Abstract
Clinical practice guidelines recommend that clinicians implement the 5As (Ask, Advise, Assess, Assist, and Arrange) for smoking cessation at every clinical encounter. We sought to examine the prevalence of patient- and clinician-reported 5As in two primary care and one HIV care clinics in San Francisco, California between August 2013 and March 2014 (n = 462 patients and n = 61 clinicians). We used multivariable logistic regression analysis to identify factors associated with receipt of the 5As, adjusting for patient demographics, patient insurance, clinic site, patient tobacco use, and patient comorbidities. The patient-reported prevalence of 5As receipt was as follows: Ask, 49.9%; Advise, 47.2%; Assess, 40.6%; any Assist, 44.9%; and Arrange, 22.4%. In multivariable analysis, receipt of Advise, Assess, and Assist were associated with older patient age. Whereas patients with HIV had a lower odds of reporting being advised (AOR 0.5, 95% CI 0.3–0.8) or assessed for readiness to quit (AOR 0.6, 95% CI 0.4–0.9), patients with pulmonary diseases had higher odds of reporting being assisted (AOR 1.6, 95% 1.0–2.6) than patients without these diagnoses. Although the majority of clinicians reported asking (91.8%), advising (91.8%), and assessing (93.4%) tobacco use ‘most of the time’ or ‘always’ during a clinical encounter, fewer reported assisting (65.7%) or arranging (19.7%) follow-up. Only half of patients reported being screened for tobacco use and fewer reported receipt of the other 5As, with significant disparities in receipt of the 5As among patients with HIV. Our findings confirm the need for interventions to increase clinician-delivered cessation treatment in primary and HIV care.
Keywords: Smoking cessation, 5As for smoking cessation, Primary care
Highlights
-
•
Clinical practice guidelines recommend the use of 5As for smoking cessation.
-
•
Patient reports of Assist and Arrange were low in primary care and HIV care.
-
•
There were significant disparities in the receipt of 5As among patients with HIV.
-
•
Digital interventions could facilitate clinician-delivered 5As for patients.
1. Introduction
Tobacco use is the leading preventable cause of death, and is responsible for > 480,000 deaths annually in the United States (U.S.) (U.S. Department of Health and Human Services, 2014). The major causes of excess mortality among smokers stem from smoking-related cancers, cardiovascular disease and respiratory disease (Centers for Disease Control and Prevention, 2008a, Jha et al., 2013). Although the past 4 decades have seen significant declines in the prevalence of smoking in the general population, prevalence remains high among certain populations (Prevention CfDCa, 2014, Jamal et al., 2015). Low-income persons (Prevention CfDCa, 2014, Jamal et al., 2015), racial/ethnic minorities (Jamal et al., 2015, Centers for Disease Control and Prevention, 2005), persons with mental health disorders or substance use disorders (Schroeder and Morris, 2010), indigent persons living with HIV/AIDS (Vijayaraghavan et al., 2014), and persons who are uninsured or publicly insured (Centers for Disease Control and Prevention, n.d.), bear a disproportionate burden of tobacco-related morbidity and mortality (Centers for Disease Control and Prevention, 2008b).
Primary care clinicians are in a unique position to help patients quit smoking by employing strategies outlined in the U.S. Public Health Service guidelines (Fiore et al., 2008). These guidelines recommend that all clinicians offer brief interventions for smoking cessation at all or nearly all encounters using the 5As (Ask about smoking, Advise cessation, Assess readiness to quit, Assist with motivation and/or cessation, and Arrange follow-up) (Fiore et al., 2008) Most smokers in the general population are interested in quitting smoking and almost half attempt to quit smoking yearly (Centers for Disease Control and Prevention, 2011). Smokers are receptive to counseling for smoking cessation (Fiore et al., 2008), and about half report having received advice to quit from a health professional (Centers for Disease Control and Prevention, 2011, Kruger et al., 2012). Most smokers cite clinician's advice to quit smoking as an important motivator for smoking cessation (Kruger et al., 2012, Gilpin et al., 1993). Receipt of clinician-delivered counseling, in particular the more intensive Assist and Arrange interventions for smoking cessation has been shown to increase cessation (Fiore et al., 2008, Park et al., 2015). Receipt of all the 5As compared to one or none during a clinical encounter has been associated with increased use of cessation services (Kruger et al., 2016).
Despite patients' interest in receiving counseling, there is significant variability in clinician delivery of the 5As (Park et al., 2015, Ferketich et al., 2006, Thorndike et al., 2007). Previous research has shown that while most smokers are screened for tobacco use, fewer are advised to quit or assessed for their readiness to quit, and only a minority report receipt of clinician-delivered Assist (pharmacotherapy and/or more intensive counseling) or Arrange (Park et al., 2015, Ferketich et al., 2006, Jamal et al., 2012). Fewer than 25% of Medicaid-enrolled smokers reported receiving assistance with cessation (Chase et al., 2007). Racial/ethnic minorities, persons of lower socioeconomic status, and younger persons are less likely to receive clinician-delivered cessation interventions (Danesh et al., 2014, Browning et al., 2008, Ferketich et al., 2014). Patient comorbidity and time spent with the physician are also associated with lower probability of receiving smoking cessation interventions in clinical care (Jamal et al., 2015, Ferketich et al., 2006, Silfen et al., 2015).
In this study, we examined the prevalence of receipt of clinician-delivered 5As among patients in two diverse primary care clinics and one HIV care clinic and patient-related factors associated with receipt of the 5As. Consistent with previous studies (Park et al., 2015, Ferketich et al., 2006, Jamal et al., 2012), we hypothesized that receipt of Ask, Advise, and Assess would be higher than Assist and Arrange. We hypothesized that receipt of 5As would vary by clinic because of the distribution of patient comorbidity, and that patients with HIV/AIDS and those with mental health disorders or substance use disorders would be less likely to receive 5As. Among a subgroup of patients and their clinicians, we examined the indirect association between patient-reported receipt of 5As and clinician-reported overall adherence to 5As during their clinical practice.
