Abstract
Social determinants of health play an important role in diagnosis, prevention, health outcomes, and quality of life. The objective of this study was to examine existing standards, vocabularies, and terminologies for items related to Residence, Living Situation, and Living Conditions and to synthesize them into model representations. Sources were identified through literature and keyword searches, and an examination of commonly used resources. Each source was systematically analyzed by two reviewers, mapped to topic area(s), and further mapped to a model representation. A total of 27 sources were identified and reviewed. Seven of the sources had no items, i.e. concepts, elements, or values, related to the three topic areas while SNOMED-CT had the most items at 436 followed by the US Census at 174. While none of the identified sources encompassed a complete representation for documenting the three topic areas, their synthesis together results overall in more comprehensive representations.
Introduction
Social and individual behavioral factors play an important role in diagnosis, prevention, health outcomes, and quality of life.1, 2 As defined by the World Health Organization, “social determinants of health are the conditions in which people are born, grow, live, work, and age”.3 Social determinants of health (SDOH) can cause illness, exacerbate chronic illness, but can also prevent disease and improve health. When considered broadly, SDOH includes behavioral components, such as alcohol, drug, and tobacco use; diet; and physical and environmental factors that may influence an individual’s health such as living conditions, social support, occupation and its associated exposures, and physical activities. These factors contribute to mortality as well as account for being a dominant causal mechanism for many types of disease.4–8
With respect to SDOH related to Residence, Living Situation, and Living Conditions, insecurity related to housing, for example, has been associated with poor health among children,9 barriers related to access to health care,10 and the need for chronic disease management.11 Living situation, residence, and physical living conditions all have been shown to have significant impact on a patient’s health outcomes.12, 13 Since SDOH have a significant impact on patient health as risk factors, they should be considered when assessing and prescribing interventions and can serve to influence provider recommendations. For example, if a patient requires a weekly treatment at a distant location, lives in a residential facility, and relies on public transportation, then a weekly treatment plan may not be realistic without additional support, and the patient could become non-compliant. Or, if the patient is homeless, then a treatment plan that requires the use of a refrigerated antibiotic is most likely not a feasible option.
While much work has been done to demonstrate the deleterious effect of behaviors such as alcohol and tobacco use on health outcomes,14 many other social determinants particularly around physical and environmental factors have not been investigated as thoroughly or linked as deliberately to health outcomes. Housing, for example, has been studied with respect to the impact of homelessness on various conditions and housing related exposures.15–24 However, little work has been done around examining the health affects of housing density or with whom the patient lives.25 In a number of cases, the benefits of housing interventions including different types supportive housing have been demonstrated on physical and mental health.26–32 Moreover, knowledge regarding the patient’s physical living space, who the patient lives with, and living conditions would be of benefit clinicians and other stakeholders in providing patient-centered and more appropriate care and services.33
Electronic health record (EHR) systems provide an unprecedented opportunity to collect and analyze patient data at the point of care and for improving our understanding of disease and healthcare outcomes with secondary use of this data. If leveraged fully, SDOH data may be collected at the point of care within these systems and then re-used. For instance, SDOH can be analyzed along with clinical data to more fully evaluate patient outcomes, generate evidence-based care guidelines, and identify patients who may benefit from special services or interventions or those who may be at higher risk for preventable events. Despite the opportunity of EHRs, standard terminologies and well-designed discrete data collection tools for social history have not been widely developed and incorporated to different EHR systems. In most cases, SDOH documentation may be entered as structured data or unstructured text (e.g., in clinical notes or free-text data collection fields). This leaves a large gap in the data that can be used to enhance patient care as well as facilitate population health research to further the study of SDOH impact to health. The development of standard representations for SDOH information and ultimately optimized data collection tools will ultimately facilitate analytics, clinical decision support, and re-use and interoperability of this information.
To start bridging this gap, work to define and harmonize SDOH standards for inclusion in the EHR has been done,34, 35 including recent National Academy of Medicine (NAM; formerly Institute of Medicine) reports recommending social and behavioral domains and measures for EHRs for inclusion in Stage 3 Meaningful Use requirements.35 Some work (Chen et al. and Melton et al.)36, 37 has also been done to model social history from clinical notes and public health surveys including residence and living situation. The goal of this study is to expand upon these previous model representations for Residence, Living Situation, and Living Conditions through synthesis of a collection of interface terminologies, standards/specifications, documentation guidelines, and measures/surveys, evaluate the coherence of documentation, and ultimately contribute to a preliminary model representation that will be used to inform design and development of data collection tools in the EHR for these topic areas.38
Methods
The topic areas of Residence, Living Situation, and Living Conditions examined in this study are defined and summarized from a literature search in Table 1. This study was performed in three phases: (1) identifying sources potentially containing references to at least one of the three topic areas; (2) analyzing each data source for specific items related to each topic area; and, (3) synthesizing items into comprehensive representations for each of the three target topic areas. For the purpose of this analysis, all references found were weighted equally whether they were a concept, survey question, element, or member of a value list and termed as “items”.
