Abstract
Patient portal research has focused on medical outpatient settings, with little known about portal use during hospitalizations or by surgical patients. We measured portal adoption among patients admitted to surgical services over two years. Surgical services managed 37,025 admissions of 31,310 unique patients. One-fourth of admissions (9,362, 25.3%) involved patients registered for the portal. Registration rates were highest for admissions to laparoscopic/gastrointestinal (55%) and oncology/endocrine (50%) services. Portal use occurred during 1,486 surgical admissions, 4% of all and 16% of those registered at admission. Inpatient portal use was associated with patients who were white, male, and had longer lengths of stay (p < 0.01). Viewing health record data and secure messaging were the most commonly used functions, accessed in 4,836 (72.9%) and 1,626 (24.5%) user sessions. Without specific encouragement, hospitalized surgical patients are using our patient portal. The surgical inpatient setting may provide opportunities for patient engagement using patient portals.
Introduction
Patient portals are web-based applications that enable patients to view portions of their electronic health record (EHR) and interact with their healthcare providers.1-3 The United States government defines a patient portal as “a secure online website that gives patients convenient 24-hour access to personal health information from anywhere with an Internet connection.”2 The data within a portal is typically managed by a healthcare institution and allows patients to have access to personal health information, including recent doctor visits, discharge summaries, medications, immunizations, allergies, and laboratory results. More advanced portals enable patients to schedule appointments, message their providers4, and sometimes maintain personal health records.5 Increasingly, health care systems offer portals to their patients, and consumers adopt them quickly.6, 7 Hospitals are motivated to provide patient portals by financial incentives created by the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 and Meaningful Use criteria.8-9 Consumers are also demanding such technology and transparency from their health care providers.10
The majority of research about patient portals has been performed in the primary care or medical specialty settings with a paucity of research focusing on acute care specialties, such as surgery, or acute care settings, such as the hospital.11-15 Two recent systematic reviews of over 100 studies on the effectiveness of patient portals revealed only three studies exploring portal use outside of primary care or medical specialties.16, 17 Our prior research demonstrated that after broad deployment of a patient portal across clinical specialties, surgeons were the second most frequent specialty to use patient-provider messaging.18 Further, messaging adoption by surgical patients and providers grew rapidly across surgical subspecialties.6 As healthcare organizations increasingly deploy patient portals across clinical specialties to meet Meaningful Use objectives, we anticipate the use of patient portals by the understudied acute care population to continue to grow.
Many trials investigating patient portals involve outpatient management of chronic diseases, but very little is known regarding patient use of patient portals while in the hospital for an acute illness or after surgery.18, 19 Masterson et al. have described their development of a personalized inpatient portal to improve patient engagement while in the hospital, but results are not yet reported.11 Very small studies have assessed the efficacy of providing patients with tablet computers for specific encouragement of portal use during inpatient stay, showing patients utilized and appreciated the ability to view their health information.20, 21 At Brigham and Women’s Hospital, a web-based patient-centered tool kit offering many common patient portal functions was implemented and evaluated in the medical intensive care unit and oncology unit settings.22 Studies of this system have shown encouraging trends for the adoption and sustained usage of such technologies in the acute care setting.23 Although the functions commonly offered by patient portals meet important needs of hospitalized patients24, 25, there has been a reluctance to encourage portal usage by hospitalized patients. Many patient portals have policies that would discourage inpatient usage, such as specific delays for availability of test results or several business day expectations for answering of secure messages.26 Nonetheless, healthcare consumers often find innovative ways to use health information technologies. To address existing gaps in the literature about the use of patient portals by surgical patients in acute care settings, we sought to characterize the adoption and use of a patient portal by patients admitted to surgical services at a large academic medical center.
Methods
Study Setting
This study was conducted at Vanderbilt University Medical Center (VUMC), a private, non-profit, academic institution in Nashville, Tennessee, which provides primary and regional referral care to adults and children. VUMC encompasses Vanderbilt University Hospital (VUH) and Vanderbilt Children’s Hospital (VCH), with over 900 inpatient beds and 50,000 inpatient admissions per year.
Patient Portal
VUMC launched the My Health At Vanderbilt (MHAV) patient portal in 2005, with implementation across the clinical enterprise completed in 2007. After initial implementation, a physician champion introduced MHAV to providers, and technical support staff was available to patients, physicians, and staff as the portal was introduced in individual clinical units. MHAV was promoted to patients through flyers posted in outpatient clinics. This process was repeated, beginning in adult primary care, and then extending to adult and pediatric specialties. Programs did not promote MHAV use in the inpatient setting until 2014, when a link to the MHAV was made available through interactive television in the hospital rooms of VUH.