2. Methods
2.1. Study patients and sampling
This study includes the analysis of cross-sectional data from the pre-implementation evaluation of patients and clinicians who were enrolled in a larger study of a randomized controlled trial of a computer tablet intervention to increase clinician adherence to 5As (Kalkhoran et al., 2016). We recruited patients and clinicians from 3 diverse clinics: an academic general internal medicine practice in a University-affiliated public hospital (“site 1”), an academic general internal medicine practice at a University-affiliated hospital (“site 2”), and an academic HIV practice at a University-affiliated public hospital (“site 3”) (Kalkhoran et al., 2016). Data were collected between August 2013 and March 2014.
We recruited current smokers (i.e. having smoked at least 100 cigarettes in their lifetime and having smoked at least 1 cigarette in the past 7 days) who were 18 years or older, Spanish- or English-speaking, and engaged in primary or urgent care in any of the 3 clinics. We recruited clinicians, including post-graduate trainees, who were in internal medicine or family medicine specialties, engaged in patient care in one of the three clinic sites, and planned to continue to work in their current location for at least 1 year. All study protocols were approved by the University of California San Francisco, Committee on Human Research.
2.2. Study procedures
Trained research staff approached patients in clinic waiting rooms prior to their primary care or urgent care clinic visits (i.e. the index clinic visit). Research staff screened patients for eligibility, enrolled patients into the study, and obtained written informed consent. Research staff administered a brief demographic questionnaire prior to the index visit, and a post-visit questionnaire (either in person or by telephone) on tobacco use behaviors and receipt of the 5As within 72 h of their visit. We were unable to complete all of the follow-up assessments by phone because some patients lacked functioning telephones. If the patient was unsure that he or she could be contacted by telephone, we completed the follow-up assessment in person. Patients received a $20 gift card for completing the pre- and post-visit questionnaires.
We recruited and consented clinicians by email, and asked them to complete a self-administered online questionnaire about demographics, tobacco use behaviors, and adherence to 5As counseling. Clinician assessments took place at a different time, and were unrelated to the patients' index visits. We gave clinicians a $25 gift card for completing the questionnaire.
2.3. Study measures
2.3.1. Patients
Prior to the index visit, patients self-reported information on: demographics (age and sex); race/ethnicity (Hispanic/Latino, White, Black or African American, Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaskan Native, Other/Mixed); and education (less than high school, high school or general education development, some college, or college degree or more). Patients self-reported whether they had health insurance, and if they did, they reported the type (Medicare, Medi-Cal or Medicaid, HMO or PPO, Healthy San Francisco or Healthy Worker, Other). Research staff confirmed with clinic staff whether patients were seeking primary or urgent care on the day of the visit. We estimated average daily cigarette consumption from patient self-reports of the number of days smoked and the number of cigarettes smoked per day. We obtained information on time to first cigarette after waking, and dichotomized responses as < 30 min and ≥ 30 min.
After the index visit, we asked patients to self-report receipt of the 5As during that visit. We asked patients whether their clinician had asked about their smoking, advised them to quit smoking, assessed their readiness to quit smoking, assisted them in building motivation and/or their smoking cessation attempt, and arranged for follow-up. Patients self-reported whether they had received each of the Assist components, as defined in the clinical practice guidelines (Fiore et al., 2008), including: planning to set a quit date, willingness to take steps to get ready to stop smoking, addressing roadblocks to quitting smoking, obtaining tips to cope with cigarette cravings, receiving patient education about quitting smoking, receiving information on outside resources for cessation (e.g. telephone quit line), obtaining information on smoking cessation medications, receiving a prescription for a cessation medication, and setting a quit date at that visit.
We extracted data on patient comorbidities from the clinical records using ICD-9 codes. We focused on the following comorbidities that may be associated with receipt of 5As: HIV (V08, 042.x–044.x), mental health disorders (300.x, 296.x, 295.x, 309.81, 311.x), drug dependence (304.x, 305.x), alcohol dependence (393.x), cancer (140.x–172.x, 174.x–195.8, 200.x–208.x, 238.6), pulmonary disease (490.x–505.x, 506.5, 416.7, 416.9, 508.1, 508.8), cerebrovascular disease (430.x-438.x, 362.34), cardiovascular disease (401.x–405.x, 410.x–414.x, 440.x, 444.x), and glaucoma (365.x).
2.3.2. Clinicians
Clinicians self-reported information on demographics (age and sex) and race/ethnicity (Hispanic/Latino, Black or African American, Asian or Pacific Islander, White, Native American or Alaskan Native, Other/Mixed). We obtained information on clinicians' primary practice location, primary degree, number of years in clinical practice (0–2 years, 2–5 years, 5–10 years, 10–20 years, > 20 years), and the time that they spent in direct patient care (0%–40%, 41%–80%, 81%–100%). Clinicians self-reported whether they had ever smoked at least 100 cigarettes in their lifetime. Ever smokers self-reported whether they were current smokers. We asked clinicians how frequently they adhered to the 5As [Ask, Advise, Assess, Assist (encourage to set a quit date, discuss medications, or refer to smoking cessation treatment) (Fiore et al., 2008), and Arrange] overall in their outpatient practice using the following response options: “Never”, “Rarely”, “Some of the time”, “Most of the time”, or “Always”. Clinicians also reported whether they had heard about the 5As, whether they had received training to administer the 5As, whether they would be interested in more 5As training, and the proportion of their patients who were smokers.
