Abstract
An unusual case of a penetrating grass awn in an eyelid of a dog is reported. A 6-month-old mixed breed dog was referred to the Ophthalmology Unit of the Veterinary Teaching Hospital of Camerino University for anorexia, lethargy, left monolateral ocular swelling and pain to the left eye, present from 1 month. Ophthalmic examination of the left eye showed copious and purulent discharge, and ultrasonography revealed the presence of an abscess containing a grass foreign body. The grass awn was surgically removed. Three days after surgery, the dog showed a marked improvement, with a total resolution obtained in 7 days. To the authors’ knowledge, penetrating foreign bodies such as the one of this paper have never been described before in literature.
Keywords: Dog, Foreign body, Grass awn, Lid abscess, Swollen eyelid, Ultrasonography
Riassunto
Questo articolo descrive un particolare caso di corpo estraneo palpebrale di origine vegetale Un cane meticcio di sei mesi di età è stato riferito all’Unità di Oftalmologia dell’Ospedale Veterinario Didattico dell’Università di Camerino per la presenza di anoressia letargia e tumefazione oculare monolaterale sinistra associata a dolore presenti da un mese. L’esame oftalmologico dell’occhio sinistro ha messo in evidenza la presenza di abbondante essudato purulento e la valutazione ultrasonografica ha mostrato la presenza a livello palpebrale di un ascesso contenente un corpo estraneo vegetale che è stato rimosso chirurgicamente. Tre giorni dopo la chirurgia il cane già manifestava un marcato miglioramento con una guarigione completa dopo una settimana. In bibliografia non sono stati mai descritti corpi estranei vegetali penetranti a livello palpebrale come quello riportato nel presente articolo.
Introduction
Grass foreign bodies (FBs) in soft tissue structures represent a fairly frequent problem in veterinary medicine, because they are seldom promptly recognized on initial physical examination or diagnostic imaging evaluation, the signs are non-specific and patients return weeks to months later with complication such as swelling, mass lesion or draining tracts [1, 2].
In most cases, when the ocular region is concerned, the foreign body lies in the anterior segment of the eye, especially cornea and conjunctiva [3, 4].
Intraocular and intraorbital FBs have been previously described mainly in dogs, rarely in cats and occasionally in farm animals [5–12]. In addition, organic FB such as wood, plant material and porcupine quills may also penetrate into the posterior segment of the eye [6, 7].
Regardless of the nature of the FB, the presenting ophthalmic disease is highly variable, depending on the interval between trauma and presentation, degree of anterior and/or posterior segment penetration and retention, or loss of the FB [13–16]. Managing options depend on clinical presentation and range from conservative medical treatment to surgery to remove the FB and/or address concurrent ocular injuries [17–21].
The aim of this study is to present clinical findings, management and outcomes of a penetrating palpebral grass awn in a dog.
Case report
A 6-month-old, male, mixed breed, short-coated dog was referred to the Ophthalmology Unit of the Veterinary Teaching Hospital of the University of Camerino for ophthalmic evaluation. The dog was presented because of left unilateral ocular swelling, pain to the left eye (reluctance and pain elicited with eyelid manipulation), anorexia and lethargy present from the previous month. Physical examination confirmed clinical abnormalities limited to the left eye and eyelids. There was no history or evidence of trauma.
Ophthalmic examination of the left eye showed copious, purulent discharge, slight reduction in palpebral fissure, swollen (about 1 cm in thickness), motionless lower lid, protrusion of third eyelid and ocular discomfort on palpation. At the level of the lateral canthus of the lower lid, a small circular scar of about 2 mm in diameter was present. In addition, the conjunctiva showed a mild degree of chemosis and hyperemia, and cornea showed a mild degree of keratitis. Pupillary size and pupillary light reflexes were normal in both eyes. Menace response was elicited only in the right eye and was not definitive for the diagnosis. Slit lamp biomicroscopy revealed mild corneal edema in the left eye; the intraocular pressures by applanation tonometry were 20 and 18 mmHg in the right and left eye, respectively. Instillation of tropicamide (Visumidriatic® 1%, Visufarma, Rome, Italy) produced good pupillary dilatation and fundus observation by direct and indirect ophthalmoscope was normal.
