Abstract
Objectives
Wearable devices are currently at the heart of just about every discussion related to the Internet of Things. The requirement for self-health monitoring and preventive medicine is increasing due to the projected dramatic increase in the number of elderly people until 2020. Developed technologies are truly able to reduce the overall costs for prevention and monitoring. This is possible by constantly monitoring health indicators in various areas, and in particular, wearable devices are considered to carry this task out. These wearable devices and mobile apps now have been integrated with telemedicine and telehealth efficiently, to structure the medical Internet of Things. This paper reviews wearable health care devices both in scientific papers and commercial efforts.
Methods
MIoT is demonstrated through a defined architecture design, including hardware and software dealing with wearable devices, sensors, smart phones, medical application, and medical station analyzers for further diagnosis and data storage.
Results
Wearables, with the help of improved technology have been developed greatly and are considered reliable tools for long-term health monitoring systems. These are applied in the observation of a large variety of health monitoring indicators in the environment, vital signs, and fitness.
Conclusions
Wearable devices are now used for a wide range of healthcare observation. One of the most important elements essential in data collection is the sensor. During recent years with improvement in semiconductor technology, sensors have made investigation of a full range of parameters closer to realization.
Keywords: Delivery of Health Care, Information Storage and Retrieval, Internet, Mobile Applications, Smartphone, Telemedicine
I. Introduction
The Internet of Things (IoT) is a new concept, providing the possibility of healthcare monitoring using wearable devices. The IoT is defined as the network of physical objects which are supported by embedded technology for data communication and sensors to interact with both internal and external objects states and the environment [1].
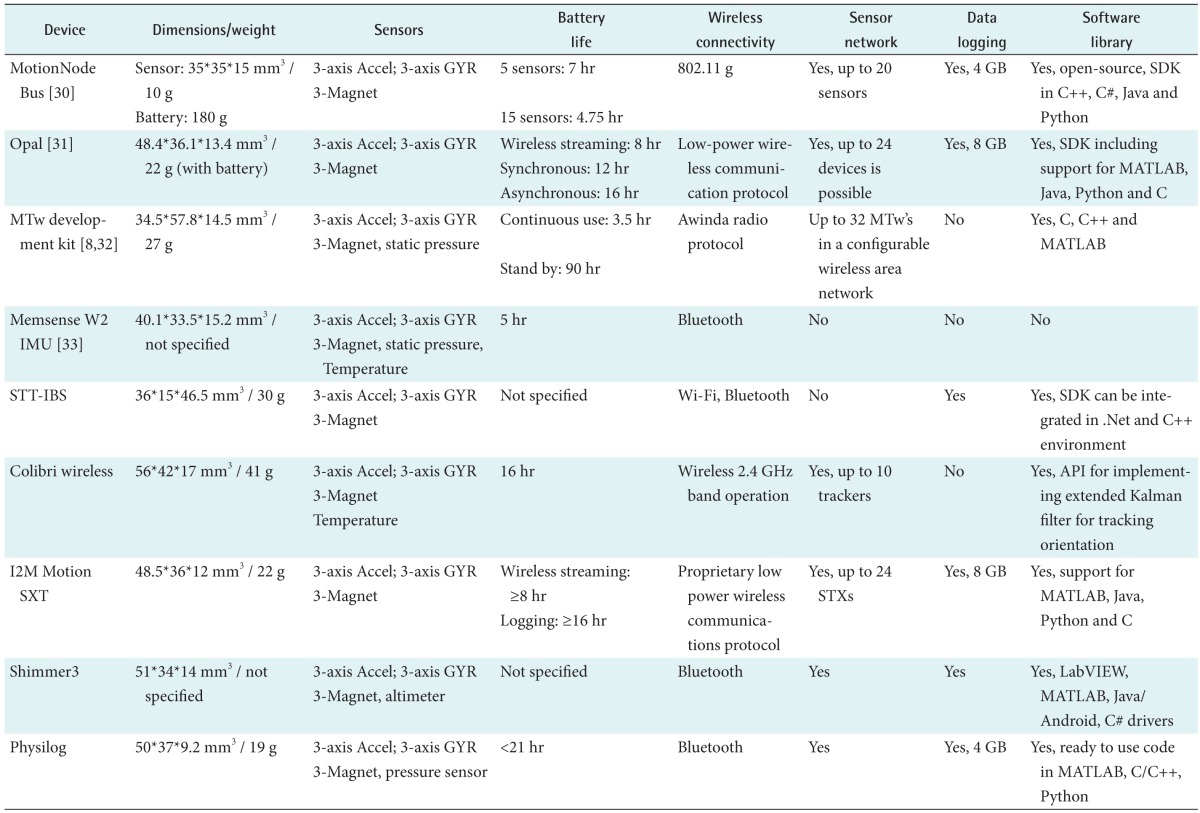
In the last decade, wearable devices have attracted much attention from the academic community and industry and have recently become very popular. The most relevant definition of wearable electronics is the following: “devices that can be worn or mated with human skin to continuously and closely monitor an individual's activities, without interrupting or limiting the user's motions” [2]. Table 1 provides more transparent information on the importance of wearable devices and the IoT market [3,4,5].
Table 1. Importance of wearable devices and Internet of Thing (IoT) in market.
Today, the range of wearable systems, including micro-sensors seamlessly integrated into textiles, consumer electronics embedded in fashionable clothes [6], computerized watches, belt-worn personal computers (PCs) with a head mounted display [7], glasses [8], which are worn on various parts of the body [9] are designed for broadband operation. The field of wearable health monitoring systems is moving toward minimizing the size of wearable devices, measuring more vital signs, and sending secure and reliable data through smartphone technology. Although there has been an interest in observing comprehensive bio/non-bio medical data for the full monitoring of environmental, fitness, and medical data recently [10], but one obvious application of wearable systems is the monitoring of physiological parameters in the mobile environment. The majority of commercially available wearable devices are one-lead applications to monitor vital signs. However, most of such recreational devices are not suitable for the medical monitoring of high risk patients. Those devices that have been qualified for medical use are usually simple [11].