Table 1:
Definitions and sentence/statement examples for target SDOH topic areas.
| Topic Area | Definition | Examples |
|---|---|---|
| RESIDENCE | Describes dwelling types, physical residence, and geographic location. Include safety considerations such as railings or number of floors and steps. | “Apartment building living” “Living in mobile home” “Lives in a nursing home” |
| LIVING SITUATION | With whom does the patient live such as roommates, family members, multiresident dwelling as well as how many others they live with. | “Lives alone” “Total number of people living in the household.” “Lives with family” |
| LIVING CONDITION | Environmental cleanliness and precautions against infection and disease. Includes sanitation, safety, inadequate water, sewage disposal, heating or cooling, presence of mold, odors, insects, rodents. | “Inadequate heating/cooling” “Presence of lead-based paint” “Cluttered living space” “Presence of mold” “Excessive pets” |
Qualifying sources were identified via literature and Internet searches using search terms that included: “<EHR or EMR> documentation”, “social documentation <standards or terminology>“, “social worker documentation <standards or terminology>“, “physical therapy documentation <standards or terminology>“, “occupational therapy documentation <standards or terminology>“, “social determinants documentation”, “<EHR or EMR> residence”, “<EHR or EMR> living situation”, and “<EHR or EMR> living conditions”. Additional sources were suggested by subject matter experts, and professional organization websites for physical therapy, occupational therapy, and social work were examined and also searched using the above list of terms. A source was included in the final set if it contained references to or specific items related to one or more of the three topic areas of Residence, Living Situation, or Living Conditions.
Each of the identified sources were grouped into one of four categories: (1) Interface Terminology, (2) Standards/Specifications/Coding Terminology, Vocabulary, (3) Documentation Guideline, and (4) Measures/Surveys. These categories were partly based upon the sources own definition, as well as the type and function of the source, i.e. how it is used in health IT and patient care. Each individual source was examined to identify specific items related to each of the three broad topic areas of Residence, Living Situation, or Living Conditions. The source search was limited to assessment-related items and excluded interventional references. Those sources that were available electronically were searched systematically using the provided search tools, such as the IHTSDO SNOMED-CT browser39 or the standard search mechanisms provided by each source. Sources available in book or paper form were searched manually. The initial list of search terms used was derived from the literature search. The list was further iteratively refined as sources were examined. The final list of search terms used included: “home”, “house”, “housing”, “residence”, “live”, “living”, “lives”, “people”, “mold”, “insect”, “rodent”, “water”, “heat”, “social”, and “density”. All sources were reexamined and searched by two reviewers using this final complete list of search terms. Any discrepancies between the primary and secondary review were subsequently evaluated and the final list of items was amended accordingly to compile a final comprehensive list by consensus. In cases where a source contained items from another standard or terminology source, the duplicates were excluded from the data set in the final analysis.
Each item identified from within each source was then mapped to one of the three topic areas of Residence, Living Situation, and Living Conditions. Each item was then further analyzed and then mapped to specific element axes and values from a previously defined model resulting in an enhanced and more comprehensive model for Residence, Living Situation, and Living Conditions.37 Element axes and values were added to the previous model representation or expanded on to accommodate findings from this review.
Results
A total of 27 data sources were identified as potentially having applicable items for one or more of the three topic areas. Of the 27 sources, seven sources were excluded during the initial analysis due to lack of detail or specificity. Those included the Meaningful Use Stage 2 Requirements and the EHR Certification Requirements, which did not include specific items directly related to the target topic areas for this study. The Nursing Management Minimum Data Set also did not contain relevant items. The Centers for Medicare Social Work Documentation Guidelines (MSWDG) and the Medicare Rehabilitation Documentation Requirements (MRDR) did contain references to the target topics areas; however, these sources were very high level and did not provide sufficiently detailed information appropriate for this work. Lastly, the Nursing Interventions Classification (NIC) and Uniform Terminology for Occupational Therapy contained items related to interventions and patient activity and not assessments, therefore these two sources were excluded from the final analysis. Secondary review of the 27 sources confirmed these results.
The remaining 20 sources contained applicable items for one or more of the three topic areas. Nineteen of the 20 sources contained some references to Residence totaling 643 items not including the United State Board on Geographic Names, which in itself contained millions of items for national and international named geographic locations (Table 2). SNOMED-CT had the highest number of items related to Residence at 265, followed by the US Census at 160, and third was HL7 at 58 items. Fifteen of the 20 sources contained items related to Living Situation totaling 96 items, the highest being again SNOMED-CT with 62 items, followed by openEHR with 7 items, and the US Census with 6 items. Lastly, 11 of the 20 sources had references to Living Conditions totaling 197 items. The source with the most references to Living Conditions was once again SNOMED-CT with 109 items followed by the Health Indicators Warehouse with 24 items and lastly NANDA-I with 19 items.
