Abstract
Federal law now requires FDA to disseminate information on chemicals in cigarette smoke, but it is unclear how best to do so. In a 2 × 2 between-subjects experiment, participants received a message about chemicals in cigarette smoke (e.g., “Cigarette smoke has benzene.”) along with an additional randomly assigned messaging strategy: a “found-in” (e.g., “This is found in gasoline.”), a health effect (e.g., “This causes heart disease.”), both, or neither. Participants were U.S. probability phone samples of 5000 adults and 1123 adolescents, and an online convenience sample of 4130 adults. Adding a health effect elicited greater discouragement from wanting to smoke cigarettes (all p < .05) as did adding a found-in (all p < .05). However, including both messaging strategies added little or nothing above including just one. These findings can help the FDA and other agencies develop effective and parsimonious messages about cigarette smoke constituents.
Keywords: Tobacco control, Cigarette smoke constituents, Health communication, Common products, Health effects
Introduction
Globally, cigarette smoking causes 6.3 million deaths annually, including 602,000 from exposure to secondhand smoke (Lim et al., 2012). The fundamental source of the harm from smoking is the array of thousands of constituents (chemicals and other toxic components) in cigarette smoke, including at least 72 carcinogens (Rodgman & Perfetti, 2013; Hecht, 2012). The general public knows little about what is in constituent smoke, with most people only being able to reliably identify carbon monoxide, nicotine, and “tar” (Hall et al., 2014). Only one-third of American smokers know that cigarette smoke contains ammonia and arsenic and fewer know it contains lead, mercury, or radioactive elements (Cummings et al., 2004; Siahpush, 2006). The general public also has limited knowledge about the many health effects of smoking—for example, only 40 % reported knowing that smoking can cause impotence (ITC Project, 2014).
Many smokers want to learn more about the constituents in smoke (Crawford et al., 2002). Prior studies have found that health communication campaigns that include constituent information have the potential to both increase knowledge and reduce smoking intentions (Siahpush, 2006; Swayampakala et al., 2015; Thrasher et al., 2013). Recognizing the potential utility of health messages about constituents, the Food and Drug Administration (FDA) recently launched “The Real Cost” youth tobacco prevention campaign, which highlights the presence and harmful effects of toxic constituents in cigarette smoke (FDA, 2014).
Guidelines for Article 10 of the WHO Framework Convention on Tobacco Control (FCTC) require each member to disclose information about the toxic constituents and emissions of tobacco products to inform the public about the “health consequences, addictive nature, and mortal threat” posed by smoking and smoke exposure (WHO Working Group 2014). Multiple countries now require constituent messages on cigarette packs. For example, Australian cigarette packs have messages such as “WARNING: BDE (1,3 Butadiene) is found in large amounts in tobacco smoke. BDE causes leukaemia and other cancers.” Mexico has implemented constituent-related messages including “CONTAINS THALLIUM: Poison used in rat poison and insecticides.” The example from Australia provides the name of the constituent and then describes a negative health effect associated with exposure to it whereas the example from Mexico explains that the constituent thallium, which is found in cigarettes, is also found in rat poison. It is currently unclear which type of messaging strategy most effectively conveys the risks of cigarette smoking and whether both strategies together are more effective in eliciting quit intentions and behavior.
The U.S. Family Smoking Prevention and Tobacco Control Act gave the FDA authority to require tobacco companies to provide constituent information to consumers, such as on cigarette packs (Family Smoking Prevention et al., 2009). Because most constituents have technical-sounding names that are unfamiliar to the lay public, learning that cigarette smoke contains a particular constituent is often either uninformative or results in individuals inferring meaning and potential harms that may have little factual basis (Moracco et al., 2016). In other words, unless one is a chemist, a list of chemical names alone is often not useful to lay people. Given the high smoking rate among less educated Americans, constituent information without context is likely to be of little use to those who need it most (Jamal et al., 2015).
Although both of the health effect and “found-in” messaging strategies are widely employed, no published studies to date have explicitly tested whether these two strategies, either separately or in combination, are more effective in discouraging smoking than a message with a constituent by itself. The elaboration likelihood model suggests that when individuals are motivated and cognitively capable of assessing a health message's arguments, they process the message with a greater degree of elaboration, often leading to long-term changes in corresponding attitudes and beliefs (Jones et al., 2003; Petty and Cacioppo, 1986). Otherwise, changes are more short-lived. We expect that adding a health effect or found-in strategy to a constituent message would increase an individual's motivation to think about and process the message, leading to a greater impact on smoking-related attitudes and beliefs than a message that simply presents the name of a constituent. Constituent messages with both strategies may be more potent than those with only one.
