Abstract
Background
Although insomnia has been identified as a robust predictor of suicidal ideation and behaviors, little is known about the mechanisms by which sleep disturbances confer risk for suicide. We investigated thwarted belongingness as an explanatory link between insomnia symptoms and suicidal ideation across three military service member and veteran samples.
Methods
Data were collected among United States military service members and veterans (N1=937, N2=3,386, N3=417) who completed self-report measures of insomnia symptoms, thwarted belongingness, suicidal ideation, and related psychiatric symptoms (e.g., anxiety, hopelessness). Bias-corrected bootstrap mediation analyses were utilized to examine the indirect effects of insomnia symptoms on suicidal ideation through thwarted belongingness, controlling for related psychiatric symptoms.
Results
Consistent with study hypotheses, thwarted belongingness significantly accounted for the relationship between insomnia and suicidal ideation across all three samples; however, insomnia symptoms did not significantly account for the relationship between thwarted belongingness and suicidal ideation, highlighting the specificity of our findings.
Limitations
This study utilized cross-sectional, self-report data.
Conclusions
Insomnia may confer suicide risk for military service members and veterans, in part, through the pathway of thwarted belongingness. Additional prospective studies are warranted to further delineate this model of risk. Our results offer a potential target for the therapeutic prevention of suicide, via the promotion of belongingness, among service members and veterans experiencing insomnia symptoms.
Keywords: Insomnia, Suicidal Ideation, Loneliness, Thwarted Belongingness, Military, Veterans
Introduction
In the past decade, rates of suicide and suicide attempts have increased among United States military personnel (LeardMann et al., 2013; Ramchand et al., 2011) and veterans (Department of Veterans Affairs Office of Public and Intergovernmental Affairs, 2016; LeardMann et al., 2013). Currently, the prevalence of suicidal behaviors among service members exceeds rates found among matched civilian populations (Nock et al., 2014; Nock et al., 2015; Ursano, Heeringa, et al., 2015; Ursano, Kessler, et al., 2015). In response, there has been a call for increased suicide prevention efforts among both military personnel and veteran populations (Kuehn, 2009; Ramchand et al., 2011). To inform these efforts and illuminate potential points of intervention, there is a critical need to identify suicide risk factors and to understand the pathways by which these factors lead to suicidal thoughts and behaviors.
Among the most robust risk factors for suicide is insomnia (see Bernert, Kim, Iwata, & Perlis, 2015 and Pigeon, Pinquart, & Conner, 2012 for review). For instance, insomnia has been repeatedly shown to predict future suicidal ideation (Wong and Brower, 2012; Wong et al., 2011) as well as death by suicide (Bernert, Turvey, Conwell, & Joiner, 2014; Goldstein, Bridge, & Brent, 2008; Kodaka et al., 2014). This association has also been demonstrated among military service members and veterans. For example, a study by Ribeiro and colleagues (2012) found that insomnia symptoms predicted suicidal ideation among a sample of military service members above and beyond other risk factors (e.g., hopelessness, depression, diagnosis of posttraumatic stress disorder [PTSD]). In another study, veteran suicide decedents who reported sleep disturbances at their last health care visit died within a shorter period of time after this visit than those without sleep disturbances (Pigeon et al., 2012a). These findings highlight insomnia as a critical warning sign for suicide among veterans.
Given this well-established link, there is a strong rationale to better understand the pathways by which insomnia and sleep disturbances confer risk for suicide among military service members and veterans, especially since insomnia is highly prevalent in these populations (Capaldi et al., 2011; Kroenke et al., 1998; Lewis et al., 2009; Miller et al., 2011; Neylan et al., 1998; Peterson et al., 2008; Seelig et al., 2010). Since few studies to date have empirically tested the mechanisms underlying the association between insomnia and suicide risk, a theoretical approach may provide a useful framework for exploring this relationship.
The interpersonal theory of suicide (Joiner, 2005; Van Orden et al., 2010), which has amassed growing empirical support (e.g., Bryan, Morrow, Anestis, & Joiner, 2010; Christensen, Batterham, Soubelet, & Mackinnon, 2013; Cukrowicz, Jahn, Graham, Poindexter, & Williams, 2013; Czyz, Berona, & King, 2014; Joiner & Van Orden, 2008), may provide one possible explanation for the robust connection between insomnia and suicide risk. This theory proposes that lethal and near-lethal suicide attempts occur when an individual has both the desire and capability for suicidal behavior. Suicidal desire emerges when thwarted belongingness (i.e., the feeling that one does not belong) and perceived burdensomeness (i.e., the belief that one’s death is worth more than one’s life) co-occur. Capability for suicide is characterized by increased pain tolerance and fearlessness about death.
Using the interpersonal theory as a guide, insomnia may confer risk for suicide specifically by increasing feelings of thwarted belongingness. Since insomnia is defined by recurrent difficulties falling asleep, staying asleep, and/or waking up too early (American Psychiatric Association [APA], 2013), those suffering from insomnia are likely to experience extended periods of wakefulness during hours when the majority of the population is asleep. This experience may itself be lonely. Clinically significant insomnia also leads to functional impairment, including minor irritations and interferences in one’s social life and relationships (see Sateia, Doghramji, Hauri, & Morin, 2000, and Shochat, Cohen-Zion, & Tzischinsky, 2014, for review). For example, studies have found that poor sleep is associated with difficulties both establishing and maintaining relationships (Roberts and Duong, 2013; Roberts et al., 2001). This may then result in isolation and feelings of loneliness. Furthermore, inadequate sleep is related to impaired emotion regulation abilities (see Walker, 2009 for review). Indeed, studies have shown that individuals with poor sleep quality may have greater difficulties reappraising negative situations (Mauss et al., 2013) and chronic sleep restriction may impact the effective regulation of emotions (Baum et al., 2014). These difficulties may, in turn, increase individuals’ vulnerability to maladaptive thoughts about their belongingness. Taken together, chronic insomnia may contribute to feelings of loneliness (cf. thwarted belongingness), resulting in elevated suicidal desire and, ultimately, greater suicide risk.
Findings from recent studies support this proposed pathway. Our research group has found both a cross-sectional and prospective relationship between insomnia symptoms and loneliness across six samples, including undergraduates, community-dwelling adults, and military personnel. Similarly, Chu and colleagues (2016) not only found a significant association between insomnia symptoms and thwarted belongingness but also demonstrated that thwarted belongingness significantly accounted for the association between insomnia and suicidal ideation in a sample of South Korean university students. Chu and colleagues (in press) replicated these findings across three additional samples—U.S. undergraduates, adult mental health outpatients, and adult primary care patients—and demonstrated that this pattern of findings remained even after controlling for anxiety symptoms. Finally, Nadorff and colleagues (2014) examined the relationship between insomnia symptoms, interpersonal theory constructs, and suicide risk in two undergraduate samples. Interpersonal theory constructs did not significantly account for the relationship between insomnia symptoms and suicidal ideation in one of the samples. However, in the other sample, this relationship was no longer significant after controlling for interpersonal theory constructs. These findings suggest that interpersonal theory constructs, including thwarted belongingness, may serve as an explanatory link between insomnia and suicide risk. Consistent with this assertion, a study of older adults also revealed that insomnia symptoms were no longer related to suicide risk after controlling for interpersonal theory variables (Golding et al., 2015). However, these equivocal results emphasize the need for further investigation into the relationship between these symptom constellations.
The Present Investigation
In considering the (1) relatively high rates of suicidal thoughts and behaviors among military service members and veterans, (2) prevalence of sleep disturbances in these populations, and (3) vast body of evidence identifying insomnia as a potent suicide risk factor, empirical exploration of the mechanisms underlying the relationship between insomnia and suicide risk is indicated. As such, we investigated whether thwarted belongingness may serve as an explanatory link between insomnia symptoms and suicidal ideation across three large samples of military service members and veterans. Based on prior research and propositions of the interpersonal theory of suicide, we hypothesized that (1) insomnia symptom severity would be associated with more severe suicidal ideation and greater thwarted belongingness, and (2) thwarted belongingness would significantly account for the relationship between insomnia symptoms and suicidal ideation, controlling for related psychiatric symptoms. To evaluate the specificity of effects, we conducted secondary analyses to examine whether insomnia symptoms may serve as an explanatory link in the association between thwarted belongingness and suicidal ideation.
Consistent with similar studies we controlled for symptoms associated with both sleep problems and suicide risk. Specifically, where possible, we controlled for: (1) anxiety sensitivity and anxiety symptoms (Capron et al., 2012; Hendin, Maltsberger, & Szanto, 2007; Johnson, Roth, & Breslau, 2006); (2) perceived burdensomeness (Christensen et al., 2013; Cukrowicz et al., 2013; Nadorff et al., 2014); and (3) general hopelessness (Beck, Brown, & Steer, 1989; Beck, Steer, Kovacs, & Garrison, 1985; Woosley, Lichstein, Taylor, Riedel, & Bush, 2014). We also controlled for depression symptoms where possible (Brown et al., 2000; Cavanagh et al., 2003); however, these analyses were exploratory in light of evidence for conceptual and empirical problems with controlling for depression in analyses predicting suicidal ideation (Rogers et al., 2016). Lastly, though less is known about perceived burdensomeness’ role in the insomnia and suicidal ideation relationship, this construct is posited as necessary for the emergence of suicidal desire (Joiner, 2005; Van Orden et al., 2010). Thus, where possible, we conducted exploratory analyses examining: (1) thwarted belongingness and perceived burdensomeness as parallel explanatory factors and (2) whether perceived burdensomeness moderated thwarted belongingness’ mediating effects. All participants provided informed consent prior to study participation, and relevant Institutional Review Boards approved procedures for each study.
