Abstract
Background
Distress intolerance (DI) is conceptualized as an individual difference reflective of the ability to tolerate aversive psychological states. Although high DI has demonstrated cross-sectional associations with multiple forms of psychopathology, few studies have tested key facets of its theoretical conceptualization. Specifically, little research has been conducted on DI's theorized role as an incrementally valid prospective moderator of the relationship between daily stressful events and affective symptoms reflective of preoccupation with aversive internal (e.g., depression, worry) rather than external stimuli (e.g., social anxiety).
Method
A non-clinical sample (N = 147; 77% female; M age = 19.32) in which high DI individuals were oversampled was recruited. Participants completed baseline measures of DI and trait negative affect followed by six diary entries over a two-week period in which participants reported on daily stressors, negative affect, worry, depressive, and social anxiety symptoms.
Results
Hierarchical linear models revealed that DI positively predicted depressive and worry, but not social anxiety symptoms, independent of daily stressors and negative affect. Further, a significant interaction effect was found such that the positive association between daily stressor(s) occurrence and daily worry was significant at high, but not low DI, and a similar trend-level interaction effect was observed for depressive symptoms. The interaction for social anxiety symptoms was non-significant
Limitations
Utilization of a non-clinical sample precludes generalization of results to clinical samples. Only self-reported DI was assessed, limiting conclusions to perceived as opposed to behaviorally-indexed DI.
Conclusions
Results largely supported DI's theoretical conceptualization as an incrementally valid moderator of stress responding with relevance to particular affective symptoms.
Keywords: Distress intolerance, Worry, Depression, Social anxiety, Longitudinal
1. Introduction
Research on psychopathology etiology has shifted from focusing on identifying risk factors for individual conditions to identifying transdiagnostic risk factors that span multiple psychological conditions (Insel et al., 2010; Krueger and Eaton, 2015). Distress intolerance (DI), conceptualized as an individual difference variable that increases individuals' propensity to negatively appraise and respond avoidantly to acute negative affect (Leyro et al., 2010), has been identified as an important transdiagnostic risk factor. DI has been theoretically posited and empirically supported as a risk factor for multiple psychopathological conditions, including mood and anxiety, substance use, and personality disorders (Allan et al., 2014; Corstorphine et al., 2007; Gratz et al., 2006; Leyro et al., 2010). Further, these relations appear to be robust to the influence of trait neuroticism/negative affect (NA) on psychopathology (e.g., Cougle et al., 2011; Keough et al., 2010).
Extant research on DI has primarily relied on cross-sectional designs. These data provide strong evidence of a positive association between DI and symptoms of psychopathology in nonclinical and clinical samples (Allan et al., 2014, 2015; Bujarski et al., 2012; Cougle et al., 2011; Ellis et al., 2013; Keough et al., 2010). Although important, these studies are limited in their ability to test important aspects of DI's theoretical conceptualization. Specifically, DI is conceptualized as an individual difference variable that moderates the response to acute distress rather than being redundant with negative affect itself (Leyro et al., 2010). Some cross-sectional work has found associations between DI and symptoms of various forms of psychopathology independent of trait negative affect and current distress (Cougle et al., 2011; Keough et al., 2010), but studies are needed to test DI's theorized role as a prospective predictor of maladaptive responding to acute stressors above and beyond trait/state negative affect. Studies of this kind would provide empirical support for the notion of DI as an important individual difference moderator of response to acute distress rather than an artifact of negative emotional reactivity.
Few studies have explicitly tested DI's theorized role as a moderator of acute stress responding, though some empirical support has been found in recent laboratory investigations (Norberg et al., 2015; Shaw and Timpano, 2016). Both Norberg et al. (2015) and Shaw and Timpano (2016) found DI to predict hoarding-relevant behavior after laboratory-induced stress, but not in a neutral condition. However, these studies utilized laboratory mood induction procedures, precluding the possibility of testing DI's prospective role as a moderator of response to ecologically valid stressors. Two existing prospective studies utilizing daily diary methodology found significant, positive associations between DI and daily intrusive cognition independent of trait negative affect (Macatee et al., 2015, 2013), but in only one of these studies was DI found to significantly moderate the effect of daily stressors on daily symptoms (Macatee et al., 2013). To summarize, preliminary laboratory and prospective data support DI's theorized role as a moderator of response to acute stress, though extant prospective data is mixed, suggesting the need for more investigation of this aspect of DI's conceptualization.
Among mood and anxiety symptoms, accumulating data suggests that DI is less robustly associated with symptoms of social anxiety and compulsive behavior relative to worry, obsessions, and depressive symptoms (Cougle et al., 2011, 2012, 2013; Keough et al., 2010; Macatee et al., 2013, 2015; Magidson et al., 2013; Norr et al., 2013). Both social anxiety and compulsions (e.g., washing/ checking behavior) are characterized by specific, external situations (i.e., social situations, contact with contaminants) that elicit anxiety and avoidance. Further, such situations are generally avoided primarily to prevent specific feared outcomes rather than reduce the incidental negative emotional arousal (McKay et al., 2004; Moscovitch, 2009). In contrast, generalized worry and obsessional symptoms are thought to be primarily driven by avoidance of aversive internal stimuli rather than specific external situations and their associated feared outcomes (Borkovec et al., 2004; Newman and Llera, 2011; Rachman, 1997). Similarly, behavioral (e.g., social withdrawal) and cognitive (e.g., rumination) characteristics of depression are thought to function as attempts to reduce aversive internal stimuli (e.g., low mood) (Giorgio et al., 2010; Jacobson et al., 2001). Thus, individuals with high DI may be more likely to respond to stressor-elicited increases in negative emotional arousal with behavior primarily focused on escape from the unpleasant affect as opposed to behavior focused on avoidance of a specific feared outcome. Although these data are suggestive of DI's specificity to psychopathology symptoms in which aversive internal rather than external stimuli are central, extant work is limited in that few studies have prospectively examined DI's theorized role as a moderator of response to acute stressors across multiple types of mood/anxiety symptoms.
