Highlights
-
•
De Garengeot hernia with a groin subcutaneous abscess is rare.
-
•
Appendectomy and herniorrhaphy via the same incision may be more effective.
-
•
Clinicians should consider de Garengeot hernia in patients with a groin hernia.
Keywords: De Garengeot hernia, Femoral hernia, Acute appendicitis, Subcutaneous abscess, Appendectomy, McVay’s technique
Abstract
Introduction
De Garengeot hernia is rare. Although previous reports have suggested various surgical options according to patient condition, comorbidities, surgeon preference, and clinical findings during surgery, a treatment strategy has not been established.
Presentation of case
An 81-year-old woman presented with an irreducible tender mass that was subsequently diagnosed as an incarcerated femoral hernia with a subcutaneous abscess in the right groin. Intraoperative findings revealed a necrotic and perforated appendix strangulated by the femoral ring for which an appendectomy and herniorrhaphy was performed concurrently through the hernia sac. The subcutaneous abscess cavity was washed thoroughly and a drainage tube was placed within it. The patient recovered uneventfully.
Discussion
We suggest that the approach through the inguinal incision in both appendectomy and herniorrhaphy with drainage may be useful in avoiding intra-abdominal contamination in cases of de Garengeot hernia with subcutaneous abscess.
Conclusion
Here, we described a case of de Garengeot hernia with a subcutaneous abscess in the groin. Clinicians should consider de Garengeot hernia in patients with a groin hernia, make an early diagnosis, and promptly provide surgical treatment to reduce the risk of complications.
1. Introduction
De Garengeot hernia, a femoral hernia containing the vermiform appendix, is rare [1]. Preoperative diagnosis of de Garengeot hernia is very difficult because it lacks specific symptoms or imaging findings; thus, it is often diagnosed during the surgery following the diagnosis of atypical incarcerated femoral hernia involving any part of the bowel [2].
The optimal treatment strategy for de Garengeot hernia has not been established, possibly due to its rarity. The use of prosthetic mesh in hernia repair and appendectomy of a non-inflamed appendix remains controversial [3], [4], and previous reports suggested various surgical options: laparoscopic or open hernia repair, with or without mesh, with or without appendectomy determined according to intraoperative findings, status, comorbidities, and previous abdominal surgeries [3], [5], [6], [7]. Moreover, there are few reports of de Garengeot hernia with groin subcutaneous abscess [6].
Here we report a case of de Garengeot hernia with perforated appendicitis and groin subcutaneous abscess. This work has been reported in line with the SCARE criteria [8].
2. Presentation of case
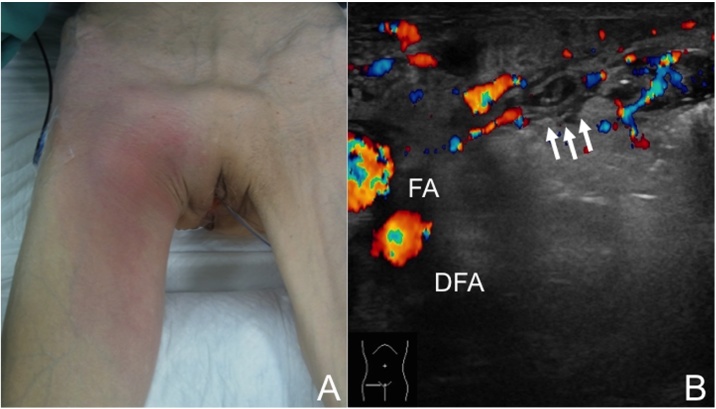
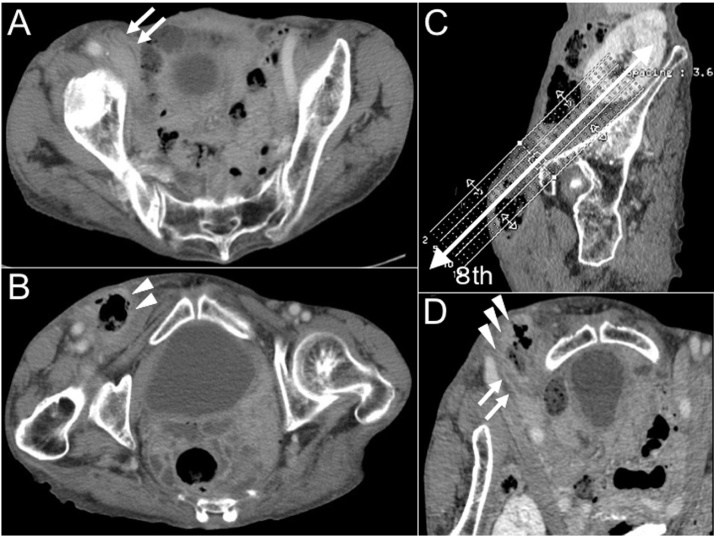