Table 2:
Sources and item counts
| # | Data Sources | # Items** | Total | Total Residence | Total Living Situation | Total Living Condition | |||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | |||||||
| Interface Terminology | 1 | The Omaha System: A Key to Practice, Documentation, and Information Management Second Edition40 | 28 | 27 | 0 | 28 | 11 | 1 | 16 |
| 2 | Nursing Interventions Classifications (NIC)41 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 3 | Nursing Outcomes Classifications (NOC)42 | 26 | 24 | 0 | 26 | 19 | 0 | 7 | |
| 4 | North American Nursing Diagnosis Association International Diagnoses: Definitions and Classifications (NANDA-I)43 | 34 | 22 | 0 | 34 | 14 | 1 | 19 | |
| 5 | Clinical Care Classification (CCC)44 | 6 | 4 | 0 | 6 | 2 | 2 | 2 | |
| 6 | Nursing Minimum Data Set (NMDS)45 | 6 | 0 | 0 | 6 | 5 | 1 | 0 | |
| 7 | Nursing Management Minimum Data Set (NMMDS)46 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 8 | Outcome and Assessment Information Set (OASIS)47 | 3 | 3 | 0 | 3 | 0 | 3 | 0 | |
| Standard, Specification, Coding Terminology, Vocabulary | 9 | Meaningful Use Stage 248 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10 | 2014 Electronic Health Record Certification Requirements49 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 11 | IOM Report Social and Behavioral Domains35 | 6 | 0 | 0 | 6 | 6 | 0 | 0 | |
| 12 | openEHR50 *** | 14 | 0 | 3 | 17 | 10 | 7 | 2 | |
| 13 | Systematized Nomenclature of Medicine--Clinical Terms (SNOMED CT) 51 | 402 | 402 | 34 | 436 | 265 | 62 | 109 | |
| 14 | Medical Subject Headings (MeSH) 52 | 17 | 5 | 1 | 18 | 15 | 2 | 1 | |
| 15 | Logical Observation Identifiers Names & Codes (LOINC®)53 | 4 | 4 | 7 | 11 | 8 | 3 | 0 | |
| 16 | Health Level 7 Version 3: Behavioral Health Model54 | 59 | 37 | 0 | 59 | 58 | 1 | 0 | |
| 17 | HL7 Fast Healthcare Interoperability Resources (FHIR)55 | 12 | 12 | 0 | 12 | 12 | 0 | 0 | |
| 18 | Public Health Information Network (PHIN) Vocabulary56 | 9 | 1 | 3 | 12 | 10 | 2 | 0 | |
| 19 | United States Board on Geographic Names (USBGN)57 | * | * | * | * | * | * | * | |
| Documentation Guideline | 20 | Occupational Therapy Practice Framework: Domain and Process (3rd Edition) (OT Framework)58 | 4 | 4 | 1 | 5 | 2 | 1 | 2 |
| 21 | Uniform Terminology for Occupational Therapy (UTOT) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 22 | CMS Social Work Documentation Guidelines (CMSSWDG)59 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 23 | Amer. Physical Therapy Assoc. Guidelines: Physical Therapy Documentation of Patient/Client Mgmt.58, 60 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | |
| 24 | Medicare Rehab. Documentation Requirements (MRDR)61 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Measure, Survey | 25 | PhenX Toolkit62, 63 | 32 | 32 | 3 | 35 | 25 | 3 | 7 |
| 26 | Health Indicators Warehouse (HIW)64 | 34 | 1 | 11 | 45 | 20 | 1 | 24 | |
| 27 | Unites States Census 65 | 158 | 26 | 16 | 174 | 160 | 6 | 8 | |
| TOTAL | 855 | 605 | 79 | 934 | 643 | 96 | 197 | ||
USBGN contains all national and international geographic location names.
# Items: A=Primary reviewer findings, B=Secondary reviewer confirmation of primary findings, C=Items added by secondary reviewer, i.e. items missed by primary reviewer.
Total Residence, Living Situation, Living condition counts not mutually exclusive for this source
Identified items were further manually evaluated and classified using the previously published model representations as a foundation (Table 3).37 Logical groupings of items were derived and individual items were mapped to an existing element axis or new elements axes were added to accommodate findings related specifically to the three topic areas. The most prevalent mapping was to Residence Detail with 13 sources containing items, and the second most prevalent was Residence Type, which was found in 12 of the 20 sources. Nine sources had items mapping to Living Situation Detail, 9 sources had items mapping to Living Conditions Detail, and 7 had items mapping to Living Condition Type. Of the 20 sources, PhenX Toolkit, openEHR and the US Census had the broadest coverage of elements and values.
