Abstract
Background: Psychosocial distress among patients with limited life expectancy influences treatment decisions, treatment adherence, and physical health. Veterans may be at elevated risk of psychosocial distress at the end of life, and understanding their mental healthcare needs may help identify hospitalized patients to whom psychiatric services should be targeted.
Objective: To examine mental illness prevalence and mental health treatment rates among a national sample of hospitalized veterans with serious physical illnesses.
Design, Subjects, and Measurements: This was a retrospective study of 11,286 veterans hospitalized in a Veterans Health Administration acute care facility in fiscal year 2011 with diagnoses of advanced cancer, congestive heart failure, chronic obstructive pulmonary disease, and/or advanced HIV/AIDS. Prevalent and incident mental illness diagnoses during and before hospitalization and rates of psychotherapy and psychotropic use among patients with incident depression and anxiety were measured.
Results: At least one-quarter of the patients in our sample had a mental illness or substance use disorder. The most common diagnoses at hospitalization were depression (11.4%), followed by alcohol abuse or dependence (5.5%), and post-traumatic stress disorder (4.9%). Of the 831 patients with incident past-year depression and 258 with incident past-year anxiety, nearly two-thirds received at least some psychotherapy or guideline-concordant medication within 90 days of diagnosis. Of 191 patients with incident depression and 47 with incident anxiety at time of hospitalization, fewer than half received mental healthcare before discharge.
Conclusions: Many veterans hospitalized with serious physical illnesses have comorbid mental illnesses and may benefit from depression and anxiety treatment.
Keywords: : depression, hospitalized, mental health, veterans
Introduction
Addressing psychological distress among patients with chronic physical illnesses is particularly important in the context of life-limiting physical illnesses. Among patients with limited life expectancy, there are unique psychosocial issues related to the impact of mental illnesses on treatment decisions, treatment adherence, worsened physical health status, and increased healthcare use.1–4 However, there is concern that these psychosocial issues are not being adequately addressed. Reported depression in the last year of life has increased by over 25% since 1998,5 with nearly half of decedents in a nationally representative sample reported to have “unmet need for anxiety and/or sadness” in the last month of life.6
Veterans with serious, life-limiting physical illnesses may be at especially high risk for psychosocial distress.7 Caregivers of veterans report that patients experienced emotional distress near the end of life 1.5 times more often than caregivers of nonveterans.8 Among veterans with serious physical illnesses, small regional studies suggest there are unmet needs for mental healthcare,9,10 but to our knowledge, no nationwide examination of the degree to which seriously physically ill veterans experience mental illness and receive mental healthcare treatment has been performed. Understanding prevalence and incidence of mental disorders across a variety of serious physical illnesses is a crucial first step toward ensuring that mental healthcare resources are targeted to the patients who need them most.
In this study, we present patterns of mental illness and mental healthcare among veterans hospitalized for advanced cancer, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), or HIV/AIDS. We focus on treatment of depression and anxiety, the most common mental illnesses encountered in our sample; treatment of symptoms of these disorders is a marker of high-quality comprehensive care for seriously physically ill adults.11,12
Methods
Sample
Our sample includes 11,286 veterans who were admitted to a VA hospital in fiscal year (FY) 2011. All veterans with one or more of the following diagnoses during the index hospitalization were initially included in the sample: advanced cancer (metastatic solid tumor, central nervous system malignancies, metastatic melanoma, locally advanced head and neck cancer, locally advanced pancreatic cancer; n = 2432, 21.6%), COPD (n = 5825, 51.6%), CHF (n = 4559, 40.4%), and/or advanced HIV/AIDS with comorbid cancer, cachexia, or cirrhosis (n = 104, 0.9%) (see Supplementary Appendix for ICD-9 codes available online at www.liebertpub.com/jpm). These diagnoses were selected to identify patients with potentially limited life expectancy.13 To ensure a similar intensity of prior VA encounters in which a mental illness could have been detected, all patients in our sample had at least one ICU admission in the year before the index hospitalization or two or more hospitalizations in a six-month period in the year before the index hospitalization. Patients with dementia or delirium diagnoses during the index hospitalization were excluded. Index hospitalizations had to last at least 48 hours and could not be primarily for chemotherapy or acute psychiatric care. We used data from the VA Medical SAS Inpatient and Outpatient Datasets, Decision Support System National Data Extracts, and Vital Status Files. This study was approved by the James J Peters VA Medical Center Institutional Review Board.