An 81-year-old woman with hypertension, dementia, and a history of hysterectomy for uterine prolapse was admitted for evaluation of right groin pain, difficulty in walking, and fever (38.0 °C). These symptoms started 4 days prior to admission. She had neither abdominal pain nor nausea (vomiting), indicating appendicitis or bowel obstruction. On physical examination, an irreducible mass with tenderness bulged out (6 cm in size) and was located inferior and outer side than the pubic tubercle in the right groin. Moreover, redness and swelling of the skin were evident from the right groin to the anterior portion of the femoral region (Fig. 1A). The laboratory data were as follows: white blood cell count, 8900/μL (normal range, 3400–9500/μL); and C-reactive protein level, 7.68 mg/dL (normal range, <0.5 mg/dL). Ultrasonography revealed a tubular blind-ending structure medial to the femoral artery and a displaced femoral vein (Fig. 1B). An incarcerated femoral hernia involving any part of the bowel was suspected. Abdominal contrast-enhanced computed tomography (CT) revealed a tubular structure passing through the inside of the femoral artery. Moreover, a subcutaneous gas-filled abscess was adjacent to the tip of the structure and spread to the anterior portion of the femoral region (Fig. 2).
Fig. 1.
Physical findings and ultrasonographic image.
(A) An irreducible mass with tenderness bulged out (6 cm in size) and was located inferior and outside the pubic tubercle in the right groin. Redness and swelling of the skin were revealed from the right groin to the anterior portion of the femoral region. (B) A tubular blind-ended structure (white arrows) medial to the femoral artery and vein. The femoral vein was displaced. FA, femoral artery; DFA, deep femoral artery.
Fig. 2.
Computed tomography image.
(A) Contrast-enhanced computed tomography (CT) scan in horizontal view revealing a tubular structure passing through the inside of the right femoral artery (white arrows). (B) The CT scan in horizontal view revealing a gas-filled subcutaneous abscess that was adjacent to the tip of the structure and spread to the anterior portion of the femoral region (white arrow heads). (C) A schema of reconstructed CT images parallel to the femoral canal. (D) The reconstructed CT images in the 8th section of (C) showing a subcutaneous gas-filled abscess (white arrow heads).
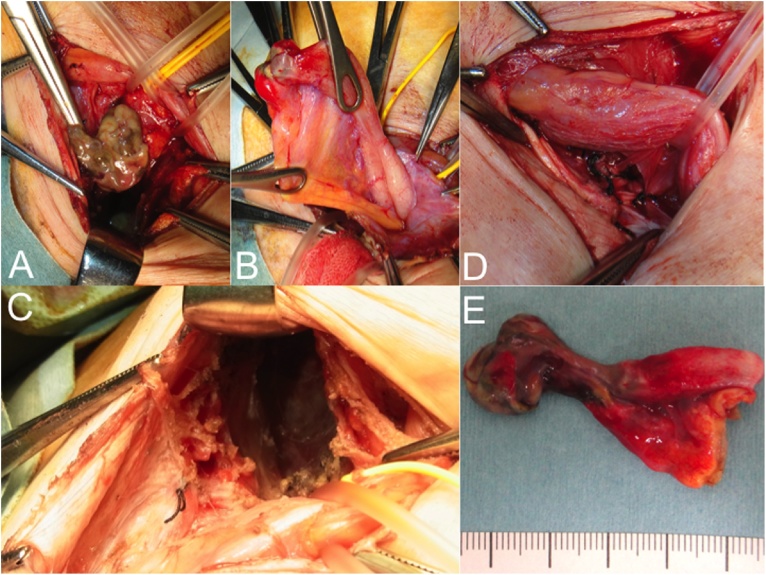
Under the diagnosis of an incarcerated right femoral hernia involving the perforated bowel and groin subcutaneous abscess, the patient consented to undergo emergency surgery. The inguinal canal was opened using the anterior approach and the posterior wall was transected to reach the preperitoneal space. The hernia sac was irreducible and strangulated by the femoral ring. When the inguinal ligament was amputated to open the femoral ring, pus was drained, and the contaminated and decaying hernia sac that contained the necrotic perforated appendix was revealed (Fig. 3A–C). An appendectomy was performed through the hernia sac and the femoral hernia was repaired using McVay’s technique (Fig. 3D). The subcutaneous abscess cavity was washed thoroughly and a drainage tube was placed. Escherichia coli and Bacteroides fragilis were isolated from the pus. Pathological examination revealed gangrenous appendicitis: the incarcerated appendix tip had marked ischemic and necrotic changes with thrombosis throughout the thickness of the wall (Fig. 3E). We carefully monitored the postoperative course owing to the advanced age of the patient. The patient recovered uneventfully and was discharged 14 days postoperatively. Two years after the surgery, she is alive and has no evidence of hernia recurrence.