All patients who receive medical care at VUMC may register for access to MHAV. MHAV users may authorize another individual, termed a delegate, to access their MHAV account on their behalf. Our policies for MHAV accounts for pediatric patients are similar to those developed for other major children’s hospitals.5 For patients under 13 years of age, parents or guardians (called surrogates) may access MHAV account on behalf of their child. Adolescents 13 years of age and older may have their own, parent-controlled MHAV accounts.26 MHAV provides access to selected portions of the medical record, appointment scheduling, account and bill management, targeted health education materials, and secure messaging with healthcare providers.26, 27 MHAV is now a well-established patient portal, with over 327,000 registered users and over 300,000 logins per month by 50,000 unique users. MHAV is directly linked to the VUMC EHR, StarPanel, and thus, content is continually updated. MHAV allows access to selected health information from the EHR, including clinical visit summaries, laboratory results, and medication lists. Some information is immediately available and other sensitive content is only viewable after short delays to allow for physician review and management. MHAV messages are managed by clinical groups based on provider preferences. Some providers directly answer all patient-initiated messages, and others have messages triaged by administrative and clinical staff members, any of whom may respond. Tailored educational materials are available within MHAV based on patient problems and medication lists. Specific policies and procedures developed to enhance patient and provider adoption are published elsewhere.26
Study Population
We examined all admissions to surgical services at VUMC and all use of the MHAV patient portal by patients admitted by a surgical service or their delegates or surrogates between January 1, 2012 and December 31, 2013. This time period was chosen after a rise in anecdotal reporting of inpatient MHAV usage and prior to the promotion of portal registration and usage through interactive television in the hospital. We sought to examine inpatient portal access in the absence of specific programs to promote such usage.
Measures
For each admission during the study period, we recorded patient age, sex, and race, as well as admitting service, International Classification of Disease (ICD-9) admission diagnosis code, and length of stay. We categorized admitting services using 21 surgical specialties reflecting the departmental organization at VUMC: cardiac, thoracic, otolaryngology, emergency general, general, gastrointestinal/laparoscopic, liver transplant, neurosurgery, oncology/endocrinology, oral/maxillofacial, orthopedic, pediatric, pediatric trauma, pediatric urology, plastic, renal transplant, spinal, trauma, burn, urology, and vascular. MHAV users include VUMC patients who have registered for MHAV, delegates, and surrogates. For each admission, we considered the patient registered with MHAV if they had a portal account by the time of discharge. MHAV use during a hospital admission was defined as any MHAV activity through the admitted patient’s or any affiliated delegate/surrogate accounts occurring between the date/time of admission and the date/time of discharge. We determined the total number of inpatient MHAV user sessions across user types. For each session, we classified the type of portal function utilized as account management, appointments, education materials, laboratory test results, messaging, or other.
Analysis
We calculated the total number of inpatient admissions to each surgical service, as well as the number of these surgical patients who were registered for MHAV either before or during their admission. We also calculated the number of these patients who specifically registered for MHAV during inpatient stay. We constructed descriptive distributions and summary statistics of MHAV registration and use status across patient demographics and admission characteristics. Continuous variables were summarized with medians and inter-quartile ranges. Categorical variables were summarized as counts and frequencies. We modeled inpatient use among admissions of registered patients using a logistic model controlling for month of admission, race, sex, age at admission, length of stay, and admitting service. Standard errors were adjusted to account for correlation among multiple admissions for the same patient. All analyses were conducted in R version 3.0.1.28
Results
During the study period, VUMC surgical services managed 37,025 admissions of 31,310 unique patients. Demographics of the unique patients admitted to a surgical service listed in Table 1.
Table 1.
Demographic and clinical characteristics of unique patients admitted to a surgical service at VUMC 2012-2013. Counts and percentages or median and IQR.
| Characteristic | All | % | VCH | % | VUH | % |
|---|---|---|---|---|---|---|
| Total | 31,310 | 5,002 | 26,308 | |||
| Race | ||||||
| White | 26,380 | 84.3 | 3,845 | 76.9 | 22,535 | 85.7 |
| Black | 3,497 | 11.2 | 715 | 14.3 | 2,782 | 10.6 |
| Unknown | 975 | 3.1 | 298 | 6 | 677 | 2.6 |
| Asian/Pacific Islander | 355 | 1.1 | 123 | 2.5 | 232 | 0.9 |
| Native American/Alaskan | 103 | 0.3 | 21 | 0.4 | 82 | 0.3 |
| Sex | ||||||
| Male | 17,939 | 57.3 | 2,875 | 57.5 | 15,064 | 57.3 |
| Female | 13,371 | 42.7 | 2,127 | 42.5 | 11,244 | 42.7 |
| Age at first admission (years) | 49 (IQR 26-63) | 6 (IQR 2-13) | 54 (IQR 39-65) | |||
| Age categories (decades in years) | ||||||
| <10 | 3,175 | 10.1 | 3,152 | 63 | 23 | 0.1 |
| 10-19 | 2,694 | 8.6 | 1,792 | 35.8 | 902 | 3.4 |
| 20-29 | 2,863 | 9.1 | 39 | 0.8 | 2,824 | 10.7 |
| 30-39 | 3,099 | 9.9 | 8 | 0.2 | 3,091 | 11.7 |
| 40-49 | 4,040 | 12.9 | 4 | 0.1 | 4,036 | 15.3 |
| 50-59 | 5,457 | 17.4 | 4 | 0.1 | 5,453 | 20.7 |
| 60-69 | 5,609 | 17.9 | 3 | 0.1 | 5,606 | 21.3 |
| 70-79 | 3,218 | 10.3 | 0 | 0 | 3,218 | 12.2 |
| 80-89 | 1,035 | 3.3 | 0 | 0 | 1,035 | 3.9 |
| 90 or older | 120 | 0.4 | 0 | 0 | 120 | 0.5 |
| Age categories (pediatric) | ||||||
| 0-1yr | 1156 | 3.7 | 1145 | 22.9 | 11 | 0 |
| 2-5yrs | 1,142 | 3.6 | 1,132 | 22.6 | 10 | 0 |
| 6-10yrs | 1,072 | 3.4 | 1,070 | 21.4 | 2 | 0 |
| 11-15yrs | 1,231 | 3.9 | 1,208 | 24.2 | 23 | 0.1 |
| 16-18yrs | 928 | 3 | 364 | 7.3 | 564 | 2.1 |
| over 18yrs | 25,781 | 82.3 | 83 | 1.7 | 25,698 | 97.7 |
MHAV Registration Status
Of the 37,025 admissions during the study period, 9,362 (25.3%) involved patients registered for MHAV and 7,549 (24.1%) unique patients were registered for MHAV during at least one admission in the study period. In 194 admissions, the patient registered for MHAV during an inpatient stay rather than enrolling in MHAV prior to the admission. The MHAV registration rate was higher at VUH than VCH, with 27.0% of unique patients admitted to VUH having a portal account compared to 8.8% among unique patients admitted to VCH.