Study 1
In Study 1, we tested the mediating role of thwarted belongingness in the relationship between insomnia symptoms and suicidal ideation, controlling for hopelessness and anxiety sensitivity, in a sample of military services members and veterans.
Methods
Participants and Procedures
A total of 937 United States military service members and veterans were included in Study 1. Participants ranged in age from 18 to 88 years (M=38.2, SD=14.5), and the sample was predominantly male (82.1%). In terms of race, 67.9% identified as White, 15.2% Black/African American, 1.7% American Indian/Alaska Native, 1.5% Multiracial, 1.1% Asian, 0.7% Native Hawaiian/Other Pacific Islander, and 11.9% declined to state. For branch of service, 49.6% reported an Army affiliation, 21.7% Navy, 18.1% Marine Corps, 7.0% Air Force, 0.5% Coast Guard, 0.1% National Guard, and 2.9% other. Participants’ current military status (i.e., active duty, reserve, separated) was not systematically collected. Data were aggregated from fifteen independent studies funded by the Military Suicide Research Consortium (MSRC). There was variation across studies in recruitment methods, study setting, study aims and designs, and survey administration. However, all participants were asked to complete the same battery of self-report measures at baseline/study enrollment.
Measures
Due to study setting constraints, factor analyses of prior datasets were used to select a subset of items from each measure to comprise a brief assessment battery (Gutierrez and Joiner, 2016). This common set of survey items was administered across all fifteen studies.
Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986)
A 5-item version of the 16-item ASI was used to assess individuals’ tendency to fear the consequences of bodily sensations related to anxiety. Items are rated on a 5-point scale (1=Very Little, 5=Very Much), with total scores ranging from 5 to 25 and greater scores reflecting greater anxiety sensitivity. The ASI has demonstrated strong psychometric properties (Zvolensky et al., 2001), and its internal consistency in this study was strong (α=.91).
Beck Hopelessness Scale (BHS; Beck, Weissman, Lester, & Trexler, 1974)
A 3-item version of the original 20-item BHS was used to assess hopelessness. Participants are asked to rate statements about their attitudes toward the future as “True” or “False.” Total scores on the abbreviated BHS range from 0 to 3, with higher scores reflecting greater hopelessness. The BHS has been shown to have good internal consistency and reliability (Beck et al., 1974; Steed, 2001), and the 3-item BHS in this study demonstrated adequate internal consistency (α=.62).
Depressive Symptom Inventory – Suicidality Subscale (DSI-SS; Metalsky & Joiner, 1997)
The DSI-SS is a 4-item measure of suicidal ideation severity. Individuals are presented with four statement groups (e.g., controllability of thoughts) and select the statement from each group that best characterizes them. DSI-SS total scores range from 0 to 12, with increasing scores indicating greater symptom severity. The DSI-SS demonstrates good psychometric properties (Joiner, Pfaff, & Acres, 2002), including compared to other suicide risk measures (Batterham et al., 2014). Internal consistency of the DSI-SS was good (α=.86).
Insomnia Severity Index (ISI; Bastien, Vallieres, Morin, Vallières, & Morin, 2001)
An abbreviated 5-item version of the 7-item ISI was used to measure insomnia symptom severity. Individuals are asked to rate various sleep complaints (e.g., difficulties falling asleep) on a 5-point Likert scale. Total scores on the abbreviated ISI range from 0 to 20, with greater scores signaling more severe insomnia symptoms. Prior studies indicate that the full ISI has high internal consistency and validity (Bastien et al., 2001; Morin et al., 2011). In this study, the abbreviated ISI demonstrated good internal consistency (α=.82).
Interpersonal Needs Questionnaire–Thwarted Belongingness Subscale (INQ-TB; Van Orden, Cukrowicz, Witte, & Joiner, 2012)
An adapted 5-item version of the 9-item INQ-TB was used to detect thwarted belongingness. Individuals rate each item on a 7-point Likert scale, and total scores range from 5 to 35, with higher scores signaling greater thwarted belongingness. The INQ has good internal consistency and predictive validity (Van Orden, Cukrowicz, Witte, & Joiner, 2012), including when a shortened version is utilized (Hill et al., 2015). The abbreviated INQ-TB used in this study demonstrated good internal consistency (α=.89).
Data Analytic Plan
Bias-corrected bootstrap mediation analyses (5,000 bootstrap resamples; Preacher & Hayes, 2008) were utilized to test the study hypothesis that INQ thwarted belongingness would significantly account for the relationship between ISI insomnia symptoms and DSI-SS suicidal ideation. Analyses controlled for both ASI anxiety sensitivity and BHS hopelessness. As noted above, to test the specificity of indirect effects, secondary analyses were conducted to test whether ISI insomnia symptoms would significantly account for the relationship between INQ thwarted belongingness and DSI-SS suicidal ideation, again controlling for ASI anxiety sensitivity and BHS hopelessness. Effects were considered statistically significant if the 95% confidence interval (CI) did not cross zero. Data regarding perceived burdensomeness and depression symptoms were not collected in this study; thus, we were unable to conduct exploratory analyses in this sample.
Results
Descriptive Statistics (Table 1)
Table 1.
Means, Standard Deviations, and Intercorrelations for Self-Report Measures
| STUDY 1 | 1 | 2 | 3 | 4 | 5 | M | SD | Range | α |
|---|---|---|---|---|---|---|---|---|---|
| ISI Insomnia Symptoms1 | -- | 11.49 | 4.91 | 0–20 | .82 | ||||
| 2. INQ Thwarted Belongingness2 | .22** | -- | 19.98 | 8.24 | 5–35 | .89 | |||
| 3. DSI-SS Suicidal Symptoms | .21** | .33** | -- | 3.30 | 3.03 | 0–12 | .86 | ||
| 4. BHS Hopelessness3 | – .11** | .29** | – .27** | -- | 1.23 | 1.11 | 0–3 | .62 | |
| 5. ASI Anxiety Sensitivity4 | .41** | .25** | .34** | – .13** | -- | 13.18 | 6.20 | 5–25 | .91 |
| STUDY 2 | 1 | 2 | 3 | 4 | 5 | M | SD | Range | α |
| 1. ISI Insomnia Symptoms1 | -- | 4.43 | 3.73 | 0–20 | .87 | ||||
| 2. INQ Thwarted Belongingness5 | .27** | -- | 7.20 | 4.57 | 4–28 | .91 | |||
| 3. DSI-SS Suicidal Symptoms | .11** | .21** | -- | .03 | .25 | 0–7 | .70 | ||
| 4. INQ Perceived Burdensomeness5 | .22** | .35** | .32** | -- | -- | 4.43 | 1.70 | 4–28 | .87 |
| STUDY 3 | 1 | 2 | 3 | 4 | 5 | M | SD | Range | α |
| 1. ISI Insomnia Symptoms | -- | 16.08 | 7.87 | 3–31 | .94 | ||||
| 2. INQ Thwarted Belongingness | .60** | -- | 30.16 | 14.53 | 9–62 | .85 | |||
| 3. SBQ-R Suicide Risk | .34** | .49** | -- | 8.12 | 2.75 | 4–18 | .81 | ||
| 4. INQ Perceived Burdensomeness | .54** | .73** | .55** | -- | 14.18 | 10.14 | 7–42 | .96 | |
| 5. MHP-P Anxiety Symptoms | .66** | .63** | .40** | .63** | -- | 8.20 | 3.80 | 3–15 | .90 |
| 6. MHP-P Depression Symptoms | .70** | .77** | .48** | .67** | .70** | 8.55 | 3.55 | 3–15 | .86 |
p < .01
5-item version of the 7-item ISI
5-item version of the 9-item INQ-TB
3-item version of the 20-item BHS
5-item version of the 16-item ASI
8-item version of the INQ, with 4 INQ-TB and 4 INQ-PB items
Note. ISI = Insomnia Severity Index; INQ = Interpersonal Needs Questionnaire; DSI-SS = Depressive Symptoms Index—Suicidality Subscale; BHS = Beck Hopelessness Scale; ASI = Anxiety Sensitivity Index; SBQ-R = Suicidal Behavior Questionnaire—Revised; MHP-P = Multidimensional Health Profile—Psychosocial Functioning
More severe ISI insomnia symptoms were significantly correlated with more severe DSI-SS suicidal ideation (r=.21, p<.01) and greater levels of INQ thwarted belongingness (r=.22, p<.01). Greater INQ thwarted belongingness was also significantly associated with more severe suicidal ideation (r=.33, p<.01).