Fig. 3.
Intraoperative and macroscopic findings.
(A and B) Strangulated hernia sac containing the necrotic and perforated appendix. (C) The subcutaneous abscess cavity in craniocaudal view. (D) Hernia repair with McVay’s technique after appendectomy through the hernia sac. (E) The incarcerated appendix tip had marked ischemic and necrotic changes with thrombosis in the full thickness of the wall.
3. Discussion
De Garengeot hernia, defined as a femoral hernia containing a vermiform appendix [1], was first described by Rene Jacques Croissant De Garengeot in 1731. This entity is rare, reportedly occurring in only about 1% of femoral hernia cases [9]. Moreover, de Garengeot hernia with acute appendicitis is extremely rare, constituting 0.08–0.13% of acute appendicitis cases [10]. It is more common in women, especially postmenopausal women, and often occurs on the right side [11].
The occurrence of bowel obstruction is rare because only the appendix is incarcerated in de Garengeot hernia. Affected patients do not usually have typical symptoms of peritonitis but rather local signs such as erythema and tenderness of the groin because the tight femoral ring that isolates the appendix from the peritoneal cavity prevents the inflammation from spreading throughout the entire intraperitoneal space [3]. The absence of typical clinical symptoms may prevent the preoperative diagnosis of de Garengeot hernia. Most cases of an obtained preoperative diagnosis of de Garengeot hernia have been diagnosed by CT. The following CT findings may help in the diagnosis: a tubular blind-ended structure within a femoral hernia and a low positioned cecum [11], [12].
Although the optimal treatment strategy for de Garengeot hernia has not been established due to its rarity, emergency open appendectomy and herniorrhaphy were performed concurrently through the same inguinal incision as mentioned in most previous reports [11]. The use of prosthetic mesh in hernia repair has been avoided in a contaminated field to prevent infection in cases of abscess or perforation. On the other hand, some reports described that it is possible to use prosthetic mesh in hernia repair when there are no signs of abscess or perforation regardless of appendicular inflammation [10], [13].
De Garengeot hernia with a concurrent groin subcutaneous abscess is extremely rare. To the best of our knowledge, there was only one previous report [6], in which the hernia was treated with laparoscopic appendectomy and open herniorrhaphy using the inguinal approach. Moreover, there are increasing reports of the usefulness of the laparoscopic approach including laparoscopic appendectomy followed by laparoscopic or open hernia repair [4], [6], [14]. Some authors have recommended the laparoscopic approach for the diagnosis and repair of groin hernias with an atypical presentation or when the contents of the hernia cannot be determined using clinical or radiological exams [6], [14]. However, the laparoscopic approach may have a risk of intra-abdominal contamination when the incarcerated appendix is released unexpectedly in cases of subcutaneous abscess. In this case, the hernia was treated with open appendectomy and herniorrhaphy through the same inguinal incision. A drainage tube was placed into the subcutaneous abscess cavity and the patient’s postoperative course was uneventful. We suggest that the approach through the inguinal incision in both appendectomy and herniorrhaphy with drainage may be better for avoiding intra-abdominal contamination in such cases.