2.4. Statistical analysis
We reported sample characteristics for patients and clinicians using means (SD) for continuous variables and proportions for categorical variables. We reported the patient-reported receipt of each of the 5As. We examined the bivariate association of receipt of the 5As and patient demographics, clinic site, and tobacco use characteristics using logistic regression analysis accounting for clustering of patients within providers. We conducted logistic regression analyses with a backward elimination algorithm, adjusting for patient demographics, visit type, insurance status, clinic site, tobacco use characteristics, and patient comorbidities. Covariates with a p-value of 0.2 or lower were retained.
We examined adherence to the 5As among clinicians, and categorized responses as “Never”, “Rarely or Sometimes”, or “Most of the time or Always”. We examined the bivariate association of clinician adherence to the 5As by clinician demographics, clinic site, and clinical practice characteristics using the chi-square statistic for categorical variables and the t-test for continuous variables. For the sub-sample of patients who had a study clinic visit with one of the participating clinicians, we fit logistic regression models to examine the indirect association between patient-reported receipt of the specific 5As components and clinician adherence to the same components. We did this to obtain a global assessment, as opposed to a visit-specific assessment, of the communication between patients and clinicians around the 5As for smoking cessation. Models for each component of the 5As were adjusted for patient demographics, visit type, insurance status, clinic site, tobacco use characteristics, and clinician report of the corresponding 5As. All analyses were conducted using Stata, version 11.
3. Results
3.1. Patient-reported receipt of the 5As
We recruited 493 patients, of whom 462 (93.7% response rate) patients completed the pre- and post-index visit questionnaires. The analytic sample included 462 patients, with 16.7% were enrolled in site 1, 23.6% were enrolled in site 2, and 59.7% were enrolled in site 3 (Table 1). Average age was 50.8 years (SD 11.2), 67.3% were male, and 42.2% were African American. The majority (79.4%) were current daily smokers and nearly two-thirds (60.9%) smoked within 30 min of waking. The majority of patients had at least one mental health disorder (79.9%) or a drug dependence disorder (88.1%).
Table 1.
Patient demographics and tobacco use characteristics.
| Total N = 462 Mean (SD) or N (%) |
Site 1 N = 77 Mean (SD) or N (%) |
Site 2 N = 109 Mean (SD) or N (%) |
Site 3 N = 276 Mean (SD) or N (%) |
P-value | |
|---|---|---|---|---|---|
| Age | 50.8 (11.2) | 54.8 (10.3) | 52.8 (13.3) | 48.8 (10.1) | < 0.001 |
| Sex | |||||
| Female | 142 (30.7) | 33 (42.9) | 56 (51.4) | 53 (19.2) | < 0.001 |
| Male | 311 (67.3) | 44 (57.1) | 53 (48.6) | 214 (77.5) | |
| Transgender/other | 9 (1.95) | 0 (0.0) | 0 (0.0) | 9 (3.3) | |
| Race/ethnicity | |||||
| White | 142 (30.7) | 16 (20.8) | 36 (33.0) | 90 (32.6) | < 0.003 |
| African American | 195 (42.2) | 43 (55.8) | 44 (40.4) | 108 (39.1) | |
| Hispanic/Latino | 84 (18.2) | 12 (15.6) | 15 (13.8) | 57 (20.7) | |
| Asian | 10 (2.2) | 3 (3.9) | 2 (1.8) | 5 (1.8) | |
| Native Hawaiian/PI | 2 (0.4) | 0 (0.0) | 1 (0.9) | 1 (0.4) | |
| American Indian/Alaskan native | 12 (2.6) | 0 (0.0) | 1 (0.9) | 11 (3.9) | |
| Other/Mixed | 17 (3.7) | 3 (3.9) | 10 (9.2) | 4 (1.5) | |
| Education | < 0.03 | ||||
| Less than high school | 88 (19.1) | 17 (22.1) | 11 (10.1) | 60 (21.7) | |
| High school or GED | 141 (30.5) | 22 (28.6) | 28 (25.7) | 91 (32.9) | |
| Some college | 177 (38.3) | 31 (40.3) | 52 (47.7) | 94 (34.1) | |
| College degree or more | 56 (12.1) | 7 (9.1) | 18 (16.5) | 31 (11.2) | |
| Health insurance | < 0.001 | ||||
| None | 12 (2.6) | 5 (6.5) | 0 (0.0) | 7 (2.5) | |
| HMO/PPO | 34 (7.4) | 3 (3.9) | 27 (24.8) | 4 (1.5) | |
| Healthy San Francisco/healthy workersa | 76 (16.5) | 20 (25.9) | 6 (5.6) | 50 (18.1) | |
| Medi-Cal | 52 (11.3) | 12 (15.6) | 10 (9.2) | 30 (10.9) | |
| MediCal/MediCare | 249 (53.9) | 27 (35.1) | 51 (46.8) | 171 (61.9) | |
| Other | 19 (4.1) | 5 (6.5) | 2 (1.8) | 12 (4.4) | |
| Type of visit | 0.9 | ||||
| Urgent care | 82 (17.7) | 13 (16.9) | 19 (17.4) | 50 (18.1) | |
| Primary care | 380 (82.3) | 64 (83.1) | 90 (82.6) | 226 (81.9) | |
| Clinicsb | |||||
| Site 1 | 77 (16.7) | -- | -- | -- | |
| Site 2 | 109 (23.6) | -- | -- | -- | |
| Site 3 | 276 (59.7) | -- | -- | -- | |
| Smoking statusc | < 0.02 | ||||
| Current daily | 365 (79.4) | 63 (81.8) | 76 (69.7) | 226 (82.5) | |
| Current non-daily | 95 (20.7) | 14 (18.2) | 33 (30.3) | 48 (17.5) | |
| Average daily cigarette consumptionc | 10 (8.4) | 10.1 (8.3) | 9.0 (7.6) | 10.4 (8.7) | 0.9 |
| Time to first cigarette after wakingc | 0.3 | ||||
| 30 min or less | 280 (60.9) | 46 (59.7) | 60 (55.1) | 174 (63.5) | |
| ≥ 30 min | 180 (39.1) | 31 (40.3) | 49 (44.9) | 100 (36.5) | |
| Comorbidities | |||||
| HIV | 270 (58.4) | 5 (6.5) | 0 (0.0) | 265 (96.0) | < 0.001 |
| Cancer | 74 (16.0) | 9 (11.7) | 17 (5.6) | 48 (17.4) | 0.5 |
| Mental health disordersd | 369 (79.9) | 57 (74.0) | 87 (79.8) | 225 (81.5) | 0.3 |
| Alcohol dependence | 78 (16.9) | 23 (29.9) | 8 (7.3) | 47 (17.0) | < 0.001 |
| Drug dependence | 407 (88.1) | 71 (92.2) | 93 (85.3) | 243 (88.0) | 0.4 |
| Cerebrovascular disease | 43 (9.3) | 13 (16.9) | 10 (9.2) | 20 (7.3) | < 0.04 |
| Pulmonary disease | 101 (21.9) | 45 (58.4) | 55 (50.5) | 1 (0.4) | < 0.001 |
| Cardiovascular diseased | 287 (62.1) | 67 (87.0) | 72 (66.1) | 148 (53.6) | < 0.001 |
| Glaucoma | 29 (6.3) | 4 (5.2) | 12 (11.0) | 13 (4.7) | 0.07 |
-- Not applicable.