Measures
Prevalence of depression and anxiety
We identified prevalence of depression and anxiety during the hospitalization, in the year before hospitalization, and in the period spanning five years to one year before hospitalization. Depression was identified by at least one inpatient diagnosis code, one primary outpatient code, or two secondary outpatient codes on different dates.14 Similar criteria were used to identify anxiety disorders (see Supplementary Appendix for ICD-9 codes).
Incidence of depression and anxiety
Following previous VA studies, depression and anxiety, if present, were counted as incident if there were no depression or anxiety diagnosis codes or prescriptions for antidepressants or anxiolytics in the previous 120 days.14,15 Incident diagnoses were measured during the hospitalization and in the year before hospitalization.
Prevalence of other mental illness and substance use diagnoses at index hospitalization
We identified prevalence of other mental illnesses or substance use disorders at the index hospitalization with an inpatient diagnosis code. Alcohol abuse/dependence, drug (excluding tobacco) abuse/dependence, schizophrenia spectrum disorder, bipolar disorder, other psychosis or delusion, and adjustment disorder at the index hospitalization were identified.
Treatment for incident depression or anxiety
Guidelines for incident depression and anxiety generally call for either psychotherapy or an appropriate psychotropic medication to be provided soon after diagnosis.16,17 We examined receipt of psychotropic medication or psychotherapy within the 90 days after an incident depression or anxiety diagnosis in the year before hospitalization18 (or between diagnosis and index hospitalization, whichever time period was shorter). Medications were counted for depression if they were listed in the VA/Department of Defense (DoD) clinical practice guidelines for major depressive disorder.16 Medications were counted for anxiety if they were listed in general anxiety care guidelines19,20 or VA/DoD post-traumatic stress disorder (PTSD) guidelines.17 For incident depression/anxiety identified during the index hospitalization, we defined treatment as psychotherapy or psychotropic medications provided before discharge.
Analyses
We calculated descriptive statistics of rates of prevalent and incident mental illnesses and rates of psychotherapy and psychotropic medication use. We used chi-square tests to determine whether mental illness prevalence or rates of mental healthcare differed significantly by the presence or absence of each physical comorbidity. Analyses were completed with Stata 14.21
Results
Sample characteristics
The mean age of patients in our sample was 68 (SD = 10). The sample was primarily male (245 [2.2%] of patients were female) and white (8466 patients [75%] were white, 2140 [19%] were black, and 680 [6.0%] were other race). The mean length of stay was 8 days (SD = 11 days), and 510 patients (4.5%) died during the index hospitalization.
Prevalence of mental illness or substance abuse diagnoses at index hospitalization
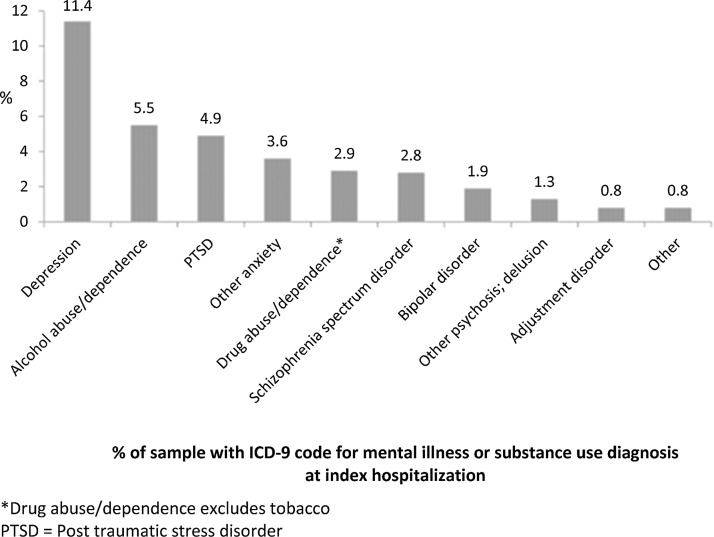
One-quarter (27%) of the sample had at least one mental illness or substance abuse diagnosis recorded during the hospitalization. Depression was the most common diagnosis (11.4%), followed by alcohol abuse or dependence (5.5%), PTSD (4.9%), and other anxiety disorder (3.6%, includes generalized anxiety disorder [GAD], panic, social phobia, obsessive compulsive disorder, and acute stress) (Fig. 1).