Several studies have examined the effectiveness of different types of pictorial warning labels for cigarette smoking and the psychological processes through which these labels impact smoking behaviors (Cameron et al., 2015; Noar et al., 2016). However, researchers have not examined the most effective types of constituent disclosures that could be integrated into or supplement graphic warning labels, a critical research need for FCTC implementation (Hammond et al., 2013). Our study sought to address this research gap on constituent messaging strategies. Using three national U.S. samples, we presented messages about cigarette smoke constituents that experimentally varied health effect and found-in strategies. Because the impact of health messages sometimes varies by demographic factors such as socioeconomic status, sex, and smoking status (Huang & Shen 2016; Spence et al., 2013; Toll et al., 2008; Viswanath and Ackerson, 2011), we also explored the relative effectiveness of these strategies across selected subpopulations.
Methods
Participants
From September 2014 to June 2015, we recruited a U.S. national sample of 5014 adults (ages 18 and older) using random digit dial landline and cell phone frames. Details on sampling design and survey methods are available elsewhere (Boynton et al., 2016). In parallel, using a multiframe approach with both random digit dial and list assisted sampling frames, we recruited a national population-based sample of 1125 adolescents. We also recruited an online convenience sample of 4137 adults in October 2014 using Amazon Mechanical Turk (www.mturk.com). Due to missing data on the outcome variable, the sample sizes for analyses were 5000 (adult phone), 1123 (adolescent phone), and 4130 (adult online).
Procedures
Interviewers obtained verbal consent from respondents and, for adolescents, also from a parent or guardian. In a 2 × 2 between-subjects factorial experiment, participants received one randomly-assigned message about a harmful constituent in cigarette smoke. The first experimental factor manipulated whether the message included a health effect (e.g., permanent breathing problems) associated with a given constituent. The second experimental factor manipulated whether the message described a constituent's familiar use or source that we refer to as a “found in” (e.g., fertilizer). Thus, participants received a message with information about a constituent in one of four conditions: either, both, or neither (control) of the health effect and found-in messaging strategies corresponding to that constituent. To ensure that the results were not idiosyncratic to a particular constituent, each message focused on one of six randomly assigned constituents (i.e., acrolein, ammonia, benzene, crotonaldehyde, formaldehyde, or naphthalene). We selected these constituents from the FDA's list of harmful and potentially harmful cigarette and cigarette smoke constituents (FDA, 2012). The message elements appear in Table 1. Participants in the phone surveys heard messages over the phone, while those in the online survey read them as text on a screen. An example of a message with both strategies is, “Cigarette smoke has ammonia. This is found in fertilizer and causes permanent breathing problems.” “Cigarette smoke has acrolein,” is an example of a control message. The IRB at the University of North Carolina approved all three studies.
Table 1.
Constituent message components
| Constituent | Found-in | Health effect |
|---|---|---|
| “Cigarette smoke has ...” | “This is ...” | “This causes ...” |
| Ammonia | found in fertilizer | permanent breathing problems |
| Acrolein | found in car exhaust | heart disease |
| Benzene | found in gasoline | heart disease |
| Crotonaldehyde | used to make insecticides | cancer |
| Formaldehyde | used to preserve dead bodies | cancer |
| Naphthalene | used to make toilet bowl deodorizers | permanent breathing problems |
Constituent messages with both strategies presented a found-in followed by the corresponding health effect in a single sentence
Measures
The phone and internet surveys used functionally identical items. The primary outcome was discouragement from wanting to smoke, which was measured with an item asking, “How much does this [the constituent message] discourage you from wanting to smoke?” Response options were “not at all” (coded as 1), “a little” (2), “somewhat” (3), and “a lot” (4). We conducted multiple rounds of cognitive interviews with 18 adult and adolescent smokers and nonsmokers to assess comprehension of the primary outcome measure (Willis, 2005). Participants found the item to be clearly worded and interpreted the item as intended.