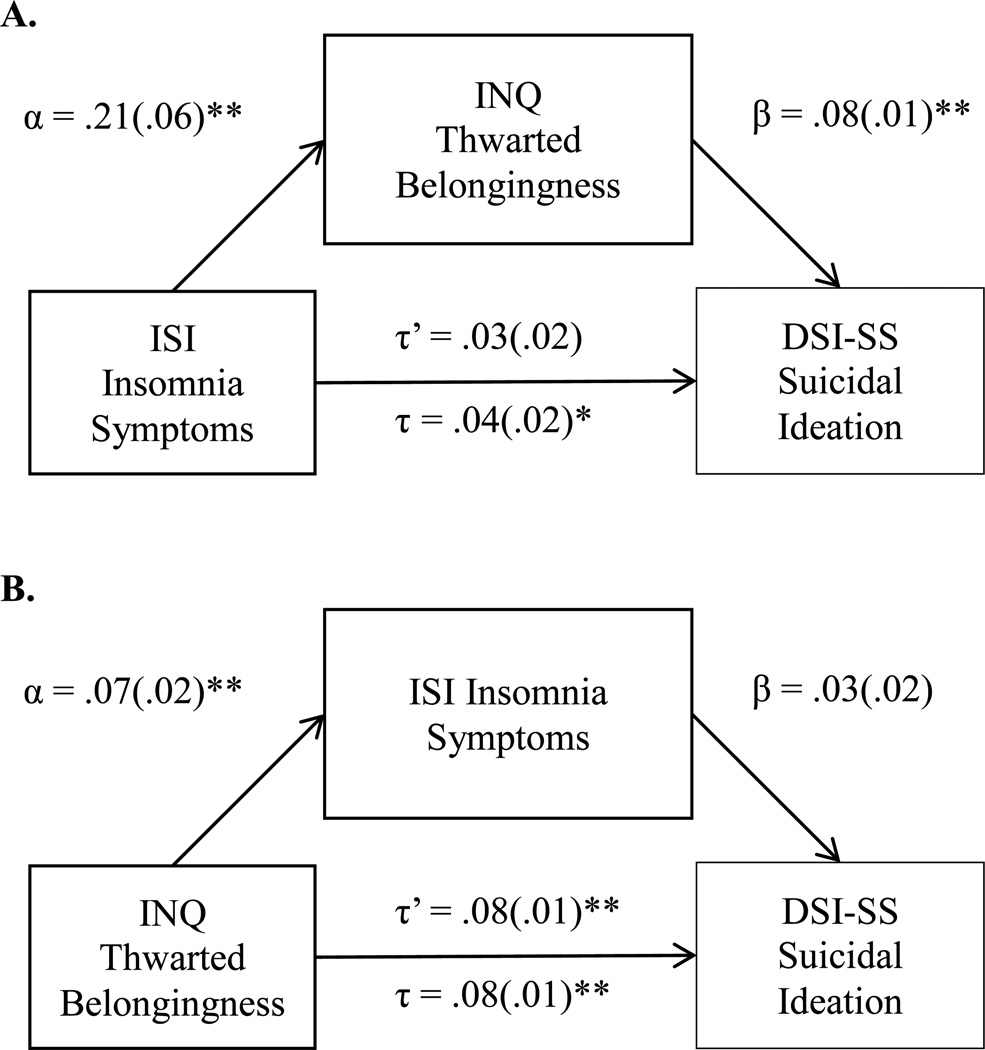
Primary Analyses: Thwarted Belongingness as a Mediator (Figure 1A)
Figure 1.
Study 1 Unstandardized Regression Coefficients and Standard Errors from Mediation Analyses
p < .05; ** p < .01
Note. α = independent variable to mediator path; β = mediator to dependent variable path; τ’ = direct effects of independent variable on dependent variable; τ = total effects of independent variable on dependent variable; ISI = Insomnia Severity Index; INQ = Interpersonal Needs Questionnaire; DSI-SS = Depressive Symptoms Index—Suicidality Subscale; Analyses controlling for anxiety sensitivity and hopelessness
The overall regression model was significant (F[3,933]=65.14, p<.01) and accounted for 17.3% of the variance in suicidal ideation. ISI insomnia symptoms were significantly associated with INQ thwarted belongingness (B=.21, SE=.06, p<.01), and INQ thwarted belongingness was significantly associated with DSI-SS suicidal ideation (B=.08, SE=.01, p<.01); however, the direct effects of ISI scores on DSI-SS scores were not significant (B=.03, SE=.02, p=.19), indicating an “indirect only” effect. The indirect effects of ISI scores on DSI-SS scores through INQ-TB scores were significant (95% CI: .01, .03). All analyses controlled for BHS hopelessness and ASI anxiety sensitivity.
Secondary Analyses: Insomnia Symptoms as a Mediator (Figure 1B)
The overall regression model was significant (F[3,393]=82.46, p<.01), explaining 21.0% of the variance in DSI-SS suicidal ideation. Although INQ thwarted belongingness was significantly associated with ISI insomnia symptoms (B=.07, SE=.02, p<.01), ISI insomnia symptoms were not significantly associated with DSI-SS suicidal ideation (B=.03, SE=.02, p=.19). The direct effects of INQ-TB scores on DSI-SS scores were significant (B=.08, SE=.01, p<.01); however, the indirect effects of INQ-TB scores on DSI-SS scores through ISI scores were not (95% CI: -.01, .01). Similarly, all analyses included BHS hopelessness and ASI anxiety sensitivity as covariates.
Discussion
Findings are consistent both with study hypotheses and prior studies in this domain. As noted previously, findings from our research group indicate that more severe insomnia symptoms have been shown to be associated with greater levels of thwarted belongingness, even after controlling for anxiety symptoms. These findings also mirror results from a study by Chu and colleagues (2016), in which thwarted belongingness significantly accounted for the association between insomnia symptoms and suicidal ideation in a sample of South Korean undergraduates. This finding suggests that the relations between insomnia symptoms, thwarted belongingness, and suicidal ideation may demonstrate similar patterns across populations and may not be specific to South Korean young adults or military service members and veterans. In our current sample, it is also worthwhile to note that thwarted belongingness remained a significant mediator even after controlling for hopelessness and anxiety sensitivity, both of which have been associated with suicide risk and sleep problems (Beck, 1986; Capron et al., 2012; Klonsky, Kotov, Bakst, Rabinowitz, & Bromet, 2012). This finding underscores the robustness of this study’s results. On the other hand, insomnia symptoms did not significantly account for the relationship between thwarted belongingness and suicidal ideation, highlighting the specificity of the relationship between these variables. Despite these findings, the use of abbreviated measures and heterogeneity of the sample (e.g., both service members and veterans recruited across 15 distinct studies with varying aims and designs) represented limitations of this study. Indeed, inconsistent with prior work (Beck et al., 1989; Woosley et al., 2014), hopelessness was negatively associated with insomnia symptoms and suicidal ideation, which may have been due to the BHS’ low internal consistency (i.e., α=.62).
Study 2
Study 2 aimed to address Study 1’s limitation of sample and study design heterogeneity (i.e., use of aggregated data from fifteen unique studies) by examining thwarted belongingness as an explanatory factor in the relationship between insomnia symptoms and suicidal ideation, controlling for perceived burdensomeness, in a single sample of Army recruiters.
Methods
Participants and Procedures
A total of 3,386 Army recruiters participated in Study 2. Participants were majority male (91.5%) and ranged in age from 20 to 57 years (M=29.91, SD=4.93). For self-reported race/ethnicity, the majority identified as White (66.2%), followed by Black/African American (14.8%), Hispanic/Latino (13.5%), Asian (2.7%), Native Hawaiian/Other Pacific Islander (1.6%), and American Indian/Alaska Native (1.1%). Detailed study procedures have previously been published (see Ribeiro et al., 2015).
Measures
As in Study 1, given study setting constraints, a subset of items from each measure was selected via factor analyses of prior datasets to comprise a brief survey battery.
ISI (Bastien, Vallieres, Morin, Vallières, & Morin, 2001)
The same abbreviated 5-item version of the 7-item ISI from Study 1 was used to measure insomnia symptom severity. In the current study, the abbreviated ISI exhibited good internal consistency (α=.87).
INQ (Van Orden, Cukrowicz, Witte, & Joiner, 2012)
For this study, an abbreviated 8-item version of the 15-item INQ was utilized. Four items measured thwarted belongingness (INQ-TB) and four perceived burdensomeness (INQ-PB). Responses occur on a 7-point response scale (1=Not at all true for me; 7=Very true for me). The INQ-TB and INQ-PB were found to have good to strong internal consistency in this study (α=.91 and .87, respectively).
DSI-SS (Metalsky & Joiner, 1997)
See Study 1 for a full description of the DSI-SS. In this study, the DSI-SS also demonstrated adequate internal consistency (α=.70).
Data Analytic Plan
Study 2 employed the same data analytic approach as Study 1. Based on available self-report measures, we controlled for INQ perceived burdensomeness rather than ASI anxiety sensitivity and BHS hopelessness. Additionally, exploratory bootstrap mediation analyses were conducted to evaluate: (1) INQ-TB and INQ-PB as parallel mediators of the relationship between ISI insomnia symptoms and DSI-SS suicidal ideation; and (2) INQ-PB as a moderator of INQ-TB’s mediating role in the relationship between ISI insomnia symptoms and DSI-SS suicidal ideation.