Table 3:
Source item mapping to model elements.
| Element | Brief Description and Values | OMAHA | NOC | NANDA-I | CCC | NMDS | MA OASIS | IOM | OpenEHR | SNOMED CT | MeSH Terms | LOINC | Health Level 7 | FHIR | PHIN | USBGN | OT Framewk | APTAG | PhenX Toolkit | HIW | US Census | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Status | Current, past, or future status | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| 2 | Subject | Who (other than patient). | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||
| 3 | Patient | For whom the data are being recorded. | ✓ | ✓ | ✓ | |||||||||||||||||
| 4 | Family member | Member of family (spouse, partner, | ✓ | ✓ | ✓ | |||||||||||||||||
| 5 | Side of family | Maternal or paternal | ✓ | ✓ | ✓ | |||||||||||||||||
| 6 | Unrelated | Not related to patient | ✓ | ✓ | ✓ | |||||||||||||||||
| 7 | Other | Adopted | ✓ | ✓ | ✓ | |||||||||||||||||
| 8 | Negation | Absence | ✓ | |||||||||||||||||||
| 9 | Certainty | Confidence of statement | ✓ | |||||||||||||||||||
| 10 | Temporal | Items related to time and dates | ✓ | ✓ | ✓ | |||||||||||||||||
| 11 | Start date | Date began, exact or estimated | ✓ | |||||||||||||||||||
| 12 | End date | Date ended, exact or estimated | ✓ | |||||||||||||||||||
| 13 | Start age | Age began | ✓ | |||||||||||||||||||
| 15 | Duration | Length of time | ✓ | |||||||||||||||||||
| 16 | Quantity | Quantity of subject or detail | ✓ | |||||||||||||||||||
| 17 | Residence Age | Age of dwelling, exact or estimated | ✓ | |||||||||||||||||||
| 18 | Residence Build Time Point | Point in time when residence was built | ✓ | |||||||||||||||||||
| 19 | Residence Type | Type of physical dwelling | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| 20 | Geographic Location | Generic geographic location | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| 21 | Geographic Location detail | Specific location (country, state, zip) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| 22 | Residence Detail | Physical details (levels, stairs, railings) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| 23 | Living Situation Detail | Details related to living situation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||
| 24 | Living Conditions Type | Type of sanitation, hazards, clutter, | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||
| 25 | Living Conditions Detail | Details related to Living Condition Type | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
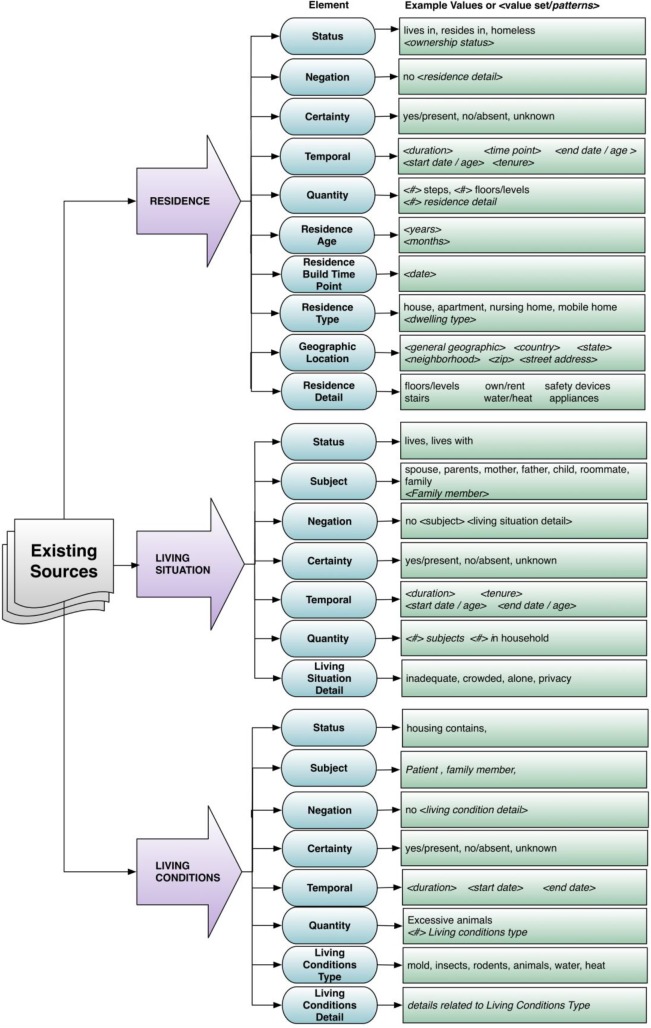
Model representations were developed from the mappings. The model representation for Residence uniquely contains items to describe the physical dwelling type, such as “House”, “Apartment “, or “Group Home” as well as details about that physical dwelling including presence and number stairs, and other safety items such as railings. There are also items to collect data about age of the residence, residence build time point as well as geographic location. The model representation for Living Situation includes more detail around Subject since this topic area is related to whom the patient is living with as well as Living situation Detail. Lastly, the model representation for Living Conditions includes an entity to document Living Conditions Type, which refers to the type of hazard such as “mold”, “insects”, or “animals” as well as Living Conditions Detail, which includes details about the Living Conditions Type or more general information about Living Conditions such as “Control environmental pests” (Figure 1).
