Abstract
This study presents a qualitative content analysis of nurses’ satisfaction and issues with current electronic health record (EHR) systems, as reflected in one of the largest international surveys of nursing informatics. Study participants from 45 countries (n=469) ranked their satisfaction with the current state of nursing functionality in EHRs as relatively low. Two-thirds of the participants (n=283) provided disconcerting comments when explaining their low satisfaction rankings. More than one half of the comments identified issues at the system level (e.g., poor system usability; non-integrated systems and poor interoperability; lack of standards; and limited functionality/missing components), followed by user–task issues (e.g., failure of systems to meet nursing clinical needs; non nursing-specific systems) and environment issues (e.g., low prevalence of EHRs; lack of user training). The study results call for the attention of international stakeholders (educators, managers, policy makers) to improve the current issues with EHRs from a nursing perspective.
Introduction
The benefits of converting from paper-based systems to electronic health records (EHRs) are being advocated for in various nations around the globe, leading for a push for healthcare professionals, including nurses, to adopt EHRs. In 2012, the EHR adoption rates were relatively high and those numbers grew in the last few years, for example: Sweden and Germany adoption rate was over 80%, the United States (U.S.) 69%, France 67%, Canada 56%, and Switzerland 41%1.
An increased awareness of the importance of usability and other system issues have accompanied the increased adoption of EHRs by healthcare providers2. A systematic review of empirical studies of EHRs identified the potential benefits of this technology in supporting patient care and clinical documentation3. However, reaping these benefits require addressing challenges related to implementation, adoption, and satisfaction of EHRs. The careful consideration of sociotechnical contexts and links between the clinicians, patients, and technology should be taken into account during the EHR development and implementation processes3. Barriers to EHR adoption included cumbersome system functionalities, lack of interoperability, and hardware issues in a study examining the use of EHR in community settings in the U.S.4. This study highlighted the impact of usability on nurses’ workflow, satisfaction, efficiency, and adoption of the EHR, as well as the importance of considering the interaction between system functionality, usability, and clinician workflow. The far reaching negative effects of poor system usability are exemplified by the call for solutions to poorly designed EHRs by the American Medical Association in 2014. This resulted from physicians’ frustration and dissatisfaction with EHR usability and increasingly negative perceptions of EHRs since 20105. Nurses have expressed similar dissatisfaction with EHRs related to the system’s poor fit with clinical workflow, disruptions to productivity, and negative impacts on nurse-patient communication. In one survey of 13,650 nurses in the U.S. in 2014, 92% expressed dissatisfaction with EHRs, 85% noted that they struggled with continually flawed systems, and 67% reported using workarounds to avoid the unresolved flaws of EHR systems6. Beyond causing frustration and being time-consuming for clinicians7, poor EHR usability may also result in adverse events, medical errors, and other unintended negative consequences. Clearly, the usability of EHRs has important implications for patient safety and quality of care8.
While the impact of EHR implementation on nursing is increasingly recognised, the complexities of how the technology is adopted in clinical nursing practice remains poorly understood9. Nevertheless, nurses are still called upon to be key drivers towards the move from paper-based to electronic systems. Furthermore, nurses’ participation in decision-making, development, and evaluation of EHR development and implementation is being increasingly emphasized9. Although nurses represent approximately one-third of hospital employees and nursing is one of the largest EHR user groups, nurses’ perceptions of EHRs are rarely surveyed and remain largely unknown2. For example, only two out of 346 identified usability studies of healthcare information technology conducted between 2003 to 2009 examined systems use by nurses10. A specific examination of usability issues related to nurses’ use of EHRs is warranted as the usability issues faced by nurses may differ from the issues faced by other healthcare professions11–12.
The International Medical Informatics Association–Nursing Informatics Special Interest Group (IMIA-NISIG) Students Working Group members aimed to fill this gap in health information technology research by conducting an international survey of the state of nursing informatics. Our survey solicited responses from participants from 45 countries on various health informatics topics, one of which was the respondents’ perceptions of the usability of EHR systems. In this paper, we present the results of two survey questions related to respondents’ level of satisfaction with, and comments relating to, the current state of EHRs used by nurses.
Methods
Survey creation and distribution
This study had a cross-sectional survey design with online data collection. The questionnaire was developed based on current nursing informatics literature13–14 that explored current and future trends in nursing informatics. The questionnaire was iteratively developed, revised, and edited by the members of the IMIA-NI students working group. The group also shared the questionnaire with several international nursing informatics experts within the IMIA-NISIG leadership. Experts were defined as individuals with multiple publications that examined general informatics trends. Based on several rounds of expert recommendations, comments, and feedback, the group revised the questionnaire until a final version was developed. The online survey version used Google forms and was pilot-tested to assure its adequate functionality before the international distribution.