Results
Descriptive Statistics (Table 1)
Again, more severe ISI insomnia symptoms were significantly associated with more severe DSI-SS suicidal ideation (r=.11, p<.01) and greater levels of INQ thwarted belongingness (r=.27, p<.01). Greater levels of INQ thwarted belongingness were significantly related to more severe DSI-SS suicidal ideation (r=.21, p<.01).
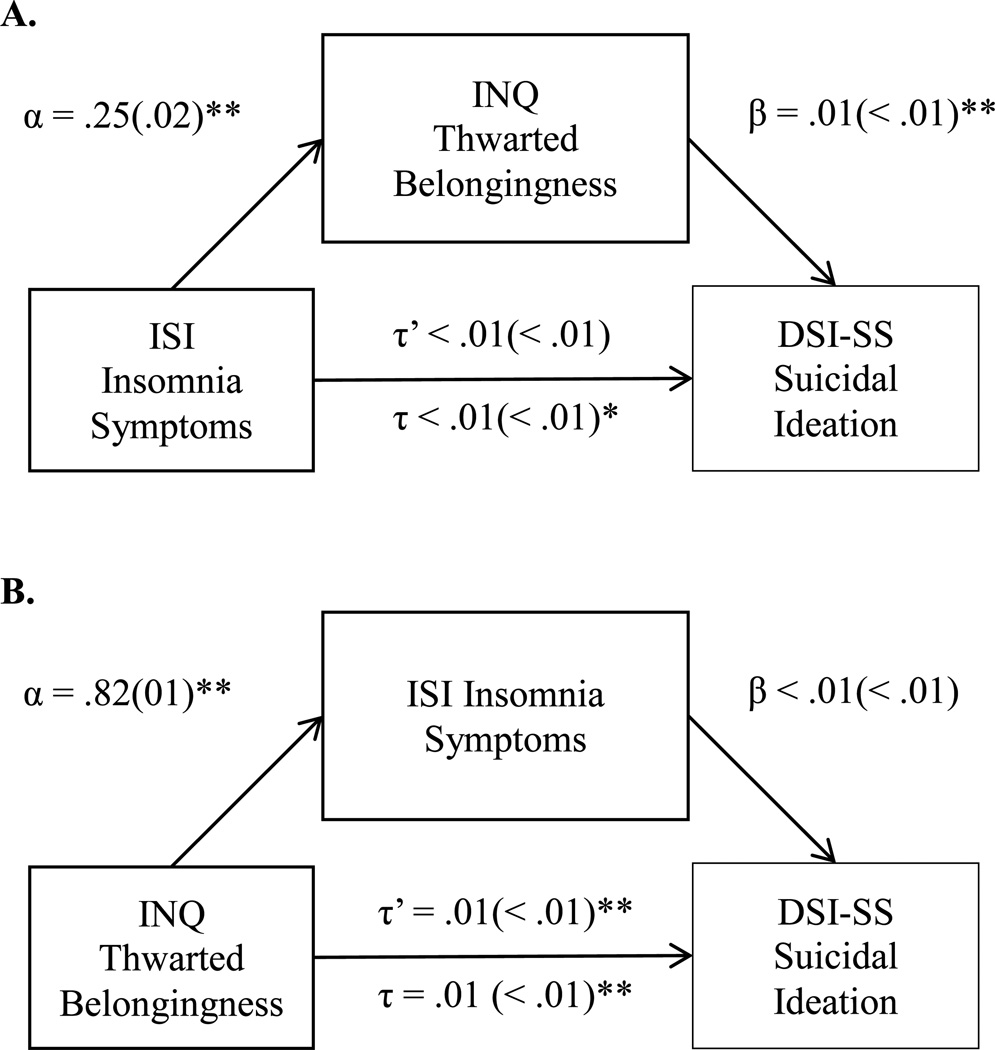
Primary Analyses: Thwarted Belongingness as a Mediator (Figure 2A)
Figure 2.
Study 2 Unstandardized Regression Coefficients and Standard Errors from Mediation Analyses
* p < .05; ** p < .01
Note. α = independent variable to mediator path; β = mediator to dependent variable path; τ’ = direct effects of independent variable on dependent variable; τ = total effects of independent variable on dependent variable; ISI = Insomnia Severity Index; INQ = Interpersonal Needs Questionnaire; DSI-SS = Depressive Symptoms Index—Suicidality Subscale; Analyses controlling for perceived burdensomeness
The overall regression model was significant (F[3,3382]=141.93, p<.01; R2=.11). ISI insomnia symptoms were significantly correlated with INQ thwarted belongingness (B=.25, SE=.02, p<.01), and INQ thwarted belongingness was significantly correlated with DSI-SS suicidal ideation (B=.01, SE<.01, p<.001). The direct effects of ISI scores on DSI-SS scores were not significant (B<.001, SE<.01, p=.36), indicating an “indirect only” effect, in which the indirect effect of ISI scores on DSI-SS scores through INQ-TB scores was significant (95% CI: <.01, .01). All analyses controlled for INQ perceived burdensomeness.
Secondary Analyses: Insomnia Symptoms as a Mediator (Figure 2B)
Again, the overall regression model was significant (F[3,3382]=141.93, p<.01; R2=.11). INQ thwarted belongingness was significantly associated with ISI insomnia symptoms (B=.18, SE=.01, p<.01); however, ISI insomnia symptoms were not significantly associated with DSI-SS suicidal ideation (B<.01, SE<.01, p=.36). The direct effects of INQ thwarted belongingness on DSI-SS suicidal ideation were significant (B=.01, SE<.01, p<.01), but the indirect effects of INQ-TB scores on DSI-SS scores through ISI scores were not significant (95% CI: <-.01, <.01). Of note, INQ-PB burdensomeness was included as a covariate in all analyses.
Exploratory Analyses: Effects of Perceived Burdensomeness
The overall regression model with INQ-TB and INQ-PB as parallel mediators was significant (F[3,3382]=141.92, p<.01; R2=.11). The mediating effects of INQ-TB scores (95% CI: >.01, >.01) and INQ-PB scores (95% CI: >.01, .01) were both significant; however, the pairwise contrast indicated that neither effect was significantly stronger (95% CI: -.01, >.01). Moderated mediation analyses revealed that INQ-PB did not serve as a moderator of INQ-TB’s mediating role in the relationship between ISI insomnia symptoms and DSI-SS suicidal ideation (95% CI: -.01, >.02).
Discussion
Findings from Study 2 were consistent with those from Study 1 and further suggest that thwarted belongingness may serve as an explanatory link in the relationship between insomnia symptoms and suicide risk. Notably, perceived burdensomeness was included as a covariate in analyses. Perceived burdensomeness is strongly associated with suicide risk and depression symptoms (Cukrowicz, Cheavens, Van Orden, Ragain, & Cook, 2011; Jahn, Cukrowicz, Linton, & Prabhu, 2011; Van Orden et al., 2008). Therefore, that our hypotheses were supported even after controlling for this construct is particularly striking. Additionally, similar to Study 1, insomnia symptom severity did not mediate the relationship between thwarted belongingness and suicidal ideation, which emphasizes the specificity of the relationships between these variables. Once again, however, the use of abbreviated measures represented a limitation of the current study. Participants in this sample also reported relatively low rates of suicidal ideation; thus, further work is needed to replicate these findings in a higher-risk military sample.
Interestingly, our exploratory analyses indicated that, when examined as parallel mediators, both perceived burdensomeness and thwarted belongingness served as explanatory factors in the association between insomnia symptoms and suicide risk. As noted previously, insomnia has been shown to impact daytime functioning and emotion regulation abilities (Sateia et al., 2000; Walker, 2009); thus, it is not surprising that more severe insomnia symptoms may then contribute to beliefs that one is a burden on others, explaining this pattern of findings. It is also worth noting that perceived burdensomeness did not moderate thwarted belongingness’ mediating effects, suggesting that thwarted belongingness may serve as an explanatory link between insomnia and suicidal ideation regardless of how severe an individual’s perceptions of being a burden are. This appears to contrast somewhat with propositions of the interpersonal theory (Joiner, 2005; Van Orden et al., 2010) and thereby warrants further investigation.
Study 3
Similar to Studies 1 and 2, we evaluated thwarted belongingness as an explanatory factor in the relationship between insomnia and suicidal ideation. However, Study 3 controlled for anxiety symptoms and perceived burdensomeness, and it utilized full versions of study measures.
Methods
Participants and Procedures
A total of 417 United States military veterans participated in Study 3. Participants ranged in age from 20 to 98 years (M=50.73, SD=16.65), and the majority of participants were male (67.8%). For race/ethnicity, 86.4% of participants identified as White/Caucasian, 7.3% as Multiracial, 1.7% as Black/African American, 0.2% as American Indian/Alaska Native; and 2.2% declined to state. In terms of branch of service, 36.5% reported an Army affiliation, 17.5% Navy, 1% Air Force, 7.7% Marine Corps, 2.6% National Guard, 1.9% Army Reserves, 0.7% Coast Guard, and 16.8% refused to answer. Participants were recruited from the community and completed a battery of web-based self-report measures.
Measures
ISI (Bastien, Vallieres, Morin, Vallières, & Morin, 2001)
The full 7-item ISI was used to measure insomnia symptom severity. Total scores range from 0 to 28, and increasing scores represent increasing severity of insomnia symptoms. In the current study, the full-scale ISI was found to have good internal consistency (α=.94).