Figure 1:
Preliminary Enhanced Model Representations of Residence, Living Situation, and Living Conditions.
Discussion
While SDOH represent important considerations in the provision of patient care and are also becoming more important in population health management, a number of important gaps in their use continue to exist. Currently, SDOH are not consistently or well-documented in the EHR, particularly the three topic areas on which this work is focused: Residence, Living Situation, and Living Conditions. By working towards synthesis of existing sources to derive enhanced models, we are starting to bridge this gap. Ultimately, the enhanced model representations could be used to inform the design and development of associated EHR documentation tools. To that end, our focus was to err on comprehensiveness in collecting assessment items associated with these topic areas rather than provided or resulting outcomes of those interventions.
A preliminary search for data sources in the form of interface terminologies, standards, specifications, coding terminologies, vocabularies, documentation guidelines, measures, and surveys yielded 27 possible sources that potentially contained items related to the three topic areas. While some sources were eliminated, collating the remaining 20 was highly informative. While no single source was completely comprehensive for all three topic areas, there was overall coverage to support an enhanced model representation. The most broadly comprehensive source was SNOMED-CT, which contained the highest number of relevant items overall, as well as ranking first for the highest number of items for each of the three individual topic areas. The US Census survey ranked second for total items as well as second for Residence (Table 2).
Collectively, the final set of 20 sources were very diverse in specificity primarily because they had distinct but different purposes and uses. For example, OMAHA, NIC, NOC, NANDA-I, and CCC are intended to assist in nursing documentation whereas HL7 is a standard intended for broader data exchange and the US Census and the OASIS are intended to collect data for population surveillance. Lastly, the US Board on Geographic Names was an outlier as it contained millions of very specific items for named geographic locations including city, state, county, country, as well as landmarks and bodies of water. This source could be helpful in standardizing how we model and record geographic locations. As a result of this variability in use and purpose, some sources contained high level, broad concepts, while others contained very specific items and very lengthy, detailed value lists. This diversity presented a challenge in the harmonization phase of the project. For example, SNOMED-CT lists “Housing, local environment and transport finding” with a diverse value list that includes residence types such as “apartment” and “mobile home” as well as living conditions such as “Lives in damp conditions” and “Presence of lead-based paint” while HL7 listed a specific item “primaryResidenceSetting PrimaryResidence” that has an extensive value list associated with it that contained types of physical dwellings. In many cases the lack of specificity caused an item to be counted in more than one topic area. One example of this was found in the Open EHR source that had an item “Description of the home environment”. This could include a description of any of the three topic areas and was counted as such in the final analysis. Ultimately, due to the variability in specificity of the items the data sources, in the final analysis and harmonization, all references to the three topic areas were weighted equally as items whether they were high level broad concepts, questions, elements, or individual values within a value list. This allowed for equal comparison and categorization of the items into the model representation.
Analysis of the final 20 data sources demonstrated that the topic areas of Residence, Living Situation, and Living Conditions are being included in those sources with Residence being most prevalent, specifically Residence Detail (details about the physical structure of the dwelling including safety features) and Residence Type (type of physical dwelling such as house, apartment, group home, nursing home). References to Living Situation were not very detailed. Many of the sources included some indication of whom the patient was living with but the value lists were very nonspecific including values such as “family” or “partner/spouse”. Items related to Living Conditions were mostly related to water, sewage, electricity, and heat availability with some references to sanitation specifically insects or rodents. Present, but much less prevalent, were references related to subject other than patient, as were references to temporality, certainty, quantity, and negation, i.e. the absence of an item or condition. Despite these unique challenges, the analysis of these sources, generated 934 items that were ultimately mapped to model elements resulting in enhanced model representations for the three topic areas.
The contributions of this work represent a step towards further informing biomedical standards for the representation of social determinants of health, specifically Residence, Living Situation, and Living Conditions. Next steps will be to further enhance this model representation and ultimately inform the design of EHR data collection tools through the incorporation of EHR unstructured and semi-structured text classifications. One unexpected challenge this work was the complexity of the sources and the difficulty in categorizing them into logical groupings. In future work it may be of interest to examine and develop standard definitions for these types of sources.