The objective of this paper is to review wearable health care devices both in scientific papers and commercial efforts. Our aim is to address the most important wearable devices, which measure effective parameters in health status directly. Readers can obtain comprehensive and useful information on the most reliable currently available devices and technical concepts in this area.
The rest of this review paper is organized as follows. The need for health monitoring when the user is in motion and under changing environmental conditions are investigated in Section II. In Section III recent research efforts in wearable devices are presented in three subsections. The first subsection discusses motion tracking and the research approaches and implementations in this area, and then some of the most recent commercial devices are compared. We then discuss the monitoring of environmental conditions and vital signs through wearable devices in subsections 2 and 3. In Section IV, the challenges of potentially available devices are discussed. Conclusion are finally summarized with suggestions for future works.
II. Wearable Devices in Health Monitoring
In today's world, where time is precious, people, the working class especially, spend most of the day shuttling between various tasks and tend to ignore their health and fitness [6]. Even a simple appointment with a doctor in a clinic can require several tests set for diagnosis, prescription, and finally treatment, which can take a lot of time. Therefore, many patients only go to a clinic when they are suffering from a serious illness. Hence, many people are seeking for an alternative, such as a device that can be worn on the body, which would not only continuously monitor the user's health in real time but also provide timely insights on various health parameters to the user as well as his or her physician [6].
1. Motion Trackers
The measurement of human movement (motion tracking) has several useful applications in sports, medical, and other branches of studies. Such applications include fall risk assessment, quantifying sports exercise, studying people habits, and monitoring the elderly. Wearable trackers are becoming increasingly popular for two main reasons. They can motivate the user during the daily workout to perform more exercise, while providing activity measurement information through a smartphone without manual calculation [12]. Also, they enable the wearer to become aware of the daily distance walked, which is very useful to ensure that the user maintains sufficient activity in the daily routine to maintain a healthy life. In particular, to accurately observe motion of the human body, 3-axis accelerometers, magnetometers, and gyroscopes sensors obtain data, each for a specific purpose. These sensors can be used for human activity recognition in the ubiquitous computing domain as well [13]. Gyroscopes and magnetometers are auxiliary sensors that can be separately be combined with accelerometers to compensate the lack of accuracy in obtained data for motion tracking. In most cases, the combination of these three sensors lead to 9DoF.
Human motion detection has a wide range of application, from sports and recreation to biomedical. In recent years, consumer electronics have employed many semiconductor-based tracking system to allow users to access various kinds of interface control that use body motions and gestures [14]. An important application of motion tracking is health care. However, due to need for high accuracy in the biomedical field, these devices are not typically designed only for medical application. The initial concept of using uniaxial accelerometer sensors in motion tracking was introduced in 1996 by Veltink and Boom [15]. To introduce the concept of motion tracking in the medical application world, multiple clinical studies have been performed on posture estimation using accelerometers [16,17,18]. An accelerometer alone cannot provide precise information; therefore, in 1997, researchers improved the performance of trackers and integrated semiconductor-based gyroscopes to perform bio-mechanical assessments and gait analysis [19]. Four years later in 2002, Mayagoitia et al. [20] introduced the initial framework of tracking lower extremities with a fusion of accelerometers and gyroscopes in the 2D sagittal plane. When the trackers became more reliable using an integrated gyroscope, the primary focus for clinical applications using inertial motion tracking was gait analysis [21]. To apply this device for clinical purposes, and in particular gait motion, gravity sensitive accelerometers are used to estimate the tilt angles between the gravity vector and the sensor's axes [19]. The first version of the most recently integrated sensors (accelerometer, gyroscope, and magnetometer) which provide very accurate data with 9DoF, was proposed in 2006 by Roetenberg [22]. He proposed using a set of tri-axial accelerometers, tri-axial gyroscopes, and a magnetometer to estimate and monitor human motion.
A few 9DoF wireless inertial measurement units (IMUs) are commercially available and have been used for research projects [23,24,25]. Due to the high risk of falling in the elderly, motion trackers as wearable devices are used in medical health monitoring for fall detection.
1) Motion measurement in body tracking
A new design was presented by Bertolotti et al. [26] to apply for objective measurements of trunk or limb movements for the assessment of human body balance and control abilities. This system is based on a 72 MHz, 32-bit CPU (STM32F303VC; STMicroelectronics, Geneva, Switzerland) embedding a high performance ARM CortexM4, 32-bit RISC core, with the potential of supporting several sensors externally with high performance in both SPI and I2C mode. In this research, the sensor components (STMicroelectronics sensors) have a linear range and a sensitivity that allow proper measurement of body movements. Online processing, in the sense of data acquisition from different sensors, filtering, and data generation are performed at a high frequency of up to 72 MHz. Body movements are measured using 9DoF sensors: three inertial sensors, an accelerometer, a magnetometer, and a gyroscope. The full-scale values of the sensors can be modified by means of specific commands sent by the microcontroller [27,28]. The size of the whole device, including all components in the box (circuit board, the Bluetooth module, and the battery) are 60 mm × 35 mm × 20 mm. The box is made of transparent plastic to allow the observation of LED indicators working on the board. The device proposed and implemented by this research group was designed to be used for three kinds of movement monitoring. The first and second types of movement monitoring are referred to as short- and long-term data monitoring. In the first type, the device is only connected to a PC to observe the results. In the second case, data are observed and locally stored for long-term monitoring. In the third type, the most important component is the body network, i.e. multiple units deployed on the subject's body and wired to a gateway unit, which can have a local memory or a wireless connection to a PC or hand-held device (full body monitoring of exercises) [29].
2) Commercially available user devices applied in research papers
The following two subsections report on the advantages and disadvantages of commercially available devices and the tools that have been used in research for performance evaluation.