INQ (Van Orden, Cukrowicz, Witte, & Joiner, 2012)
The full 15-item INQ was utilized for this study, with 9 items measuring thwarted belongingness (INQ-TB), and 6 items measuring perceived burdensomeness (INQ-PB). The INQ-TB and INQ-PB demonstrated good to strong internal consistency in this study (α=.85 and .96, respectively).
Suicidal Behaviors Questionnaire-Revised (SBQ-R; Osman et al., 2001)
The 4-item SBQ-R is a measure of lifetime and past-year suicidal ideation, as well as future likelihood of suicidal behavior. Total scores range from 3 to 18, and greater scores signal greater suicide risk. Past studies have shown that the SBQ-R has good internal consistency and convergent validity (Osman et al., 2001), and it demonstrated good internal consistency in this study (α=.81).
Multidimensional Health Profile—Psychosocial Functioning (MHP-P; Ruehlman, Lanyon, & Karoly, 1999)
The MHP-P is a 58-item broadband measure of psychosocial and health functioning. Three items probing anxiety symptoms and three probing depression symptoms were included in this study. Respondents rate each item (e.g., “How often have you felt worried?”) on a 1 to 5 Likert scale (1=Not at all; 5=Very). Total scores on both the MHP-P anxiety and depression subscales range from 3 to 15, with increasing scores representing greater symptom severity. The MHP-P anxiety and depression subscales have good internal consistency and convergence with other anxiety and depression measures (Ruehlman et al., 1999). In our study, both MHP-P anxiety and depression subscales demonstrated acceptable internal consistency (α=.90 and .86, respectively).
Data Analytic Plan
Study 3 utilized the same data analytic approach as Study 2; however, the SBQ-R was used to measure suicidal ideation. Also, primary and secondary analyses controlled specifically for INQ perceived burdensomeness and MHP-P anxiety symptoms. We then conducted analyses additionally controlling for MHP-P depression symptoms, but we recommend that these results be interpreted with caution due to evidence suggesting that what remains when depression is covaried out of suicidal ideation lacks conceptual meaning (Rogers et al., 2016). Exploratory analyses first controlled for MHP-P anxiety symptoms and then both MHP-P anxiety and depression symptoms.
Results
Descriptive Statistics (Table 1)
More severe ISI insomnia symptoms were significantly associated with more severe SBQ-R suicide risk (r=.34, p<.01) and greater levels of INQ-TB thwarted belongingness (r=.60, p<.01). Greater levels of INQ-TB thwarted belongingness were also significantly correlated with more severe SBQ-R suicide risk (r=.49, p<.01).
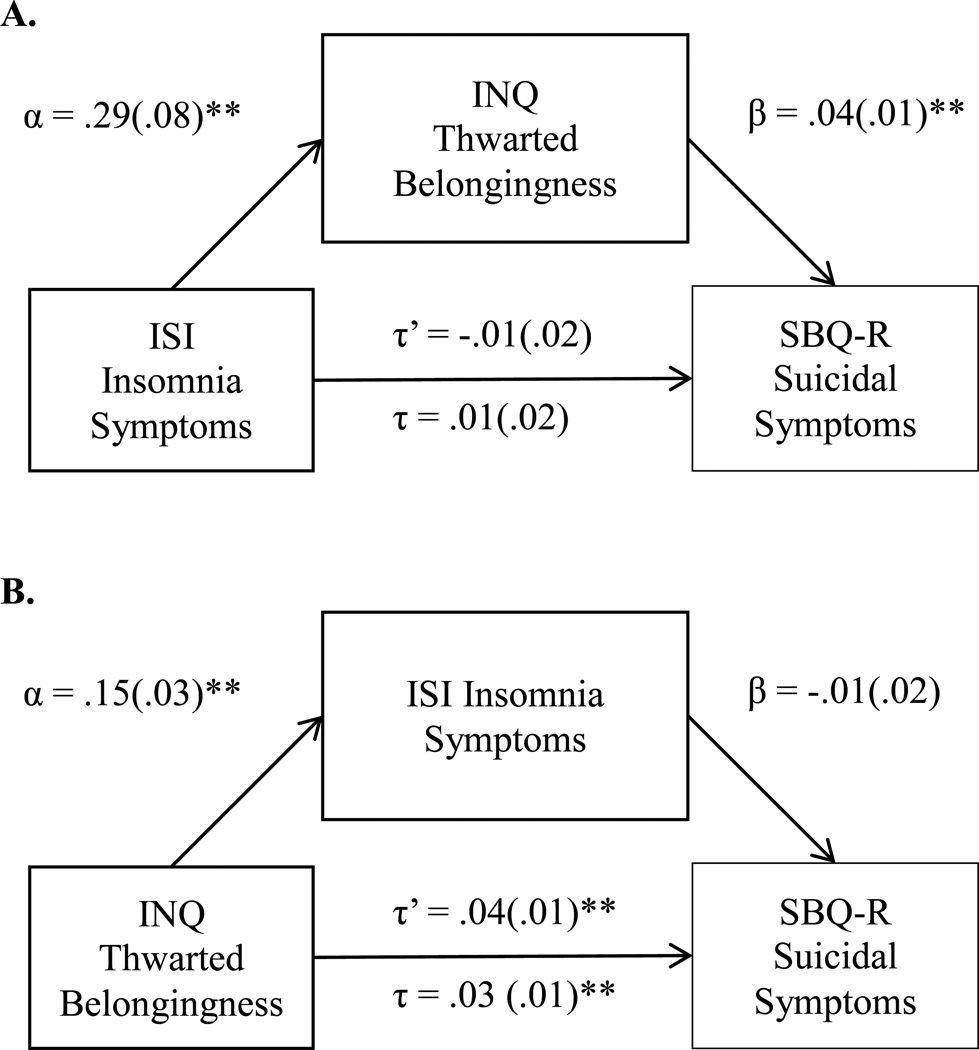
Primary Analyses: Thwarted Belongingness as a Mediator (Figure 3A)
Figure 3.
Study 3 Unstandardized Regression Coefficients and Standard Errors from Mediation Analyses
** p < .01
Note. α = independent variable to mediator path; β = mediator to dependent variable path; τ’ = direct effects of independent variable on dependent variable; τ = total effects of independent variable on dependent variable; ISI = Insomnia Severity Index; INQ = Interpersonal Needs Questionnaire; SBQ-R = Suicidal Behaviors Questionnaire—Revised; Analyses controlling for anxiety symptoms and perceived burdensomeness
The overall regression model was significant (F[4,412]=48.16, p<.01) and explained 31.9% of the variance in suicidal ideation. More severe ISI insomnia symptoms were significantly associated with greater INQ-TB thwarted belongingness (B=.39, SE=.08, p<.01), and INQ-TB thwarted belongingness was significantly associated with more severe SBQ-R suicide risk (B=.04, SE=.01, p<.01). The direct effects of ISI scores on SBQ-R scores were not significant (B=-.01, SE=.02, p=.82); however, the indirect effects of ISI scores on SBQ-R scores through INQ-TB scores was significant (95% CI: .01, .03), indicating an “indirect only” effect. INQ-PB perceived burdensomeness and MHP-P anxiety symptoms were included as covariates in these analyses. When additionally controlling for MHP-P depression symptoms, INQ-TB scores no longer accounted for the association between ISI scores and SBQ-R scores (95% CI: <-.01, .02).
Secondary Analyses: Insomnia Symptoms as a Mediator (Figure 3B)
The overall regression model was significant (F[4,412]=48.16, p<.01) and accounted for 31.9% of the variance in suicidal ideation. Greater INQ-TB thwarted belongingness was significantly associated with more severe ISI insomnia symptoms (B=.15, SE=.03, p<.01), but more severe ISI insomnia symptoms were not significantly associated with more severe SBQ-R suicide risk (B=-.01, SE=.02, p=.82). The direct effects of INQ-TB thwarted belongingness on SBQ-R suicide risk were significant (B=.04, SE=.01, p=.01), but the indirect effects of INQ-TB scores on SBQ-R scores through INQ-TB scores were not (95% CI: -.01, .01). Similarly, we controlled for INQ-PB perceived burdensomeness and MHP-P anxiety symptoms in all of these analyses. When additionally controlling for MHP-P depression symptoms, ISI scores no longer accounted for the relationship between INQ-TB and SBQ-R scores (95% CI: -.01, >.01).
Exploratory Analyses: Effects of Perceived Burdensomeness
The overall regression model with INQ-TB and INQ-PB as parallel mediators, controlling for MHP-P anxiety symptoms, was significant (F[5,408]=39.38, p<.01, R2=.33). Both mediators significantly accounted for the association between ISI and SBQ-R scores (INQ-TB 95% CI: .01, .06; INQ-PB 95% CI: .07, .14); however, neither was identified as exerting a significantly stronger effect (95% CI: -.04, .01). When also controlling for MHP-P depression symptoms, neither INQ-TB (95% CI: >-.01, .01) nor INQ-PB (95% CI: -.01, .02) significantly mediated the relationship between ISI insomnia symptoms and SBQ-R suicide risk. Moderated mediation analyses revealed that INQ-TB served as an explanatory factor in the relationship between ISI insomnia symptoms and DSI-SS suicidal ideation, controlling for MHP-P anxiety symptoms, at low (i.e., −1 SD; 95% CI: .03, .06) but not high (i.e., +1 SD; 95% CI: -.01, .02) levels of INQ-PB. The same pattern of findings was observed when additionally controlling for MHP-P depression symptoms (i.e., at low levels of INQ-PB, 95% CI: <.01, .03; at high levels of INQ-PB, 95% CI: -.01, .01).