The study received a supportive ethical statement (Institutional Review Board exempt approval) from the University of Turku (Finland), where it was coordinated. The questionnaire was translated from English into six languages (Arabic, Korean, Portuguese, Spanish, Mandarin and Swedish). Each translation was conducted by a native speaking nurse with a background in informatics. The translation was validated by at least two other native speaking nursing informatics professionals and revised until the final version for distribution was generated. Responses to the open ended questions collected with the different translated versions of the survey were translated back to English for analysis. The translations were conducted by the nurses who translated the original survey questions and each translated response was validated for accuracy by one or two additional native language speakers fluent in English. Data were collected in August - October 2015.The following inclusion criteria were outlined in the survey invitation: any nurse (or other allied health professional) with experience in nursing informatics either in clinical practice or academia was eligible to participate. These groups were targeted in an effort to obtain a comprehensive overview of current trends in academia, as well as to explore issues with EHRs identified by clinicians. We used snowball sampling strategy to reach as many international respondents as possible. The IMIA-NISIG student working group’s members were invited to collaborate on the study and distribute a cover letter and the links to the survey to their networks. Eighteen students from fourteen countries actively participated in distributing the survey through their professional networks. These included global and local health informatics associations (e.g., IMIA, AMIA, etc.), clinical settings (hospitals and outpatient settings), and academic institutions.
The survey consisted of 24 questions with both structured and open-ended response options. Eight of the questions were focused on demographics (i.e., professional background; highest degree received; clinical or academic position; years of informatics experience; and country and city) and eighteen questions pertained to the current or future state of nursing informatics.
To date, results of two survey questions related to current and future trends in nursing informatics have been presented in two published papers15–16. This paper focuses on the two questions that related to respondents’ satisfaction with the current state of EHRs used by nurses. The two questions were: 1) Are you satisfied with the current state of nursing computerized documentation (in electronic health records) in your country/hospital?; and 2) If you are not satisfied with the current state of nursing computerized documentation (in electronic health records) in your country/hospital, please provide a few reasons. Responses to question one were collected using sliding Likert scale ranging from 1 to 10, where 1 indicated the lowest level of satisfaction and 10 the highest level. Responses to question two were open ended without a text length limitation.
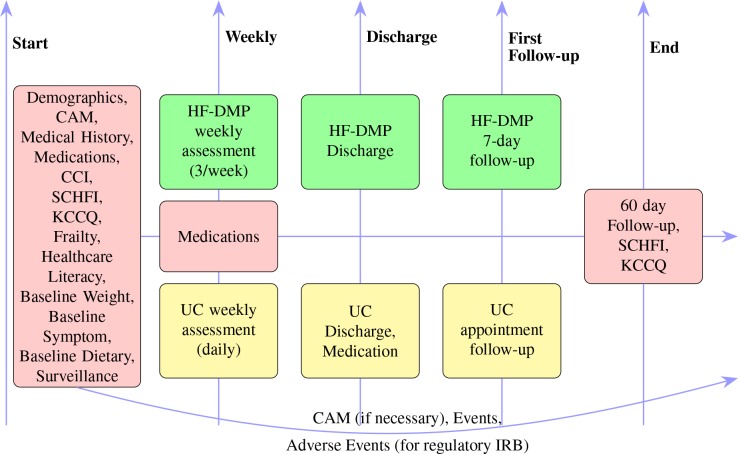
Conceptual framework: A Stratified View of Health Information Technology usability evaluation (SV-HIT) was used as a conceptual framework10 to guide the qualitative analysis in this study. SV-HIT was created as a result of a review of 319 articles that evaluated health information technology used by clinicians. The model has 3 levels, as illustrated in Figure 1.
Figure 1:
A Stratified View of Health Information Technology usability evaluation (SV-HIT),adapted from10.
Level 1- User-Task Issues: Targets system specifications to understand any issues with user–task interactions during the system development. This level focuses on several key questions, including “How can an information technology system be used to support the needs/tasks?” and “What are the user needs?”; Level 2- System Issues: Targets task performance to assess systems and human–computer interaction, user–task–system or system–task interactions. The key questions are: “Does the information system work for the task?” and “What is the quality, speed, accuracy, and completeness of user -system interaction performance?”; Level 3- Environment Issues: Incorporates environmental factors to identify work processes and system impact in a real clinical setting. Key questions include: “What are the organizational, user and other factors affecting system use?” and “How does the system impact healthcare?”
Quantitative analysis: First, the general sample demographic and the professional characteristics were summarized. Then, respondents’ characteristics were compared between those who provided comments on issues with EHR versus those who did not, using standard statistical tests (Chi-square/exact Fisher test or t-test).
Qualitative analysis: Open-ended questions were independently analysed by two authors experienced with qualitative data analysis (CR and MT). Thematic analysis, a qualitative descriptive approach for identifying, analysing and reporting themes within data17, was used to analyse the responses. First, each response was examined independently by the two authors and one or more themes for each response were suggested. Data were collated in an Excel spreadsheet. For example, the response, “The current EHR systems are cumbersome, not intuitive, and require too much clicking,” was classified as related to “Poor usability”. After an initial categorization of all the responses, the authors discussed the themes that emerged and consolidated them into eight major themes and an additional Other category. Each author then went back to the original responses and revised the themes for each of the responses. The themes for each response were then merged and the two authors achieved consensus on the themes for each response17. Finally, each theme was mapped to one of the 3 SV-HIT levels (task- user/ system/ or environmental issues). For example, Poor usability theme was mapped to the System issues level whereas Lack of support at the hospital or policy levels theme was mapped to Environmental issues level. The results were shared with two additional authors for validation. The summary statistics and description of the major themes that emerged are presented in this paper. As illustrated in Figure 1, the three different levels have some degree of overlap. This was evident in our work where some themes that emerged were inter-related. For example, the Limited system functionality theme (System issues level) was related to the Systems failing to meet nursing clinical needs theme (User-task level), and vice versa.