Healthy San Francisco is a program designed to make health care services available to uninsured San Francisco residents. Healthy Workers is a health insurance program administered by San Francisco Health Plan.
Site 1 is an academic general internal medicine practice in a University-Affiliated public hospital, Site 2 is an academic general internal medicine practice in a University-affiliated hospital, Site 3 is an HIV practice in a University-affiliated public hospital.
Data on cigarette smoking missing for 2 people.
Mental health disorders include Anxiety, Somatoform, dissociative disorder, bipolar disorder, schizophrenia, post traumatic stress disorder, and depression. Cardiovascular disease includes hypertension.
Sites 1 and 3 served predominantly underserved populations. Patients in site 1 (55.8%) had a higher proportion of African American patients compared to site 2 (40.4%) and site 3 (39.1%) (p < 0.003) (Table 1). Patients in site 1 were more likely to be older (54.8 years) compared to site 2 (52.6 years) and site 3 (48.7%) (p < 0.001). Patients in site 1 (27.8%) were more likely to report receiving medical coverage through the Healthy San Francisco program for uninsured patients compared to patients in site 2 (5.5%) and site 3 (18.6%) (p < 0.001). Patients in site 1 had more comorbidities than patients in the other 2 sites.
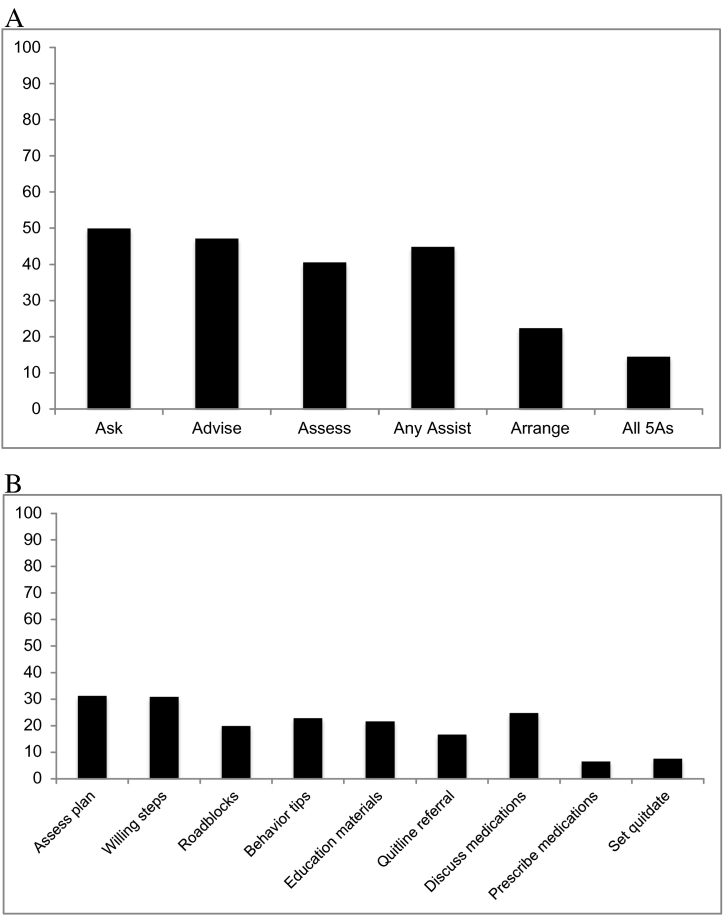
The patient-reported prevalence of 5As receipt during their index visit was as follows: 49.9% Ask; 47.2% Advise; 40.6% Assess; 44.9% any Assist; 22.4% Arrange, and 14.5% for all 5As (Fig. 1A). The least frequently reported types of Assist included receiving prescriptions for smoking cessation (6.5%) and assistance with setting a quit date (7.6%; Fig. 1B).
Fig. 1.
A: Proportion of patients who self-reported receipt of 5As (N = 462)
B: Proportion of patients who self-reported receipt of components of Assist (N = 462).