To summarize, a large body of literature has consistently demonstrated positive associations between DI and a broad array of psychopathology, but few studies have explicitly tested important aspects of DI's theoretical conceptualization (Leyro et al., 2010). First, most research has examined DI/psychopathology associations using cross-sectional designs. Prospective studies in which daily-level stressors and symptoms of psychopathology are assessed are needed to test DI's theorized role as an incrementally valid moderator of response to acute stressors independent of more parsimonious constructs. Specifically, it needs to be shown that poor tolerance of distress moderates the effect of acute stressors on symptoms above and beyond the general tendency to experience negative emotions (i.e., trait negative affect) and daily negative emotional reactivity (i.e., state negative affect). Second, few studies have tested theoretically-driven hypotheses regarding DI's specificity with particular psychopathology symptom types. Studies are needed in which DI's theorized role as a moderator of stressor responding is tested with respect to psychopathology symptoms that vary in the centrality of avoidance of aversive internal versus external stimuli.
To address these limitations, daily diary methodology was used to test the theorized role of DI as a moderator of response to acute stress independent of trait and state negative affect across a two-week period. Daily social anxiety, worry, and depressive symptoms were assessed to test DI's expected differential relationship across symptoms that primarily reflect preoccupation with aversive internal versus external stimuli. These specific symptoms were chosen due to their high co-occurrence (Brown et al., 2001), providing a particularly stringent test of DI's hypothesized differential relationship across symptom types. We predicted that baseline DI, but not trait negative affect, would interact with the occurrence of an acute stressor(s) such that higher DI would predict greater daily depressive/worry symptoms on days in which stressors occurred above and beyond the effects of negative emotional reactivity, but would be unrelated to social anxiety symptoms.
2. Method
2.1. Participants
To test the present study's hypotheses, a non-clinical sample recruited as part of a larger study on DI and emotional information processing was utilized. However, note that the results reported herein have not been published or submitted elsewhere. The sample was recruited from the undergraduate psychology student population at a large southeastern university (N = 165; 77% female; M age = 19.32, SD = 1.96) over three semesters. Participants earned course credit for completing the study. The sample was predominantly Caucasian (70.9%), although other ethnicities were also represented (Hispanic: 13.3%, African-American: 11.5%, Asian: 1.2%, American Indian or Alaskan Native: 0.6%, Other: 2.4%).
3. Measures
3.1. Baseline measures
3.1.1. Distress intolerance
The Distress Intolerance Index (DII; McHugh and Otto, 2012) is a 10-item self-report measure designed to assess an individual's perceived ability to tolerate distressing affective states (e.g., “I can't handle feeling distressed or upset”). The DII is composed of the items from three DI measures (i.e., Distress Tolerance Scale; Simons and Gaher, 2005; Anxiety Sensitivity Index; Peterson and Reiss, 1992; Frustration-Discomfort Scale; Harrington, 2005) that consistently demonstrated the strongest loadings on a latent DI factor across three samples (McHugh and Otto, 2012). Items are scored on a 5-point Likert-type scale ranging from 0 (very little) to 4 (very much) such that higher scores indicate less perceived ability to tolerate distressing states (M = 10.01, SD = 8.73). The DII has demonstrated good test-retest reliability (Cakir, 2016) and strong internal consistency across multiple studies (Cakir, 2016; McHugh and Otto, 2011; Szuhany and Otto, 2015). Most importantly, the DII has demonstrated superior convergent validity with behavioral measures of DI relative to other tolerance measures (McHugh and Otto, 2011; McHugh et al., 2016; Seo and Kwon, 2016; Szuhany and Otto, 2015). In the current study, the DII demonstrated excellent internal consistency (α =.94).
3.1.2. Trait negative affect
Trait Negative Affect (NA) was indexed using the 10-item NA subscale of the Positive and Negative Affect Schedule-Expanded Form (PANAS-X; Watson and Clark, 1999). Respondents are asked to read various words describing negative emotions (e.g., “Upset,” “Nervous”) and indicate the extent to which they generally feel that way using a 5-point Liker-type scale ranging from 1 (Very slightly or not at all) to 5 (Extremely) (M = 19.13, SD = 7.85). Previous research has demonstrated acceptable internal consistency, temporal reliability, and convergent validity for the PANAS-NA (Watson and Clark, 1999). In the current study, the PA-NAS-NA demonstrated excellent internal consistency (α =.90).
3.2. Daily measures
3.2.1. Daily stressful events
Participants completed a self-report version of the Daily Inventory of Stressful Events (DISE; Almeida et al., 2002) to assess the occurrence of specific types of stressors that had occurred that day. Almeida and colleagues (2002) used seven stem questions reflecting broad categories of stressor types derived from a nationally representative sample. Interrater agreement on stressor classification was high (κ =.66 −.95) and daily stressors demonstrated small associations with daily distress (rs =.02 −.31), suggesting that stressor occurrence using these categories is not redundant with negative affect. Participants responded to seven yes/no questions based on Almeida and colleague's (2002) classifications regarding different sorts of stressors that may have occurred throughout the day, including arguments, potential arguments that were let go to avoid disagreement, work/school stress, home stress, discrimination events, friend/relative stress, and stressors not captured by the other categories. A dichotomous daily stressor variable was created to indicate the presence (i.e., at least one or more stressors) or absence of stressful life events for a particular day. Greater endorsement of daily stressors has been significantly associated with established, validated measures of stressful events in prior work (Macatee et al., 2015), suggestive of convergent validity. In the current study, endorsed stressors averaged across all seven categories were rated as moderately stressful based on a 1 (‘Not at all Stressful’) to 4 (‘Very Stressful’) scale (M = 2.57, SD = 0.88), providing evidence that the DISE events in the current study were perceived as stressful. Amongst all of the daily diary entries completed in the current study (n = 627), 55.5% indicated that they had experienced at least one stressful event that day.