Results
A total of 469 respondents (the sample for this paper) answered the question regarding their satisfaction with EHRs used by nurses. Table 1 presents the sample characteristics. Most of the participants were nurses (89%). The rest were other healthcare professionals, including health informaticians, pharmacists, biomedical engineers, etc. Most of the participants had at least a Master’s degree and more than five years of experience in informatics. Slightly more than one-third (36.2%) of the participants had formal training in informatics. When the question was relevant, most of the participants indicated that they occupied a middle management position or higher and/or held an academic rank of teacher or professor.
Table 1:
Survey participant characteristics
| Category | Total study population (n = 469) | Respondents who commented on issues with EHR (n = 283) | Respondents who did not comment on issues with EHR (n = 186) | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Profession | Nurse Other |
420 (89.6%) 44(9.4%) |
255(90.2%) 27(9.5%) |
165(88.7%) 17(9.1%) |
| Education** | Bachelors Masters PhD Other |
136(29%) 201(43.3%) 111(23.5%) 20(4.3%) |
67(23.5%) 117(41.8%) 88(30.9%) 11(3.9%) |
69(37.1%) 84(45.2%) 23(12.4%) 9(5.4%) |
| Years of nursing informatics experience** | 0-5years 6-10 years 11-15 years 16-20 years 21-45 years |
178(38%) 100(21.3%) 69(14.7%) 54(11.5%) 51(10.9%) |
94(33%) 57(20%) 45(15.8%) 40(14%) 40(14.7%) |
84(45.2%) 43(23.1%) 24(12.9%) 14(7.5%) 11(5.9%) |
| Formal training in informatics* | Yes No Other |
170(36.2%) 267(56.9%) 28(6%) |
105(37.2%) 152(53.7%) 23(8.1%) |
65(34.9%) 115(61.8%) 5(2.7%) |
| Clinical Position (if relevant)** | Staff Middle management Upper management Other |
128(27.3%) 133(28.4%) 55(11.7%) 76(16.2%) |
62(21.8%) 77(27%) 42(15.1%) 56(20%) |
66(35.5%) 56(30.1%) 13(7%) 20(10.8%) |
| Academic Position (if relevant)** | Student Teacher Professor Other |
75(16%) 73(15.6%) 91(19.4%) 58(12.3%) |
36(12.6%) 34(11.9%) 73(26%) 44(15.8%) |
39(21%) 39(21%) 18(9.7%) 14(7.5%) |
| World Health Organization (WHO) regions** | Africa Western Pacific Eastern Mediterranean Europe South-East Asia Americas Region |
3(0.6%) 142(30.3%) 16(3.4%) 59(12.6%) 21(4.5%) 199(42.4%) |
2(0.7%) 61(21.4%) 5(1.8%) 42(14.7%) 10(3.5%) 146(51.6%) |
1(0.5%) 81(43.5%) 11(5.9%) 17(9.1%) 11(6.5%) 53(28.5%) |
| Average satisfaction with nursing EHR** | Mean=4.5 (SD=2.3) |
Mean=3.7 (SD=2.3) | Mean= 5.6 (SD=2.2) |
Indicates p-value levels <.05 in bivariate comparisons (chi-square/exact Fisher test or t-test) of characteristics between participants who commented on the issues with nursing electronic health records vs. those who did not comment.
Indicates p-value levels <.001 in bivariate comparisons (chi-square/exact Fisher test or t-test) of characteristics between participants who commented on the issues with nursing electronic health records vs. those who did not comment.
The respondents’ satisfaction with the current state of EHRs
The average satisfaction with the current state of EHRs used by nurses was 4.5 (SD= 2.3) on a scale from 1 (not at all satisfied) to 10 (very satisfied). Some geographic regions (and countries) were represented by a small number of respondents (e.g. from the African countries or Eastern Mediterranean region). We also conducted an association analysis between the respondents’ levels of EHR satisfaction and background characteristics (e.g., level of education, academic & clinical positions, etc.) but did not identify significant associations, thus, these results are not presented here.