The surveys assessed age, sex, race, ethnicity, education (own education for adults and maternal education for adolescents), numeracy, household income (adults only), and smoking status. To assess numeracy, the surveys asked, “In general, which of these numbers shows the biggest risk of getting disease?” (Lipkus et al., 2001). Response options were “1 in 100”, “1 in 1000”, or “1 in 10” (the correct response). We coded participants who answered this question correctly as having high numeracy and others as having low numeracy. For the adult surveys, we defined a current smoker as someone who had smoked at least 100 cigarettes in their life and currently smokes every day or some days; for the adolescent survey, we defined a current smoker as someone who smoked at least once in the past thirty days (Arrozola et al., 2015; Davis et al., 2009).
Statistical analysis
We analyzed data from the three samples separately. To determine whether randomization created equivalent groups, we used multiple logistic and multinomial logistic regression to examine whether five demographic characteristics (sex, race, numeracy, smoking status, and income among adults or maternal education among adolescents) predicted the experimental condition for health effect, found-in, and their interaction in each sample. Across 45 models, 5 associations were statistically significant (all p < .05); because analyses adjusting for the factors involved in these associations (sex, numeracy, smoking status, and income) did not substantively change the experimental results, we present only the unadjusted estimates.
We used 2 × 2 between-subjects factorial ANOVA to examine the impact of the health effect and found-in strategies on discouragement from wanting to smoke and computed partial eta squared to characterize effect sizes. In exploratory analyses, we used three-way ANOVA to examine potential moderators (age and income among adults, sex, race, ethnicity, education, numeracy, and smoking status) of the impact of these strategies on discouragement. The majority of respondents across all three samples selected the highest level of discouragement (“a lot”) in response to their assigned message, resulting in negatively skewed distributions. In order to confirm that this non-normality did not affect our results, we employed the PROC MULTTEST procedure in SAS for post hoc comparisons, using the bootstrap method to adjust p-values for all t-tests. Because this bootstrapping procedure is non-parametric, it is robust to violations of normality. We conducted analyses in March 2015 to February 2016 using SAS (v. 9.4) and unweighted data. All significance tests were two-tailed and used a critical alpha of .05.
Results
Sample characteristics
The mean ages of adult phone and online participants were 45.9 (SD = 17.3) and 33.6 (SD = 10.9). Around one-third (34.2 %) of adult phone participants and many (43.2 %) online participants had a bachelor's or advanced degree (Table 2). In the adolescent sample, 52.3 % had a mother with a bachelor's or advanced degree. A minority of adults (23.0 % phone, 37.8 % online) and adolescents (3.7 %) were smokers.
Table 2.
Sample characteristics
| Adolescent phone n = 1123 % |
Adult phone n = 5000 % |
Adult online n = 4130 % |
|
|---|---|---|---|
| Age (years) | |||
| 13–17 | 100 | – | – |
| 18–25 | – | 16.2 | 24.5 |
| 26–34 | – | 14.9 | 39.8 |
| 35–14 | – | 15.5 | 19.2 |
| 45–54 | – | 19.8 | 9.9 |
| 55–64 | – | 17.9 | 5.6 |
| 65+ | – | 15.7 | 1.0 |
| Male | 49.8 | 47.3 | 49.4 |
| Race | |||
| White | 80.1 | 69.6 | 83.0 |
| Black | 10.6 | 19.6 | 7.6 |
| Native American | 1.6 | 2.7 | 0.9 |
| Asian | 2.0 | 2.1 | 5.0 |
| Other | 5.7 | 6.0 | 3.5 |
| Hispanic | 7.5 | 8.7 | 8.3 |