(1) Part 1: Comparison of nine motion tracking devices applied in research
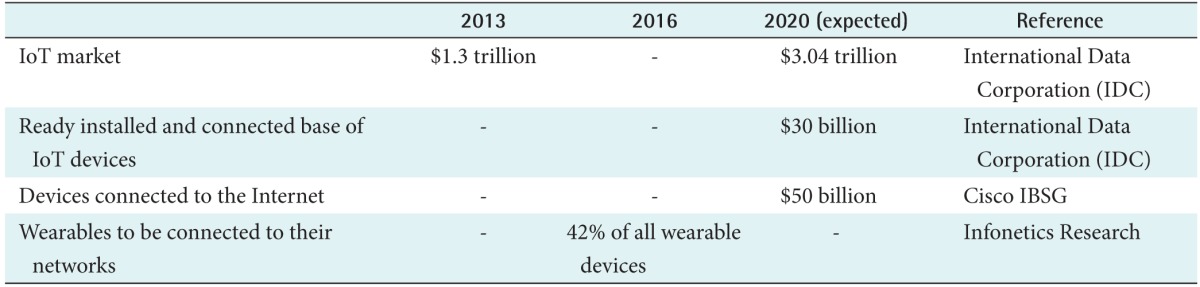
In the first part, nine devices with different evaluated parameters are presented in Table 1 and are compared [29]. To identify the benefits, some expected merits have to be determined and comparison is performed based on it. Long-term monitoring for further diagnosis is one of the main purposes of health care monitoring. To achieve this aim, a device has to store data temporarily in memory and send it to a cloud computing or medical station to be stored permanently. To fulfill these necessities, data buffering, which requires SD memory and RAM are of concern. On the other hand, for data transmission, Bluetooth and Wi-Fi compatibility are essential.
Many of these devices come only with customized software application. Some of them allow a user to build his/her commercially devices own application on it but others. A characteristic that, at the first glance, does not sound crucial is the firmware. To take full advantage of a development kit, in some cases, customization is necessary, but not all device manufacturers provide such compatibility.
Here, the nine devices that have been used and investigated in research are introduced, and important features are studied. Wearable devices are restricted by several factors. The most critical elements are size, battery life, weight, and capability of adding on-board sensors. In Table 2, all mentioned elements are compared, and additional parameters, including connectivity, software, and firmware compatibility are taken into consideration.
Table 2. Comparison of nine commercially available motion tracking devices applied in research.
Accel: accelerometer, GYR: gyroscope, Magnet: magnetometer.
Table 2 presents nine commercially available wireless motion trackers that have been used in research and are produced by various companies and manufacturers (MotionNode Bus [30], Opal [31], MTw development kit [32], Memsense W2 IM2 [33], STT-IBS [34], Colibry wireless [35], I2M motion SXT [36], Shimmer 3 [37], Physilog [38]). We have attempted to present the most recent research works and devices in the market.
(2) Part 2: Comparison of four top wrist-worn device commercially available in market
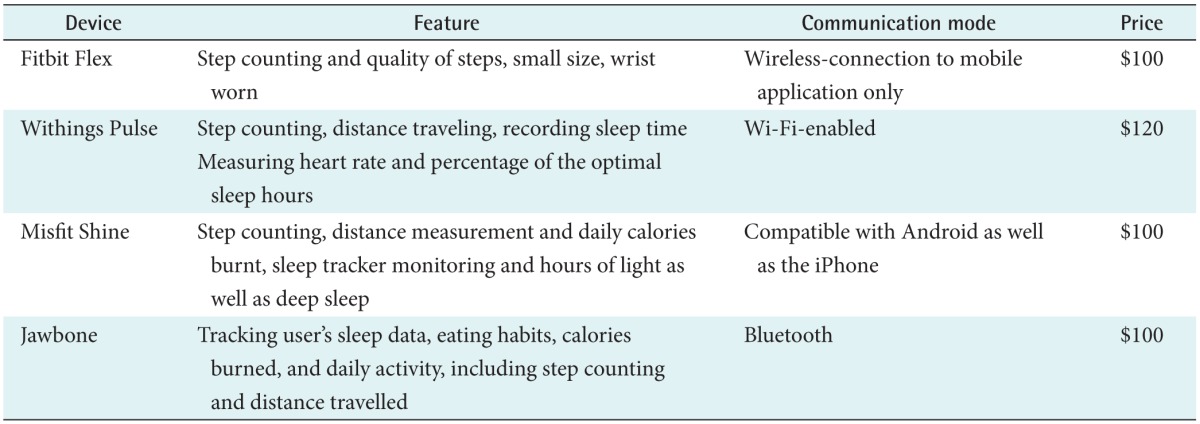
In this subsection, the most popular and recent commercial motion trackers are compared [27]. First, the four most popular wristband-style wearable commercial devices—Fitbit Flex, Withings Pulse, Misfit Shine, and Jawbone Up24 (Figure 1)—are introduced and briefly described. Then, according to the previously mentioned merits, these commercial devices are compared [31]. An important requirement from wearers is the visualization of actual and real data. Therefore, the accuracy of fitness tracking is one of the key factors of device selection. According to the quality of the used components and software, some devices perform better than others. Obtained experimental results from each device, are used to study both the accuracy and ease-of-use of the four wearable devices. This study was performed in Korea. The devices for experiments were selected among the 10 top available wearable device in the market. The four wearable devices considered in the experiments [25,39] were selected randomly. The four devices are described in detail below. Further information is summarized in Table 3, which briefly compares the features of the four wearable devices. The commercial name of device, country of manufacturing, tasks ability, and price are provided for each one.
Figure 1. (A-D) Four popular motion tracker wearable devices. (E) Four popular motion tracker wearable devices wristworn.

Table 3. Features of four wearable devices.