3.2.2. Daily worry symptoms
A three-item version of the Penn State Worry Questionnaire (PSWQ; Berle et al., 2011) was employed to assess daily worry on a 1 (‘Not at all typical of me today’) to 5 (‘Very typical of me today’) scale (M = 4.90, SD = 2.96). Berle and colleagues (2011) showed that the brief version of the PSWQ had convergent/discriminant validity and internal consistency (α =.85) comparable to the standard PSWQ. In the current sample, the brief PSWQ demonstrated excellent internal consistency (α =.92).
3.2.3. Daily depressive symptoms
The Mood and Anxiety Symptom Questionnaire – General Distress-Depression subscale (MASQ-GDD; Wardenaar et al., 2010) is a 12-item questionnaire that was used to assess for daily symptoms of depression. Respondents are asked to rate the extent to which they experienced each symptom on a 5-point Likert type scale ranging from 1 (not at all) to 5 (extremely) (M = 19.76. SD = 10.19). For the current study, wording regarding the experience of symptoms in the past week was altered to reflect experience of symptoms that day to index daily symptoms of depression. The MASQ-GDD has shown adequate convergent and discriminant validity as well as good internal consistency in previous studies (Wardenaar et al., 2010). To assess convergent/discriminant validity of the modified MASQ-GDD used in the present study, between-person variance in daily MASQ-GDD scores attributable to baseline MASQ-GDD scores was calculated by transforming t-values into correlation coefficients (Bryk and Raudenbush, 1992, p. 65). Analyses revealed a positive association between baseline MASQ-GDD scores and daily MASQ-GDD scores, r =.51, B =.53, SE =.07, t(145) = 7.21, p < 0.001, that remained significant, r =.41, B =.41, SE =.08, t(144) = 5.45, p <..01, after controlling for baseline PANAS-NA scores, r =.22, B =.25, SE =.09, t(144) = 2.67, p =.008, results suggestive of validity. In the current study, the MASQ-GDD demonstrated excellent internal consistency (α =.96).
3.2.4. Daily social anxiety symptoms
The State Social Anxiety (SSA; Kashdan and Steger, 2006) measure is a 7-item questionnaire that was used to assess daily symptoms of social anxiety. Respondents are asked to indicate the extent to which they experienced each symptom that day on a 5-point Likert-type scale ranging from 1 (very slightly/not at all) to 5 (extremely) (M = 11.53. SD = 6.10). The SSA has been used in prior daily diary studies and has demonstrated excellent reliability as well as convergent/discriminant validity (Kashdan and Steger, 2006). In the current study, the SSA demonstrated excellent internal consistency (α =.94).
3.2.5. Daily negative affect
The NA subscale of the short form of the PANAS was used to measure daily NA in the present study (PANAS-NA; Mackinnon et al., 1999). The PANAS has been used to index emotional reactivity in prior investigations (Sloan, 2004) and the short form of the PANAS has been shown to have good internal consistency (α =.87; Mackinnon et al., 1999) and validity (Gyollai et al., 2011). Further, the NA subscale has been used to index daily negative emotionality in prior longitudinal studies (Hawkins et al., 2013; Macatee et al., 2015). The NA subscale is composed of five negative emotion words and the participant is asked to indicate the extent to which he or she experienced each negative emotion that day (M = 8.26, SD = 4.16). In the current sample, the NA subscale of the short form of the PANAS demonstrated good internal consistency (α =.89).
3.3. Procedure
After providing written informed consent, participants completed baseline questionnaires. Participants also completed two eye-tracking tasks and underwent a stress induction not relevant to the present study's hypotheses. Participants were told that they would be receiving e-mailed links to a daily diary questionnaire battery three days per week (i.e., Monday, Tuesday, Thursday) at 6:00PM for the next two weeks. The daily diary questionnaire battery contained measures of stressful events, negative affect, worry symptoms, depressive symptoms, and social anxiety symptoms. Further, participants were instructed to complete each daily diary questionnaire battery within 24 h (i.e., before 6:00PM the following day). All study procedures were IRB-approved and in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
4. Data analysis
4.1. Data preprocessing
Of the 165 participants who were consented, 89.1% (n = 147) completed at least one of their six diary entries (completed entries: M = 4.22, SD = 1.52), with 51% (n = 75) completing at least five of the total six entries. Entries were excluded if they were completed more than 24 h after they were sent (13.78% of all entries) or if the control item to ensure the participant was paying attention (e.g., ‘Please select ‘Strongly agree’ for this item’) was answered incorrectly (16.62% of all entries). In total, 627 valid daily diaries were available for analysis.
4.2. Data analysis strategy
To examine the associations between DI, daily stress, daily NA, and daily symptoms, hierarchical linear models were constructed (HLM 7.0; Bryk and Raudenbush, 1992). Hierarchical linear modeling (HLM) was chosen because this framework takes into account the lack of independence among repeated, within-subject measurements and easily handles variations in number of within-subject measurements by assuming that the observed data points are representative of the population of all possible time points. All equations were constructed such that Level 1 included repeated, within-subject variables and Level 2 included between-subject variables.