In bivariate analyses, older patient age was associated with increased receipt of 5As (Supplementary Table 1, Supplementary Table 2). Patients in site 3 were less likely to report having received Ask, Advise, Assess, or any Assist components of 5As compared to patients in site 1. In multivariable models, older patient age was associated with higher odds of receipt of Advise, Assess, and Assist interventions (Table 2). Patients in site 3 had a lower likelihood of being asked about tobacco use (AOR 0.3, 95% CI 0.2–0.6) than those in site 1 (Table 3). Patients with HIV had a lower likelihood of being advised (AOR 0.5, 95% CI 0.3–0.8) or assessed (AOR 0.6, 95% CI 0.4–0.9) than those without. Patients with pulmonary disease had a higher likelihood of being assisted (AOR 1.8, 95% CI 1.1–2.8) and patients with cardiovascular disease had a higher likelihood of having follow-up arranged (AOR 2.2, 95% CI 1.3–3.8) than patients without these diagnoses (Table 3). Patients with cardiovascular disease had a higher likelihood of reporting receipt of all the 5As during the index visit (AOR 1.9, 95% CI 1.1–3.5).
Table 2.
Multivariable logistic regression analysis with backward elimination of patient-related factors associated with receipt of 5As (N = 462).
| AskAdjusted odds ratio (95% CI)a | AdviseAdjusted odds ratio (95% CI)a | AssessAdjusted odds ratio (95% CI)a | AssistAdjusted odds ratio (95% CI)a | ArrangeAdjusted odds ratio (95% CI)a | All 5AsAdjusted odds ratio(95% CI)a | |
|---|---|---|---|---|---|---|
| Ageb | 1.1 (0.9–1.2) | 1.1 (1.0–1.2)|| | 1.1 (1.0–1.2)|| | 1.1 (1.0–1.2)¶ | --c | --c |
| Sex | ||||||
| Male | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Female | 1.3 (0.9–1.8) | 1.4 (1.0–1.9) | --c | --c | --c | --c |
| Race/ethnicity | ||||||
| Nonwhite | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| White | --c | 0.7 (0.5–1.1) | 0.7 (0.4–1.1) | --c | --c | 0.6 (0.3–1.2) |
| Clinicsd | ||||||
| Site 1 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Site 2 | 0.7 (0.4–1.2) | --c | --c | --c | --c | --c |
| Site 3 | 0.3 (0.2–0.6)# | --c | --c | --c | --c | --c |
| Average daily cigarette consumption | 1.0 (0.9–1.0) | 1.0 (1.0–1.04) | --c | --c | --c | 1.0 (1.0–1.1)|| |
| Comorbidities | ||||||
| HIV | --c | 0.5 (0.3–0.8)¶ | 0.6 (0.4–0.9)|| | --c | --c | --c |
| Mental health disorders | 0.7 (0.4–1.1) | --c | 0.7 (0.4–1.1) | 0.7 (0.5–1.1) | 0.7 (0.4–1.1) | --c |
| Drug dependence | --c | --c | 1.5 (0.9–2.6) | --c | --c | --c |
| Pulmonary disease | --c | --c | --c | 1.8 (1.1–2.8)|| | 1.4 (0.9–2.3) | 1.5 (0.8–2.9) |
| Cardiovascular disease | --c | --c | --c | --c | 2.2 (1.3–3.8)¶ | 1.9 (1.1–3.5)|| |
| Glaucoma | --c | --c | --c | --c | --c | 0.3 (0.1–1.7) |
P-values were obtained from logistic regression analysis, accounting for clustering by provider.
The odds ratio represents the odds of receiving counseling for every 5-unit increase in age.
Variables were omitted from the model if p > 0.2.
Site 1 is an academic general internal medicine practice in a University-Affiliated public hospital, Site 2 is an academic general internal medicine practice in a University-affiliated hospital, Site 3 is an HIV practice in a University-affiliated public hospital.
p < 0.005.
p < 0.001.
p < 0.05.
Table 3.
Provider sample characteristics.
| Total N = 61 Mean (SD) or N (%) |
|
|---|---|
| Age | 38.9 (10.6) |
| Sex | |
| Female | 44 (72.1) |
| Male | 17 (27.9) |
| Race/ethnicity | |
| White | 39 (63.9) |
| African American | 1 (1.6) |
| Hispanic/Latino | 6 (9.8) |
| Asian | 12 (19.7) |
| Native Hawaiian/PI | 0 (0.0) |
| American Indian/Alaskan native | 0 (0.0) |
| Other/mixed | 3 (4.9) |
| Education | |
| Physician | 54 (88.5) |
| Nurse practitioner | 7 (11.5) |
| Years in practice | |
| 0–2 years | 21 (34.4) |
| 2–5 years | 8 (13.1) |
| 5–10 years | 7 (11.5) |
| 10–20 years | 19 (31.2) |
| > 20 years | 6 (9.8) |
| Percentage of time spent in patient care | |
| 0%–40% | 22 (36.1) |
| 41%–80% | 17 (27.9) |
| 81%–100% | 22 (36.1) |
| Clinicsa | |
| Site 1 | 24 (39.3) |
| Site 2 | 26 (42.6) |
| Site 3 | 11 (18.0) |
| Smoking status | |
| Ever smoker | 7 (11.5) |
| Current smoker | 0 (0.0) |
| Heard of 5As | 55 (90.2) |
| Received training for 5As | 44 (72.1) |
| Interested in more 5As training | 49 (80.3) |
| Proportion of patients who smoke | |
| 0%–24% | 24 (39.3) |
| 25%–49% | 34 (55.7) |
| 50%–74% | 2 (3.3) |
| 75%–100% | 1 (1.6) |
Site 1 is an academic general internal medicine practice in a University-Affiliated public hospital, Site 2 is an academic general internal medicine practice in a University-affiliated hospital, Site 3 is an HIV practice in a University-affiliated public hospital.
3.2. Clinician-reported adherence to the 5As
Of the 61 clinicians, 39.3% reported working in site 1, 42.6% reported working in site 2, and 18.0% reported working in site 3 (Table 3). The majority of clinicians were physicians (88.5%). Of the clinicians, 11.5% reported being ever smokers; none of them currently smoked. Almost all (90.2%) had heard of the 5As, 72.1% had received training for 5As, and 80.3% reported being interested in receiving more training to implement the 5As.