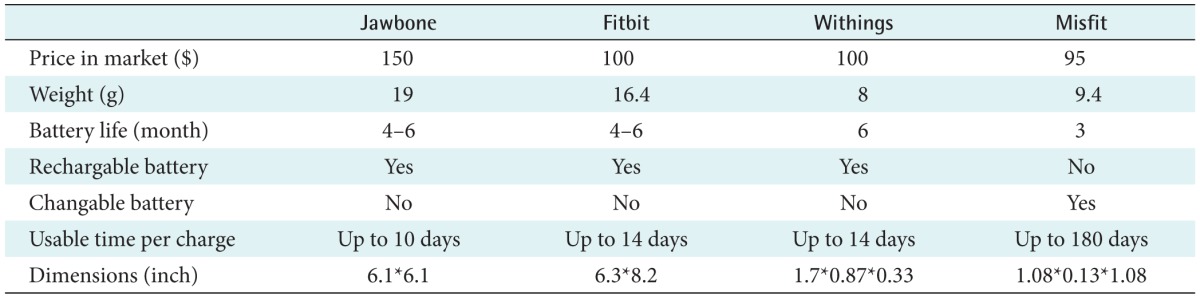
In Table 4, the features and communication mode of these four popular wearable devices are summarized. The purpose of the table is easy comparison of the devices [40,41,42,43].
Table 4. Features and communication modes of four commercial wearable devices.
2. Vital Signs Measurement
Many wearable devices have been implemented to measure critical elements in healthcare monitoring. The majority of these devices are in one lead such as electrocardiogram (ECG) and electroencephalogram (EEG) measurement, skin temperature, etc. There have been recent efforts in wearable devices to provide multi-task vital signs measurement. Here, we present the most creative and recent papers in this area.
Many devices, structures, designs, and solutions for remote wearable ECG monitoring, which plays a vital role in health monitoring have been proposed in the literature and industry. Generally, these solution are hard to implement and are not efficient enough in power consumption or performance. Some of them are remarkable but do not have the possibility of merging with other out signals from different systems.
1) Body-worn smart clothing
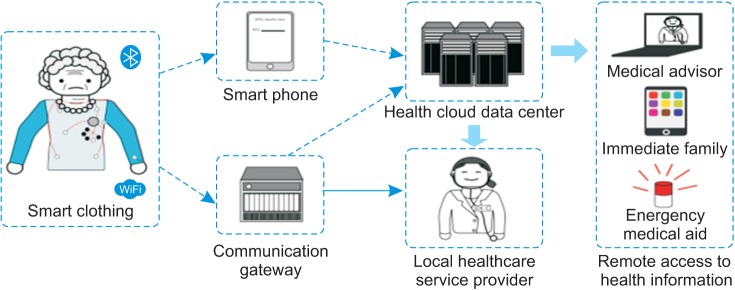
To obtain health care status's signals from various physiological indicators due to forming a source data center for comprehensive health monitoring, a ‘smart clothing’ design was presented in [44]. To make smart clothing systems intelligent, an infrastructure incorporating smartphones, mobile applications, cloud computing, and big data analytic is required to communicate in the structured design [45].
Although several research approaches in the field of health monitoring have been proposed and implemented, the existing solutions in different aspects have failed for long-term health monitoring [45]. Traditional health monitoring, which often collects one or a very limited number of physiological signals, is not very useful for chronic diseases in a full-range health monitoring system.
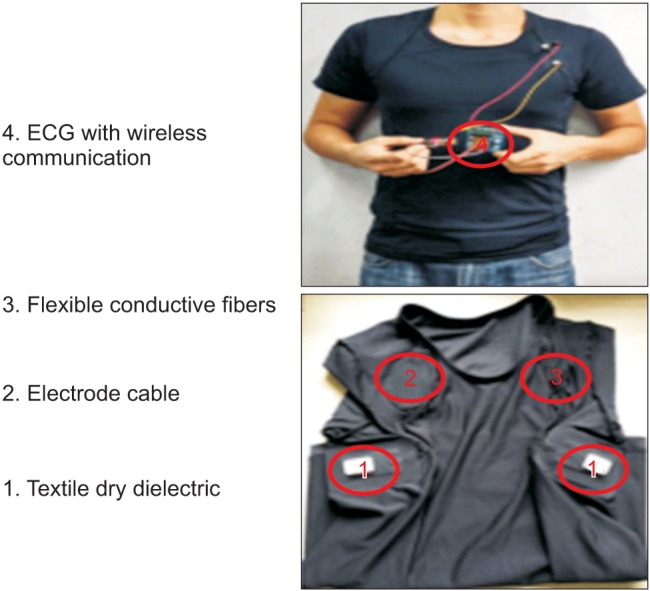
Sensor deployment on the body is the main difference between old wearable devices and smart clothing [45]. In smart clothing, all sensors which are used to measure the vital signs are integrated into textile clothing. Sensor placement is a critical point that has to be performed properly. To provide efficiency and a well-formed design, the quality of the used sensors, proper positioning, layout of flexible electricity cable, weak signal acquisition equipment, low-power wireless communications, and user comfort [45] are crucial factors. The fabric of the smart clothing to be worn, has to be comfortable. In this design, it has been tried to measure only vital and necessary parameters. Now the used sensors and also the location they are placed on the body are described (Figure 2).
Figure 2. Smart clothing in communication with outside world.
(1) Sensors placement
In Table 5, the position and task of each deployed sensor in smart clothing is summarized.
Table 5. Used sensor position and task in smart cloth.