Table 2 presents the demographics for all patients admitted to a surgical service compared to those registered for MHAV. Patients registered for MHAV differed from the entire patient cohort on each demographic characteristic, both overall and within each hospital (p < 0.01) with the exception of sex among patients admitted to VCH (p = 0.29). White and Asian/Pacific Islander patients were more likely to have a MHAV account than were Black, Native American/Alaskan, and other/unreported race patients. Overall, patients in their 50s and 60s were most likely to be registered for MHAV. Among patients admitted to VUH, female patients were more likely to be registered for MHAV compared to male patients (33.3% vs. 22.3%, respectively).
Table 2.
Demographic and clinical characteristics of unique patients admitted to a surgical service at VUMC 2012-2013 by MHAV registration status. Counts and percentages or median and IQR.
| Characteristic | All (n) | Registered (n) | Registered (% of total) |
|---|---|---|---|
| Race | |||
| White | 26,380 | 6,812 | 25.8 |
| Asian/Pacific Islander | 355 | 88 | 24.8 |
| Native American/Alaskan | 103 | 18 | 17.5 |
| Black | 3,497 | 545 | 15.6 |
| Unknown | 975 | 86 | 8.8 |
| Sex | |||
| Female | 13,371 | 3,941 | 29.5 |
| Male | 17,939 | 3,608 | 20.1 |
| Age at first admission (years) | 49 (IQR 26-73) | 54 (IQR 41-64) | |
| Age categories (decades) | |||
| < 10 | 3,175 | 277 | 8.7 |
| 10-19 | 2,694 | 202 | 7.5 |
| 20-29 | 2,863 | 452 | 15.8 |
| 30-39 | 3,099 | 834 | 26.9 |
| 40-49 | 4,040 | 1,193 | 29.5 |
| 50-59 | 5,457 | 1,768 | 32.4 |
| 60-69 | 5,609 | 1,821 | 32.5 |
| 70-79 | 3,218 | 801 | 24.9 |
| 80-89 | 1,035 | 186 | 18 |
| 90 or older | 120 | 15 | 12.5 |
| Age categories (pediatric) | |||
| < 6 months | 542 | 34 | 6.3 |
| 6-12 months | 248 | 33 | 13.3 |
| 12-24 months | 366 | 50 | 13.7 |
| 2-5yrs | 1,142 | 96 | 8.4 |
| 6-10yrs | 1,072 | 75 | 7.0 |
| 11-15yrs | 1,231 | 91 | 7.4 |
| 16-18yrs | 928 | 69 | 7.4 |
| over 18yrs | 25,781 | 7,101 | 27.5 |
The number and proportion of patients registered for MHAV by surgical admitting service are presented in Table 3. At the adult hospital, VUH, 8,851 of 31,448 (28.1%) admissions to surgical services involved patients registered for MHAV compared to 511 of 5,577 surgical admissions (9.2%) at VCH. The surgical services with the highest rate of MHAV registration were adult gastrointestinal/laparoscopic (54.5%) and adult oncology/endocrinology (49.6%). The surgical services with the lowest rates of MHAV registration were pediatric trauma (1.2%) and burn (1.8%).
Table 3.