Discussion
The primary findings from Study 3 were consistent both with study hypotheses and findings from Studies 1 and 2. These results underscore the explanatory role that thwarted belongingness may play in the relationship between insomnia symptoms and suicide risk. This is consistent with aforementioned experimental findings and theoretical suicide risk frameworks. Similar to Studies 1 and 2, thwarted belongingness significantly accounted for the relationship between insomnia symptoms and suicide risk, controlling for perceived burdensomeness and anxiety symptoms. This finding further emphasizes the potential prominent role of thwarted belongingness in the insomnia-suicide link. However, our pattern of findings no longer emerged after controlling for depression symptoms. It is possible that by removing the variance accounted for by depression symptoms from suicidal ideation, a large portion of what meaningfully defines suicidal ideation was covaried out (Rogers et al., 2016), thereby reducing our ability to detect significant effects. These results may also be a manifestation of the highly overlapping nature of insomnia, depression, and suicidal ideation, further complicated by our use of cross-sectional data and inability to delineate the temporal relationship between these three constructs. Though this study was more methodologically rigorous than Studies 1 and 2 due to use of more psychometrically sound measures, use of objective sleep measures and inclusion of other psychiatric symptoms as covariates (e.g., PTSD symptoms) would enhance the robustness of findings. Replication of this study across more demographically diverse samples is also needed to enhance generalizability, though we were able to replicate our hypothesized pattern of findings even when using an alternate measure of suicidal ideation (i.e., SBQ-R instead of DSI-SS), representing a strength of this investigation.
With regard to exploratory analyses, similar to Study 2, we found that perceived burdensomeness served as a parallel mediator, alongside thwarted belongingness, of the relationship between insomnia symptoms and suicide risk. Collectively, these findings identify perceived burdensomeness as another potential underlying mechanism that warrants further empirical study. In contrast to Study 2, however, thwarted belongingness emerged as an explanatory factor among those with low but not high levels of perceived burdensomeness. Even more strikingly, these moderated mediation results held even when controlling for both anxiety and depression symptoms. It may be, then, that thwarted belongingness specifically explains the relationship between insomnia symptoms and suicide risk when other robust suicide risk factors (i.e., perceived burdensomeness) are less potent. Additional research is needed, though, to replicate this result and better understand the factors that may account for this finding.
General Discussion
Overall, across military service member and veteran samples, more severe insomnia symptoms were significantly associated with more severe suicidal ideation and greater thwarted belongingness. Additionally, across samples, findings revealed that thwarted belongingness significantly accounted for the relationship between insomnia symptom severity and suicidal ideation. However, insomnia symptoms did not conversely appear to explain the relationship between thwarted belongingness and suicidal ideation.
First, our findings are consistent with previous work demonstrating a strong association between insomnia symptoms and thwarted belongingness and prior studies showing that thwarted belongingness may help to account for the relationship between sleep disturbances and suicidal ideation (Chu et al., 2016; Nadorff et al., 2014). As mentioned previously, the repeated experience of wakefulness while most others are asleep and impairments in social functioning resulting from fatigue and irritability—both of which are hallmark symptoms of insomnia (APA, 2013)—are likely to increase feelings of loneliness and social isolation. These effects of sleep deprivation may also make it more difficult for individuals to manage conflict in their interpersonal relationships (i.e., due to diminished executive function and interpreting behavioral intentions), further contributing to a sense of thwarted belongingness. These hypothesized connections are also supported by literature demonstrating that sleep disturbances may contribute to greater difficulties in emotion regulation (Gruber and Cassoff, 2014; Gujar et al., 2011; Kyle et al., 2014; Mauss et al., 2013), poorer mood and negative affect (Baum et al., 2014), and increased reactivity to daily stressors (Minkel et al., 2012; Zohar et al., 2005). Each of these problems likely serves to decrease positive interpersonal connectedness by increasing frequency and severity of negative social interactions, as well as decreasing interest or motivation to engage in social situations. Thus, it is unsurprising that, across samples, sleep problems were associated with thwarted belongingness, and thwarted belongingness significantly accounted for the relationship between insomnia symptoms and suicidal ideation. Strikingly, these effects remained even when controlling for other psychiatric symptoms (e.g., anxiety, hopelessness, perceived burdensomeness), each of which have been shown to be important suicide risk factors (Beck, Brown, & Steer, 1989; Brown, Beck, Steer, & Grisham, 2000; Capron et al., 2012; Joiner et al., 2009), underscoring the significance of these present findings. Of note, these effects did not remain in the one sample for which we were able to control for depression symptoms, but further work—particularly prospective research—is needed to delineate the nature of the relationship between these highly overlapping constructs.
That insomnia symptom severity did not appear to significantly account for the association between thwarted belongingness and suicidal ideation is also noteworthy. This finding reveals the potential specificity of thwarted belongingness as an explanatory link in the relationship between sleep disturbances and suicidal ideation among service members and veterans. That is, poor sleep appears to be related to suicide risk in part because it may contribute to feelings of social disconnection. Social disconnection and sleep problems have been associated in with each other in this and other investigations (Cacioppo et al., 2002; Hawkley and Cacioppo, 2010), and it appears that their relationship to suicide risk is specific to thwarted belongingness as a link between insomnia and suicidal ideation.
It is also notable that the same pattern of findings held in all three of our studies. Given the variation across samples with regard to military status, branch of service, and demographics, this consistency bolsters evidence for our hypothesis that insomnia may confer risk for suicide among military service members and veterans by increasing feelings of loneliness and social disconnection. Additionally, the correspondence between our findings and aforementioned similar studies with non-military samples (Chu et al., 2016; Nadorff et al., 2014) suggests that pathways between insomnia symptoms, thwarted belongingness, and suicidal ideation may be relatively similar across populations, and indicates that similar prevention and intervention approaches can be utilized across vulnerable groups to thwart the trajectory from insomnia to suicidal ideation.
Finally, on this point, our results suggest that sleep disturbances and thwarted belongingness may be important therapeutic targets to reduce suicide risk among military service members and veterans. Fortunately, efficacious interventions, such as cognitive-behavioral therapy for insomnia (CBT-I; Edinger & Means, 2005), exist to treat insomnia. In addition to being effective in addressing insomnia complaints (Edinger et al., 2009, 2001; Koffel et al., 2015), studies also suggest that CBT-I reduces symptoms of depression and suicidality in the general population (Manber et al., 2011, 2008) and veterans (Trockel et al., 2015). Furthermore, since sleep problems appear to predict soldiers’ treatment engagement above and beyond other psychiatric symptoms (e.g., suicidal ideation, hopelessness; Hom et al., 2016), a focus on assessing and treating insomnia may represent a strategic suicide prevention approach among service members. Findings from our study also indicate that assessment of loneliness, social isolation, and social connectedness, particularly among service members and veterans with sleep problems, may be clinically useful. Routine assessment and monitoring of thwarted belongingness can critically inform suicide risk level categorizations and reveal potential areas for problem-solving, development of coping skills, restructuring of negative thoughts, and behavioral activation techniques (e.g., developing interpersonal effectiveness skills, scheduling social activities; see Joiner, Van Orden, Witte, & Rudd, 2009 as a guide). This may, in turn, reduce suicide risk and mitigate the impact of sleep disturbances on suicidal ideation.
Limitations and Future Directions
This investigation’s limitations should also be considered. First, since only cross-sectional data were collected, we were unable to investigate causal relationships between variables of interest. Future prospective studies will be critical in evaluating these relationships. However, our analyses were grounded in prior theoretical and empirical findings, and we were able to test an alternate model. Second, further work is indicated to replicate study findings in more demographically diverse samples. Such investigations may also be enhanced by the collection of additional military service information (e.g., years of service; deployment characteristics) to examine the factors moderating the relationships between constructs of interest. Third, as noted above, only self-report data was utilized. Implicit measures of suicidal ideation (e.g., Nock et al., 2010) and objective sleep disturbance measures (e.g., polysomnography) may help circumvent stigma concerns and inaccurate reporting in future studies. Abbreviated self-report measures were also used in a number of cases, which may have impacted our findings by reducing our ability to detect significant effects and yielding relatively low correlations in some instances. Though these abbreviated versions have demonstrated preliminary reliability and validity (Gutierrez and Joiner, 2016), use of full-length, robustly validated measures is indicated for replication studies. Last, we were limited in available symptom measures; thus, it may be useful for future studies to control for other psychiatric symptoms often associated with sleep disturbances and suicidal ideation (e.g., PTSD; APA, 2013). There were also some symptom measures (e.g., depression symptoms) that were not available across all samples. Consequently, research is needed to replicate our results and resolve equivocal findings (e.g., moderated mediation results). On this point, factors other than thwarted belongingness may help to explain the relationship between insomnia and suicidal ideation (e.g., overarousal; Ribeiro et al., 2012; Ribeiro et al., 2014). Thus, further research is warranted to identify other mechanisms that might account for the strong association between insomnia and suicide risk, including further probing perceived burdensomeness as an explanatory link.