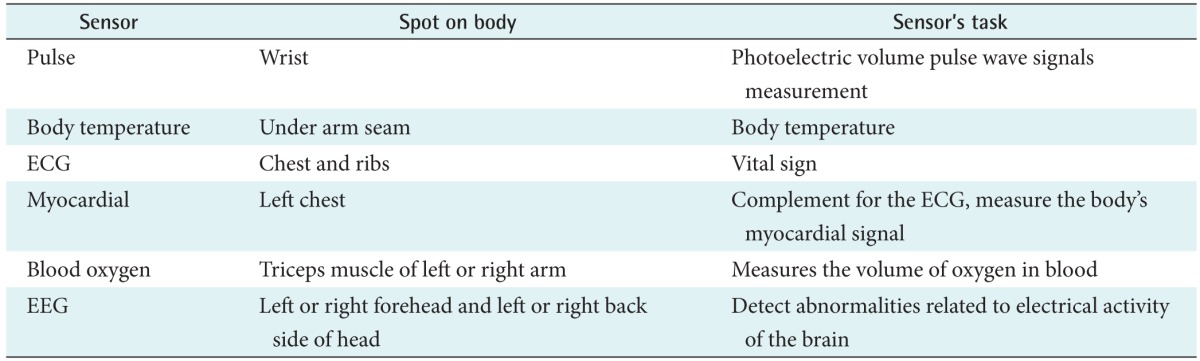
ECG: electrocardiogram, EEG: electroencephalogram.
When all sensors are positioned appropriately, each sensor must be wrapped by a flexible covering layer to protect the sensor and to make the device comfortable to be worn by the user. Further textile electrodes touch the user's skin to sense and transmit the data. These electrodes must be sewn on the cloth from the inside. Once the sensors and devices are powered on, they will come into operation. It is possible to wash smart clothing (Figure 3). However, it should be noted that some components are not washable and waterproof, but these can be removed easily by the wearer, and reinstallation is straightforward [44].
Figure 3. Washable smart clothing.
There are three major drawbacks to smart clothing:
- Intra-smart-clothing system: In the first step, it is necessary to consider the wearer's physical body shape, type of disease to be monitored, and daily habits [45]. In fact, in many cases, it is necessary to customize the smart clothing for the applicant. In addition, technical feasibility, comfort level, and cost effectiveness are serious concerns for the manufacturer.
- Communications for inter-smart clothing: A device structure design brings the user benefits when it can communicate with the outside world and transmit data. Inter smart-clothing design focuses on the communication problem of interconnecting smart clothing with the outside world. It is the intermediate level of structure device for the closed-loop system of smart clothing to be connected to cloud. The second use of this level could assist connection to a local medical center.
- Beyond-smart-clothing (BSC) on clouds: To complete the procedure of data collection, transmission, and analysis, cloud computing is essential. In fact, according to some pre-defined algorithms, data are sent to a medical center, appropriate decisions are taken by medical doctors, physicians, or other healthcare professionals. In emergency cases, some feedback must be sent to the user to inform him or her about his/her health's status. Thus, cloud computing is integrated in BSC [46]. There are various technological possibilities for the basis of BSC, such as cloud computing, big data, machine learning, etc. [44].
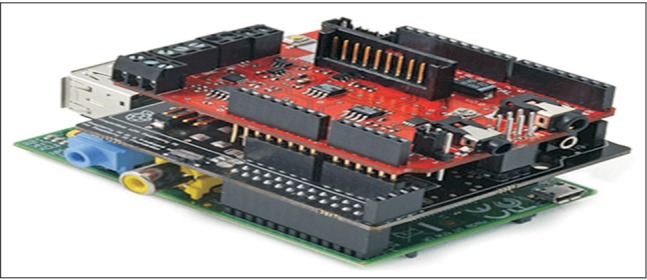
2) Wire-based wearable devices: limited physiological and environmental parameters measurement
In [47], a novel approach to medical monitoring was introduced by Sanfilippo and Pettersen. The methodology is wire-based and many vital signs are measured. This wearable integrated health-monitoring system is based on the e-Health Sensor Platform [48] V2.0, which is the first biometric shield for Arduino and Raspberry Pi. However this device is not licensed for medical health monitoring. The system allows researchers to measure and investigate health through body monitoring by using 10 sensors to observe vital signs and perform motion tracking. EEG, ECG, and body temperature measurement are carried out by these sensors, which are connected to the platform. A push button is considered for emergency cases. Collected data are used in two scenarios. In the first, the user is monitored in real time, and in the second, sensitive data are transmitted to be analyzed for medical diagnosis.
In this paper, a wearable health sensor monitoring system based on a multi-sensor fusion approach is outlined. The implemented device consists of a chest-worn device that embeds a controller board, an ECG sensor, a temperature sensor, an accelerometer, a vibration motor, a color-changing light-emitting diode (LED), and a push-button [47].
The embedded vibration motor makes it possible to actuate distinctive haptic feedback patterns according to the wearer's health state. Haptic feedback, informs the wearer about his or her health status in three different states. When it does not vibrate, it indicates a normal state; through low-frequency and high-frequency vibration, abnormal data observation and potential risk are indicated, respectively [49].
To address privacy concerns, data is encrypted before transmission. Data collected for permanent storage are sent to cloud storage, while data to be visualized in real-time, are sent directly to a laptop or smart phone.
The structural framework is based on a multi-sensor fusion approach. In particular, a client-server pattern is adopted in [47]. A chest-worn device, comprising an Arduino Uno board based on the ATmega328 micro-controller, an Arduino Wi-Fi Shield, e-Health Sensor Shield, a vibrating motor, and push button, operates as a client and remotely communicates with a server. The server is implemented in three levels of logic and communication.
The device structure is implemented in three layers (Figure 4). The bottom and basic layer is Arduino ATmega328. To enable communication capabilities to this proposed wearable device, an Arduino Wi-Fi Shield [50] is stacked on top of the adopted controller board, which forms the second layer. In detail, the Arduino Wi-Fi Shield allows the client to communicate with the server by using the 802.11 wireless specification (Wi-Fi) [48]. The communication between the Arduino Wi-Fi Shield and the Arduino Uno board uses long wirewrap headers that extend through the shield. The third and top layer is implemented when the wearer's biometric data are gathered, and an e-Health Sensor Shield [51] is stacked on top of the adopted communication module.
Figure 4. Arduino Uno board (an Arduino Wi-Fi Shield, e-Health Sensor Shield).