Unconditional, random ANOVA models were examined first in order to partition variance in daily ratings of symptoms into Level 1 and Level 2. Substantial variability between subjects was found for daily worry symptoms, ICC =.57, χ2 = 965.19, p < 0.001, depressive symptoms, ICC =.66, χ2 = 1376.44, p < 0.001, and social anxiety symptoms, ICC =.59, χ2 = 1079.83, p < 0.001, indicating that hierarchical modeling of the data was necessary.
Second, time was added as a Level 1 predictor in separate models to determine whether daily symptoms changed throughout the course of the study and whether time should be consequently included in the final models. Kolmogorov-Smirnov tests indicated that daily worry symptoms, D =.28, p < 0.001, daily depressive symptoms, D =.22, p < 0.001, and daily social anxiety symptoms, D =.23, p < 0.001, were not normally distributed, and so robust standard errors were used in all subsequent analyses (Garson, 2012). Results indicated that the fixed effect of time approached significance for worry, t(478) = −1.86, p =.06, and was significant for depressive, t(473) = −2.34, p =.02, and social anxiety, t(477) = −4.01, p < 0.001, symptoms. Thus, time was included as a fixed effect in all models.
To evaluate the hypothesized prospective, moderating role of DI on daily-level associations between the occurrence of a stressor(s) and symptoms, Level 1 and Level 2 variables were added as fixed effects in order to examine predictors of daily symptoms. Daily occurrence of a stressor(s), daily negative affect, and time were entered as Level 1 predictors. DI and trait negative affect were grand mean-centered and entered as Level 2 variables. Finally, cross-level interaction terms between Level 2 DI and trait negative affect and the Level 1 daily stressor(s) occurrence variable were also entered. Daily negative affect was group mean-centered, whereas the dichotomous stressor variable and time were entered uncentered.
5. Results
5.1. Descriptive statistics
Means and standard deviations for baseline and daily measures are presented in Table 1.
Table 1.
Descriptives.
| M or % | SD | |
|---|---|---|
| Baseline measures | ||
| Age | 19.32 | 1.96 |
| Sex (% female) | 77 | |
| Ethnicity (% minority) | 29.1 | |
| DII | 10.44 | 9.19 |
| PANAS-NA | 19.02 | 7.80 |
| Daily measures | ||
| Stress (% days in which stressor(s) occurred) | 55.5 | |
| PANAS-NA | 8.26 | 4.16 |
| MASQ-GDD | 19.76 | 10.19 |
| PSWQ | 4.90 | 2.96 |
| SIAS | 11.53 | 6.10 |
Note. DII = Distress Intolerance Index; PANAS-NA =Positive and Negative Affect Schedule − Negative Affect Subscale; MASQ-GDD = Mood Anxiety Symptom Questionnaire − General Distress Depressive subscale; PSWQ = Penn State Worry Questionnaire; SIAS = Social Interaction Anxiety Scale.
5.2. Relationships between DI, daily stress, daily NA, and daily worry symptoms
Consistent with hypotheses, DI was significantly positively associated with daily worry (see Table 2). Further, the cross-level interaction term between Level 2 DI, but not trait negative affect, and daily stressor(s) occurrence was significant. To test the effect of daily stressor(s) occurrence on daily worry symptoms at varying levels of DI, regression coefficients, coefficient variances, and covariances were entered into an online calculator to compute simple slopes of the relationship between daily stressor (s) occurrence and daily worry symptoms at low (−1 SD) and high (+1 SD) DI (Preacher et al., 2006). A significant positive relationship between daily stressor(s) occurrence and daily worry symptoms was found at high (+1 SD) DI (B = 1.45, SE = 0.27, z = 5.46, p < 0.001), but not low (−1 SD) DI (B = 0.07, SE = 0.22, z = 0.32, p =.75) (see Fig. 1).
Table 2.
Effects of distress intolerance and daily stress on daily worry symptoms.
| Coefficient | SE | t-ratio | Approximate df | p Value | |
|---|---|---|---|---|---|
| Fixed effects | |||||
| Intercept of daily | |||||
| Worry | 4.38 | 0.25 | 17.95 | 144 | <0.001 |
| Level 2 variables | |||||
| DI | 0.06 | 0.02 | 3.06 | 144 | 0.003 |
| Trait NA | 0.09 | 0.03 | 3.10 | 144 | 0.002 |
| Level 1 variables | |||||
| Time | 0.01 | 0.05 | 0.19 | 474 | 0.85 |
| NA | 0.32 | 0.05 | 6.90 | 474 | <0.001 |
| Stress | 0.76 | 0.18 | 4.22 | 474 | <0.001 |
| Interaction effects | |||||
| Stress✻DI | 0.08 | 0.02 | 4.23 | 474 | <0.001 |
| Stress✻Trait NA | −0.04 | 0.03 | −1.53 | 474 | 0.13 |
| SD | Variance component | df | Chi-square | p Value | |
|
| |||||
| Random effects | |||||
| Between-subjects | |||||
| Residual | 1.75 | 3.07 | 144.00 | 826.58 | <0.001 |
| Within-subjects | |||||
| Residual | 1.62 | 2.63 | |||
Note: DI = Distress Intolerance; NA = Negative Affect.
Fig. 1.
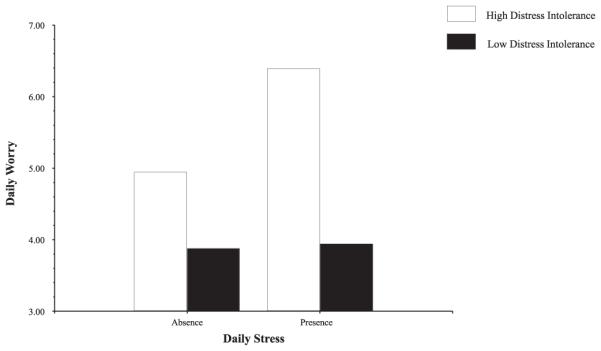
Effect of high vs. low DI on the association between the occurrence of a daily stressor and daily worry symptoms. Note that the y-axis scale has been truncated for greater visibility of differences; the full scale range is 3–15.