Surgical admitting service and MHAV registration among 2012-2013 VUMC admissions, categorized into Vanderbilt Children’s Hospital (VCH) and Vanderbilt University Hospital (VUH). (Reg = Registered)
| Surgical Admitting Service | All | Reg (n) | Reg (%) | All (VCH) | Reg(n) (VCH) | Reg(%) (VCH) | All (VUH) | Reg(n) (VUH) | Reg(%) (VUH) |
|---|---|---|---|---|---|---|---|---|---|
| Total | 37,025 | 9,362 | 25.3 | 5,577 | 511 | 9.2 | 31,448 | 8,851 | 28.1 |
| Year of admission | |||||||||
| 2012 | 18,270 | 4,471 | 24.5 | 2,655 | 215 | 8.1 | 15,615 | 4,256 | 27.3 |
| 2013 | 18,755 | 4,891 | 26.1 | 2,922 | 296 | 10.1 | 15,833 | 4,595 | 29 |
| GI/Laparoscopic | 1,574 | 858 | 54.5 | 1 | 1 | 100 | 1,573 | 857 | 54.5 |
| Oncology/Endocrine | 1,206 | 598 | 49.6 | 0 | 0 | 0 | 1,206 | 598 | 49.6 |
| Spinal | 27 | 13 | 48.1 | 0 | 0 | 0 | 27 | 13 | 48.1 |
| Thoracic | 1,068 | 481 | 45 | 1 | 1 | 100 | 1,067 | 480 | 45 |
| General | 2,006 | 855 | 42.6 | 23 | 1 | 4.3 | 1,983 | 854 | 43.1 |
| Renal Transplant | 504 | 205 | 40.7 | 4 | 0 | 0 | 500 | 205 | 41 |
| Liver Transplant | 534 | 207 | 38.8 | 3 | 1 | 33.3 | 531 | 206 | 38.8 |
| Neurological | 4,239 | 1,461 | 34.5 | 391 | 84 | 21.5 | 3,848 | 1,377 | 35.8 |
| Urology | 2,658 | 805 | 30.3 | 50 | 4 | 8 | 2,608 | 801 | 30.7 |
| Cardiac | 957 | 279 | 29.2 | 9 | 0 | 0 | 948 | 279 | 29.4 |
| Emergency General | 1,444 | 385 | 26.7 | 1 | 0 | 0 | 1,443 | 385 | 26.7 |
| Otolaryngology | 2,030 | 521 | 25.7 | 574 | 75 | 13.1 | 1,456 | 446 | 30.6 |
| Orthopedic/Rehab | 6,602 | 1,672 | 25.3 | 1,011 | 84 | 8.3 | 5,591 | 1,588 | 28.4 |
| Vascular | 525 | 121 | 23 | 1 | 0 | 0 | 524 | 121 | 23.1 |
| Plastic | 1,435 | 283 | 19.7 | 451 | 53 | 11.8 | 984 | 230 | 23.4 |
| Oral/Maxillofacial | 286 | 44 | 15.4 | 49 | 2 | 4.1 | 237 | 42 | 17.7 |
| Pediatric Urology | 269 | 25 | 9.3 | 269 | 25 | 9.3 | 0 | 0 | 0 |
| Pediatric | 2,292 | 175 | 7.6 | 2,287 | 175 | 7.7 | 5 | 0 | 0 |
| Trauma | 6,032 | 352 | 5.8 | 10 | 0 | 0 | 6,022 | 352 | 5.8 |
| Burn | 1,083 | 19 | 1.8 | 191 | 2 | 1 | 892 | 17 | 1.9 |
| Pediatric Trauma | 254 | 3 | 1.2 | 251 | 3 | 1.2 | 3 | 0 | 0 |
Inpatient Use of MHAV
Portal usage occurred during 1,486 surgical admissions (4% of all admissions and 16% of registered user admissions) involving 1,270 unique patients. 6,634 portal user sessions occurred during surgical inpatient admissions. For admissions during which MHAV was accessed, the median number of MHAV sessions was 2 (IQR 1-4); however, during some admissions, patients accessed MHAV more than 20 times, with a few users accessing MHAV over 80 times during admission. Normalizing by length of stay, the median number of MHAV sessions per inpatient day was 2.0 (IQR 1.0-3.1) among admissions with MHAV use.
In unadjusted tests among admissions involving MHAV registered patients, admissions with inpatient portal use differed from those without portal use in terms of length of stay, race, sex, and admitting service (p < 0.01), but did not differ on patient age. These findings were observed overall and within VUH admissions only. Among admissions to VCH, admissions with portal use were longer than admissions without use (median LOS 5 vs. 3 days; p < 0.01).
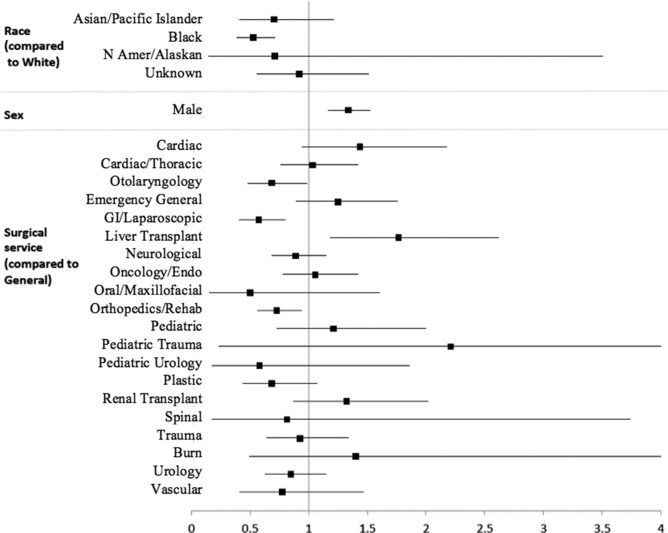
Adjusting for patient demographics and admission characteristics, white race, male sex, increased length of hospital stay, and admitting service were associated with inpatient portal use (p < 0.01). Figure 1 demonstrates the odds ratios (OR) for inpatient portal use based on demographics and admission service. Black patients were significantly less likely than white patients to use the portal or have MHAV accessed on their behalf during hospitalization (OR 0.53, 95% CI 0.39-0.71). Male patients were more likely to use the portal or have MHAV accessed on their behalf during hospitalization than female patients (OR 1.33, 95% CI 1.17-1.52). Compared to general surgery admissions, admissions to the liver transplant service were at 76% higher odds of portal use (OR 1.76, 95% CI 1.19-2.62). Admissions to the liver transplant service were also more likely to use the portal than those to neurological, plastic, gastrointestinal/laparoscopic, otolaryngology, and orthopedic surgery services. Otolaryngology (OR 0.69, 95% CI 0.48-0.98), gastrointestinal/laparoscopic (OR 0.57, 95% CI 0.41-0.80), and orthopedic surgery (OR 0.73, 95% CI 0.56-0.94) admissions showed a decreased likelihood of portal use compared to general surgery admissions.