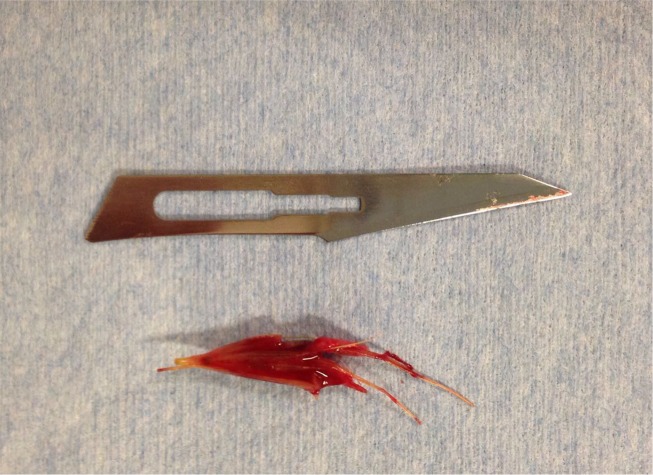
Ocular and orbital ultrasonography was performed using an ultrasonograph (MyLabTM ClassC, Esaote, Genova, Italy) with a multi-frequency linear transducer (4–13 MHz), with the dog in sternal decubitus position, under general anesthesia. The left lower eyelid echogenicity was altered: an ill-marginated, hypoechoic area between muscle fibers, containing two linear reflecting interfaces, was present. This ultrasonogram was compatible with abscess and intra-palpebral grass awn (Fig. 1). A white blood cell count revealed neutrophilia with a left shift of leukocyte formula, possibly related to the intra-palpebral abscess; nevertheless, the dog was carefully examined to rule out other sites of infection that were not found.
Fig. 1.
Ultrasonographic view. Lid appears swollen with ill-marginated, hypoechoic area between muscle fibers and contained two linear reflecting interfaces, compatible with penetrating palpebral grass awn (asterisk indicates anterior chamber, while arrowhead ventral orbital rim)
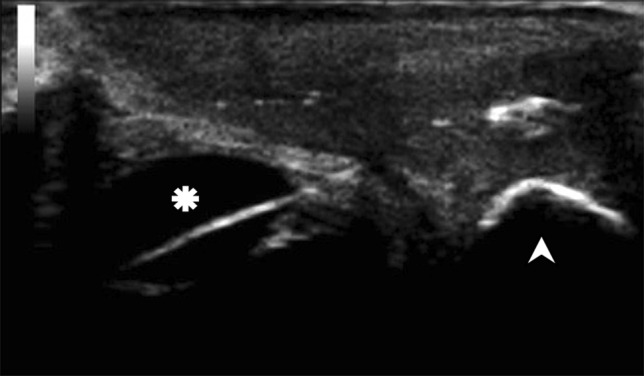
Due to the absence of drainage tract and considering the awn trapped into the muscular planes of the orbicularis oculi, the FB was removed surgically (Fig. 2) with a clamp inserted into the abscess cavity, after soft tissue dissection in the lateral third of the lower lid.
Fig. 2.
Grass awn after surgical removal (scalpel blade number 11)
Immediate post-operative treatment consisted of marbofloxacin 2 mg/kg (Marbocyl®, Vetoquinol Italia, Bertinoro, Italy) q24h for a week, amoxicillin and clavulanic acid 12.5 mg/kg (Synulox®, Zoetis, Rome, Italy) q12h for a week, meloxicam 0.1 mg/kg (Metacam®, Boheringer Ingelheim, Rhein, Germany) q24h for 3 days, and fluocinolone and neomycin eyedrops (Iridex®, Ceva Vetem, Agrate Brianza, Italy) q8h for 5 days.
Three days after surgery, the dog was re-examined and marked improvement occurred; the ocular discharge had ceased, palpebral swelling was reduced and the lower lid regained mobility. The third eyelid protrusion was also resolved, and anorexia and lethargy disappeared.
After a week, the left lower lid returned to normal in appearance and thickness, and the skin incision was completely healed.
Discussion
FBs in subcutaneous and underlying soft tissue structures in animals are a common problem, especially in pets [3, 4, 6, 10, 14] and represent a diagnostic challenge [1, 2, 17, 22, 23].
Regarding the eye and ocular region, FBs are usually located at different portions in the globe, affecting typically the cornea, anterior segment and/or within the orbital space [1, 3–10]; in these cases, the identified materials consist of plant material, wood splinters, glass, gunshot pellets, metallic fragments, porcupine quills and others [6, 7, 17].
Concerning palpebral and periocular FBs, they have been very rarely reported [20, 21] and usually affect hunting dogs [2].
In this paper, a case of an intra-palpebral grass awn in a puppy was reported and, to the authors’ knowledge, penetrating FB such as the one in this report has never been described before in literature.
Ocular reaction to FBs is variable depending on the size and composition, localization, degree of anterior and/or posterior segment penetration and mechanical irritation [4, 13–16].