FIG. 1.
One-quarter (27.4%) of the sample (veterans hospitalized with advanced cancer, heart failure, COPD, and/or HIV/AIDS) had one or more mental illness or substance use diagnoses during the index hospitalization.
Differences in mental illness prevalence and incidence by physical illness
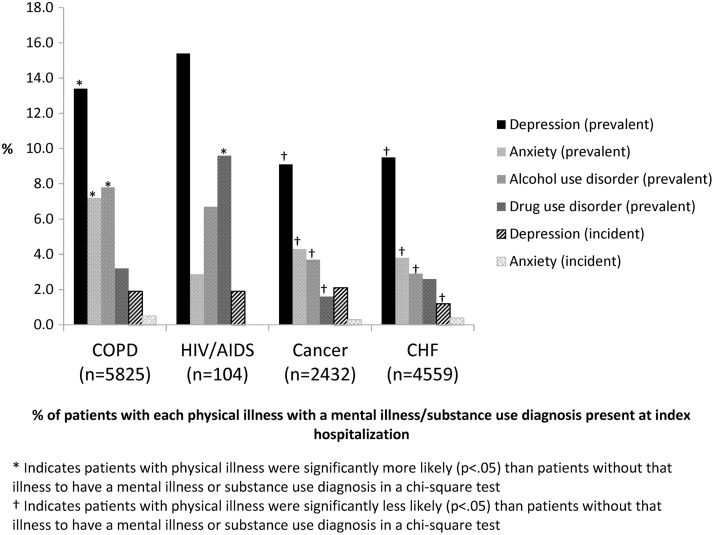
We examined whether there were differences in frequencies of depression, anxiety, and substance use disorders by physical illness. Patients with COPD had higher frequencies of mental illness and substance abuse diagnoses during the index hospitalization than patients without these illnesses (Fig. 2). Depression was observed among 13.4% of patients with COPD and 9.3% of patients without COPD (p < 0.001). Patients with COPD were more than twice as likely as patients without COPD to have an alcohol use disorder (7.8% vs. 3.1%, p < 0.001). Patients with HIV/AIDS were more than three times as likely as patients without HIV/AIDS to have a drug use disorder recorded (9.6% vs. 2.8%. p < 0.001).
FIG. 2.
COPD associated with higher frequencies of prevalent depression, anxiety, and substance use diagnoses. COPD, chronic obstructive pulmonary disease.
Prevalence and incidence of depression and anxiety before hospitalization
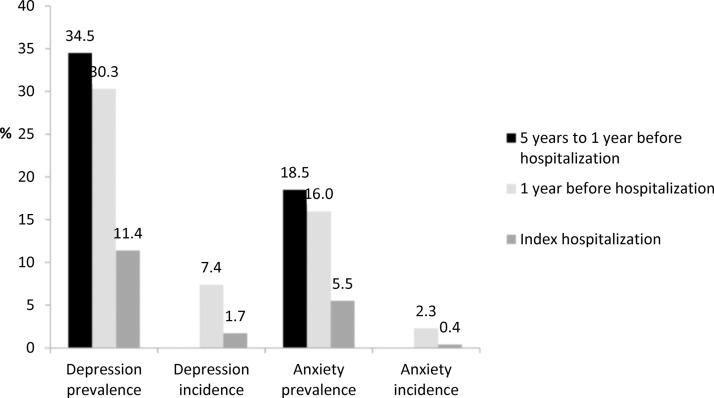
The prevalence of depression and anxiety in the year before hospitalization was more than double what was recorded during the index hospitalization (Fig. 3), suggesting that the percentages in Figures 1 and 2 are conservative estimates. Nearly one-third (30.3%) of seriously physically ill veterans in our sample had a diagnosis of depression in the year before hospitalization, and more than one-third (34.5%) had a diagnosis of depression between five years and one year before hospitalization. A substantial minority of patients received incident diagnoses of depression (7.4%) in the year before hospitalization.
FIG. 3.
Percentage of patients with incident and prevalent depression and anxiety during the index hospitalization and the five years before hospitalization.