Figure 1.
Odds ratios for inpatient MHAV use among registered admissions
Among admissions with inpatient use of MHAV, the portal was accessed through the patient’s account in 92.7% of admissions, through a delegate account in 2.6% of admissions, and through a surrogate account in 5.5% of admissions (see Table 4). Although patients utilized a variety of portal functions, viewing health record data (i.e. laboratory results, medication lists, or clinical documents) and secure patient-provider messaging were the most common, accessed in 4,836 (72.9%) and 1,626 (24.5%) of total inpatient user sessions, respectively (see Table 4).
Table 4.
Number of inpatient user sessions accessing each MHAV function, overall and by user role.
| Any user (n) | Patient (n) | Delegate (n) | Surrogate (n) | |
|---|---|---|---|---|
| Total sessions | 6,634 | 6,243 | 127 | 264 |
| Viewing health record | 4,836 | 4,563 | 77 | 196 |
| dMaetas saging | 1,626 | 1,489 | 54 | 83 |
| Educational materials | 521 | 521 | 0 | 0 |
| Appointments | 495 | 462 | 10 | 23 |
| Account management | 72 | 67 | 2 | 3 |
| Other | 120 | 112 | 1 | 7 |
Tables 5 and 6 describe the most prevalent ICD-9 diagnosis codes for all admissions and admissions with inpatient use of the patient portal to VUH (adults) and VCH (pediatrics), respectively. The three most frequent diagnoses among adult patients who utilized the portal while hospitalized were postoperative infection, morbid obesity, and intestinal obstruction. In contrast, the 3 most frequent diagnoses among pediatric patients who used the portal while inpatient were scoliosis and kyphoscoliosis, esophageal reflux, and hypertrophy of tonsils with adenoids.
Table 5.
Top 10 most prevalent ICD9 diagnosis codes of patients at VUH (adults; n = # of admissions)
| All admissions to VCH | Admissions to VUH with inpatient MHAV use | ||
|---|---|---|---|
| ICD-9 | n | ICD-9 | n |
| 185 - Mal neoplasm prostate | 771 | 998.59 - Other postop infection | 34 |
| 278.01 - Morbid obesity | 759 | 278.01 - Morbid obesity | 25 |
| 998.59 - Other postop infection | 610 | 560.9 - Intestinal obstruction | 21 |
| 189.0 - Mal neoplasm kidney | 464 | 189.0 - Mal neoplasm kidney | 21 |
| 715.36 - Osteoarthrosis lower leg | 433 | 403.9 - Hypertensive chronic kidney disease | 20 |
| 715.35 - Osteoarthrosis pelvis | 254 | 198.3 - Secondary mal neoplasm brain/spinal | 19 |
| 560.9 - Intestinal obstruction | 242 | V55.2 - Attention to ileostomy | 17 |
| 733.82 - Nonunion of fracture | 223 | 715.36 - Osteoarthrosis lower leg | 17 |
| 403.91 - Hypertensive chronic kidney disease | 221 | 562.11 - Diverticulitis of colon | 14 |
| 414.01 - Coronary Atherosclerosis | 194 | 997.49 - Other digestive sys complications | 13 |
Table 6.
Top 10 most prevalent ICD9 diagnosis codes of patients at VCH (children; n = # of admissions)
| All admissions to VCH | Admissions to VUH with inpatient MHAV use | ||
|---|---|---|---|
| ICD-9 | n | ICD-9 | n |
| 750.5 - Hypertrophic pyloric stenosis | 233 | 737.30 - Scoliosis and kyphoscoliosis | 5 |
| 540.9 - Acute appendicitis w/o peritonitis | 224 | 530.81 - Esophageal reflux | 4 |
| 474.10 - Hypertrophy of tonsil w/ adenoids | 145 | 474.10 - Hypertrophy of tonsil w/ adenoids | 4 |
| 737.30 - Scoliosis and kyphoscoliosis | 134 | 276.51 - Dehydration | 4 |
| 540.0 - Acute appendicitis w/ peritonitis | 126 | 996.63 - Complication nervous sys implant | 3 |
| 812.41 - Supracondylar fracture humerus | 109 | 787.22 - Dysphagia oropharyngeal phase | 3 |
| 998.11 - Hemorrhage complicating procedure | 89 | 560.81 - Peritoneal adhesions w/ obstruction | 3 |
| 756.0 - Congenital anomalies of skull/face | 86 | 556.9 - Ulcerative colitis unspecified | 3 |
| 996.2 - Complication nervous sys implant | 85 | 756.19 - Other congenital anomalies spine | 2 |
| 540.1 - Acute appendicitis w/ abscess | 84 | 742.59 - Other cong anomalies spinal cord | 2 |
Discussion
This study documents modest and somewhat unexpected usage of a patient portal by hospitalized surgical patients; it is one of the first studies to report inpatient portal adoption outside of a specific program or technology designed for the hospital setting. Without promotion for use in the inpatient setting, 4% of all admitted surgical patients and 16% of patients registered for the portal utilized the portal while in the hospital. With a known lack of research about technologies to engage patients in the inpatient setting29, this study suggests that existing technologies such as patient portals may have a role in meeting the needs of hospitalized patients and their families.