| Education | |||
| < high school | 4.2 | 10.5 | 1.0 |
| High school degree or equivalent | 16.3 | 24.7 | 12.5 |
| Some college | 17.0 | 20.7 | 30.9 |
| Associate's degree | 10.3 | 9.9 | 12.4 |
| College degree | 31.9 | 21.2 | 33.7 |
| Master's degree | 16.8 | 10.1 | 7.4 |
| Professional or doctoral degree | 3.5 | 2.9 | 2.0 |
| Low numeracy | 27.2 | 32.0 | 8.3 |
| Income, annual | |||
| $0–$24,999 | – | 28.2 | 22.7 |
| $25,000–$49,999 | – | 26.2 | 34.6 |
| $50,000–$74,999 | – | 19.1 | 23.0 |
| $75,000–$99,999 | – | 10.8 | 12.0 |
| $100,000 or more | – | 15.7 | 7.8 |
| Smoker | 3.7 | 23.0 | 37.8 |
For adolescents, education is the mother's highest level of education. For adults, being a smoker is defined as having ever smoking at least 100 cigarettes and currently smoking every day or some days for adults. For adolescents, it is defined as having smoked at least 1 of the past 30 days
Adolescent phone survey
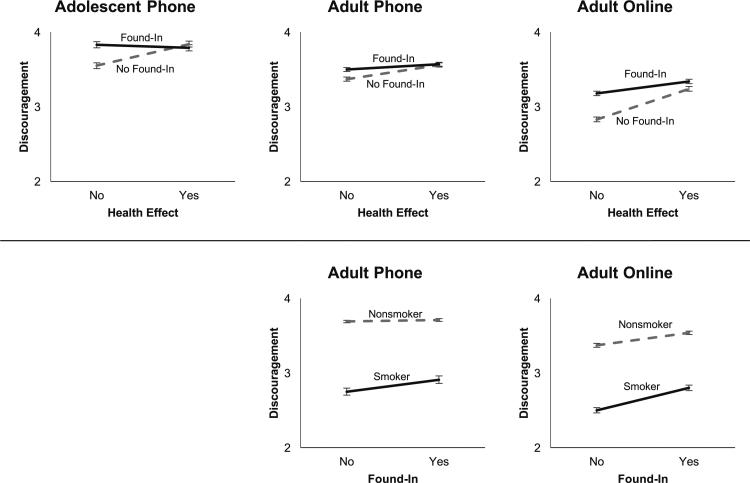
Adolescents who received a message with a health effect had higher discouragement (M = 3.82, SD = 0.62) than those who did not (M = 3.69, SD = 0.71; p = .002), and those who received a message with a found-in had higher discouragement (M = 3.81, SD = 0.62) than adolescents who did not (M = 3.69, SD = 0.71; p = .003; Table 3). The effect sizes were similar for health effect and found-in . Found-in strategies moderated the impact of health effect strategies (p < .001; Fig. 1, Panel 1). Post-hoc analyses showed that messages with only a health effect elicited greater discouragement than messages with neither strategy (p < .001). Messages with only a found-in or both strategies did not differ from each other.
Table 3.
Impact of health effect and found-in messaging strategies on discouragement from wanting to smoke
| Adolescent phone |
Adult phone |
Adult online |
||||
|---|---|---|---|---|---|---|
| df | F | df | F | df | F | |
| Health effect | 1 | 9.91* | 1 | 6.21* | 1 | 89.67** |
| Found-in | 1 | 8.94* | 1 | 24.41** | 1 | 52.05** |
| Health effect × found-in | 1 | 17.66** | 1 | 6.08* | 1 | 15.85** |
Adolescent phone: n = 1123; Adult phone: n = 5000; Adult online: n = 4130. df = degrees of freedom
p < 0.05
p < 0.001
Fig. 1.
Panel 1 (top): Interaction between health effect and found-in strategies. Panel 2 (bottom): Interaction between found-in and smoking status. Error bars show standard errors
Adult phone survey
Adults who received a message with a health effect had higher discouragement (M = 3.57, SD = 0.91) than those who did not (M = 3.43, SD = 1.00; p < .001). Those who received a message with a found-in had higher discouragement (M = 3.54, SD = 0.94) than adults who did not (M = 3.47, SD = 0.97; p = .01; Table 3). The health effect strategy accounted for somewhat more variance in discouragement than the found-in strategy . The impact of health effect strategies was moderated by found-in strategies (p = .01; Fig. 1, Panel 1). Post-hoc analyses showed that messages with only a health effect caused higher discouragement than messages with neither strategy (p < .001). Messages with a found-in only or both strategies were not different from each other.
Nonsmokers (M = 3.71, SD = 0.78) were more discouraged than smokers (M = 2.83, SD = 1.16; F(1, 4985) = 858, p < .001). In exploratory analyses, we found that the interaction between found-in and smoking status was statistically significant (F(1,4985) = 5.33, p = .02; Fig. 1, Panel 2). Smokers who received a message with a found-in (M = 3.71, SD = 0.78) had higher discouragement than those who heard a message without a found-in (M = 3.70, SD = 0.77; p = .02), but nonsmokers had overall high discouragement that did not differ by found-in condition.