An exploratory analysis was conducted to test if the relationship between DI and worry was independent of co-occurring daily depressive symptoms. The model predicting daily worry symptoms was rerun with daily depressive symptoms entered as an additional Level 1 predictor. The Level 2 main effect of DI remained significant, B = 0.07, SE = 0.02, t(144) = 3.28, p =.001, as did the cross-level interaction between DI and the daily stressor (s) occurrence variable, B = 0.07, SE = 0.02, t(467) = 3.76, p < 0.001.
5.3. Relationships between DI, daily stress, daily NA, and daily depressive symptoms
Consistent with hypotheses, DI was significantly positively associated with daily depressive symptoms (see Table 3). Partially consistent with hypotheses, the cross-level interaction term between Level 2 DI, but not trait negative affect, and daily stressor(s) occurrence approached significance. To test the effect of daily stressor(s) occurrence on daily depressive symptoms at varying levels of DI, regression coefficients, coefficient variances, and covariances were entered into an online calculator to compute simple slopes of the relationship between daily stressor(s) occurrence and daily depressive symptoms at low (−1 SD) and high (+1 SD) DI (Preacher et al., 2006). A significant positive relationship between daily stressor(s) occurrence and daily depressive symptoms was found at high (+1 SD) DI (B = 3.06, SE = 0.90, z = 3.40, p < 0.001), but not low (−1 SD) DI (B = 1.14, SE = 0.61, z = 1.86, p =.06) (see Fig. 2).
Table 3.
Effects of distress Intolerance and daily stress on daily depressive symptoms.
| Coefficient | SE | t-ratio | Approximate df | p Value | |
|---|---|---|---|---|---|
| Fixed effects | |||||
| Intercept of daily | |||||
| Depression | 18.38 | 0.78 | 23.41 | 144 | <0.001 |
| Level 2 variables | |||||
| DI | 0.26 | 0.09 | 2.82 | 144 | 0.005 |
| Trait NA | 0.37 | 0.10 | 3.72 | 144 | <0.001 |
| Level 1 variables | |||||
| Time | −0.05 | 0.14 | −0.33 | 469 | 0.74 |
| NA | 0.96 | 0.13 | 7.58 | 469 | <0.001 |
| Stress | 2.10 | 0.55 | 3.82 | 469 | <0.001 |
| Interaction effects | |||||
| Stress✻DI | 0.11 | 0.06 | 1.79 | 469 | 0.07 |
| Stress✻Trait NA | −0.02 | 0.07 | −0.34 | 469 | 0.74 |
| SD | Variance component | df | Chi-square | p value | |
|
| |||||
| Random effects | |||||
| Between-subjects | |||||
| Residual | 6.23 | 38.84 | 144.00 | 1109.85 | <0.001 |
| Within-subjects | |||||
| Residual | 4.97 | 24.71 | |||
Note. DI = Distress Intolerance; NA = Negative Affect.
Fig. 2.
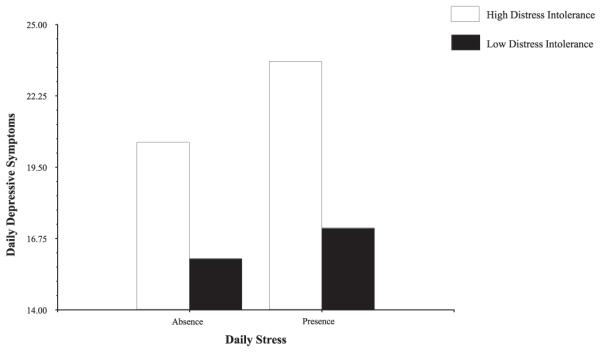
Effect of high vs. low DI on the association between the occurrence of a daily stressor and daily depressive symptoms. Note that the y-axis scale has been truncated for greater visibility of differences; the full scale range is 12–60.
An exploratory analysis was conducted to test if the relationship between DI and depressive symptoms was independent of co-occurring daily worry symptoms. The model predicting daily depressive symptoms was rerun with daily worry symptoms entered as an additional Level 1 predictor. The Level 2 main effect of DI remained significant, B = 0.30, SE = 0.10, t(144) = 3.14, p =.002, but the cross-level interaction between DI and the daily stressor(s) occurrence variable became non-significant, B = 0.04, SE = 0.06, t(467) = 0.69, p =.49.
5.4. Relationships between DI, Daily Stress, Daily NA, and daily social anxiety symptoms
Consistent with hypotheses, both the main effect of DI and the cross-level interaction term between Level 2 DI and daily stressor (s) occurrence were non-significant in the prediction of daily social anxiety symptoms (see Table 4).
Table 4.
Effects of distress Intolerance and daily stress on social anxiety symptoms.
| Coefficient | SE | t-ratio | Approximate df | p Value | |
|---|---|---|---|---|---|
| Fixed effects | |||||
| Intercept of daily | |||||
| SA | 11.40 | 0.50 | 22.98 | 144 | <0.001 |
| Level 2 variables | |||||
| DI | 0.08 | 0.06 | 1.35 | 144 | 0.18 |
| Trait NA | 0.26 | 0.08 | 3.48 | 144 | <0.001 |
| Level 1 variables | |||||
| Time | −0.23 | 0.10 | −2.24 | 473 | 0.03 |
| NA | 0.34 | 0.09 | 3.61 | 473 | <0.001 |
| Stress | 1.35 | 0.43 | 3.15 | 473 | 0.002 |
| Interaction effects | |||||
| Stress✻DI | 0.10 | 0.06 | 1.56 | 473 | 0.12 |
| Stress✻Trait NA | −0.05 | 0.08 | −0.65 | 473 | 0.52 |
| SD | Variance component | Df | Chi-square | p Value | |
|
| |||||
| Random effects | |||||
| Between-subjects | |||||
| Residual | 3.59 | 12.91 | 144.00 | 787.98 | <0.001 |
| Within-subjects | |||||
| Residual | 3.58 | 12.82 | |||
Note: SA = Social Anxiety; DI = Distress Intolerance; NA = Negative Affect.