Inert or hardly accessible foreign bodies, and those that could cause excessive trauma if removed, should be left in situ [4, 21]. Wood and plant material are not inert and usually harbor bacteria and/or fungi that evoke a septic FB reaction, giving rise to a chronic infection [2, 22]. Hunting and working dog breeds are more exposed to this disease because of increased contact with grass awn, and longer coats probably play a role of predisposition to grass awn retention [2].
The most common plant material isolated in ocular anterior segment and adnexa are represented by grass seeds and florets; the sharp anterior end of the floret of the awn can readily penetrates the skin and be retained by the coat of the animal. The barbed nature of the awn prevents retrograde migration and consequently progressive forward migration occurs, promoted by any movement of the animal [1, 2]. The clinical syndromes produced by grass awn migration are varied as evidenced by the numerous locations in which the awn may lodge and the resultant clinical manifestation produced [2]. Within the eye, grass awns usually lodge in the conjunctiva or nictitating membrane [2, 21], while more, in general, grass awns usually lodge in the external ear canal, causing, in some cases, the rupture of the tympanic membrane, or in interdigital spaces, causing draining tracts; grass awns could also be frequently found in the respiratory and also in the thoracic cavity [17–19, 21–24].
The nature, size and position of the retained FBs may be assessed by ophthalmic examination and diagnostic imaging techniques [17, 21]. Radiographic surveys are often the initial diagnostic imaging modality for the detection of metallic FBs, though soft tissue swelling could be the only radiographic finding for different kinds of FBs [1, 21]. Radiography is also able to highlight the presence of underlying bone involvement and occasionally periosteal reaction is visualized [1].
Ultrasonography provides a useful diagnostic tool for identification of both radiopaque and non-radiopaque FBs in soft tissues and can be used successfully in multiple areas of the body, including the eye [21, 22]. Furthermore, FBs are frequently encapsulated and there is exudate surrounding them that helps in identifying them [22].
In this report, the vegetal FB was identified by ultrasonography, and the appearance was similar to that found in other soft tissues, revealing an ill-marked hypoechoic intra-palpebral area with linear hyperechoic structures in it, where the hypoechoic area correspond to the palpebral abscess and the hyperechoic interfaces are due to the awn.
According to the capability of detecting FBs in soft tissue and when there might be a suspicion of it, ultrasonography should always be performed in dogs presenting with a swollen eyelid.
The removal of such kind of FBs could be performed with mini-invasive techniques, ultrasound-guided or surgically. In the first case, the FB could be removed through its draining tract; it is important to position the tip of the forceps close to the awn and repetitive attempts could in fact determine the introduction of air, making awn localization and clamp positioning more difficult [22]. The removal of the FB could be difficult in case of small parts, rupture of the FB during removal attempts or when an accurate tissue dissection is not possible [2, 21, 22].
In the present report, due to the absence of a draining tract and the awn being trapped into the muscular planes of the orbicularis oculi, the FB was completely removed surgically by accurate tissue dissection.
Grass awn poses sometimes a diagnostic challenge for the veterinary ophthalmologist and the use of ultrasonography should always considered when an eyelid appears thickened and inflamed.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All procedures have been executed in accordance with the Regulations on Animal Welfare in Veterinary Practice.
Informed consent
Informed written consent was obtained from the owner of the dog included in the study.
References
- 1.Armbrust LJ, Biller DS, Radlinsky MG, Hoskinson JJ. Ultrasonographic diagnosis of foreign bodies associated with chronic draining tracts and abscesses in dogs. Vet Rad Ultra. 2003;44:66–70. doi: 10.1111/j.1740-8261.2003.tb01452.x. [DOI] [PubMed] [Google Scholar]
- 2.Brennan KE, Ihrke PJ. Grass awn migration in dogs and cats: a retrospective study of 182 cases. JAVMA. 1983;182:1201–1204. [PubMed] [Google Scholar]