Conclusions
While this is a compilation and harmonization of a unique and diverse set of sources, overall, the diversity of the data sources contributed to a broader more detailed model than in previous work. Our results demonstrate that there are many sources that are currently being used to inform data collection with regards to Residence, Living Situation, and Living Conditions. While none of the sources were completely comprehensive, once harmonized they served to inform a more detailed model representation for the three topic areas that can be used towards developing more comprehensive data collection tools in the EHR.
Acknowledgements
This work was supported by the National Library of Medicine of the National Institutes of Health (R01LM011364) and University of Minnesota Clinical and Translational Science Award (8UL1TR000114-02). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
References
- 1.HealthyPeople. Gov: U.S. Department of Health & Human services. 2012. [cited 2015 3/2/2015]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39.
- 2.Hernandez LM, Blazer DG, editors. The National Institutes of. Washington (DC); 2006. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. [PubMed] [Google Scholar]
- 3.Social Determinants of Health: World Health Organization. 2014. [cited 2014 1/7/2014]. Available from: http://www.who.int/social_determinants/sdh_definition/en/index.html.
- 4.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–12. [PubMed] [Google Scholar]
- 5.Marmot MG, Shipley MJ, Rose G. Inequalities in death--specific explanations of a general pattern? Lancet. 1984;1(8384):1003–6. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 6.McGinnis JM. Health in America--the sum of its parts. JAMA. 2002;287(20):2711–2. doi: 10.1001/jama.287.20.2711. [DOI] [PubMed] [Google Scholar]
- 7.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995. Spec No:80-94. [PubMed]
- 8.Babor TF, Sciamanna CN, Pronk NP. Assessing multiple risk behaviors in primary care. Screening issues and related concepts. Am J Prev Med. 2004;27(2):42–53. doi: 10.1016/j.amepre.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 9.Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, et al. US Housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–14. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bisgaier J, Rhodes KV. Cumulative adverse financial circumstances: associations with patient health status and behaviors. Health Soc Work. 2011;36(2):129–37. doi: 10.1093/hsw/36.2.129. [DOI] [PubMed] [Google Scholar]
- 11.Vijayaraghavan M, Jacobs EA, Seligman H, Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved. 2011;22(4):1279–91. doi: 10.1353/hpu.2011.0131. [DOI] [PubMed] [Google Scholar]
- 12.Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socioeconomic outcomes. Cochrane Database Syst Rev. 2013;2:CD008657. doi: 10.1002/14651858.CD008657.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shaw M. Housing and public health. Annu Rev Public Health. 2004;25:397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- 14.Jane-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25(6):515–36. doi: 10.1080/09595230600944461. [DOI] [PubMed] [Google Scholar]
- 15.Kipke MD, Weiss G, Wong CF. Residential status as a risk factor for drug use and HIV risk among young men who have sex with men. AIDS Behav. 2007;11(6):56–69. doi: 10.1007/s10461-006-9204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Milloy MJ, Marshall BD, Montaner J, Wood E. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9(4):364–74. doi: 10.1007/s11904-012-0137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suglia SF, Duarte CS, Sandel MT. Housing quality, housing instability, and maternal mental health. J Urban Health. 2011;88(6):1105–16. doi: 10.1007/s11524-011-9587-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinstein LC, Lanoue MD, Plumb JD, King H, Stein B, Tsemberis S. A primary care-public health partnership addressing homelessness, serious mental illness, and health disparities. J Am Board Fam Med. 2013;26(3):279–87. doi: 10.3122/jabfm.2013.03.120239. [DOI] [PubMed] [Google Scholar]
- 19.Costa-Font J. Housing assets and the socio-economic determinants of health and disability in old age. Health Place. 2008;14(3):478–91. doi: 10.1016/j.healthplace.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Rollins C, Glass NE, Perrin NA, Billhardt KA, Clough A, Barnes J, et al. Housing instability is as strong a predictor of poor health outcomes as level of danger in an abusive relationship: findings from the SHARE Study. J Interpers Violence. 2012;27(4):623–43. doi: 10.1177/0886260511423241. [DOI] [PubMed] [Google Scholar]
- 21.Leff HS, Chow CM, Pepin R, Conley J, Allen IE, Seaman CA. Does one size fit all? What we can and can’t learn from a meta-analysis of housing models for persons with mental illness. Psychiatr Serv. 2009;60(4):473–82. doi: 10.1176/ps.2009.60.4.473. [DOI] [PubMed] [Google Scholar]