Conclusions
Although prior work has established a robust association between insomnia and suicide risk, as well as between thwarted belongingness and suicide risk, this three-study investigation represents the first evaluation of these constructs among military service members and veterans within a single model. Although further, prospective studies are needed to investigate these associations in additional, diverse military and veteran samples, and with more rigorous measurement techniques, our results are an important first step in understanding the role of thwarted belongingness as a link between insomnia symptom severity and suicidal ideation in military service member and veteran populations, and reveal potential avenues for future research and suicide prevention efforts.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Bastien CH, Vallieres A, Morin CM, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Batterham P, Ftanou M, Pirkis J, Brewer J, Mackinnon A, Beautrais A, Fairweather-Schmidt A, Christensen H. A systematic review and evaluation of measures for suicidal ideation and behaviors in population-based research. Psychol. Assess. 2014;27:501–512. doi: 10.1037/pas0000053. [DOI] [PubMed] [Google Scholar]
- Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J. Child Psychol. Psychiatry. 2014;55:180–190. doi: 10.1111/jcpp.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. Hopelessness as a predictor of eventual suicide. Ann. N. Y. Acad. Sci. 1986;487:90–96. doi: 10.1111/j.1749-6632.1986.tb27888.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. J. Consult. Clin. Psychol. 1989;57:309–310. doi: 10.1037//0022-006x.57.2.309. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: A 10-year prospective study of patients hospitalized with suicidal ideation. Am. J. Psychiatry. 1985;142:559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J. Consult. Clin. Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr. Psychiatry Rep. 2015;17:1–9. doi: 10.1007/s11920-015-0554-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Turvey CL, Conwell Y, Joiner TE. Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: A longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71:1129–1137. doi: 10.1001/jamapsychiatry.2014.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown G, Beck A, Steer R, Grisham J. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J. Consult. Clin. Psychol. 2000;68:371–377. [PubMed] [Google Scholar]
- Bryan CJ, Morrow CE, Anestis MD, Joiner TE. A preliminary test of the interpersonal-psychological theory of suicidal behavior in a military sample. Pers. Individ. Dif. 2010;48:347–350. [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, Hobson JA. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychol. Sci. 2002;13:384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Capaldi VF, Guerrero ML, Killgore WDS. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil. Med. 2011;176:879–888. doi: 10.7205/milmed-d-10-00440. [DOI] [PubMed] [Google Scholar]
- Capron DW, Fitch K, Medley A, Blagg C, Mallott M, Joiner T. Role of anxiety sensitivity subfactors in suicidal ideation and suicide attempt history. Depress. Anxiety. 2012;29:195–201. doi: 10.1002/da.20871. [DOI] [PubMed] [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: A systematic review. Psychol. Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Christensen H, Batterham PJ, Soubelet A, Mackinnon AJ. A test of the Interpersonal Theory of Suicide in a large community-based cohort. J. Affect. Disord. 2013;144:225–234. doi: 10.1016/j.jad.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Chu C, Hom MA, Rogers ML, Ringer FB, Hames JL, Suh S, Joiner TE. Is insomnia lonely? Exploring thwarted belongingness as an explanatory link between insomnia and suicidal ideation in a sample of South Korean university students. J. Clin. Sleep Med. 2016 doi: 10.5664/jcsm.5784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Hom MA, Rogers ML, Stanley IH, Ringer-Moberg FB, Podlogar MC, Hirsch JK, Joiner TE. Insomnia and suicide-related behaviors: A multi-study investigation of thwarted belongingness as a distinct explanatory factor. J. Affect. Disord. doi: 10.1016/j.jad.2016.08.065. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukrowicz KC, Cheavens JS, Van Orden KA, Ragain RM, Cook RL. Perceived burdensomeness and suicide ideation in older adults. Psychol. Aging. 2011;26:331–338. doi: 10.1037/a0021836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukrowicz KC, Jahn DR, Graham RD, Poindexter EK, Williams RB. Suicide risk in older adults: Evaluating models of risk and predicting excess zeros in a primary care sample. J. Abnorm. Psychol. 2013;122:1021–1030. doi: 10.1037/a0034953. [DOI] [PubMed] [Google Scholar]
- Czyz EK, Berona J, King CA. A prospective examination of the Interpersonal-Psychological Theory of Suicidal Behavior among psychiatric adolescent inpatients. Suicide Life Threat. Behav. 2014 doi: 10.1111/sltb.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs Office of Public and Intergovernmental Affairs. VA conducts nation’s largest analysis of veteran suicide. Washington, D.C: 2016. [Google Scholar]
- Edinger JD, Means MK. Cognitive-behavioral therapy for primary insomnia. Clin. Psychol. Rev. 2005;25:539–558. doi: 10.1016/j.cpr.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Olsen MK, Stechuchak KM, Means MK, Lineberger MD, Kirby A, Carney CE. Cognitive behavioral therapy for patients with primary insomnia or insomnia associated predominantly with mixed psychiatric disorders: a randomized clinical trial. Sleep. 2009;32:499–510. doi: 10.1093/sleep/32.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia: a randomized controlled trial. JAMA. 2001;285:1856–1864. doi: 10.1001/jama.285.14.1856. [DOI] [PubMed] [Google Scholar]
- Golding S, Nadorff MR, Winer ES, Ward KC. Unpacking sleep and suicide in older adults in a combined online sample. J. Clin. Sleep Med. 2015;11:1385–1392. doi: 10.5664/jcsm.5270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J. Consult. Clin. Psychol. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R, Cassoff J. The interplay between sleep and emotion regulation: Conceptual framework empirical evidence and future directions. Curr. Psychiatry Rep. 2014;16:500. doi: 10.1007/s11920-014-0500-x. [DOI] [PubMed] [Google Scholar]
- Gujar N, Yoo SS, Hu P, Walker MP. Sleep deprivation amplifies reactivity of brain reward networks, biasing the appraisal of positive emotional experiences. J. Neurosci. 2011;31:4466–4474. doi: 10.1523/JNEUROSCI.3220-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez PM, Joiner TE. The Military Suicide Research Consortium Common Data Elements: Psychometric support, clinical, and research utility. Orlando/Kissimmee, FL: Military Health System Research Symposium (MHSRS); 2016. [Google Scholar]
- Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendin H, Maltsberger JT, Szanto K. The role of intense affective states in signaling a suicide crisis. J. Nerv. Ment. Dis. 2007;195:363–368. doi: 10.1097/NMD.0b013e318052264d. [DOI] [PubMed] [Google Scholar]
- Hill RM, Rey Y, Marin CE, Sharp C, Green KL, Pettit JW. Evaluating the Interpersonal Needs Questionnaire: Comparison of the reliability, factor structure, and predictive validity across five versions. Suicide Life Threat. Behav. 2015;45:302–314. doi: 10.1111/sltb.12129. [DOI] [PubMed] [Google Scholar]
- Hom MA, Lim IC, Stanley IH, Chiurliza B, Podlogar MC, Michaels MS, Buchman-Schmitt JM, Silva C, Ribeiro JD, Joiner TE. Insomnia brings soldiers into mental health treatment, predicts treatment engagement, and outperforms other suicide-related symptoms as a predictor of major depressive episodes. J. Psychiatr. Res. 2016;79:108–115. doi: 10.1016/j.jpsychires.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahn DR, Cukrowicz KC, Linton K, Prabhu F. The mediating effect of perceived burdensomeness on the relation between depressive symptoms and suicide ideation in a community sample of older adults. Aging Ment. Health. 2011;15:214–220. doi: 10.1080/13607863.2010.501064. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J. Psychiatr. Res. 2006;40:700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, Rudd MD. Main predictions of the interpersonal-psychological theory of suicidal behavior: empirical tests in two samples of young adults. J. Abnorm. Psychol. 2009;118:634–646. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Jr, Van Orden KA, Witte TK, Rudd MD. The interpersonal theory of suicide: Guidance for working with suicidal clients. Washington, D.C: American Psychological Association; 2009. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why People Die by Suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Joiner TE, Pfaff JJ, Acres JG. A brief screening tool for suicidal ideation in adolescents and young adults in general health settings: Reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behav. Res. Ther. 2002;40:471–481. doi: 10.1016/s0005-7967(01)00017-1. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Van Orden KA. The Interpersonal-Psychological Theory of Suicidal Behavior indicates specific and crucial psychotherapeutic targets. Int. J. Cogn. Ther. 2008;1:80–89. [Google Scholar]
- Klonsky ED, Kotov R, Bakst S, Rabinowitz J, Bromet EJ. Hopelessness as a predictor of attempted suicide among first admission patients with psychosis: a 10-year cohort study. Suicide Life. Threat. Behav. 2012;42:1–10. doi: 10.1111/j.1943-278X.2011.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodaka M, Matsumoto T, Katsumata Y, Akazawa M, Tachimori H, Kawakami N, Eguchi N, Shirakawa N, Takeshima T. Suicide risk among individuals with sleep disturbances in Japan: a case-control psychological autopsy study. Sleep Med. 2014;15:430–435. doi: 10.1016/j.sleep.2013.11.789. [DOI] [PubMed] [Google Scholar]