Receipt of any mental healthcare for incident depression and anxiety
Nearly two-thirds of patients with incident past-year anxiety (64%) or depression (60%) received at least some psychotherapy or guideline-concordant medication (Table 1). Among patients with incident depression or anxiety at the index hospitalization, fewer than half received mental healthcare before discharge (39% of patients with depression and 23% of patients with anxiety). Among patients with incident depression at the index hospitalization, patients with advanced cancer were more likely to receive mental healthcare than patients without advanced cancer (51.0% vs. 34.3%, p = 0.04). There were no other significant differences by physical comorbidity in receipt of mental healthcare for incident diagnoses during the index hospitalization.
Table 1.
Frequencies of Any Mental Healthcare among Patients with Incident Depression or Anxiety During Index Hospitalization or in Year before Hospitalization
| Received any psychotropic medication or psychotherapy, n (%) | Received any psychotropic medication, n (%) | Received any psychotherapy, n (%) | |
|---|---|---|---|
| Index hospitalization | |||
| Incident depression (n = 191) | 74 (38.7) | 66 (34.6) | 16 (8.4) |
| Incident anxiety (n = 47) | 11 (23.4) | 11 (23.4) | 0 (0.0) |
| Year before hospitalization | |||
| Incident depression (n = 831) | 496 (59.7) | 384 (46.2) | 289 (34.8) |
| Incident anxiety (n = 258) | 164 (63.6) | 115 (44.6) | 101 (39.2) |
Most mental healthcare provided during the index hospitalization came in the form of psychotropic medication. The most common antidepressants prescribed were citalopram, mirtazapine, and sertraline, and the most common medications for incident anxiety were trazodone and citalopram. Psychotherapy was accessed more often before hospitalization than during the hospitalization (35% of patients with incident past-year depression and 39% with incident past-year anxiety received some psychotherapy).
Discussion
At least one-quarter of the veterans in our sample had a mental illness or substance use disorder while hospitalized for a serious physical illness. This may be an underestimate, however, given the substantially higher prevalence of depression and anxiety observed in the years before hospitalization and the potential for underreporting of substance use. Many treatment guidelines for mental illnesses among seriously physically ill patients concern the treatment of depression or focus on patients with cancer.22,23Although depression was the most common mental illness observed in our sample, a significant subsample of our patients experienced anxiety and alcohol abuse/dependence. Moreover, our results suggest that patients with advanced COPD may have an especially high mental illness burden.
The frequencies of past-year depression and anxiety that we observed in veterans with serious physical illnesses are higher than those observed in hospitalized veterans with less severe physical illnesses.24,25 Moreover, the rate of past-year depression in our sample was 70% higher than that observed among veterans receiving care within a patient-centered medical home.26
These results highlight the need for mental and physical health integration initiatives to be expanded to include patients with life-limiting physical illnesses. Coordination of mental and physical healthcare and increased mental health staffing are priorities within the Veterans Health Administration (VHA), but integration and staffing initiatives have primarily focused on primary care patients.27
Although resolution of an acute physical crisis may be the priority of a seriously ill patient's hospitalization, initiating treatment of incident depression and anxiety before discharge may be beneficial to the patient. Depression and anxiety are associated with worse pain and greater likelihood of hospital readmission.4,28–30 Patients with incident depression or anxiety during the index hospitalization almost exclusively received psychotropic medication and not psychotherapy. It is unclear whether the patients in our sample were deemed too ill to access or benefit from psychotherapy, were disinterested in psychotherapy, or whether psychotherapy was not provided for some other reason. It is also possible that these patients were receiving psychosocial care, but not formal psychotherapy, from social workers, chaplains, or other palliative care providers. However, given that recommended first-line depression and anxiety treatment is either psychotherapy or medication16,17 and that drug therapy is associated with adverse drug–drug and drug–condition interactions in seriously ill patients, reasons for low use of psychotherapy in the hospital among patients with serious comorbid physical illness should be explored further.
Limitations
Depression is underrecognized as well as under-recorded in administrative data,31 and we are unable to distinguish between patients without a diagnosis and those with a diagnosis that is not recognized or recorded. In outpatient settings, anxiety and substance use disorders may be overdiagnosed if reliant on a single diagnosis code.32,33 To mitigate these concerns, secondary outpatient depression or anxiety diagnoses were only counted if patients had two of these on different days.