- 3.Tetas Pont R, Matas Riera M, Newton R, Donaldson D. Corneal and anterior segment foreign body trauma in dogs: a review of 218 cases. Vet Ophthalmol. 2015;1:1–12. doi: 10.1111/vop.12312. [DOI] [PubMed] [Google Scholar]
- 4.Tovar MC, Huguert E, Gomezi MA. Orbital cellulitis and intraocular abscess caused by migrating grass in a cat. Vet Ophthalmol. 2005;8:353–356. doi: 10.1111/j.1463-5224.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt GM, Dice PF, Koch S. Intraocular lead foreign bodies in four canine eyes. JSAP. 1975;16:33–39. doi: 10.1111/j.1748-5827.1975.tb05713.x. [DOI] [PubMed] [Google Scholar]
- 6.Bussanich MN, Rootman J. Intraocular foreign body in a dog. Can Vet J. 1981;22:207–210. [PMC free article] [PubMed] [Google Scholar]
- 7.Grahn BH, Szentimrey D, Pharr JW, Farrow CS, Fowler D. Ocular and orbital porcupine quills in the dog: a review and case series. Can Vet J. 1995;36:488–493. [PMC free article] [PubMed] [Google Scholar]
- 8.Brightman AH, Mclaughlin SA, Brogdon JD, Ream VB, Szajerski ME. Intraorbital foreign body in the dog: a case report. Vet Med. 1985;80:45–48. [Google Scholar]
- 9.Chaudieu G. Les corps étrangers intra-oculaires. Le Point Vétérinaire. 1994;26:117–124. [Google Scholar]
- 10.Hartley C, McConnel JF, Doust R. Wooden orbital foreign body in a Weimaraner. Vet Ophthalmol. 2007;10:390–393. doi: 10.1111/j.1463-5224.2007.00569.x. [DOI] [PubMed] [Google Scholar]
- 11.Fisher K, Hendrix D. Conjunctivitis and ulcerative keratitis secondary to conjunctival plant foreign bodies in a herd of alpacas (Lama Pacos) Vet Ophthalmol. 2012;15:110–114. doi: 10.1111/j.1463-5224.2011.00939.x. [DOI] [PubMed] [Google Scholar]
- 12.Fazili MR, Buchoo BA, Bhattacharyya HK. Successful management of a delayed case of a corneal foreign body in a cow. Turk J Vet Anim Sci. 2010;34:295–298. [Google Scholar]
- 13.Greven CM, Engelbrecht NE, Slusher MM, Nagy SS. Intraocular foreign bodies: management, prognostic factors and visual outcomes. Ophthalmology. 2000;107:608–612. doi: 10.1016/S0161-6420(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 14.Chen WL, Tseng CH, Wang IJ, Hu FR. Removal of semitranslucent cactus spines embedded in deep cornea with the aid of a fiberoptic illuminator (Brief reports) Am J Ophthalmol. 2002;134:769–771. doi: 10.1016/S0002-9394(02)01676-8. [DOI] [PubMed] [Google Scholar]
- 15.Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Ho AC, Regillo CD. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol. 2008;146:427–433. doi: 10.1016/j.ajo.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 16.Essex RW, Yi Q, Charles PGP, Allen PJ. Post-traumatic endophthalmitis. Ophthalmology. 2004;111:2015–2022. doi: 10.1016/j.ophtha.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 17.Mandell DC, Holt E. Ophthalmic emergencies. Vet Clin North Am Small Anim Pract. 2005;35(2):455–480. doi: 10.1016/j.cvsm.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Rebhun WC. Conjunctival and corneal foreign bodies. VM SAC. 1973;68:874–877. [PubMed] [Google Scholar]
- 19.Cullen CL, Grahn BH. Diagnostic ophthalmology. Right corneal foreign body, secondary ulcerative keratitis, and anterior uveitis. Can Vet J. 2005;46:1054–1055. [PMC free article] [PubMed] [Google Scholar]
- 20.Hendrix DVH (2013) Diseases and Surgery of the Canine Conjunctiva and Nictitating Membrane. In: Veterinary Ophthalmology, 5th edn (ed. Gelatt KN). Ames: John Wiley & Sons, pp 945-975
- 21.Ledbetter EC, Gilger BC. Diseases and surgery of the canine cornea and sclera. In: Gelatt KN, editor. Veterinary ophthalmology. 5. Ames: John Wiley & Sons; 2013. pp. 976–1049. [Google Scholar]
- 22.Gnudi G, Volta A, Bonazzi M, Gazzola M, Bertoni G. Ultrasonographic features of grass awn migration in the dog. Vet Rad Ultra. 2005;46:423–426. doi: 10.1111/j.1740-8261.2005.00077.x. [DOI] [PubMed] [Google Scholar]
- 23.Cerquetella M, Laus F, Paggi E, Zuccari T, Spaterna A, Tesei B. Bronchial vegetal foreign bodies in the dog—localization in 47 cases. JVMS. 2013;75(7):959–962. doi: 10.1292/jvms.12-0494. [DOI] [PubMed] [Google Scholar]
- 24.Caivano D, Bufalari A, Giorgi ME, Conti MB, Marchesi MC, Angeli G, Porciello F, Birettoni F. Imaging diagnosis—transesophageal ultrasound-guided removal of a migrating grass awn foreign body in a dog. Vet Rad Ultra. 2014;55(5):561–564. doi: 10.1111/vru.12088. [DOI] [PubMed] [Google Scholar]