III. Challenges and Bottlenecks for Medical IoT
Leading wearable devices based on IoT platforms must provide simple, powerful application access to IoT devices. Many platforms and structures have been proposed by the scientific community, and commercial devices are already available for bio-metric/medical parameter measurement. However, there are serious challenges in this way. The following are four key capabilities that leading platforms must enable:
- Simple and secure connectivity: A good IoT platform is expected to provide easy connection of devices and perform device management functions in three levels of data collection, data transmission to a hub, and permanent storage and observation in a medical station. These steps must be secured; therefore, data encryption is necessary.
- Power consumption: To provide the wearer with easy device management and long-term monitoring without interruption, power loss is becoming more important. This is strictly correlated to the number of parameters that are observed, efficient code programming, as well as good data packing, encryption, and compression.
- Wearability: Wearable devices have been designed for various types of bio-medical monitoring to assisting users in living long, healthy lives. This point is more significant when these devices are intended to be worn by elderly users. Therefore, such devices must be easy to wear, easy to carry, and comfortable. These requirements are fulfilled with a light, small, and well-structured device. A wearable device is expected to be small and light weight, and should be able to be used for a long time.
- Reduced risk in data loss: When data is collected by a microcontroller and transmitted to a smartphone or cloud storage, there is a possibility of disconnection and consequently data loss. This must be reduced as much as possible to provide safe health monitoring. It may be possible through temporary data saving (buffering) in the microcontroller providing a large memory.
IV. Conclusion
Wearable devices are becoming popular in various fields from sport and fitness to health monitoring. In particular, due to the increasing elderly population throughout the world, wearable devices are becoming important for long-term health monitoring. The main aim of this work was to give a comprehensive overview of this area of research and to report the full range of tools in area of wearable health monitoring devices. In this review paper, we have reported both research works and commercial devices to study and investigate the currently available technology. In preparing this paper, we studied the literature from various points of view. Based on consultation with expert scientists in environmental engineering and medicine, we believe that, motion trackers, gas detectors, and vital signs are the most important elements in health monitoring; therefore, to achieve the full range of health monitoring, all these parameters were studied. In each field, a variety of methodologies are employed, but not all are efficient and effective. The most important criteria in this study was the possibility of using the device in the real world, performance, efficiency, and power consumption. In addition, we considered the price of each device. Finally, the most challenging bottleneck and some conclusions regarding the promising future in the IoT is presented.
Among all implemented works so far, no efficient solution has been proposed for comprehensive monitoring in gas detection, motion tracking, and vital sign monitoring to integrate all these into a single device. It might be possible to realize this in future work by creating a system with following characteristics:
- #MULTIPLE sensors on ONE sensor node,
- #MULTIPLE nodes on ONE individual,
- #MULTIPLE individuals on ONE cloud system.
Monitoring of an individual with number of parameters in his working/living environment is possible. Moreover, computational models and software development for data encryption and data compression have to be investigated for more efficiency. In the first scenario above, which seems to be the best approach, there are serious restrictions in available sensors. To realize this wearable possibility, appropriate components must be located properly and must function well. In the second scenario, tasks can be dedicated to each node. For instance, motion tracking sensors can be implemented on one sensor node, and vital sign monitoring can be implemented on another. The third scenario is merging of the first and second methodology, which could widen the range of users and the range of practical application.
Acknowledgments
We would also like to express our gratitude to Professor Norbert Stoll for valuable technical guidance and sharing his knowledge to complete this work.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.LeHong H, Velosa A. Hype cycle for the Internet of Things, 2014 [Internet] Stamford (CT): Gartner Inc.; 2014. [cited at 2017 Jan 25]. Available from: https://www.gartner.com/doc/2804217/hype-cycle-internet-things- [Google Scholar]
- 2.Gao W, Emaminejad S, Nyein HY, Challa S, Chen K, Peck A, et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature. 2016;529(7587):509–514. doi: 10.1038/nature16521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Business Wire. Finding success in the new IoT ecosystem: market to reach $3.04 trillion and 30 billion connected "Things" in 2020, IDC says [Internet] San Francisco (CA): Business Wire; 2014. [cited at 2017 Jan 25]. Available from: http://www.businesswire.com/news/home/20141107005028/en/Finding-Success-IoTEcosystem-Market-Reach-3.04. [Google Scholar]
- 4.Wilson J Infonetics survey unveils businesses' plans for mobile security, Internet of Things, wearables [Internet] London: HIS Inc.; 2015. [cited at 2017 Jan 25]. Available from: https://technology.ihs.com/527159/infonetics-survey-unveils-businesses-plans-for-mobile-security-internet-of-things-wearables. [Google Scholar]