Our study showed that patient portals were more likely to be used during hospitalization for patients who were white, male, and had extended lengths of stay. Outpatient studies of patient portals have shown similar disparities with decreased use by minorities, especially African Americans.30-32 In contrast to our findings, prior studies suggest that portal use is fairly similar between women and men, with most studies demonstrating slightly higher registration rates and usage by women.31 Of note, we cannot determine from usage logs whether the portal was actually used personally by the patient, or rather another individual using the patient’s login information.
In our study, the services with the most registered portal users included those with significant pre-operative relationships, including gastrointestinal and laparoscopic (including a large majority of bariatric surgery patients) and oncology and endocrine surgery. ICD-9 diagnosis codes for adults registered for the portal aligned with the service designations, with the most common diagnoses being prostate cancer and morbid obesity. Interestingly, the most frequent ICD-9 code of adult patients using the portal while inpatient was post-operative infection, suggesting patients with a complication may be more likely to utilize the portal to view personal health information and contact providers. The only service that showed portal usage increased over that of general surgery in hospitalized patients was liver transplantation, potentially due to frequent laboratory monitoring and clinical complexity of patients.
Prior research has shown encouraging adoption of similar technologies during hospitalization, but usually in the context of a specific research program in which registration was encouraged and usage was supported by training. Wilcox and colleagues piloted a customized inpatient personal health record in cardiothoracic surgery patients and found medication tracking tools to be an effective means to increase inpatient engagement.33 Burke reported enthusiastic adoption of a web-based multimedia EHR for patients with congenital cardiac disease and their parents with a 93% adoption rate and 67% of use occurring during hospitalization.34 Notably, this study was conducted in families with children undergoing surgical repair of congenital cardiac abnormalities, who likely have long-standing relationships with their surgeons. O'Leary and colleagues showed that patient use of a portal designed specifically with inpatient information including team members, medication lists, and daily agendas on tablet computers within a general medical service unit could improve the ability of patients to identify physicians and roles by over 25%.35 In contrast to prior work focused on technologies developed for inpatient setting, our study demonstrated substantial use of a patient portal designed for the outpatient setting, by patients who were hospitalized and their caregivers, without specific encouragement or training, and in the presence of policies that might discourage inpatient use.
There are many potential benefits to using a patient portal during inpatient admissions. First and foremost, even minor surgeries are considered major life events for most patients and families, and they offer “teachable moments” when otherwise unengaged individuals might consider making important healthcare changes.36 Introducing patient portals during hospitalizations may provide tools for patients and families to learn about health problems and engage in their care. Furthermore, hospital team members, including physicians, residents, and nursing staff are highly dynamic,37 and many hospitalized patients are unable to identify their physicians.38, 39 Hospitalized patients frequently have multiple active conditions, tests, and procedures, with acute illness and its associated stress making it difficult for patients and families to retain information provided on daily rounds or at discharge.35, 40-42 Others have shown that patients and caregivers desire access to the daily plan of care and team member roles, often not present in patient portals.43, 44 Patient portals can allow patients to review their health data, schedule and view post-operative appointments, and communicate with providers. In the inpatient setting, hospital staff can provide training and support to assist patients and their families with registration and navigation of portal functions, giving them the knowledge and experience needed to promote ongoing engagement.45 Use and familiarity with the portal prior to discharge may increase the portal usage on an outpatient basis. For example, patients may feel more comfortable communicating problems or concerns post-operatively through secure messaging after using it as an inpatient.
Such changes could have a significant impact on surgical workflow. Some patients who undergo certain operations may not require a face-to-face follow up, and provider-patient messaging could be utilized to ensure the patient is recovering as expected post-operatively. A pilot study at our institution has shown that over three-fourths of patients undergoing elective general surgery procedures were satisfied with online follow up, and post-operative complications were not missed by online visits.46 Portal follow-up can potentially prevent patients from travelling long distances or missing work or school for unnecessary face-to-face clinic visits. This approach also benefits providers as follow-up appointments are typically included within the global payment period.
This study has important limitations. The design is retrospective, and the research was done at single large academic medical center with a locally-developed patient portal. The findings may not apply to other clinical settings or portal implementations, and therefore may not be generalizable to all hospitals. However, our portal functions and many of the MHAV procedures and policies are similar to those reported by others.7 One main difference is that MHAV was broadly deployed across clinical specialties soon after implementation, and our findings represent those of an established portal in use across the clinical enterprise for over 5 years. We have not assessed factors that may contribute to adoption and usage of the portal, such as encouragement by specific providers or teams. Further, we do not know the platform on which the portal was used by patients, the clinical context in which the portal was accessed, or other measures of usability or satisfaction, which would further inform the interpretation of our usage data. These questions are the subject of our ongoing research projects.