6. Discussion
The present study's results were largely consistent with hypotheses. In line with DI's theoretical conceptualization (Leyro et al., 2010), DI significantly moderated the effect of daily stress on daily worry/depressive symptoms such that the positive relationship between stressor(s) occurrence and symptoms was present in individuals with high but not low DI. Further, the significant moderation effect was specific to DI and not accounted for by negative affect, providing empirical support for the theoretical notion that DI is a moderator of response to negative affect rather than redundant with negative affect itself. Consistent with DI's theoretical conceptualization and accumulating data on its specificity within the internalizing symptom domain (Cougle et al., 2011; Macatee et al., 2013, 2015), both main and interaction effects were found for daily depressive and worry, but not social anxiety symptoms, extending prior work by demonstrating symptom specificity prospectively in response to ecologically valid stressors. Interestingly, exploratory analyses revealed that DI's moderating effect on the association between daily stress and daily depressive symptoms was attributable to co-occurring daily worry, suggesting that high DI may specifically increase susceptibility to excessive and uncontrollable worry in the context of stress.
The observed specificity between DI and worry/depressive, but not social anxiety symptoms is consistent with theoretical conceptualizations of DI emphasizing negative reactivity to and avoidance of aversive internal stimuli (Leyro et al., 2010). Social anxiety generally involves specific, external threats (e.g., talking to a stranger) and relatively circumscribed feared outcomes (e.g., negative evaluation), whereas the focus of distress and avoidance in worry and depression is more internal and vaguely defined. Results of the present study suggest that prior findings of a positive relationship between DI and social anxiety (Keough et al., 2010; Laposa et al., 2015) may be attributable to co-occurring worry/depressive symptoms or trait negative affect. Indeed, the main effect of trait negative affect, but not DI, emerged as a significant predictor of daily social anxiety symptoms in the present study. Relatedly, daily negative affect and daily stressor(s) occurrence were significantly associated with daily social anxiety, suggesting that DI's specificity to worry and depressive symptoms was not attributable to a differential relationship between daily stress and worry, depressive, and social anxiety symptoms. Instead, the data suggest that daily stress was associated with increased reporting of all symptom types, but individuals with high DI appear to be particularly vulnerable to increased worry/depressive symptoms regardless of stressor occurrence and increased worry specifically on days in which stressors occurred.
The present findings are consistent with a growing body of literature on DI and intrusive cognition across affective disorders (i.e., obsessions, rumination, worry; Cougle et al., 2011, 2012, 2013; Macatee et al., 2013, 2015; Magidson et al., 2013). Because individuals with high DI perceive negative affect as particularly aversive, they may be more likely to respond to acute negative affect with worry specifically given its putative avoidance function with respect to aversive internal stimuli (Borkovec et al., 2004). Indeed, one theory argued that worry is utilized to avoid abrupt increases in negative affect (i.e., the emotional contrast avoidance model of worry; Newman and Llera, 2011), which may underlie the unique effect of DI on stress-elicited worry observed in the present study.
The present study has some limitations. First, although the sampling strategy ensured representation of high DI individuals, the sample was uncharacterized with regard to psychopathology. However, the mean DII score observed in the present sample was one standard deviation below the score reported in a treatment-seeking sample of outpatients (McHugh et al., 2014), suggesting that the present sample contained some individuals similar to individuals with diagnosed psychopathology. Nevertheless, future studies should determine if the observed results also emerge in clinical samples. Second, although the DII was specifically chosen due to accumulating evidence of its convergence with behavioral DI measures (McHugh and Otto, 2011; McHugh et al., 2016; Seo and Kwon, 2016; Szuhany and Otto, 2015), the observed associations have generally been small to medium in magnitude. Thus, the behavioral measures capture unique variance in the DI construct and so it is unclear if similar findings would emerge using behavioral DI measures. Future studies should include both self-report and behavioral measures of DI to ascertain the nature of the relationship between the DI construct and daily stressor-elicited symptoms. Third, the daily diary period was relatively short and the rate of non-compliance could be improved. Future studies should consider providing stronger incentives for participation and using longer follow-up periods to ensure the relationships observed in the present study are stable.
The results of the present study have clinical implications. Given evidence that DI can be reduced with targeted interventions (Bornovalova et al., 2012; Macatee and Cougle, 2015), psychosocial treatments for individuals with depressive and anxiety disorders, particularly those who present with high levels of worry, may benefit from inclusion of DI-targeted intervention modules. Indeed, recent approaches to the treatment of co-morbid generalized anxiety disorder and major depressive disorder emphasize emotional acceptance and flexible responding to distress (Mennin et al., 2015). Future treatment research in these populations should consider measuring DI as a possible mechanism of action, particularly with regard to improvements in responding to acute distress.
Footnotes
Contributions
Richard Macatee was responsible for study design and the results/discussion. Brian Albanese completed the introduction. Norman Schmidt and Jesse Cougle consulted on study design and provided edits. All authors approved the present manuscript.
Conflicts of interest
None.
