharge. (15) The ability to record decision points and to review decisions over time might be one of the most important advances afforded by OODA approaches.
OODA may also have a roll in coordinating care across disciplines. One way it could do this is by providing an interdisciplinary “blackboard” for recording observations, orienting facts and hypotheses, decisions, and actions that are transdisciplinary. One reason that physicians, nurses and other providers might not view each others documentation as often as they should (1), might be the orientation of that documentation around SOAP models targeted at diagnosis specific to their own discipline. Medicine (and even subspecialties of medicine), nursing, dentistry and other disciplines all make diagnoses of that often may be of limited relevance to other disciplines. But what if as each discipline were writing their note, they could mark up observations, orientations, etc. as being important for the situational awareness of other providers. This might not take re-entry of data—rather in a coded data environment, one might mark up a fact for sharing. The OODA model might be very good for organizing data sharing as a neutral framework. A transdisciplinary blackboard might also allow providers to identify facts that are unexplained or request help from other disciplines in confirming predictions.
Conclusions
While the SOAP model has served practitioners well for over 50 years, the nature of the tasks that physicians perform has evolved over that time, its limitations are well known. The purpose of this article is to introduce OODA, a tested cognitive framework that has potential lessons for how doctors should write notes to improve the clarity of their thinking and to make their reasoning more transparent so that the writer and subsequent readers of notes can learn from care. OODA reflects the evolution of SOAP over time but also introduces new concepts related to temporality and explicit decision cycles for clinical care. This paper does not address the issues of how to link OODA notes together or the potential medical-legal issues of having every decision open for review in a medical record. These are complex issues; however, pragmatic issues, should not be allowed to thwart strategies to improve patient care. Small improvements in cognitive aids for note writing used many times a day by hundreds of thousands of physicians might have large impacts. Research is needed to identify the optimal framework for cognitive support during note writing. OODA is an example of a proven framework that may have important implications for medicine and which could potentially serve as a replacement for SOAP.
Acknowledgements
This paper is dedicated to a former student who wishes to remain anonymous but deserves credit for introducing me to the concepts of advocated by Boyd and his OODA Loop. While I must honor his wishes for privacy, I also wish to express my heartfelt thanks for teaching-his-teacher, and for his insights and enthusiasm.
Funding Statement
This work was supported by NLM Training Grant No. T15LM007124.
References
- 1.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. Journal of American Medicaal Informatics Association. 2011;18:112–7. doi: 10.1136/jamia.2010.008441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartzband P, Groopman J. Off the record--avoiding the pitfalls of going electronic. New England Journal of Medicine. 2008;358(16):1656–8. doi: 10.1056/NEJMp0802221. [DOI] [PubMed] [Google Scholar]
- 3.Hirschtick RE. A piece of my mind. John Lennon’s elbow. JAMA. 2012;308(5):463–4. doi: 10.1001/jama.2012.8331. [DOI] [PubMed] [Google Scholar]
- 4.Weed LL. Medical records that guide and teach. The New England Journal of Medicine. 1968;278(11):593–600. doi: 10.1056/NEJM196803142781105. [DOI] [PubMed] [Google Scholar]
- 8.Donnelly WJ, Brauner DJ. Why SOAP is Bad for the Medical Record. Archive Internal Medicine. 1992;152(3):481–4. [PubMed] [Google Scholar]
- 9.Bowen J. Eduational strategies to promote clinical diagnostic reasoning. The New England Journal of Medicine. 2006;355(21):2217–25. doi: 10.1056/NEJMra054782. [DOI] [PubMed] [Google Scholar]
- 10.Singh H, Giardina TD, Petersen LA, Smith MW, Paul LW, Dismukes K, et al. Exploring situational awareness in diagnostic errors in primary care. BMJ Quality and Safety. 2012;(21):30–8. doi: 10.1136/bmjqs-2011-000310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Using SOAP, SOAPIE, and SOAPIER formats. Nursing. 1999;29(9):75. doi: 10.1097/00152193-199909000-00028. [DOI] [PubMed] [Google Scholar]