Conclusions
This study demonstrates modest use of a patient portal by hospitalized surgical patients without specific encouragement. Disparities in portal adoption among minority patients may occur in the inpatient setting. Although designed for the outpatient setting, patient portals may have a role in meeting consumer health information needs and engaging surgical patients both during and after hospitalizations. The perioperative period may offer a uniquely teachable time in which to engage patients and families in their care, and using a portal during hospitalization could support online postoperative follow up, which can benefit both patients and providers. Additional research is needed to determine the best ways to leverage patient portals during inpatient admissions to improve care.
Acknowledgements
Jamie Robinson and Sharon Davis were supported by the 5T15LM007450-12 training grant from the National Library of Medicine.
References
- 1.Otte-Trojel T, de Bont A, van de Klundert J, Rundall TG. Characteristics of patient portals developed in the context of health information exchanges: Early policy effects of incentives in the meaningful use program in the united states. J Med Internet Res. 2014;16(11):e258. doi: 10.2196/jmir.3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Healthit. Gov. What is a patient portal? [updated 11/2/20152/14/2016]. Available from: http://www.healthit.gov/providers-professionals/faqs/what-patient-portal.
- 3.Patient portal. Https://en.Wikipedia.Org/wiki/patient_portal. Accessed february 29, 2016.
- 4.Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: A systematic review. J Med Internet Res. 2015;17(2):e44. doi: 10.2196/jmir.3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourgeois FC, Mandl KD, Shaw D, Flemming D, Nigrin DJ. Mychildren’s: Integration of a personally controlled health record with a tethered patient portal for a pediatric and adolescent population. AMIA Annu Symp Proc. 2009;2009:65–69. [PMC free article] [PubMed] [Google Scholar]
- 6.Shenson JA, Cronin RM, Davis SE, Chen Q, Jackson GP. Rapid growth in surgeons’ use of secure messaging in a patient portal. Surg Endosc. 2015 doi: 10.1007/s00464-015-4347-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: Evidence on health outcomes, satisfaction, efficiency, and attitudes: A systematic review. Ann Intern Med. 2013;159(10):677–687. doi: 10.7326/0003-4819-159-10-201311190-00006. [DOI] [PubMed] [Google Scholar]
- 8.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 9.2015 edition health information technology (health it) certification criteria, 2015 edition base electronic health record (ehr) definition, and onc health it certification program modifications. Final rule. Fed Regist. 2015;80(200):62601–62759. [PubMed] [Google Scholar]
- 10.Gold M, Hossain M, Mangum A. Consumer engagement in health it: Distinguishing rhetoric from reality. EGEMS (Wash DC) 2015;3(1):1190. doi: 10.13063/2327-9214.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masterson Creber R, Prey J, Ryan B, et al. Engaging hospitalized patients in clinical care: Study protocol for a pragmatic randomized controlled trial. Contemp Clin Trials. 2016;47:165–171. doi: 10.1016/j.cct.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.North F, Crane SJ, Chaudhry R, et al. Impact of patient portal secure messages and electronic visits on adult primary care office visits. Telemed J E Health. 2014;20(3):192–198. doi: 10.1089/tmj.2013.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung C, Padman R, Shevchik G, Paone S. Who are portal users vs. Early e-visit adopters? A preliminary analysis. AMIA Annu Symp Proc. 2011;2011:1070–1079. [PMC free article] [PubMed] [Google Scholar]
- 14.Hanberger L, Ludvigsson J, Nordfeldt S. Use of a web 2.0 portal to improve education and communication in young patients with families: Randomized controlled trial. J Med Internet Res. 2013;15(8):e175. doi: 10.2196/jmir.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cho AH, Arar NH, Edelman DE, Hartwell PH, Oddone EZ, Yancy WS., Jr Do diabetic veterans use the internet? Self-reported usage, skills, and interest in using my healthevet web portal. Telemed J E Health. 2010;16(5):595–602. doi: 10.1089/tmj.2009.0164. [DOI] [PubMed] [Google Scholar]
- 16.de Lusignan S, Mold F, Sheikh A, et al. Patients’ online access to their electronic health records and linked online services: A systematic interpretative review. BMJ Open. 2014;4(9):e006021. doi: 10.1136/bmjopen-2014-006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldzweig CL, Towfigh A, Maglione M, Shekelle PG. Costs and benefits of health information technology: New trends from the literature. Health Aff (Millwood) 2009;28(2):w282–293. doi: 10.1377/hlthaff.28.2.w282. [DOI] [PubMed] [Google Scholar]
- 18.Cronin R, Davis S, Shenson J, Chen Q, Rosenbloom S, Jackson G. Growth of secure messaging through a patient portal as a form of outpatient interaction across clinical specialties. Appl Clin Inform. 2015;6(2):288–304. doi: 10.4338/ACI-2014-12-RA-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das A, Faxvaag A, Svanaes D. The impact of an ehealth portal on health care professionals’ interaction with patients: Qualitative study. J Med Internet Res. 2015;17(11):e267. doi: 10.2196/jmir.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vawdrey DK, Wilcox LG, Collins SA, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428–1435. [PMC free article] [PubMed] [Google Scholar]