- 5.Evans D. The Internet of Things: how the next evolution of the Internet is changing everything [Internet] San Jose (CA): Cisco Internet Business Solutions Group; 2011. [cited at 2017 Jan 25]. Available from: http://www.cisco.com/c/dam/en_us/about/ac79/docs/innov/IoT_IBSG_0411FINAL.pdf. [Google Scholar]
- 6.Xu S, Zhang Y, Jia L, Mathewson KE, Jang KI, Kim J, et al. Soft microfluidic assemblies of sensors, circuits, and radios for the skin. Science. 2014;344(6179):70–74. doi: 10.1126/science.1250169. [DOI] [PubMed] [Google Scholar]
- 7.Martin T, Jovanov E, Raskovic D. Issues in wearable computing for medical monitoring applications: a case study of a wearable ECG monitoring device; Proceedings of the 4th International Symposium on Wearable Computers; 2000 Oct 16-17; Atlanta, GA. pp. 43–49. [Google Scholar]
- 8.Jovanov E, Gelabert P, Wheelock B, Adhami R, Smith P. Real time portable heart monitoring using low power DSP; Proceedings of International Conference on Signal Processing Applications and Technology (ICSPAT); 2000 Oct 16-19; Dallas, TX. pp. 16–19. [Google Scholar]
- 9.Swider M. Google Glass review [Internet] [place unknown]: TechRadar; 2016. [cited at 2017 Jan 25]. Available from: http://www.techradar.com/reviews/gadgets/google-glass-1152283/review. [Google Scholar]
- 10.Neubert S. Automation requires process information technologies [Internet] Rostock: Center for Life Science Automation (celisca); c2016. [cited at 2017 Jan 25]. Available from: http://139.30.204.254/celisca/index.php?id=987. [Google Scholar]
- 11.Indiegogo. Hicon smartwristband with social network icons [Internet] San Francisco (CA): Indiegogo; 2015. [cited at 2017 Jan 25]. Available from: https://www.indiegogo.com/projects/hicon-smartwristband-with-social-network-icons#/ [Google Scholar]
- 12.Anliker U, Ward JA, Lukowicz P, Troster G, Dolveck F, Baer M, et al. AMON: a wearable multiparameter medical monitoring and alert system. IEEE Trans Inf Technol Biomed. 2004;8(4):415–427. doi: 10.1109/titb.2004.837888. [DOI] [PubMed] [Google Scholar]
- 13.Gas sensor developer kit [Internet] Newark (CA): Spec Sensors; c2015. [cited at 2017 Jan 25]. Available from: https://www.spec-sensors.com/product-category/gassensor-developer-kits/ [Google Scholar]
- 14.To G, Mahfouz MR. Modular wireless inertial trackers for biomedical applications; Proceedings of 2013 IEEE Topical Conference on Power Amplifiers for Wireless and Radio Applications (PAWR); 2013 Jan 20-23; Austin, TX. pp. 172–174. [Google Scholar]
- 15.Veltink PH, Boom HB. 3D movement analysis using accelerometry theoretical concepts. In: Pedotti A, Ferrarin M, Quintern J, Reiner R, editors. Neuroprosthetics: from basic research to clinical applications. Berlin: Springer; 1996. pp. 317–326. [Google Scholar]
- 16.Foerster F, Smeja M, Fahrenberg J. Detection of posture and motion by accelerometry: a validation study in ambulatory monitoring. Comput Human Behav. 1999;15(5):571–583. [Google Scholar]
- 17.Mathie MJ, Coster AC, Lovell NH, Celler BG. Detection of daily physical activities using a triaxial accelerometer. Med Biol Eng Comput. 2003;41(3):296–301. doi: 10.1007/BF02348434. [DOI] [PubMed] [Google Scholar]
- 18.Uswatte G, Miltner WH, Foo B, Varma M, Moran S, Taub E. Objective measurement of functional upper-extremity movement using accelerometer recordings transformed with a threshold filter. Stroke. 2000;31(3):662–667. doi: 10.1161/01.str.31.3.662. [DOI] [PubMed] [Google Scholar]
- 19.Miyazaki S. Long-term unrestrained measurement of stride length and walking velocity utilizing a piezoelectric gyroscope. IEEE Trans Biomed Eng. 1997;44(8):753–759. doi: 10.1109/10.605434. [DOI] [PubMed] [Google Scholar]
- 20.Mayagoitia RE, Nene AV, Veltink PH. Accelerometer and rate gyroscope measurement of kinematics: an inexpensive alternative to optical motion analysis systems. J Biomech. 2002;35(4):537–542. doi: 10.1016/s0021-9290(01)00231-7. [DOI] [PubMed] [Google Scholar]
- 21.Takeda R, Tadano S, Todoh M, Morikawa M, Nakayasu M, Yoshinari S. Gait analysis using gravitational acceleration measured by wearable sensors. J Biomech. 2009;42(3):223–233. doi: 10.1016/j.jbiomech.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 22.Roetenberg D. Inertial and magnetic sensing of human motion [dissertation] Enschede: University of Twente; 2006. [Google Scholar]
- 23.Altun K, Barshan B, Tuncel O. Comparative study on classifying human activities with miniature inertial and magnetic sensors. Pattern Recognit. 2010;43(10):3605–3620. [Google Scholar]
- 24.Kaewkannate K, Kim S. A comparison of wearable fitness devices. BMC Public Health. 2016;16:433. doi: 10.1186/s12889-016-3059-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stables J. Best fitness trackers 2015: Jawbone, Misfit, Fitbit, Germin and more [Internet] place unknown: publisher unknown; 2015. [cited at 2017 Jan 25]. Available from: https://www.iworldonline.com.au/index.php/blog/best-fitness-trackers-2015-jawbone-misfit-fitbit-garmin-and-more/ [Google Scholar]
- 26.Misfit Shine Fitness + Sleep Monitor [Internet] Burlingame (CA): Misfit; 2015. [cited at 2017 Jan 25]. Available from: http://misfit.com/products/shine?locale=en. [Google Scholar]
- 27.STMicroelectronics. Ultra-compact high-performance eCompass module: 3D accelerometer and 3D magnetometer [Internet] Geneva: STMicroelectronics; 2013. [cited at 2017 Jan 25]. Available from: http://www.st.com/content/ccc/resource/technical/document/datasheet/56/ec/ac/de/28/21/4d/48/DM00027543.pdf/files/DM00027543.pdf/jcr:content/translations/en.DM00027543.pdf. [Google Scholar]