References
- Allan NP, Macatee RJ, Norr AM, Schmidt NB. Direct and interactive effects of distress tolerance and anxiety sensitivity on generalized anxiety and depression. Cognit. Ther. Res. 2014;38(5):30–40. [Google Scholar]
- Allan NP, Macatee RJ, Norr AM, Raines AM, Schmidt NB. Relations between common and specific factors of anxiety sensitivity and distress tolerance and fear, distress, and alcohol and substance use disorders. J. Anxiety Disord. 2015a;33:81–89. doi: 10.1016/j.janxdis.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Almeida DM, Wethington E, Kessler RC. The daily inventory of stressful events an interview-based approach for measuring daily stressors. Assessment. 2002;9(1):41–55. doi: 10.1177/1073191102091006. [DOI] [PubMed] [Google Scholar]
- Berle D, Starcevic V, Moses K, Hannan A, Milicevic D, Sammut P. Preliminary validation of an ultra-brief version of the Penn State Worry Questionnaire. Clin. Psychol. Psychother. 2011;18(4):339–346. doi: 10.1002/cpp.724. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Alcaine O, Behar ES. Avoidance theory of worry and generalized anxiety disorder. In: Heimberg R, Mennin D, Turk C, editors. Generalized Anxiety Disorder: Advances in Research and Practice. Guilford; New York: 2004. pp. 77–108. [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug Alcohol Depend. 2012;122(1):70–76. doi: 10.1016/j.drugalcdep.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J. Abnorm. Psychol. 2001;110(4):585. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage; Newbury Park, CA: 1992. [Google Scholar]
- Bujarski SJ, Norberg MM, Copeland J. The association between distress tolerance and cannabis use-related problems: the mediating and moderating roles of coping motives and gender. Addict. Behav. 2012;37(10):1181–1184. doi: 10.1016/j.addbeh.2012.05.014. [DOI] [PubMed] [Google Scholar]
- Cakir Z. Examining psychometric properties of Distress Intolerance Index and Cognitive-Behavioral Avoidance Scale. Anadolu Pskiyatri Derg. 2016;17(1):24–32. [Google Scholar]
- Corstorphine E, Mountford V, Tomlinson S, Waller S, Waller G, Meyer C. Distress tolerance in the eating disorders. Eat. Behav. 2007;8:91–97. doi: 10.1016/j.eatbeh.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Timpano KR, Fitch KE, Hawkins KA. Distress tolerance and obsessions: An integrative analysis. Depress. Anxiety. 2011;28(10):906–914. doi: 10.1002/da.20846. http://dx.doi.org/10.1002/da.20846. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Timpano KR, Goetz AR. Exploring the unique and interactive roles of distress tolerance and negative urgency in obsessions. Personal. Individ. Differ. 2012;52(4):515–520. [Google Scholar]
- Cougle JR, Timpano KR, Sarawgi S, Smith CM, Fitch KE. A multi-modal investigation of the roles of distress tolerance and emotional reactivity in obsessive-compulsive symptoms. Anxiety Stress Coping. 2013;26(5):478–492. doi: 10.1080/10615806.2012.697156. [DOI] [PubMed] [Google Scholar]
- Ellis AJ, Vanderlind WM, Beevers CG. Enhanced anger reactivity and reduced distress tolerance in major depressive disorder. Cognit. Ther. Res. 2013;37(3):498–509. [Google Scholar]
- Garson DG. Hierarchical Linear Modeling: Guide and Applications. Sage Publications; Thousand Oaks, CA: 2012. [Google Scholar]
- Giorgio JM, Sanflippo J, Kleiman E, Reilly D, Bender RE, Wagner CA, Alloy LB. An experiential avoidance conceptualization of depressive rumination: three tests of the model. Behav. Res. Ther. 2010;48(10):1021–1031. doi: 10.1016/j.brat.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal ZM, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. J. Abnorm. Psychol. 2006;115:850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Gyollai Á, Simor P, KöTELES F, Demetrovics Z. Psychometric properties of the Hungarian version of the original and the short form of the Positive and Negative Affect Schedule (PANAS) Neuropsychopharmacol. Hung. 2011;13(2):73–79. [PubMed] [Google Scholar]
- Harrington N. The frustration discomfort scale: development and psychometric properties. Clin. Psychol. Psychother. 2005;12(5):374–387. [Google Scholar]
- Hawkins KA, Macatee RJ, Guthrie W, Cougle JR. Concurrent and prospective relations between distress tolerance, life stressors, and anger. Cognit. Ther. Res. 2013;37(3):434–445. [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am. J. Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: returning to contextual roots. Clin. Psychol.: Sci. Pract. 2001;8(3):255–270. [Google Scholar]
- Kashdan TB, Steger MF. Expanding the topography of social anxiety an experience-sampling assessment of positive emotions, positive events, and emotion suppression. Psychol. Sci. 2006;17(2):120–128. doi: 10.1111/j.1467-9280.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: the association with distress tolerance and anxiety sensitivity. Behav. Ther. 2010;41(4):567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR. Transdiagnostic factors of mental disorders. World Psychiatry. 2015;14:27–29. doi: 10.1002/wps.20175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laposa JM, Collimore KC, Hawley LL, Rector NA. Distress tolerance in OCD and anxiety disorders, and its relationship with anxiety sensitivity and intolerance of uncertainty. J. Anxiety Disord. 2015;33:8–14. doi: 10.1016/j.janxdis.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychol. Bull. 2010;136(4):576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macatee RJ, Cougle JR. Development and evaluation of a computerized intervention for low distress tolerance and its effect on performance on a neutralization task. J. Behav. Ther. Exp. Psychiatry. 2015;48:33–39. doi: 10.1016/j.jbtep.2015.01.007. [DOI] [PubMed] [Google Scholar]