Adult online survey
Adults who viewed a message with a health effect had higher discouragement (M = 3.29, SD = 0.94) than those who did not (M = 3.01, SD = 1.04; p < .001), and those who received a message with a found-in had higher discouragement (M = 3.26, SD = 0.96) than those who did not (M = 3.04, SD = 1.03; p < .001; Table 3). Health effect accounted for more variance in discouragement than found-in . Found-in strategies moderated the impact of health effect strategies (p < .001; Fig. 1, Panel 1). In post hoc analyses, messages with only a health effect impacted discouragement more than messages with neither strategy (p < .001). Messages with both strategies also elicited greater discouragement than messages with only a found-in (p < .001), but this difference was smaller than the previous effect.
Nonsmokers (M = 3.45, SD = 0.85) were more discouraged than smokers (M = 2.65, SD = 1.01; F(1, 4117) = 806, p < .001). Exploratory analyses found that the interaction between found-in and smoking status was statistically significant (F(1,4117) = 7.51, p = .006; Fig. 1, Panel 2). Post-hoc analyses showed that smokers who received a message with a found-in (M = 2.80, SD = 1.02) had higher discouragement than those who received a message with no found-in (M = 2.50, SD = 0.99, p < .001). Similarly, nonsmokers (M = 3.54, SD = 0.80) who received a found-in were more discouraged than those who did not (M = 3.37, SD = 0.90, p < .001).
Discussion
Across three national samples, both health effect and found-in strategies discouraged people from wanting to smoke. The health effect strategy elicited somewhat higher discouragement than the found-in strategy. Across all three studies, messages with only a health effect caused higher discouragement than messages without either strategy. Messages with only a found-in or both strategies also elicited high discouragement, but only in the adult online survey did messages with both strategies have a greater impact than those with a found-in only. Therefore, messages with only a health effect discourage people from wanting to smoke. Adding a found-in alongside a health effect is unlikely to enhance the impact of messages that people hear. In print materials, using both strategies may offer some small added benefit.
We also explored smoking status as a moderator of the effects of the strategies. The prevalence of smoking among adults in our study (23–38 %) was somewhat higher than national estimates for a similar time period (17 %; Jamal et al., 2015). In the adult surveys, smoking status moderated the effect of the found-in strategy on discouragement from wanting to smoke. That is, smokers who received a message with a found-in had higher discouragement than those who received a message without a found-in but remained far less discouraged overall than nonsmokers in both adult surveys. In the adult online survey only, nonsmokers who received found-in strategies had higher discouragement than those who did not. These analyses suggest that found-in strategies may be processed differently by smokers and nonsmokers, which may not be the case for health effect strategies. These findings have practical importance for constituent messages in health education campaigns and related public health efforts. When space or message length is a concern, health effect strategies should be prioritized over found-in strategies because health-effect strategies were equally potent for smokers and non-smokers.
Strengths and limitations
Study strengths include the experimental design and reliable replication of our findings across three large national samples of diverse adults and adolescents and across two data collection modes. Another strength of the study is that the health effect and found-in strategies varied across six cigarette smoke constituents, which increases the robustness of our findings. The main limitation of the study is the hypothetical nature of the experiment. Additional work is needed to show whether our findings will replicate in field studies that examine smoking behavior. Use of a single item to assess the main outcome is also a limitation. Although, cognitive testing among a diverse group of people found the item to be well understood, and using multiple items would only add statistical power not reduce it.
Conclusions
Our studies respond directly to the call for studies to identify effective messages about cigarette smoke constituents (Hammond et al., 2013). The findings are congruent with previous research indicating that qualitative messages providing context about chemicals in cigarette smoke are more effective than messages providing only chemical names (Hammond et al., 2013). As FCTC signatories continue to advance and improve their policies, our findings can inform effective message design. Using either health effect or found-in strategies is more effective than simply stating the chemical name. Thus, regulatory disclosures and other communication messages should include at least one of these message strategies to maximize comprehension. The choice of strategy may depend on the audience and the available space for text. It is also possible that, over time, the impact of message novelty may trump differences between types of strategies; therefore, varying message strategies and content may be a superior approach. Rotating and replacing messages over time is important in preventing the “wear-out” of messages (Borland et al., 2009).
Future research should identify specific constituents, health effects and found-in strategies that are most effective in discouraging smoking among the public. Research should also explore the utility of other messaging strategies, such as those about how long a constituent stays in the body or how it causes a particular health problem. Additionally, research should explore whether health effect and found-in strategies are effective with other key health disparity populations such as sexual minorities that have higher rates of cigarette smoking than the national smoking average (Lee et al., 2009). Other important tasks will be to assess the effect of messaging on smoking behavior, both in reducing initiation and encouraging and supporting cessation. This work may lead to improved understanding of the underlying psychological mechanisms by which constituent messaging works. Finally, to support international tobacco control efforts, further research should determine whether our findings are replicated in other cultural and national contexts.