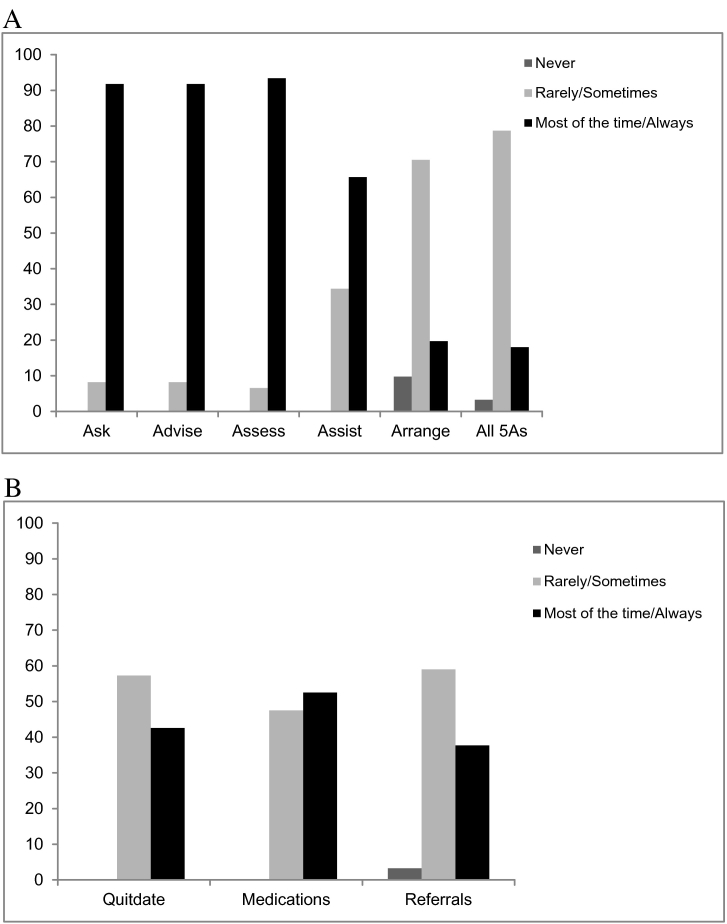
Almost all clinicians reported that during clinical encounters they had asked their patients about smoking (91.8%), advised them to quit smoking (91.8%), and assessed their readiness to quit (93.4%) “most of the time” or “always” (Fig. 2A). About two-thirds (65.7%) reported assisting patients with a quit attempt, a minority (19.7%) reported arranging for a follow-up, and a minority (18.0%) reported adhering to all the 5As either “most of the time” or “always” during clinical encounters. Among Assist components, 42.6% reported having assisted patients with setting a quit date, 52.5% discussed medications for cessation, and 37.7% provided referrals to smoking cessation resources “most of the time” or “always” during clinical encounters (Fig. 2B). Clinician demographics and practice characteristics were not associated with adherence to the 5As (data not shown).
Fig. 2.
A: Provider adherence to 5As (N = 61)
B: Self-reported provider adherence to components of Assist (N = 61).
3.3. Association of patient-reported receipt of the 5As with clinician-reported adherence to the 5As
The 61 clinicians cared for 214 of the sampled patients (Supplementary Table 3). In subgroup analysis of patient and clinician clusters, clinician-report of having advised patients to quit smoking “most of the times” or “always” during clinical encounters was positively associated with patient-report of receipt of Advise (AOR 1.9, 95% CI 1.1–3.6) during the index visit. Clinician-report of arranging follow-up overall during clinical encounters was negatively associated with patients' corresponding self-report of receipt of Arrange (AOR 0.3, 95% CI 0.1–0.8) during the index visit. Clinician-report was not associated with patient report of the other 5As. Clinician report of all the 5As “most of the times” or “always” during clinical encounters was negatively associated with patient-report of receipt of all the 5As during the index visit (AOR 0.03, 95% CI 0.002–0.8).
4. Discussion
In this study of patients seeking care in primary care and HIV clinics, patient-reported receipt of some components of the 5As was lower than the national average and among commercially insured patients. In a nationally representative sample of patients seeking ambulatory care in the U.S. between 2005 and 2009, 62.7% were screened for tobacco use (Jamal et al., 2012) and among commercially insured patients 90% were screened for tobacco use by clinicians (Quinn et al., 2005) compared to 49.9% in our study. Prevalence of receiving advice to quit (40.9%) was higher among our patients compared to a nationally representative sample of patients seeking ambulatory care (20.9%) (Jamal et al., 2012) but lower than commercially insured patients (71%) (Quinn et al., 2005) Consistent with our hypothesis, patient reports of Assist and Arrange interventions were low and comparable to other patient populations in the U.S. (Park et al., 2015, Jamal et al., 2012, Quinn et al., 2005).
In the U.S., tobacco use is concentrated among low-income populations, those with low educational attainment, racial/ethnic minority groups, persons with mental health disorders and substance use disorders (Prevention CfDCa, 2014, Jamal et al., 2015, Schroeder and Morris, 2010). These high-risk populations were overrepresented in our study: about half of the patients had high school or less than high school education, two-thirds belonged to racial/ethnic minority groups, two-thirds were publicly insured, and the majority of patients had a diagnosis of mental health disorders or substance use disorders. Although guidelines recommend screening all patients for tobacco use (Fiore et al., 2008), only half the patients self-reported being asked about their smoking and fewer received the other 5As despite being at high risk for tobacco use (Centers for Disease Control and Prevention, 2008b).