The reported issues with the current state of EHRs used by nurses
Two out of three study participants (n= 283, response rate 60.3%) answered question two and provided comments regarding issues with the current state of EHR used by nurses. Table 1 presents a comparison between participants who provided comments versus those who did not. Participants who responded to question two had significantly (p<.001, t = 9.1, df = 467) lower scores (mean=3.7, SD= 2.3) for satisfaction with the current state of EHR used for nursing than non-respondents (mean=5.6, SD= 2.2). Overall, participants who commented on the issues with EHR had significantly higher levels of education (e.g., 30.9% of those who commented had PhD vs. 12.4% of non respondents); had more years of informatics experience; were more likely to be formally trained in informatics; had higher levels of either clinical or academic positions; and were more likely be from the Europe or the Americas Would Health Organizations (WHO) regions, and not the Western Pacific region.
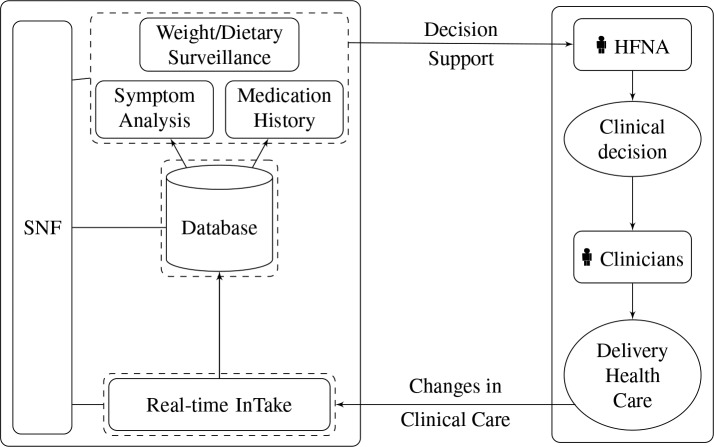
Nine themes were identified in the answers to question two, and each response was mapped to an average of two themes. Each theme was mapped to one of the SV-HIT levels. Overall, 562 concerns were identified in the 283 comments. The most commonly reported concerns were associated with system issues (54.5%), followed by user–task issues (27.5%) and environment issues (18%). Figure 2 presents the distribution of the concerns by SV-HIT levels and Table 2 presents the summary of concern levels, themes and examples of participant quotes.
Figure 2:
Distribution of concerns reported about nursing electronic health records by level*
* Percentage of issues reflect the individual concern level out of total concerns reported, e.g., 127 user-task issues/ 562 total concerns = 27.5%.
Table 2:
Survey comments distribution by level and theme with example quotes.
| Level | Theme | Number of comments (% out of total comments)* | Example quotes |
|---|---|---|---|
| USER-TASK ISSUES | Systems fail to meet nursing clinical needs | 81 (28.6) | “The development of nursing information system is not based on nursing needs [China]”; “Hard to tell the patient story [U.S.]”; “Continuing invisibility of nursing’s contribution to outcomes [U.S.]”; “Currently doesn’t feel like it enhances live patient care [Australia].” |
| Systems are not nursing specific | 46 (16.3) | “Nursing documentation is driven by accreditation & regulatory needs rather than by what actually makes a difference to the patients/families/populations [U.S.]”; “[Systems] Need more focus on nursing care (processes, measurable tasks, outcomes associated with nursing Interventions) - needs to be more intuitive to nursing knowledge [U.S.]”; “Systems do not adequately reflect nursing practice, especially the critical thinking and the processing of data and information to knowledge [U.S.].” | |
| SYSTEM ISSUES | Poor system usability | 88 (31.1) | “Poor interface design [Taiwan]”; “Very time consuming and duplicative[Finland]”; “Documentation can be hard to find. Especially in non discrete data driven areas of the hospital- like behavioral health, social services, physical and speech therapies [U.S.]”; “Too many keystrokes, and nuisance alerts [U.S.].” |
| Non- integrated systems and poor interoperability | 67 (23.7) | “[Systems are] Scattered, hard to integrate [China]”; “For care coordination and achievement of the Triple Aim, Need more Health Information Exchanges between community - acute - primary care [U.S.]”; “Lack of interoperability with other systems [U.S.].” | |
| Lack of standards & standardization | 39 (13.8) | “There is very little to no standardization on documentation to facilitate information management and retrieval [Philippines]”; “Little, if any, implementation or use of standardized terms outside of physician practice (CPT or ICD-9/ICD-10) [U.S.]”; “Little comparison of the effect of clinical practice on patient outcomes - no clear way to compare since there is no standardization of terms[Philippines]”; “A great deal of information is not standardized without standard terminologies [U.S.].” | |
| Limited functionality/missing components | 58 (20.5) | “Missing process support and a long list of small details, missing functionality for check lists [Sweden]”; “Care Management options are limited [U.S.]”; “Pediatric content is limited in both Home Health and Hospital systems and must be created [U.S.].” | |
| ENVIROMENT ISSUES | Low prevalence of EHR systems | 30 (10.6) | “Unfortunately 95% nursing records are manual records [Venezuela]”; “Few electronic records are being used [South Africa]”; “Still using paper based systems for nursing documentation with minimal electronic records [Australia].” |
| Lack of user’s training | 21 (7.4) | “Users don’t know how to use the system [U.S.]”; “Need more awareness and inservice training for Indian Nurses [India]”; “Only very few professionals are qualified or trained to practice computerized documentation [Philippines].” | |
| Other | 32 (11.3) | “Lack of participation from clinical staffs in system development [Taiwan]”; “I know nothing about how nursing EHR is created because it is controlled by our vendor [U.S.]”; “No support from the authorities [Argentina]”; “Poor understanding of the implementation of computerized documentation in nursing, both by managers as the professionals themselves [Brazil].” | |
| Total comments | 283 |
Number of comments refers to the proportion of comments reported by individual respondents, e.g., 81 comments about systems that fail to meet nursing clinical needs/ 283 comments total= 28.3%.