- 22.Ryan TJ, Arnold KJ. Residential carbon monoxide detector failure rates in the United States. Am J Public Health. 2011;101(10):e15–7. doi: 10.2105/AJPH.2011.300274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adamkiewicz G, Zota AR, Fabian MP, Chahine T, Julien R, Spengler JD, et al. Moving environmental justice indoors: understanding structural influences on residential exposure patterns in low-income communities. Am J Public Health. 2011;101(1):S238–45. doi: 10.2105/AJPH.2011.300119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson SL, Bonnie RJ. A systematic examination of smoke-free policies in multiunit dwellings in Virginia as reported by property managers: implications for prevention. Am J Health Promot. 2011;26(1):37–44. doi: 10.4278/ajhp.091005-QUAN-329. [DOI] [PubMed] [Google Scholar]
- 25.Standish K, Nandi V, Ompad DC, Momper S, Galea S. Household density among undocumented Mexican immigrants in New York City. J Immigr Minor Health. 2010;12(3):310–8. doi: 10.1007/s10903-008-9175-x. [DOI] [PubMed] [Google Scholar]
- 26.Nath SB, Wong YL, Marcus SC, Solomon P. Predictors of health services utilization among persons with psychiatric disabilities engaged in supported independent housing. Psychiatr Rehabil J. 2012;35(4):315–23. doi: 10.2975/35.4.2012.315.323. [DOI] [PubMed] [Google Scholar]
- 27.Fenwick E, Macdonald C, Thomson H. Economic analysis of the health impacts of housing improvement studies: a systematic review. J Epidemiol Community Health. 2013;67(10):835–45. doi: 10.1136/jech-2012-202124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomson H, Petticrew M, Douglas M. Health impact assessment of housing improvements: incorporating research evidence. J Epidemiol Community Health. 2003;57(1):11–6. doi: 10.1136/jech.57.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thomson H, Thomas S, Sellstrom E, Petticrew M. The health impacts of housing improvement: a systematic review of intervention studies from 1887 to 2007. Am J Public Health. 2009;99(3):S681–92. doi: 10.2105/AJPH.2008.143909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng AL, Lin H, Kasprow W, Rosenheck RA. Impact of supported housing on clinical outcomes: analysis of a randomized trial using multiple imputation technique. J Nerv Ment Dis. 2007;195(1):83–8. doi: 10.1097/01.nmd.0000252313.49043.f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henwood BF, Cabassa LJ, Craig CM, Padgett DK. Permanent supportive housing: addressing homelessness and health disparities? Am J Public Health. 2013;103(Suppl 2):S188–92. doi: 10.2105/AJPH.2013.301490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobs DE, Brown MJ, Baeder A, Sucosky MS, Margolis S, Hershovitz J, et al. A systematic review of housing interventions and health: introduction, methods, and summary findings. J Public Health Manag Pract. 2010;16(5):S5–10. doi: 10.1097/PHH.0b013e3181e31d09. [DOI] [PubMed] [Google Scholar]
- 33.de Vet R, van Luijtelaar MJ, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JR. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health. 2013;103(10):e13–26. doi: 10.2105/AJPH.2013.301491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Estabrooks PA, Boyle M, Emmons KM, Glasgow RE, Hesse BW, Kaplan RM, et al. Harmonized patient-reported data elements in the electronic health record: supporting meaningful use by primary care action on health behaviors and key psychosocial factors. J Am Med Inform Assoc. 2012;19(4):575–82. doi: 10.1136/amiajnl-2011-000576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.IOM (Institute of Medicine) Washington D.C: 2014. Capturing social and behavioral domains and measures in electronic health records: Phase 2. [PubMed] [Google Scholar]
- 36.Chen ES, Manaktala S, Sarkar IN, Melton GB. A multi-site content analysis of social history information in clinical notes. AMIA Annu Symp Proc; 2011; pp. 227–36. [PMC free article] [PubMed] [Google Scholar]
- 37.Melton GB, Manaktala S, Sarkar IN, Chen ES. Social and behavioral history information in public health datasets. AMIA Annu Symp Proc; 2012; pp. 625–34. [PMC free article] [PubMed] [Google Scholar]
- 38.Winden TJ, Chen ES, Lindemann E, Wang Y, Carter EW, Melton GB, editors. Evaluating Living Situation, Occupation, and Hobby/Activity Information in the Electronic Health Record. American Medical Informatics Association Annual Symposium Proceedings 2014; 2014; Washington DC. http://www.AMIA.orgAmerican Medical Informatics Association 2014. [Google Scholar]
- 39.International Health Terminology Standards Development Organisation (IHTSDO) SNOMED CT Browser. 2016. [cited 2016 3/8/2016]. v1.32:[Available from: http://browser.ihtsdotools.org/?perspective=full&conceptId1=404684003&edition=us-edition&release=v20150901&server=https://browser-aws-1.ihtsdotools.org/api/snomed&langRefset=900000000000509007.