- Macatee RJ, Capron DW, Guthrie W, Schmidt NB, Cougle JR. Distress tolerance and pathological worry: tests of incremental and prospective relationships. Behav. Ther. 2015;46(4):449–462. doi: 10.1016/j.beth.2015.03.003. http://dx.doi.org/10.1016/j.beth.2015.03.003. [DOI] [PubMed] [Google Scholar]
- Macatee RJ, Capron DW, Schmidt NB, Cougle JR. An examination of low distress tolerance and life stressors as factors underlying obsessions. J. Psychiatr. Res. 2013;47(10):1462–1468. doi: 10.1016/j.jpsychires.2013.06.019. http://dx.doi.org/10.1016/j.jpsychires.2013.06.019. [DOI] [PubMed] [Google Scholar]
- Mackinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, Rodgers B. A short form of the Positive and Negative Affect Schedule: evaluation of factorial validity and invariance across demographic variables in a community sample. Personal. Individ. Differ. 1999;27(3):405–416. [Google Scholar]
- McHugh RK, Kertz SJ, Weiss RB, Baskin-Sommers AR, Hearon BA, Bjorgvinsson T. Changes in distress intolerance and treatment outcome in a partial hospital setting. Behav. Ther. 2014;45(2):232–240. doi: 10.1016/j.beth.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Listhaus AR, Seitz-Brown CJ, Anderson KE, Lindberg B, Wilson A, Daughters SB. Rumination mediates the relationship between distress tolerance and depressive symptoms among substance users. Cognit. Ther. Res. 2013;37(3):456–465. doi: 10.1007/s10608-012-9488-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Otto MW. Domain-general and domain-specific strategies for the assessment of distress intolerance. Psychol. Addict. Behav. 2011;25:745–749. doi: 10.1037/a0025094. http://dx.doi.org/10.1037/a0025094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Weiss RD, Cornelius M, Martel MO, Jamison RN, Edwards RR. Distress intolerance and prescription opioid misuse among patients with chronic pain. J. Pain. 2016 doi: 10.1016/j.jpain.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Otto MW. Refining the measurement of distress intolerance. Behav. Ther. 2012;43:641–651. doi: 10.1016/j.beth.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D, Abramowitz JS, Calamari JE, Kyrios M, Radomsky A, Sookman D, Wilhelm S. A critical evaluation of obsessive–compulsive disorder subtypes: symptoms versus mechanisms. Clin. Psychol. Rev. 2004;24(3):283–313. doi: 10.1016/j.cpr.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Ritter M, Heimberg RG. An open trial of emotion regulation therapy for generalized anxiety disorder and co-occurring depression. Depress. Anxiety. 2015;32(8):614–623. doi: 10.1002/da.22377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscovitch DA. What is the core fear in social phobia? A new model to facilitate individualized case conceptualization and treatment. Cognit. Behav. Pract. 2009;16(2):123–134. [Google Scholar]
- Newman MG, Llera SJ. A novel theory of experiential avoidance in generalized anxiety disorder: a review and synthesis of research supporting a contrast avoidance model of worry. Clin. Psychol. Rev. 2011;31(3):371–382. doi: 10.1016/j.cpr.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norberg MM, Keyan D, Grisham JR. Mood influences the relationship between distress intolerance and discarding. J. Obsessive-Compuls. Relat. Disord. 2015;6:77–82. [Google Scholar]
- Norr AM, Oglesby ME, Capron DW, Raines AM, Korte KJ, Schmidt NB. Evaluating the unique contribution of intolerance of uncertainty relative to other cognitive vulnerability factors in anxiety psychopathology. J. Affect. Disord. 2013;151(1):136–142. doi: 10.1016/j.jad.2013.05.063. http://dx.doi.org/10.1016/j.jad.2013.05.063. [DOI] [PubMed] [Google Scholar]
- Peterson RA, Reiss S. Anxiety Sensitivity Index Revised Test Manual. IDS Publishing; Worthington, OH: 1992. [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J. Educ. Behav. Stat. 2006;31(4):437–448. [Google Scholar]
- Rachman S. A cognitive theory of obsessions. Behav. Res. Ther. 1997;35:793–802. doi: 10.1016/s0005-7967(97)00040-5. [DOI] [PubMed] [Google Scholar]
- Seo JW, Kwon SM. Testing an affective judgment model of distress tolerance in college heavy drinkers. Addict. Behav. 2016;58:100–103. doi: 10.1016/j.addbeh.2016.02.021. [DOI] [PubMed] [Google Scholar]
- Shaw AM, Timpano KR. An experimental investigation of the effect of stress on saving and acquiring behavioral tendencies: the role of distress tolerance and negative urgency. Behav. Ther. 2016;47(1):116–129. doi: 10.1016/j.beth.2015.10.003. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: development and validation of a self-report measure. Motiv. Emot. 2005;29(2):83–102. [Google Scholar]
- Szuhany KL, Otto MW. Contextual influences on distress intolerance: priming effects on behavioral persistence. Cognit. Ther. Res. 2015;39(4):499–507. doi: 10.1007/s10608-015-9672-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardenaar KJ, van Veen T, Giltay EJ, de Beurs E, Penninx BW, Zitman FG. Development and validation of a 30-item short adaptation of the Mood and Anxiety Symptoms Questionnaire (MASQ) Psychiatry Res. 2010;179(1):101–106. doi: 10.1016/j.psychres.2009.03.005. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule-Expanded Form. 1999 Retrieved from University of Iowa, Department of Psychology Web site: 〈 http://www.psychology.uiowa.edu/Faculty/Watson/Watson.html〉.