User-task issues
Systems fail to meet nursing clinical needs: Almost one-third of the respondents (28.6%) indicated that the systems did not meet their clinical needs. One common concern was the inability of the information systems to capture the patient story in either a narrative or structured format. An example comment was, “Too cookie cutter, does not allow for a narrative format, and does not capture the patient story [U.S.]”. Several respondents suggested that further work is needed to improve the utility of the EHR for clinical nursing. For example, “We need to develop better tools that are patient centered and tell the patient story in ways that are easy and intuitive for healthcare providers to use [U.S.]”. In addition, many respondents felt that the users of the systems perceive few benefits because electronic systems do not promote patient care. They are instead viewed as data repositories. For example, participants indicated that, “Currently it doesn’t feel like the system enhances live patient care, [Australia]” or “Large volumes of documentation lack correlation with impact on outcomes [U.S.]”. Further comments suggested little value of the collected data. For example, “Data not valuable for frontline nurses who do the documentation [U.S.]”.
Systems are not nursing specific: Several respondents (16.3%) suggested that information systems do not work well for capturing, storing, and presenting nursing knowledge. Respondents indicated that some of the electronic systems were developed for billing or regulatory reporting needs, thus their usefulness for nursing is limited. For example, respondents suggested that, “Nursing documentation is driven by accreditation & regulatory needs rather than by what actually makes a difference to the patients/families/populations [U.S.]” and “The development of nursing information system is not based on nursing needs, but for the management of hospital expenses [China]”.
Overall, many respondents felt that the current information systems are not capable of reflecting and supporting key aspects of nursing practice. For example, “Systems do not adequately reflect nursing practice, especially the critical thinking and the processing of data and information to knowledge [U.S.]”. In addition, respondents reported that nursing clinical decision support tools were very uncommon. The respondents indicated that, “Current system does not include decision support that is valuable to nurses [U.S.]”.
System issues
Poor system usability: Usability is defined as how easy it is for users to accurately and efficiently accomplish a task while using a system18. In our survey, system usability was the most reported concern with almost one-third of the respondents (31.1%) identifying multiple usability issues. The existing systems were referred to as time-consuming and slow, requiring too many key strokes to record simple information, and presenting multiple unnecessary screens that interrupt clinical thinking. Multiple respondents experienced issues with poor interface design and challenges with identifying and working with interdisciplinary documentation. Other respondents expressed that documentation is a burden and is often duplicative and hard to track chronologically. Some of the responses included, “The system is not friendly, need to open multiple screens to record information, very slow, and impractical [Brazil]” and “Time consuming, duplicate documentation, lack of discrete data, poor design, too many keystrokes, and nuisance alerts [U.S.]”.
Non-integrated systems and poor interoperability: About a quarter (23.7%) of the respondents indicated that either the systems, or the data that is collected in them, is not integrated with clinical workflows. Some of the common concerns included issues with multiple systems that were difficult to integrate. For example, “Many ‘silos’ and standalone solutions [Sweden]”, “Absence of integrated clinical database [Argentina]” and “Information is spread across many different systems [Belgium]”. One respondent noted that because they use multiple systems in their clinical practice, “Same information is documented in different areas so one ends up double, triple, and even quadruple documenting the same information [U.S.]”.
Lack of interoperability was an additional major concern for survey respondents. Many participants indicated that they require more connected systems to be able to see the patient data across care continuum and collaborate with other professions. For example, “The current systems are not sharing the pertinent information across care areas, such as homecare and acute care, there is also no sharing of information across provinces [Canada]”. Respondents felt that lack of information sharing prevents them from achieving optimal outcomes for their patients. For example, “For care coordination and achievement of the Triple Aim, need more health information exchanges between community - acute - primary care [U.S.]”.
Lack of standards & standardization: Another area of concern reported by some respondents (13.8%) was the lack of use of documentation standards and insufficient system standardization. Several respondents wished to see nursing terminologies implemented to standardize documentation and care quality assessments. For example, “Little comparison of the effect of clinical practice on patient outcomes - no clear way to compare since there is no standardization of terms, [Philippines]” and “Nursing needs to go further and use standardized languages to measure the effectiveness of interventions [Brazil]”. Several nursing terminologies were suggested to resolve the existing issues, such as the International Classification for Nursing Practice (ICNP®). Also, there were a few suggestions regarding the development of guidelines to promote interoperability and system standardization.