- 40.Martin KS. Second. St. Louis, Missouri: Elsevier Saunders; 2005. The Omaha System: A Key to Practice, Documentaiton, and Information Management. [Google Scholar]
- 41.Bulecheck GM, Butcher HK, Dochterman JM, Wagner CM. Sixth. Elsevier; 2013. Nursing Interventions Classification (NIC) p. 608. [Google Scholar]
- 42.Moorhead S, Johnson M. P, Maas M.L, Swwanson E. Fourth. Mosby Elsevier; 2008. Nursing Outcomes Classification (NOC) p. 912. [Google Scholar]
- 43.Herdman T, Kamitsuru S. Tenth. Osxford: Wiley Blackwell; 2014. NANDA International Nursing Diagnoses: Definitions and Classification 2015-2017. [Google Scholar]
- 44.Saba VK. Springer Publishing Company; 2012. Clinical Care Classification (CCC) System Version 2.5 User’s Guide; p. 257. [Google Scholar]
- 45.Goossen W, Epping P, Feuth T, Dassen T, Hasman A, van den Heuvel W. A Comparison of Nursing Minimal Data Sets. Journal of the American Medical Informatics Association: JAMIA. 1998;5(2):152–163. doi: 10.1136/jamia.1998.0050152. Journal of the American Medical Informatics Association : JAMIA 1998;5(2):152-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huber D, Schumacher L, Delaney C. Nursing Management Minimum Data Set (NMMDS) Journal of Nursing Administration. 1997 Apr;27(4):42–8. doi: 10.1097/00005110-199704000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Outcome and Assessment Information Set (OASIS), OASIS-C1/ ICD-9 Version. Centers for Medicaid & Medicare Services. Department of Health and Human Services. [cited 2015 3/7/2015]. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/OASIS/index.html?redirect=/oasis/
- 48.Meaningful Use Stage 2 Final Rule. 2014. [cited 2015 3/2/2015]. Available from: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Stage_2.html.
- 49.45 CFR Part 170 Health Information Technology: Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology. Revisions to the Permanent Certification Program for Health Information Technology Federal Register2012. 2014. [PubMed]
- 50.OpenEHR Clinical Knowledge Manager. 2015. [cited 2015 3/2/2015]. Available from: http://www.openehr.org/ckm/
- 51.US Edition of SNOMED CT(R): March 2015 Release. U.S. National Library of Medicine. [cited 2015 3/1/2015]. Available from: https://uts.nlm.nih.gov/home.html.
- 52.U.S. National Library of Medicine, Medical Subject Headings MeSH Browser (2015 MeSH) 2015. [cited 2015 3/8/2015]. Available from: http://www.nlm.nih.gov/mesh/MBrowser.html.
- 53.Logical Observation Identifiers Names and Codes (LOINC®) Regenstrief Institute, Inc; 2015. [cited 2015 3/8/2015]. Available from: http://www.loinc.org. [Google Scholar]
- 54.Health Level 7. HL7 Version 3 Domain Analysis Model: Summary Behavioral Health Record. Release 1 – US Realm. 2013. [cited 2015 3/9/2015]. Available from: http://www.hl7.org/implement/standards/product_brief.cfm?product_id=307.
- 55.Health Level 7. Fast Healthcare Interoperability Resources. 2015. [cited 2015 3/9/2015]. Available from: http://www.hl7.org/implement/standards/fhir/
- 56.Public Health Information Network (PHIN) Vocabulary. Centers for Disease Control and Prevention. 2015. [cited 2015 3/2/2015]. Available from: http://www.cdc.gov/phin/activities/vocabularv.html.
- 57.United States Board on Geographic Names, U.S. Geological Survey. U.S. Department of Commerce. 2015. [updated 10/10/2014; cited 2015 3/7/2015]. Available from: http://geonames.usgs.gov/domestic/
- 58.American Occupational Therapy Association. Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy. (3) 2014;68(1):S1–S48. [PubMed] [Google Scholar]
- 59.National Association of Social Workers. Documenting for medicare: tips for clinical social workers. [cited 2015 3/9/2015]. Available from: http://careers.socialworkers.org/documents/MedicareDocumentationTips.pdf.
- 60.American Physical Therapy Association. Guidelines: Physical Therapy Documentation of Patient/Client Management BOD G03-05-16-41. 2014. [cited 2015 3/9/2015]. Available from: http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Practice/DocumentationPatientClientManagement.pdf - search=%22guidelines%20documentation%22>.
- 61.Medicare Benefit Policy Manual. Rev. 189, 06-27-14 ed2014.
- 62.Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, et al. The PhenX Toolkit: get the most from your measures. Am J Epidemiol. 2011;174(3):253–60. doi: 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.PhenX Toolkit. [cited 2015 3/9/2015]. Available from: https://www.phenx.org/Default.aspx?tabid=59.
- 64.Health Indicators Warehouse. Centers for Disease Control. [cited 2014 6/15/2014]. Available from: http://www.healthindicators.gov.
- 65.United States Census Data, US Census Bureau, Department of Commerce. [cited 2015 3/1/2015]. Available from: http://www.census.gov/data.html.