Our dataset does not allow us to distinguish between care not provided, not recorded, and offered but refused by patients. We are unable to determine whether patients with an incident diagnosis of depression or anxiety at the index hospitalization sought mental healthcare after hospital discharge. In addition, we are unable to determine whether patients who received palliative care are more likely to have mental health diagnoses recognized or whether patients received mental healthcare outside of the VHA. Previous reports, however, suggest that veterans enrolled in VHA seek the majority of their mental healthcare within the VHA.34 In addition, we included benzodiazepines in our count of antianxiety medications, which are effective for GAD but not PTSD.17 The gaps in treatment we identify are therefore likely conservative estimates of need.
Although we focus on VHA care, gaps in mental healthcare are likely to be as large, if not larger, among seriously physically ill veterans receiving care outside of the VHA integrated health system. An estimated 73% of all veterans and 35% of VHA-enrolled veterans received their healthcare outside of the VHA in FY2014.35
Conclusion
One-quarter of veterans hospitalized with serious physical illnesses has comorbid mental illnesses, and many may benefit from depression and anxiety treatment. Increased focus on comorbid mental illnesses among the seriously physically ill may improve quality of life and symptom control among hospitalized veterans.
Supplementary Material
Acknowledgments
Dr. M.M.G. is supported by a career development award from VA HSR&D (CDA 11-201/CDP 12-255). Dr. H.G.P. is supported by the following NIH Grant Nos.: CA197730, MH095378, and MD007652. Mr. S.N. is supported by the American Federation for Aging Research.
Author Disclosure Statement
No competing financial interests exist. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- 1.Patel V, Chatterji S: Integrating mental health in care for noncommunicable diseases: An imperative for patient-centered care. Health Aff 2015;34:1498–1505 [DOI] [PubMed] [Google Scholar]
- 2.Himmelhoch S, Weller WE, Wu AW, et al. : Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care 2004;42:512–521 [DOI] [PubMed] [Google Scholar]
- 3.Miovic M, Block S: Psychiatric disorders in advanced cancer. Cancer 2007;110:1665–1676 [DOI] [PubMed] [Google Scholar]
- 4.Olfson M, Gameroff MJ: Generalized anxiety disorder, somatic pain and health care costs. Gen Hosp Psychiatry 2007;29:310–316 [DOI] [PubMed] [Google Scholar]
- 5.Singer AE, Meeker D, Teno JM, et al. : Symptom trends in the last year of life from 1998 to 2010. Ann Intern Med 2015;162:175–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teno JM, Freedman VA, Kasper JD, et al. : Is care for the dying improving in the United States? J Palliat Med 2015;18:662–666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Periyakoil VS: A never-ending battle. N Engl J Med 2015;373:2399–2401 [DOI] [PubMed] [Google Scholar]
- 8.Holland JM, Currier JM, Kirkendall A, et al. : Sadness, anxiety, and experiences with emotional support among veteran and nonveteran patients and their families at the end of life. J Palliat Med 2014;17:708–711 [DOI] [PubMed] [Google Scholar]
- 9.Garrido MM, Penrod JD, Prigerson HG: Unmet need for mental health care among veterans receiving palliative care: Assessment is not enough. Am J Geriatr Psychiatry 2014;22:540–544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malin JL, O'Neill SM, Asch SM, et al. : Quality of supportive care for patients with advanced cancer in a VA Medical Center. J Palliat Med 2011;14:573–577 [DOI] [PubMed] [Google Scholar]
- 11.Dy SM, Kiley KB, Ast K, et al. : Measuring what matters: Top-ranked quality indicators for hospice and palliative care from the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association. J Pain Symptom Manage 2015;49:773–781 [DOI] [PubMed] [Google Scholar]
- 12.Sloss E, Solomon D, Shekelle P, et al. : Selecting target conditions for quality of care improvement in vulnerable older adults. J Am Geriatr Soc 2000;48:363–369 [DOI] [PubMed] [Google Scholar]
- 13.Penrod JD, Deb P, Dellenbaug C, et al. : Hospital-based palliative care consultation: Effects on hospital cost. J Palliat Med 2010;13:1–7 [DOI] [PubMed] [Google Scholar]