Limited functionality/missing components: About one-fifth of the respondents (20.5%) reported that their EHRs lacked at least one key functionality. For example, some suggested that there is not enough coverage for specific content areas, such as pediatric nursing, homecare, or care management. Some other missing areas, mentioned earlier in the paper, included a lack of nursing clinical decision support and inability to re-use nursing data that was already collected for epidemiology and other applied clinical or research processes.
Environment issues
Low prevalence of EHR systems: One-tenth of the respondents (10.6%) indicated that their environments (countries, or a specific health setting) did not implement EHRs comprehensively. For example, “Unfortunately 95% of nursing records are manual records [Venezuela]”; “Few electronic records are being used [South Africa]”; and “Still using paper based systems for nursing documentation with minimal electronic records [Australia]”. Other respondents indicated that their settings, such as homecare, do not have EHRs. A few respondents commented on the differences between regions within countries. For example, “Nursing EHR are only utilized in tertiary private hospitals. Public hospitals in most of the country, especially in provinces, still use paper documentation [Philippines]”.
Lack of users training: Some respondents (7.4%) identified that insufficient user training prevents full use of EHR system capabilities. A few respondents believed that the generation gap between younger and older nurses requires different levels of training.
Other: Less frequent issues raised by the respondents were grouped as Other. One of the prevalent themes in this category was the lack of EHR support at organizational or policy level. For example, “Policy makers don’t even realize EHR importance so no one is taking any initiatives in this regard [Pakistan]” and “Nursing Councils should motivate Indian Nurses in using EHR [India]”. Others observed a lack of centralized initiatives regarding EHR adoption and/or development. For example, “No national policy to encourage hospitals to develop electronic nursing records [Taiwan]”. Another theme was the lack of user input into system development or refinement. For example, “I know nothing about how nursing EHR is created because it is controlled by our vendor [U.S.]”.
Discussion
Respondents assigned relatively low rankings regarding their satisfaction with the current state of EHRs used by nurses. Two thirds of the respondents specified their concerns with the current systems in their responses to the open ended question. Participants who provided comments to question number two, had lower EHR satisfaction scores, higher levels of education, more years of informatics experience, had higher level professional positions (in clinical practice and academia) and were more likely be from Europe or the Americas WHO regions than participants who did not provide comments. It is possible that more experienced and more educated participants were more likely to respond since they have experienced more EHR issues during their careers.
The literature review identified only a few studies that focused on evaluation of nurses’ use of HIT, and these studies tended to focus on one particular system domain such as usability19–20. Other interdisciplinary studies, mostly focused on medicine, identified similar trends with user perceptions of EHRs21–22. This study revealed low user satisfaction with EHRs that nurses use. More than half of the concerns were at the system issues level of the SV-HIT model, followed by user-task issues and environment issues. These results warrant further examination and potentially, are a call for the attention of international stakeholders (educators, managers, policy makers) to begin to improve the current issues with EHRs used by nurses. In practice, addressing system issues will rely on organizational supports to include end-users in the process of design, purchase, upgrade, and implementation decisions.
Specific user-task issues were identified that affected the ability of information system to support the nurse’s work. First, respondents reported that systems fail to meet nursing clinical needs, such as telling the patient story. The lack of EHRs’ ability to tell the patient story is an emerging concern in the healthcare literature regarding system usability23. Respondents also suggested that neither strict structured formats (e.g., check-lists) nor free text documentation (e.g., narrative descriptions) help with clinical decision making. Rather, they hinder a comprehensive understanding of the impact of nursing on patient outcomes. This finding reflects a long-standing discussion regarding how much of the documentation in EHRs should be structured when compared to free text24. One possible solution to this is using automated extraction of important data from free text using natural language processing25. More research on the best balance between narrative and structured documentation to meet nursing clinical needs is needed. Another concerning theme was that EHRs are not nursing specific. Respondents felt that systems were developed either for other disciplines (e.g., medicine) or to meet billing and/or regulatory requirements. Although some literature exists on creating nursing-specific EHRs24, more research and practical recommendations are critically needed.
System issues were the most reported concern about the current EHR systems. In congruence with other studies on the topic 21, 22, 27, 28 survey respondents believed that EHR systems suffer from poor usability, e.g., systems are time-consuming, slow, require too many key-strokes and overall burdensome. The survey results also confirmed the well-documented lack of systems interoperability29 and the absence of adoption of nursing terminologies30. Systems lacked key functionality for nursing, with the largest concern being nursing clinical decision support systems. Although some examples of successfully developed and implemented nursing clinical decision support systems exist31, our findings call for more development and application of these systems in clinical practice.
Respondents, mostly from developing countries, indicated that they only have few EHR systems in place. As the trend of EHR adoption increases internationally, driven by local legislations and other reasons, we expect this to change sometime in the next decade. Other environmental level issues included insufficient user training and a lack of EHR implementation support by management and/or policy makers. These issues are also supported by other U.S. and international studies30. In general, there is a need to educate nursing students, practicing nurses, faculty, nurse executives, and the inter-professional care disciplines on key aspects of nursing informatics. There are some existing approaches to increase education and awareness that can help address this issue32–33.