- 21.Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD. Tablet computers for hospitalized patients: A pilot study to improve inpatient engagement. J Hosp Med. 2014;9(6):396–399. doi: 10.1002/jhm.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dykes PC, Stade D, Chang F, et al. Participatory design and development of a patient-centered toolkit to engage hospitalized patients and care partners in their plan of care. AMIA Annu Symp Proc. 2014;2014:486–495. [PMC free article] [PubMed] [Google Scholar]
- 23.Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: A preliminary evaluation. J Am Med Inform Assoc. 2016;23(1):80–87. doi: 10.1093/jamia/ocv093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris D, Karlson A. SIGCHI Conference on Human Factors in Computing Systems. Vancouver, BC, Canada: ACM Press; 2011. Dynamic accessibility requirements for hospital patients. [Google Scholar]
- 25.Skeels M, Tan DS. Proceedings of the 1st ACM International Health Informatics Symposium. Arlington, Virginia, USA 1883087: ACM; 2010. Identifying opportunities for inpatient-centric technology; pp. 580–9. [Google Scholar]
- 26.Osborn CY, Rosenbloom ST, Stenner SP, et al. Myhealthatvanderbilt: Policies and procedures governing patient portal functionality. J Am Med Inform Assoc. 2011;18(Suppl 1):i18–23. doi: 10.1136/amiajnl-2011-000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cronin RM, Davis SE, Shenson JA, Chen Q, Rosenbloom ST, Jackson GP. Growth of secure messaging through a patient portal as a form of outpatient interaction across clinical specialties. Appl Clin Inform. 2015;6(2):288–304. doi: 10.4338/ACI-2014-12-RA-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Team RC. R foundation for statistical computing. vienna, austria: 2015. R: A language and environment for statistical computing. Http://www.R-project.Org/ [Google Scholar]
- 29.Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: A systematic review. J Am Med Inform Assoc. 2014;21(4):742–750. doi: 10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18(3):318–321. doi: 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roblin DW, Houston TK, 2nd, Allison JJ, Joski PJ, Becker ER. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc. 2009;16(5):683–689. doi: 10.1197/jamia.M3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gordon NP, Hornbrook MC. Differences in access to and preferences for using patient portals and other ehealth technologies based on race, ethnicity, and age: A database and survey study of seniors in a large health plan. J Med Internet Res. 2016;18(3):e50. doi: 10.2196/jmir.5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilcox L, Woollen J, Prey J, et al. Interactive tools for inpatient medication tracking: A multi-phase study with cardiothoracic surgery patients. J Am Med Inform Assoc. 2016;23(1):144–158. doi: 10.1093/jamia/ocv160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burke RP, Rossi AF, Wilner BR, Hannan RL, Zabinsky JA, White JA. Transforming patient and family access to medical information: Utilisation patterns of a patient-accessible electronic health record. Cardiol Young. 2010;20(5):477–484. doi: 10.1017/S1047951110000363. [DOI] [PubMed] [Google Scholar]
- 35.O'Leary KJ, Lohman ME, Culver E, Killarney A, Randy Smith G, Jr, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc. 2016;23(1):159–165. doi: 10.1093/jamia/ocv058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Warner DO. Surgery as a teachable moment: Lost opportunities to improve public health. Arch Surg. 2009;144(12):1106–1107. doi: 10.1001/archsurg.2009.205. [DOI] [PubMed] [Google Scholar]
- 37.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the united states. N Engl J Med. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199–201. doi: 10.1001/archinternmed.2008.565. [DOI] [PubMed] [Google Scholar]
- 39.Makaryus AN, Friedman EA. Does your patient know your name? An approach to enhancing patients’ awareness of their caretaker’s name. J Healthc Qual. 2005;27(4):53–56. doi: 10.1111/j.1945-1474.2005.tb00568.x. [DOI] [PubMed] [Google Scholar]
- 40.O'Leary KJ, Kulkarni N, Landler MP, et al. Hospitalized patients’ understanding of their plan of care. Mayo Clin Proc. 2010;85(1):47–52. doi: 10.4065/mcp.2009.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83–86. doi: 10.1002/jhm.566. [DOI] [PubMed] [Google Scholar]
- 42.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991–994. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 43.Kendall L, Mishra SR, Pollack A, Aaronson B, Pratt W. Making background work visible: Opportunities to address patient information needs in the hospital. AMIA Annu Symp Proc. 2015;2015:1957–1966. [PMC free article] [PubMed] [Google Scholar]
- 44.Mishra SR, Haldar S, Pollack AH, et al. Not just a receiver: Understanding patient behavior in the hospital environment, in proc 2016 chi conference on human factors in computing systems (chi ‘16) new york, ny, USA: Acm; pp. 3103–3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (pam): Conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kummerow Broman K, Oyefule OO, Phillips SE, et al. Postoperative care using a secure online patient portal: Changing the (inter)face of general surgery. J Am Coll Surg. 2015;221(6):1057–1066. doi: 10.1016/j.jamcollsurg.2015.08.429. [DOI] [PMC free article] [PubMed] [Google Scholar]