- Koffel E, Koffel J, Gehrman P. A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Med. Rev. 2015;19C:6–16. doi: 10.1016/j.smrv.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Koslowe P, Roy M. Symptoms in 18,495 Persian Gulf War veterans. Latency of onset and lack of association with self-reported exposures. J. Occup. Environ. Med. 1998;40:520–528. doi: 10.1097/00043764-199806000-00004. [DOI] [PubMed] [Google Scholar]
- Kuehn BM. Soldier suicide rates continue to rise: Military, scientists work to stem the tide. JAMA. 2009;301:1111–1113. doi: 10.1001/jama.2009.342. [DOI] [PubMed] [Google Scholar]
- Kyle SD, Beattie L, Spiegelhalder K, Rogers Z, Espie CA. Altered emotion perception in insomnia disorder. Sleep. 2014;37:775–783. doi: 10.5665/sleep.3588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, Hooper TI, Gackstetter GD, Ghamsary M, Hoge CW. Risk factors associated with suicide in current and former US military personnel. JAMA. 2013;310:496–506. doi: 10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- Lewis V, Creamer M, Failla S. Is poor sleep in veterans a function of post-traumatic stress disorder? Mil. Med. 2009;174:948–951. doi: 10.7205/milmed-d-04-0208. [DOI] [PubMed] [Google Scholar]
- Manber R, Bernert RA, Suh S, Nowakowski S, Siebern AT, Ong JC. CBT for insomnia in patients with high and low depressive symptom severity: Adherence and clinical outcomes. J. Clin. Sleep Med. 2011;7:645–652. doi: 10.5664/jcsm.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manber R, Edinger JDE, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauss IB, Troy AS, LeBourgeois MK. Poorer sleep quality is associated with lower emotion-regulation ability in a laboratory paradigm. Cogn. Emot. 2013;27:567–576. doi: 10.1080/02699931.2012.727783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metalsky GI, Joiner TEJ. The Hopelessness Depression Symptom Questionnaire. Cognit. Ther. Res. 1997;21:359–384. [Google Scholar]
- Miller NL, Shattuck LG, Matsangas P. Sleep and fatigue issues in continuous operations: A survey of U.S. Army officers. Behav. Sleep Med. 2011;9:53–65. doi: 10.1080/15402002.2011.533994. [DOI] [PubMed] [Google Scholar]
- Minkel JD, Banks S, Htaik O, Moreta MC, Jones CW, McGlinchey EL, Simpson NS, Dinges DF. Sleep deprivation and stressors: Evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion. 2012;12:1015–1020. doi: 10.1037/a0026871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, Belleville G, Bélanger L, Ivers H, Belanger L, Ivers H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadorff MR, Anestis MD, Nazem S, Harris HC, Winer ES. Sleep disorders and the interpersonal-psychological theory of suicide: Independent pathways to suicidality? J. Affect. Disord. 2014;152-154:505–512. doi: 10.1016/j.jad.2013.10.011. [DOI] [PubMed] [Google Scholar]
- Neylan TC, Marmar CR, Metzler TJ, Weiss DS, Zatzick DF, Delucchi KL, Wu RM, Schoenfeld FB. Sleep disturbances in the Vietnam generation: Findings from a nationally representative sample of male Vietnam veterans. Am. J. Psychiatry. 1998;155:929–933. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the suicidal mind: Implicit cognition predicts suicidal behavior. Psychol. Sci. 2010;21:511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS, Hwang I, Naifeh JA, Sampson NA, Schoenbaum M, Zaslavsky AM, Kessler RC. Prevalence and correlates of suicidal behavior among soldiers: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014;71:514–522. doi: 10.1001/jamapsychiatry.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Ursano RJ, Heeringa SG, Stein MB, Jain S, Raman R, X S, Chiu WT, Colpe LJ, Fullerton CS, Gilman SE, Hwang I, Naifeh JA, Roselini AJ, Sampson NA, Schoenbaum M, Zaslavsky AM, Kessler RC, the Army STARRS Collaborators. Sun X, Chiu WT, Colpe LJ, Fullerton CS, Gilman SE, Hwang I, Naifeh JA, Rosellini A, Sampson NA, Schoenbaum M, Zaslavsky AM, Kessler RC. Mental disorders, comorbidity, and pre-enlistment suicidal behavior among new soldiers in the U.S. Army: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Suicide Life Threat. Behav. 2015 doi: 10.1111/sltb.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment. 2001;8:443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil. Med. 2008;173:230–235. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Britton PC, Ilgen MA, Chapman B, Conner KR. Sleep disturbance preceding suicide among veterans. Am. J. Public Health. 2012a;(102 Suppl):S93–S97. doi: 10.2105/AJPH.2011.300470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry. 2012b;73:e1160–e1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Acosta J, Burns RM, Jaycox LH, Pernin CG. The war within: Preventing suicide in the U.S. military. Arlington, VA: 2011. [PMC free article] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav. Res. Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Bender TW, Buchman JM, Nock MK, Rudd MD, Bryan CJ, Lim IC, Baker MT, Knight C, Gutierrez PM, Joiner TE. An investigation of the interactive effects of the capability for suicide and acute agitation on suicidality in a military sample. Depress. Anxiety. 2015;32:25–31. doi: 10.1002/da.22240. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, Joiner TE., Jr Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J. Affect. Disord. 2012;136:743–750. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Silva C, Joiner TE. Overarousal interacts with a sense of fearlessness about death to predict suicide risk in a sample of clinical outpatients. Psychiatry Res. 2014;218:106–112. doi: 10.1016/j.psychres.2014.03.036. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Duong HT. Depression and insomnia among adolescents: A prospective perspective. J. Affect. Disord. 2013;148:66–71. doi: 10.1016/j.jad.2012.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Chen IG. Functioning of adolescents with symptoms of disturbed sleep. J. Youth Adolesc. 2001;30:1–18. [Google Scholar]
- Rogers ML, Stanley IH, Hom MA, Chiurliza B, Podlogar MC, Joiner TE. Conceptual and empirical scrutiny of covarying depression out of suicidal ideation. Assessment. 2016 doi: 10.1177/1073191116645907. [DOI] [PubMed] [Google Scholar]
- Ruehlman LS, Lanyon RI, Karoly P. Development and validation of the multidimensional health profile, part I: Psychosocial functioning. Psychol. Assess. 1999;11:166–176. doi: 10.1037/1040-3590.11.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 2000;23:243–308. [PubMed] [Google Scholar]
- Seelig AD, Jacobson IG, Smith B, Hooper TI, Boyko EJ, Gackstetter GD, Gehrman P, Macera CA, Smith TC. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–1622. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Med. Rev. 2014;18:75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Steed L. Further validity and reliability evidence for Beck Hopelessness Scale scores in a nonclinical sample. Educ. Psychol. Meas. 2001;61:303–316. [Google Scholar]
- Trockel M, Karlin BE, Taylor CB, Brown GK, Manber R. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38:259–265. doi: 10.5665/sleep.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursano RJ, Heeringa SG, Stein MB, Jain S, Raman R, Sun X, Chiu WT, Colpe LJ, Fullerton CS, Gilman SE, Hwang I, Naifeh JA, Nock MK, Rosellini AJ, Sampson NA, Schoenbaum M, Zaslavsky AM, Kessler RC. Prevalence and correlates of suicidal behavior among new soldiers in the U.S. Army: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Depress. Anxiety. 2015a;32:3–12. doi: 10.1002/da.22317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursano RJ, Kessler RC, Stein MB, Naifeh JA, Aliaga PA, Fullerton CS, Sampson NA, Kao TC, Colpe LJ, Schoenbaum M, Cox KL, Heeringa SG. Suicide attempts in the US Army during the wars in Afghanistan and Iraq, 2004 to 2009. JAMA Psychiatry. 2015b;72:917–926. doi: 10.1001/jamapsychiatry.2015.0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE. Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol. Assess. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol. Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J. Consult. Clin. Psychol. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Walker MP. The role of sleep in cognition and emotion. Ann. N. Y. Acad. Sci. 2009;1156:168–197. doi: 10.1111/j.1749-6632.2009.04416.x. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J. Psychiatr. Res. 2012;46:953–959. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J. Psychiatr. Res. 2011;45:505–511. doi: 10.1016/j.jpsychires.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woosley JA, Lichstein KL, Taylor DJ, Riedel BW, Bush AJ. Hopelessness mediates the relation between insomnia and suicidal ideation. J. Clin. Sleep Med. 2014;10:1223–1230. doi: 10.5664/jcsm.4208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zohar D, Tzischinsky O, Epstein R, Lavie P. The effects of sleep loss on medical residents’ emotional reactions to work events: A cognitive-energy model. Sleep. 2005;28:47–54. doi: 10.1093/sleep/28.1.47. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Goodie JL, McNeil DW, Sperry JA, Sorrell JT. Anxiety sensitivity in the prediction of pain-related fear and anxiety in a heterogeneous chronic pain population. Behav. Res. Ther. 2001;39:683–696. doi: 10.1016/s0005-7967(00)00049-8. [DOI] [PubMed] [Google Scholar]