Acknowledgments
Research reported in this publication was supported by grant number P50CA180907 from the National Cancer Institute and FDA Center for Tobacco Products (CTP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Compliance with ethical standards
Conflict of interest Sabeeh A. Baig, M. Justin Byron, Marcella H. Boynton, Noel T. Brewer, and Kurt M. Ribisl declare that they have no conflict of interest.
Human and animal rights and Informed consent All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- Arrozola R, Singh T, Corey C, Husten C, Neff L, Apelberg B, et al. Tobacco use among middle and high school students—United States, 2011–2014. MMWR. Morbidity And Mortality Weekly Report. 2015;64:381–385. [PMC free article] [PubMed] [Google Scholar]
- Borland R, Wilson N, Fong GT, Hammond D, Cummings KM, Yong H-H, et al. Impact of graphic and text warnings on cigarette packs: Findings from four countries over five years. Tobacco Control. 2009;18:358–364. doi: 10.1136/tc.2008.028043. doi:10.1136/tc.2008.028043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boynton MH, Agans RP, Bowling JM, Brewer NT, Sutfin EL, Goldstein AO, et al. Understanding how perceptions of tobacco constituents and the FDA relate to effective and credible tobacco risk messaging: A national phone survey of U.S. adults, 2014–2015. BMC Public Health. 2016 doi: 10.1186/s12889-016-3151-5. doi:10.1186/s12889-016-3151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron LD, Pepper JK, Brewer NT. Responses of young adults to graphic warning labels for cigarette packages. Tobacco Control. 2015;24:e14–e22. doi: 10.1136/tobaccocontrol-2012-050645. doi:10.1136/tobaccocontrol-2012-050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford M, Balch G, Mermelstein R. Responses to tobacco control policies among youth. Tobacco Control. 2002;11:14–19. doi: 10.1136/tc.11.1.14. doi:10.1136/tc.11.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings KM, Hyland A, Giovino G, Hastrup J, Bauer J, Bansal M. Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine & Tobacco Research. 2004;6:333–340. doi: 10.1080/14622200412331320734. doi:10.1080/14622200412331320734. [DOI] [PubMed] [Google Scholar]
- Davis S, Malarcher A, Thorne S, Maurice E, Trosclair A, Mowery P. State-specific prevalence and trends in adult cigarette smoking—United States, 1998–2007. JAMA. 2009;302:250–252. [Google Scholar]
- [22 July 2016];Family Smoking Prevention and Tobacco Control Act., Pub. L. No. 111–31. 2009 https://www.gpo.gov/fdsys/pkg/PLAW-111publ31/pdf/PLAW-111publ31.pdf.
- FDA Harmful and potentially harmful constituents in tobacco products and tobacco smoke; established list. 77 FR 20034. 2012.
- FDA FDA launches its first national public education campaign to prevent, reduce youth tobacco use. 2014 http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm384049.htm.