- 12.Meyers KC, Miller HJ. Cleaning up SOAP. Academic Medicine. 1997;72(11):933–4. doi: 10.1097/00001888-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Meyers KC, Miller HJ, Naeymi-Rad F. Problem focused knowledge navigation: Implementing the problem focused medical record and the 0-HEAP note. Proceedings of the American Medical Informatics Association AMIA Annual Fall Symposium; 1998; pp. 325–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Gensinger RA, Fowler J. ASOP: A new method and tools for capturing a clinical encounter. Proceedings : a conference of the American Medical Informatics Association / AMIA Annual Fall Symposium AMIA Fall Symposium; 1995; pp. 142–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Lenert LA, Sakaguchi FH, Weir CR. Rethinking the discharge summary: a focus on handoff communication. Academic Medicine. 2014;89(3):393–8. doi: 10.1097/ACM.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller GA. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychological Review. 1956;63:81–97. [PubMed] [Google Scholar]
- 17.Cowen N. The magic number 4 in short term memory: a reconsideration of mental storage capacity. Behavioral and Brain Sciences. 2000;24:87–185. doi: 10.1017/s0140525x01003922. [DOI] [PubMed] [Google Scholar]
- 18.Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Joint Commission Journal on Quality and Patient Safety. 2006;32(3):167–75. doi: 10.1016/s1553-7250(06)32022-3. [DOI] [PubMed] [Google Scholar]
- 19.Pope BB, Rodzen L, Spross G. Raising the SBAR: how better communication improves patient outcomes. Nursing. 2008;38(3):41–3. doi: 10.1097/01.NURSE.0000312625.74434.e8. [DOI] [PubMed] [Google Scholar]
- 20.Thomas CM, Bertram E, Johnson D. The SBAR communication technique: teaching nursing students professional communication skills. Nurse educator. 2009;34(4):176–80. doi: 10.1097/NNE.0b013e3181aaba54. [DOI] [PubMed] [Google Scholar]
- 21.Velji K, Baker GR, Fancott C, Andreoli A, Boaro N, Tardif G, et al. Effectiveness of an Adapted SBAR Communication Tool for a Rehabilitation Setting. Healthcare Quarterly. 2008;11(3):72–9. doi: 10.12927/hcq.2008.19653. [DOI] [PubMed] [Google Scholar]
- 22.Wentworth L, Diggins J, Bartel D, Johnson M, Hale J, Gaines K. SBAR: Electronic Handoff Tool for Noncomplicated Procedural Patients. Journal of Nursing Care Quality. 2011 doi: 10.1097/NCQ.0b013e31823cc9a0. [DOI] [PubMed] [Google Scholar]
- 23.Rogers EM. 5. xxi. New York: Free Press; 2003. Diffusion of innovations; p. 551. [Google Scholar]
- 24.Bosen C. Evaluation of a computeried problem oriented medical record in a hospital department: Does it support daily practice? International Journal of Medical Informatics. 2007;76:592–600. doi: 10.1016/j.ijmedinf.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 25.Endsley MR. Toward a Theory of Situation Awareness in Dynamic Systems. Human Factors. The Journal of the Human Factors and Ergonomics Society. 1995;37(1):32–64. [Google Scholar]
- 26.Richards CW. Philadelphia, Pa: Xlibris; 2004. Certain to win: The strategy of John Boyd Applied to business; 187 pp. [Google Scholar]
- 27.Amalberti R, Brami J. ‘Tempos’ management in primary care: a key factor for classifying adverse events, and improving quality and safety. BMJ Quality and Safety. 2012 doi: 10.1136/bmjqs-2011-048710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coram R. 1. Boston: Little, Brown; 2002. Boyd : the fighter pilot who changed the art of war; p. 485. [Google Scholar]
- 29.Wickramasinghe N, Bali RK, Gibbons MC, Choi JH, Schaffer JL. A systematic approach: optimization of healthcare operations with knowledge management. Journal of healthcare information management. 2009;23(3):44–50. [PubMed] [Google Scholar]
- 30.Villars PS, Veazie MQ, Berger JS, Vu QM, Campbell-McAdory AA, Frenzel JC, et al. Adaptation of the OODA Loop to reduce postoperative nausea and vomiting in a high-risk outpatient oncology population. Journal of Perianesthesia Nursing. 2008;23(2):78–86. doi: 10.1016/j.jopan.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 31.Wickens CD, Gordon SE, Liu Y. An Introduction to Human Factors Engineering. 2. Upper Saddle River, N.J: Pearson Prentice Hall; 2004. 587 pp. [Google Scholar]
- 32.Boyd JR. A Discourse on Winning and Losing. Unpublished Briefing Slides. 1992 slide 29. [Google Scholar]
- 33.Angerman WS. Air Force Institute of Technology; 2004. Coming Full Circle with Boyd’s OODA Loop Ideas: An Analysis of Innovation Diffusion and Evolution. [Google Scholar]
- 34.Wright MC, Taekman JM, Endsley MR. Objective measures of situation awareness in a simulated medical environment. Quality and Safety in Health Care. 2004;13(1):i65–71. doi: 10.1136/qshc.2004.009951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norman G, Barraclough K, Dolovich L, Price D. Iterative diagnosis. BMJ. 2009;339(b3490):747–52. doi: 10.1136/bmj.b3490. [DOI] [PubMed] [Google Scholar]
- 36.Redelmeier DA. The Cognitive Psychology of Misses Diagnoses. Annals of Internal Medicine. 2005;142:115–20. doi: 10.7326/0003-4819-142-2-200501180-00010. [DOI] [PubMed] [Google Scholar]
- 37.Edelstein L. The Hippocratic oath, text, translation and interpretation. vii. Baltimore: The Johns Hopkins press; 1943. p. 64. [Google Scholar]
- 38.Wrenn JO, Stein DM, Bakken S, Stetson PD. Quantifying clinical narrative redundancy in an electronic health record. Journal of the American Medical Informatics Association. 2010;17:49–53. doi: 10.1197/jamia.M3390. [DOI] [PMC free article] [PubMed] [Google Scholar]