Reported postoperative infection rates have reached 29%, while severe complications such as necrotizing fasciitis and death have rarely been described. Wound complications were particularly related to older age, delayed diagnosis, and poor nutritional status [3], [5]. In our case, early diagnosis and treatment might have contributed to the uneventful postoperative course of our elderly patient.
4. Conclusion
This case involved a de Garengeot hernia with concurrent groin subcutaneous abscess. Clinicians should consider de Garengeot hernia in patients with groin hernia, make an early diagnosis, and promptly provide surgical treatment to reduce the risk of complications.
Conflicts of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical approval was obtained from the ethical committee of Tsuchiya General Hospital.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Hiroaki Mashima was involved in writing the article; Masataka Banshodani designed the report and was involved in writing the article; and Masahiro Nishihara, Junko Nambu, Yasuo Kawagushi, Fumio Shimamoto, Kiyohiko Dohi, Keizo Sugino, and Hideki Ohdan provided critical intellectual content for the described work.
Guarantor
Masataka Banshodani.
References
- 1.Akopian G., Alexander M. De Garengeot hernia: appendicitis within a femoral hernia. Am. Surg. 2005;71:526–527. [PubMed] [Google Scholar]
- 2.Talini C., Oliveira L.O., Araújo A.C., Netto F.A., Westphalen A.P. De Garengeothernia: case report and review. Int. J. Surg. Case Rep. 2015;8:35–37. doi: 10.1016/j.ijscr.2014.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma H., Jha P.K., Shekhawat N.S., Memom B., Memom M.A. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11:235–238. doi: 10.1007/s10029-007-0208-5. [DOI] [PubMed] [Google Scholar]
- 4.Ramsingh J., Ali A., Cameron C., Al-Ani A., Hodnett R., Chorushyj C. De Garengeot’s hernia: diagnosis and surgical management of a rare type of femoral hernia. J. Surg. Case Rep. 2014;(February (12)):2. doi: 10.1093/jscr/rju008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen E.T., Komenaka I.K. Strangulated femoral hernia containing a perforated appendix. Can. J. Surg. 2004;47:68–69. [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas B., Thomas M., McVay B., Chivate J. De Garengeot hernia. JSLS. 2009;13:455–457. [PMC free article] [PubMed] [Google Scholar]
- 7.Comman A., Gaetzschmann P., Hanner T., Behrend M. De garengeot hernia: transabdominal preperitoneal hernia repair and appendectomy. JSLS. 2007;11:496–501. [PMC free article] [PubMed] [Google Scholar]
- 8.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg Case Rep. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 9.Tanner N. Strangulated femoral hernia appendix with perforated sigmoid diverticulitis. Proc. R. Soc. Med. 1963;56:1105–1106. doi: 10.1177/003591576305601226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beysens M., Haeck L., Vindevoghel K. Laparoscopic appendectomy combinedwith TEP for de Garengeot hernia: case report. Acta Chir. Belg. 2013;113:468–470. [PubMed] [Google Scholar]
- 11.Kalles V., Mekras A., Mekras D., Papapanagiotou I., Al-Harethee W., Sotiropoulos G. De Garengeot’s hernia: a comprehensive review. Hernia. 2013;17:177–182. doi: 10.1007/s10029-012-0993-3. [DOI] [PubMed] [Google Scholar]
- 12.Hussain A., Slesser A.A.P., Monib S., Maalo J., Soskin M., Arbuckle J. A De Garengeot Hernia masquerading as a strangulated femoral hernia. Int. J. Surg. Case Rep. 2014;5:656–658. doi: 10.1016/j.ijscr.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Priego P., Lobo E., Moreno I., Sanchez-Picot S., Gil Olarte M.A., Alonso N., Fresneda V. Acute appendicitis in an incarcerated crural hernia: analysis of our experience. Rev. Esp. Enferm. Dig. 2005;97:707–715. doi: 10.4321/s1130-01082005001000004. [DOI] [PubMed] [Google Scholar]
- 14.Al-Subaie S., Mustafa H., Al-Sharqawi N., Al-Haddad M., Othman F. A case of de Garengeot hernia: the feasibility of laparoscopic transabdominal preperitoneal hernia repair. Int. J. Surg. Case Rep. 2015;16:73–76. doi: 10.1016/j.ijscr.2015.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]