As in previous studies (Quinn et al., 2005), with the exception of age no other demographic or tobacco use characteristics were associated with receipt of the 5As. Some clinicians may believe that younger patients are not motivated to quit smoking (Messer et al., 2008). Patients with cardiovascular or pulmonary disease were more likely to receive Assist or Arrange interventions, suggesting that clinicians may be better at counseling patients for secondary prevention rather than primary prevention (Houston et al., 2005).
Consistent with our hypothesis, patients in an HIV care clinic were less likely to report being asked, advised or assessed for smoking cessation compared to those in general medicine clinics. Persons living with HIV/AIDS have high rates of smoking (Vijayaraghavan et al., 2014, Burkhalter et al., 2005) and other medical and psychiatric comorbidities (Shirley et al., 2013) that may influence receipt of the 5As. Cigarette smoking is an independent risk factor for all-cause mortality among patients living with HIV/AIDS (Crothers et al., 2005, Helleberg et al., 2013). Our findings highlight disparities in receipt of 5As among patients living with HIV/AIDS, and suggest the need for targeted interventions for this population.
Clinician-reported adherence to Ask, Advise, and Assess was higher than what has been reported in previous studies, where estimates of provider-delivered Ask, Advise, and Assess has ranged between 60% and 75% (Goldstein et al., 1998, Schnoll et al., 2006). However, patient and clinician self-reports of Assist and Arrange were low. Receipt of these more intensive stages have been associated with increased quitting success and greater abstinence rates (Park et al., 2015, Quinn et al., 2005, Stead et al., 2008). Our findings have implications for improving clinician training on providing more intensive cessation interventions.
Although one-fourth of patients reported receiving information on medications for cessation, only a minority (6.5%) were prescribed medications during their last visit. The Affordable Care Act mandates coverage of treatment of tobacco dependence; however, significant state-level barriers exist in receipt of treatment (Singleterry et al., 2015). These include prior authorization requirements, annual limits on quit attempts, limits on duration, and required copayments, which may limit prescribing behavior among clinicians and accessibility among patients (Singleterry et al., 2015). Receipt of medications may also depend on patients' interest in quitting, with unmotivated patients less likely to receive medications than those who are motivated to quit smoking (Quinn et al., 2005). Clinician-level barriers may include lack of knowledge on prescribing medications for cessation or inadequate time to discuss medications among patients with medical and psychiatric comorbidities (Thorndike et al., 2007).
Although not a direct comparison, our findings of a discrepancy between patient-reported receipt of Arrange and clinician-report suggests that clinicians could be overestimating the rate at which they counsel patients or that patients may not comprehend clinician-delivered counseling. Clinicians may arrange follow-up without communicating that smoking cessation was the intent for follow-up; thus patient perceptions of Arrange may be different from that of clinicians. Interventions that rely on a personalized, mutually-agreed upon plan between patients and clinicians could increase receipt of interventions among smokers (Kalkhoran et al., 2016, Woods and Jaen, 2010). Receipt of all the 5As among patients and adherence to all the 5As among clinicians was low. A previous study reported that receipt of all the 5As among current smokers was associated with increased use of medications and counseling services (Kruger et al., 2016). Clinicians may not have provided assist and arrange interventions if patients were unwilling to quit smoking. Our findings highlight implications of addressing all 5As irrespective of patients' readiness to quit smoking.
Our study had several limitations. Smoking status was assessed via self-report, which could lead to misclassification bias. However, self-report has been shown to be a reliable measure of smoking status among diverse patient populations (Studts et al., 2006, Bryant et al., 2011). Clinicians' adherence to the 5As was assessed by self-report of their overall practice rather than for the specific visit with the enrolled patient, limiting our ability to measure visit-level concordance between clinicians' and patients' self-reports. We were unable to determine whether receipt of Assisting and Arranging efforts were associated with patients' degree of motivation to quit smoking.
The diversity of our patient population suggests that findings could be generalizable to other high-risk populations seeking care in public primary care and HIV clinics. Despite guidelines that emphasize counseling for tobacco use for all patients, findings indicate low levels of cessation interventions among a vulnerable patient population that is at high risk for tobacco-related morbidity and mortality. Disparities in receipt of the 5As appeared to be heightened for persons living with HIV and AIDS. These findings highlight opportunities for implementing interventions that rely on a personalized, jointly agreed upon plan between patients and clinicians, and that harnesses the potential of information technology to facilitate clinician-delivered 5As for patients in primary care and HIV care clinics.
The following are the supplementary data related to this article.
Receipt of 5As by demographic, clinic site, and tobacco use characteristics.
Unadjusted odds ratio of receipt of 5As by demographic, clinic site, and tobacco use characteristics (N = 462).
Multivariable analysis of factors associated with self-reported receipt of 5As among patient and clinician clusters (N = 214).
Conflict of interest statement
External funding for all authors was provided by NIH/NIDA Grant# R01DA034253 awarded to Jason Satterfield, PhD. Sara Kalkhoran, MD is a co-author on e-cigarettes for UpToDate, Inc. and receives royalties from this. All other authors do not report any conflicts of interest.
Acknowledgments
The research presented in this paper is that of the authors and does not reflect the official policy of the NIH. External funding was provided by NIH/NIDA Grant gR01DA034253 awarded to Jason Satterfield, PhD. In accordance with the ICMJE guidelines, all authors made substantial contributions to the conception and design, or acquisition of data, or analysis and interpretation of data; were involved in drafting the manuscript or revising it critically for important intellectual content; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The work presented here has been accepted for presentation at the 2016 AMERSA National Conference, November 3, 2016. No financial disclosures were reported by the authors of this paper.