Limitations: Our study has several limitations. First, the generalizability of our survey results is limited due to small number of respondents from certain countries/geographic regions (e.g. from the African countries or Eastern Mediterranean region) and an overrepresentation of nurses with higher professional positions/ academic degrees who answered the open ended question (question two). The snowball sampling approach was also limited by the reach of our respective networks and only reached certain organizations and practitioners while others were not included. Our respondents were informaticians and thus were more likely to identify system concerns compared to nurses without an informatics specialization. Further, only a fraction of the survey respondents identified specific issues, such as a lack of documentation standards (13.8%); it is possible that the remainder of participants may have been satisfied with the state of standard terminologies in their EHRs. Finally, respondents who answered the open ended question had a lower mean EHR satisfaction score and were mostly from Europe and North and South America, with fewer responses from Asia and Pacific regions. Learning from these limitations, we are currently planning a follow-up study to explore EHR-related international concerns in more detail.
Conclusions
This study focused on nurses’ satisfaction and issues with EHRs. It is one of the largest studies of international trends in nursing informatics. Respondents from 45 countries ranked their satisfaction with the current state of EHRs relatively low. Two-thirds of more educated and more experienced study participants, mostly from the Europe or the Americas WHO regions, provided disconcerting comments explaining their low EHR rankings. More than one-half of the comments identified issues at the system level (e.g., poor system usability; lack of integrated systems and poor interoperability; lack of standards & standardization; and limited functionality/missing components), followed by user -task issues (e.g., systems fail to meet nursing clinical needs; and systems are not nursing specific) and environment issues (e.g., low prevalence of EHR systems; and lack of user’s training). Although the study sampling and analytical approaches have limitations, the results call for the attention of international stakeholders (educators, managers, policy makers) to begin to improve the current issues with EHRs used by nurses.
References
- 1.Schoen C, Osborn R, Squires D, Doty M, Rasmussen P, Pierson R, et al. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Affairs. 2012;31(12):2805–16. doi: 10.1377/hlthaff.2012.0884. [DOI] [PubMed] [Google Scholar]
- 2.Cho I, Kim E, Choi WH, Staggers N. Comparing Usability Testing Outcomes and Functions of Six Electronic Nursing Record Systems. International Journal of Medical Informatics. 2016 doi: 10.1016/j.ijmedinf.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: An evaluation of information system impact and contingency factors. International Journal of Medical Informatics. 2014;83(11):779–96. doi: 10.1016/j.ijmedinf.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 4.Sockolow PS, Liao C, Chittams JL, Bowles KH. Evaluating the Impact of Electronic Health Records on Nurse Clinical Process at Two Community Health Sites 2012; Proceedings of the 11th International Congress on Nursing Informatics; 2012. p. 381. [PMC free article] [PubMed] [Google Scholar]
- 5.AMA calls for design overhaul of electronic health records to improve usability [press release] 2014 Sep;:16. [Google Scholar]
- 6.Black Book Market Research LLC. Hospital Nurses Forced to Develop Creative Workarounds to Deal with HER System Flaws; Outdated Technologies and Lack of Interoperability. Reveals Black Book [press release] 2014 Oct 17; [Google Scholar]
- 7.Alexander G, Staggers N. A Systematic Review on the Designs of Clinical Technology: Findings and Recommendations for Future Research. ANS Advances in nursing science. 2009;32(3):252–79. doi: 10.1097/ANS.0b013e3181b0d737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metzger J, Welebob E, Bates DW, Lipsitz S, Classen DC. Mixed results in the safety performance of computerized physician order entry. Health Affairs. 2010;29(4):655–63. doi: 10.1377/hlthaff.2010.0160. [DOI] [PubMed] [Google Scholar]
- 9.Rojas CL, Seckman CA. The informatics nurse specialist role in electronic health record usability evaluation. Computers Informatics Nursing. 2014;32(5):214–20. doi: 10.1097/CIN.0000000000000042. [DOI] [PubMed] [Google Scholar]
- 10.Yen P-Y, Bakken S. Review of health information technology usability study methodologies. Journal of the American Medical Informatics Association. 2012;19(3):413–22. doi: 10.1136/amiajnl-2010-000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers ML, Sockolow PS, Bowles KH, Hand KE, George J. Use of a human factors approach to uncover informatics needs of nurses in documentation of care. International journal of medical informatics. 2013;82(11):1068–74. doi: 10.1016/j.ijmedinf.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 12.Drew BJ, Harris P, Zègre-Hemsey JK, Mammone T, Schindler D, Salas-Boni R, et al. Insights into the Problem of Alarm Fatigue with Physiologic Monitor Devices: A Comprehensive Observational Study of Consecutive Intensive Care Unit Patients. PLoS ONE. 2014;9(10):e110274. doi: 10.1371/journal.pone.0110274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saba VK, McCormick KA. Essentials of Nursing Informatics. 6th. McGraw-Hill Medical; 2015. [Google Scholar]