- 14.Chermack ST, Zivin K, Valenstein M, et al. : The prevalence and predictors of mental health treatment in a national sample of depressed veterans. Med Care 2008;46:813–820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tiwari A, Rajan M, Miller D, et al. : Guideline-consistent antidepressant treatment patterns among veterans with diabetes and major depressive disorder. Psychiatr Serv 2008;59:1139–1147 [DOI] [PubMed] [Google Scholar]
- 16.Department of Veterans Affairs/Department of Defense: VA/DoD Clinical Practice Guideline for Management of Major Depressive Disorder, 2009. www.healthquality.va.gov/guidelines/mh/mdd/index.asp (Last accessed November4, 2016)
- 17.Department of Veterans Affairs/Department of Defense: VA/DoD Clinical Practice Guideline for Management of Post-Traumatic Stress, 2010. www.healthquality.va.gov/guidelines/mh/ptsd/index.asp (Last accessed November4, 2016)
- 18.Pfeiffer PN, Ganoczy D, Zivin K, et al. : Outpatient follow-up after psychiatric hospitalization for depression and later readmission and treatment adequacy. Psychiatr Serv 2012;63:1239–1242 [DOI] [PubMed] [Google Scholar]
- 19.Baldwin DS, Anderson IM, Nutt DJ, et al. : Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology. J Psychopharmacol 2014;28:403–439 [DOI] [PubMed] [Google Scholar]
- 20.Bandelow B, Sher L, Bunevicius R, et al. : Guidelines for the pharmacological treatment of anxiety disorders, obsessive-compulsive disorder and posttraumatic stress disorder in primary care. Int J Psychiatry Clin Pract 2012;16:77–84 [DOI] [PubMed] [Google Scholar]
- 21.StataCorp: Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015 [Google Scholar]
- 22.Rayner L, Higginson IJ, Price A, et al. : The Management of Depression in Palliative Care: European Clinical Guidelines, 2010. www.epcrc.org/getpublication2.php?id=6VW4bQY9JujQVGSItDs6 (Last accessed November4, 2016)
- 23.National Comprehensive Cancer Network: Clinical Practice Guidelines in Oncology: Distress Management. Version 2.2015, 2015. www.nccn.org/professionals/physician_gls/PDF/distress.pdf (Last accessed November4, 2016)
- 24.Booth BM, Blow FC, Cook CA: Functional impairment and co-occurring psychiatric disorders in medically ill hospitalized men. Arch Intern Med 1998;158:1551–1559 [DOI] [PubMed] [Google Scholar]
- 25.Banta JE, Andersen RM, Young AS, et al. : Psychiatric comorbidity and mortality among veterans hospitalized for congestive heart failure. Mil Med 2010;175:732–741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trivedi RB, Post EP, Sun H, et al. : Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health 2015;105: 2564–2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Veterans Affairs: Report to the Secretary, A Comprehensive VHA Strategic Plan for Mental Health Services–Revised [online], 2004
- 28.Ahmedani BK, Solfberg LI, Copeland LA, et al. : Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiatr Serv 2015;66:134–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pantilat SZ, O'Riordan DL, Rathfon MA, et al. : Etiology of pain and its association with quality of life among patients with heart failure. J Palliat Med 2016. [Epub ahead of print]; DOI: 10.1089/jpm.2016.0095 [DOI] [PubMed] [Google Scholar]
- 30.Mausbach BT, Irwin SA: Depression and healthcare service utilization in patients with cancer. Psycho-Oncology 2016. [Epub ahead of print]; DOI: 10.1002/pon.4133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Townsend L, Walkup JT, Crystal S, et al. : A systematic review of validated methods for identifying depression using administrative data. Pharmacoepidemiol Drug Saf 2012;21(Suppl. 1):163–173 [DOI] [PubMed] [Google Scholar]
- 32.Davis KAS, Sudlow CLM, Hotopf M: Can mental health diagnoses in administrative data be used for research? A systematic review of the accuracy of routinely collected diagnoses. BMC Psychiatry 2016;16:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gravely AA, Cutting A, Nugent S, et al. : Validity of PTSD diagnoses in VA administrative data: Comparison of VA administrative PTSD diagnoses to self-reported PTSD Checklist scores. J Rehabil Res Dev 2011;48:21–30 [DOI] [PubMed] [Google Scholar]
- 34.McCarthy JF, Zivin K, Austin KL, et al. : Does consideration of Medicare use affect VA evaluations of treatment for new episodes of depression? Adm Policy Ment Health 2008;35:468–476 [DOI] [PubMed] [Google Scholar]
- 35.Bagalman E: The number of veterans that use VA health care services: A fact sheet. Congressional Research Service Report R43579, June 3, 2014
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.