- Hall MG, Ribisl KM, Brewer NT. Smokers’ and nonsmokers’ beliefs about harmful tobacco constituents: implications for FDA communication efforts. Nicotine & Tobacco Research. 2014;16:343–350. doi: 10.1093/ntr/ntt158. doi:10.1093/ntr/ntt158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Wakefield M, Durkin S, Brennan E. Tobacco packaging and mass media campaigns: Research needs for articles 11 and 12 of the WHO framework convention on tobacco control. Nicotine & Tobacco Research. 2013;15:817–831. doi: 10.1093/ntr/nts202. doi:10.1093/ntr/nts202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht SS. Research opportunities related to establishing standards for tobacco products under the family smoking prevention and tobacco control act. Nicotine & Tobacco Research. 2012;14:18–28. doi: 10.1093/ntr/ntq216. doi:10.1093/ntr/ntq216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Shen F. Effects of cultural tailoring on persuasion in cancer communication: A meta-analysis: Cultural tailoring in cancer communication. Journal of Communication. 2016;66:694–715. doi:10.1111/jcom.12243. [Google Scholar]
- ITC Project . ITC United States national report: Findings from the ITC US wave 1 to 8 surveys (2002–2011) Waterloo; Ontario: 2014. [Google Scholar]
- Jamal A, Homa DM, O'Connor E, Babb SD, Caraballo RS, Singh T, et al. Current cigarette smoking among adults—United States, 2005–2014. MMWR. Morbidity and Mortality Weekly Report. 2015;64:1233–1240. doi: 10.15585/mmwr.mm6444a2. doi:10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- Jones LW, Sinclair RC, Courneya KS. The Effects of source credibility and message framing on exercise intentions, behaviors, and attitudes: An integration of the elaboration likelihood model and prospect theory1. Journal of Applied Social Psychology. 2003;33:179–196. doi:10.1111/j.1559-1816.2003.tb02078.x. [Google Scholar]
- Lee JGL, Griffin GK, Melvin CL. Tobacco use among sexual minorities in the USA, 1987 to May 2007: A systematic review. Tobacco Control. 2009;18:275–282. doi: 10.1136/tc.2008.028241. doi:10.1136/tc.2008.028241. [DOI] [PubMed] [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. doi:10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Medical Decision Making: An International Journal of the Society for Medical Decision Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. doi:10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- Moracco KE, Morgan JC, Mendel J, Teal R, Noar SM, Ribisl KM, et al. My first thought was croutons: Perceptions of cigarettes and cigarette smoke constituents among adult smokers and nonsmokers. Nicotine & Tobacco Research. 2016;18(7):1566–1574. doi: 10.1093/ntr/ntv281. doi:10.1093/ntr/ntv281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: A meta-analysis of experimental studies. Tobacco Control. 2016;25:341–354. doi: 10.1136/tobaccocontrol-2014-051978. doi:10.1136/tobaccocontrol-2014-051978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petty RE, Cacioppo JT. Communication and Persuasion: Central and Peripheral Routes to Attitude Change. Springer New York; New York, NY: 1986. The Elaboration likelihood model of persuasion. pp. 1–24. doi:10.1007/978-1-4612-4964-1_1. [Google Scholar]
- Rodgman A, Perfetti TA. The chemical components of tobacco and tobacco smoke. 2nd ed. CRC Press; Boca Raton, FL: 2013. [31 August 2016]. 10.1201/b13973-1. [Google Scholar]
- Siahpush M. Socioeconomic and country variations in knowledge of health risks of tobacco smoking and toxic constituents of smoke: results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15(suppl_3):iii65–iii70. doi: 10.1136/tc.2005.013276. doi:10.1136/tc.2005.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence PR, Lachlan KA, Spates SA, Lin X. Intercultural differences in responses to health messages on social media from spokespeople with varying levels of ethnic identity. Computers in Human Behavior. 2013;29(3):1255–1259. doi:10.1016/j.chb.2012.12.013. [Google Scholar]
- Swayampakala K, Thrasher JF, Hammond D, Yong H-H, Bansal-Travers M, Krugman D, et al. Pictorial health warning label content and smokers’ understanding of smoking-related risks–a cross-country comparison. Health Education Research. 2015;30(1):35–45. doi: 10.1093/her/cyu022. doi:10.1093/her/cyu022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Murukutla N, Pérez-Hernández R, Alday J, Arillo-Santillán E, Cedillo C, et al. Linking mass media campaigns to pictorial warning labels on cigarette packages: A cross-sectional study to evaluate effects among Mexican smokers. Tobacco Control. 2013;22:e57–e65. doi: 10.1136/tobaccocontrol-2011-050282. doi:10.1136/tobaccocontrol-2011-050282. [DOI] [PubMed] [Google Scholar]
- Toll B, Salovey P, O'Malley S, Mazure C, Latimer A, McKee S. Message framing for smoking cessation: The interaction of risk perceptions and gender. Nicotine & Tobacco Research. 2008;10:195–200. doi: 10.1080/14622200701767803. doi:10.1080/14622200701767803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanath K, Ackerson LK. Race, ethnicity, language, social class, and health communication inequalities: A nationally-representative cross-sectional study. PLOS ONE. 2011;6:e14550. doi: 10.1371/journal.pone.0014550. doi:10.1371/journal.pone.0014550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Working Group . Partial guidelines for implementation of the Articles 9 and 10 of the WHO framework convention on tobacco control (regulation of the content of tobacco products and regulation of tobacco product disclosures) Switzerland; Geneva: 2014. [Google Scholar]
- Willis GB. Cognitive interviewing: A tool for improving questionnaire design. Sage Publications; Thousand Oaks, CA: 2005. [Google Scholar]