- 14.Topaz M, Ronquillo C, Pruinelli L, Ramos R, Peltonen L-M, Siirala E, et al. Central Trends in Nursing Informatics: Students’ Reflections From International Congress on Nursing Informatics 2014 (Taipei, Taiwan) 3. Vol. 33. CIN: Computers, Informatics, Nursing; 2015. pp. 85–9. [DOI] [PubMed] [Google Scholar]
- 15.Topaz M, Ronquillo C, Peltonen LM, Pruinelli L, Sarmiento RF, Badger MK, et al. Advancing Nursing Informatics in the Next Decade: Recommendations from an International Survey. Stud Health Technol Inform. 2016;(225):123–7. [PubMed] [Google Scholar]
- 16.Peltonen LM, Alhuwail D, Ali S, Badger MK, Eler GJ, Georgsson M, et al. Current Trends in Nursing Informatics: Results of an International Survey. Stud Health Technol Inform. 2016;(225):938–9. [PubMed] [Google Scholar]
- 17.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing & health sciences. 2013;15(3):398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 18.Johnson C, Johnston D, Crowle P. EHR usability toolkit: A background report on usability and electronic health records. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 19.Cho I, Kim E, Choi WH, Staggers N. Comparing Usability Testing Outcomes and Functions of Six Electronic Nursing Record Systems. International Journal of Medical Informatics. 2016 doi: 10.1016/j.ijmedinf.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Viitanen J, Kuusisto A, Nykanen P. Usability of electronic nursing record systems: definition and results from an evaluation study in Finland. Stud Health Technol Inform. 2011;164:333–8. [PubMed] [Google Scholar]
- 21.Darmon D, Sauvant R, Staccini P, Letrilliart L. Which functionalities are available in the electronic health record systems used by French general practitioners? An assessment study of 15 systems. Int J Med Inform. 2014;83(1):37–46. doi: 10.1016/j.ijmedinf.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Raglan GB, Margolis B, Paulus RA, Schulkin J. Electronic Health Record Adoption among Obstetrician/Gynecologists in the United States: Physician Practices and Satisfaction. Journal for healthcare quality: official publication of the National Association for Healthcare Quality. 2015 doi: 10.1111/jhq.12072. [DOI] [PubMed] [Google Scholar]
- 23.Varpio L, Rashotte J, Day K, King J, Kuziemsky C, Parush A. The EHR and building the patient’s story: A qualitative investigation of how EHR use obstructs a vital clinical activity. Int J Med Inform. 2015;84(12):1019–28. doi: 10.1016/j.ijmedinf.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Walsh SH. The clinician’s perspective on electronic health records and how they can affect patient care. Bmj. 2004;328(7449):1184–7. doi: 10.1136/bmj.328.7449.1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demner-Fushman D, Chapman WW, McDonald CJ. What can natural language processing do for clinical decision support? J Biomed Inform. 2009;42(5):760–72. doi: 10.1016/j.jbi.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hovenga E, Garde S, Heard S. Nursing constraint models for electronic health records: a vision for domain knowledge governance. Int J Med Inform. 2005;74(11-12):886–98. doi: 10.1016/j.ijmedinf.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 27.Viitanen J, Hypponen H, Laaveri T, Vanska J, Reponen J, Winblad I. National questionnaire study on clinical ICT systems proofs: physicians suffer from poor usability. Int J Med Inform. 2011;80(10):708–25. doi: 10.1016/j.ijmedinf.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 28.Ratwani RM, Fairbanks RJ, Hettinger AZ, Benda NC. Electronic health record usability: analysis of the user-centered design processes of eleven electronic health record vendors. Journal of the American Medical Informatics Association: JAMIA. 2015;22(6):1179–82. doi: 10.1093/jamia/ocv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sittig DF, Wright A. What makes an EHR “open” or interoperable? Journal of the American Medical Informatics Association. 2015;22(5):1099–101. doi: 10.1093/jamia/ocv060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keenan GM. Big Data in Health Care: An Urgent Mandate to CHANGE Nursing EHRs! On-line journal of nursing informatics. 2014;18(1) [PMC free article] [PubMed] [Google Scholar]
- 31.Bowles KH, Chittams J, Heil E, Topaz M, Rickard K, Bhasker M, et al. Successful electronic implementation of discharge referral decision support has a positive impact on 30- and 60-day readmissions. Res Nurs Health. 2015;38(2):102–14. doi: 10.1002/nur.21643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Topaz M, Rao A, Masterson Creber R, Bowles KH. Educating clinicians on new elements incorporated into the electronic health record: theories, evidence, and one educational project. Computers, informatics, nursing CIN. 2013;31(8):375–9. doi: 10.1097/NXN.0b013e318295e5a5. quiz 80-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goveia J, Van Stiphout F, Cheung Z, Kamta B, Keijsers C, Valk G, et al. Educational interventions to improve the meaningful use of Electronic Health Records: a review of the literature: BEME Guide No. 29. Med Teach. 2013;35(11):e1551–60. doi: 10.3109/0142159X.2013.806984. [DOI] [PubMed] [Google Scholar]