- 28.STMicroelectronics. MEMS motion sensor: ultra-stable three-axis digital output gyroscope (L3G4200D) [Internet] Geneva: STMicroelectronics; 2010. [cited at 2017 Jan 25]. Available from: http://www.st.com/content/ccc/resource/technical/document/datasheet/04/46/d6/00/be/d9/46/ae/CD00265057.pdf/files/CD00265057.pdf/jcr:content/translations/en.CD00265057.pdf. [Google Scholar]
- 29.Bertolotti GM, Cristiani AM, Colagiorgio P, Romano F, Bassani E, Caramia N, et al. A wearable and modular inertial unit for measuring limb movements and balance control abilities. IEEE Sens J. 2016;16(3):790–797. [Google Scholar]
- 30.Slaughter S, Hilbert C, Jouett N, McEwen M. Quantifying and learning human movement characteristics for fall prevention in the elderly using Inertial Measurement Units and Neural Networks; Proceedings of the 2nd International Conference of Education, Research and Innovation (ICERI); 2009 Nov 16-18; Madrid, Spain. pp. 978–984. [Google Scholar]
- 31.Aziz O, Park EJ, Mori G, Robinovitch SN. Distinguishing near-falls from daily activities with wearable accelerometers and gyroscopes using Support Vector Machines. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:5837–5840. doi: 10.1109/EMBC.2012.6347321. [DOI] [PubMed] [Google Scholar]
- 32.Frank K, Diaz EM, Robertson P, Sanchez FJ. Bayesian recognition of safety relevant motion activities with inertial sensors and barometer; Proceedings of 2014 IEEE/ION Position, Location and Navigation Symposium (PLANS); 2004 May 5-8; Monterey, CA. pp. 174–184. [Google Scholar]
- 33.Yun X, Bachmann ER, Moore H, Calusdian J. Self-contained position tracking of human movement using small inertial/magnetic sensor modules; Proceedings of 2007 IEEE International Conference on Robotics and Automation; 2007 Apr 10-14; Rome, Italy. pp. 2526–2533. [Google Scholar]
- 34.Epelde G, Carrasco E, Rajasekharan S, Jimenez JM, Vivanco K, Gomez-Fraga I, et al. Universal remote delivery of rehabilitation: validation with seniors' joint rehabilitation therapy. Cybern Syst. 2014;45(2):109–122. [Google Scholar]
- 35.Reiss A, Stricker D. Aerobic activity monitoring: towards a long-term approach. Univers Access Inf Soc. 2014;13(1):101–114. [Google Scholar]
- 36.Schall MC, Jr, Fethke NB, Chen H, Oyama S, Douphrate DI. Accuracy and repeatability of an inertial measurement unit system for field-based occupational studies. Ergonomics. 2016;59(4):591–602. doi: 10.1080/00140139.2015.1079335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schulze M, Calliess T, Gietzelt M, Wolf KH, Liu TH, Seehaus F, et al. Development and clinical validation of an unobtrusive ambulatory knee function monitoring system with inertial 9DoF sensors. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:1968–1971. doi: 10.1109/EMBC.2012.6346341. [DOI] [PubMed] [Google Scholar]
- 38.Dadashi F, Millet GP, Aminian K. Estimation of front-crawl energy expenditure using wearable inertial measurement units. IEEE Sens J. 2014;14(4):1020–1027. [Google Scholar]
- 39.Martin J. Best fitness trackers 2016: what's the best fitness tracker? The 20 Fitness bands & activity trackers you can buy in UK today [Internet] London: PC Advisor; c2016. [cited at 2017 Jan 25]. Available from: http://www.pcadvisor.co.uk/test-centre/wearable-tech/best-fitnessfitnesstrackers-2016-uk-summary-april-3498368/ [Google Scholar]
- 40.Bennett B. Fitbit Flex review [Internet] San Francisco (CA): Cnet.com; 2013. [cited at 2017 Jan 25]. Available from: https://www.cnet.com/products/fitbit-flex/ [Google Scholar]
- 41.Withings Inspire Health. Pulse Ox track improve [Internet] Issy-les-Moulineaux: Withings Inspire Health; 2015. [cited at 2017 Jan 25]. Available from: http://www.withings.com/eu/en/products/pulse? [Google Scholar]
- 42.2016 Best fitness trackers reviews: review & comparisons [Internet] New York (NY): TopTenReviews.com; 2015. [cited at 2017 Jan 25]. Available from: http://fitness-trackers-review.toptenreviews.com/ [Google Scholar]
- 43.Jawbone. There's a better version of you out there: get up and find it [Internet] [place unknown]: Jawbone; 2014. [cited at 2017 Jan 25]. Available from: https://twitter.com/jawbone/status/548633718261161985. [Google Scholar]
- 44.Spinelle L, Gerboles M, Villani MG, Aleixandre M, Bonavitacola F. Field calibration of a cluster of low-cost available sensors for air quality monitoring. Part A: Ozone and nitrogen dioxide. Sens Actuators B Chem. 2015;215:249–257. [Google Scholar]
- 45.Chen M, Ma Y, Song J, Lai CF, Hu B. Smart clothing: connecting human with clouds and big data for sustainable health monitoring. Mob Netw Appl. 2016;21(5):825–845. [Google Scholar]
- 46.Wan J, Zhang D, Sun Y, Lin K, Zou C, Cai H. VCMIA: a novel architecture for integrating vehicular cyber-physical systems and mobile cloud computing. Mob Netw Appl. 2014;19(2):153–160. [Google Scholar]
- 47.Peng L, Youn CH, Tang W, Qiao C. A novel approach to optical switching for intradatacenter networking. J Lightwave Technol. 2012;30(2):252–266. [Google Scholar]
- 48.Sanfilippo F, Pettersen KY. A sensor fusion wearable health-monitoring system with haptic feedback; Proceedings of 2015 11th International Conference on Innovations in Information Technology (IIT); 2015 Nov 1-3; Dubai, UAE. pp. 262–266. [Google Scholar]
- 49.Arduino: an open-source electronics prototyping platform [Internet] [place unknown]: Arduino; c2017. [cited at 2017 Jan 25]. Available from: http://arduino.cc/ [Google Scholar]
- 50.Cooking Hacks. e-Health Sensor Platform Complete Kit [Internet] Zaragoza: Cooking Hacks; 2015. [cited at 2017 Jan 25]. Available from: https://www.cooking-hacks.com/ehealth-sensors-complete-kit-biometric-medical-arduino-raspberry-pi. [Google Scholar]
- 51.Cooking Hacks. e-Health Sensor Shield [Internet] Zaragoza: Cooking Hacks; 2015. [cited at 2017 Jan 25]. Available from: https://www.cooking-hacks.com/ehealth-sensor-shield-biometric-medical-arduino-raspberry-pi. [Google Scholar]