References
- Browning K.K., Ferketich A.K., Salsberry P.J., Wewers M.E. Socioeconomic disparity in provider-delivered assistance to quit smoking. Nicotine Tob. Res. 2008;10:55–61. doi: 10.1080/14622200701704905. [DOI] [PubMed] [Google Scholar]
- Bryant J., Bonevski B., Paul C., Lecathelinais C. Assessing smoking status in disadvantaged populations: is computer administered self-report an accurate and acceptable measure? BMC Med. Res. Methodol. 2011;11:153. doi: 10.1186/1471-2288-11-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhalter J.E., Springer C.M., Chhabra R., Ostroff J.S., Rapkin B.D. Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine Tob. Res. 2005;7:511–522. doi: 10.1080/14622200500186064. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Health disparities experienced by black or African Americans - United States. MMWR Morb. Mortal. Wkly Rep. 2005;54:1–3. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Smoking-attributable mortality, years of potential life lost, and productivity losses – United States, 2000–2004. MMWR Morb. Mortal. Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Smoking-attributable mortality, years of potential life lost, and productivity losses - United States, 2000–2004. MMWR Morb. Mortal. Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Quitting smoking among adults - United States, 2000–2010. Morb. Mortal. Wkly Rep. 2011;60:1513–1519. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Smoking Rates for Uninsured and Adults on Medicaid More Than Twice Those for Adults With Private Health Insurance. http://wwwcdcgov/media/releases/2015/p1112-smoking-rateshtml Available at: Accessed August 23, 2016.
- Chase E.C., McMenamin S.B., Halpin H.A. Medicaid provider delivery of the 5A's for smoking cessation counseling. Nicotine Tob. Res. 2007;9:1095–1101. doi: 10.1080/14622200701666344. [DOI] [PubMed] [Google Scholar]
- Crothers K., Griffith T.A., McGinnis K.A. The impact of cigarette smoking on mortality, quality of life, and comorbid illness among HIV-positive veterans. J. Gen. Intern. Med. 2005;20:1142–1145. doi: 10.1111/j.1525-1497.2005.0255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danesh D., Paskett E.D., Ferketich A.K. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev. Chronic Dis. 2014;11 doi: 10.5888/pcd11.140053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferketich A.K., Khan Y., Wewers M.E. Are physicians asking about tobacco use and assisting with cessation? Results from the 2001–2004 national ambulatory medical care survey (NAMCS) Prev. Med. 2006;43:472–476. doi: 10.1016/j.ypmed.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Ferketich A.K., Pennell M., Seiber E.E. Provider-delivered tobacco dependence treatment to Medicaid smokers. Nicotine Tob. Res. 2014;16:786–793. doi: 10.1093/ntr/ntt221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore M.C., Jaén C.R., Baker T.B. US Dept. of Health and Human Services, Public Health Service; Rockville, MD: 2008. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline; pp. 131–144. [Google Scholar]
- Gilpin E.A., Pierce J.P., Johnson M., Bal D. Physician advice to quit smoking: results from the 1990 California tobacco survey. J. Gen. Intern. Med. 1993;8:549–553. doi: 10.1007/BF02599637. [DOI] [PubMed] [Google Scholar]
- Goldstein M.G., DePue J.D., Monroe A.D. A population-based survey of physician smoking cessation counseling practices. Prev. Med. 1998;27:720–729. doi: 10.1006/pmed.1998.0350. [DOI] [PubMed] [Google Scholar]
- Helleberg M., Afzal S., Kronborg G. Mortality attributable to smoking among HIV-1-infected individuals: a Nationwide, Population-Based Cohort Study. Clin. Infect. Dis. 2013;56:727–734. doi: 10.1093/cid/cis933. [DOI] [PubMed] [Google Scholar]
- Houston T.K., Scarinci I.C., Person S.D., Greene P.G. Patient smoking cessation advice by health care providers: the role of ethnicity, socioeconomic status, and health. Am. J. Public Health. 2005;95:1056–1061. doi: 10.2105/AJPH.2004.039909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A., Dube S.R., Malarcher A.M. Tobacco use screening and counseling during physician office visits among adults-National Ambulatory Medical Care Survey and National Health Interview Survey, United States, 2005–2009. MMWR Morb. Mortal. Wkly Rep. 2012;61(Suppl):38–45. [PubMed] [Google Scholar]
- Jamal A., Homa D.M., O'Connor E. Current cigarette smoking among adults - United States, 2005–2014. MMWR Morb. Mortal. Wkly Rep. 2015;64:1233–1240. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- Jha P., Ramasundarahettige C., Landsman V. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 2013;368:341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- Kalkhoran S., Appelle N.A., Napoles A.M. Beyond the ask and advise: implementation of a computer tablet intervention to enhance provider adherence to the 5As for smoking cessation. J. Subst. Abus. Treat. 2016;60:91–100. doi: 10.1016/j.jsat.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger J., Shaw L., Kahende J., Frank E. Health care providers' advice to quit smoking, National Health Interview Survey, 2000, 2005, and 2010. Prev. Chronic Dis. 2012;9 doi: 10.5888/pcd9.110340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger J., O'Halloran A., Rosenthal A.C., Babb S.D., Fiore M.C. Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC Public Health. 2016;16:141. doi: 10.1186/s12889-016-2798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer K., Trinidad D.R., Al-Delaimy W.K., Pierce J.P. Smoking cessation rates in the United States: a comparison of young adult and older smokers. Am. J. Public Health. 2008;98:317–322. doi: 10.2105/AJPH.2007.112060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park E.R., Gareen I.F., Japuntich S. Primary care provider-delivered smoking cessation interventions and smoking cessation among participants in the national lung screening trial. JAMA Intern. Med. 2015;175:1509–1516. doi: 10.1001/jamainternmed.2015.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevention CfDCa Current cigarette smoking among adults – United States, 2005–2012. MMWR Morb Mortal Wkly Rep. 2014;63:29–34. Centers for disease control and prevention. Current cigarette smoking among adults – United States, 2005–2012. MMWR Morb. Mortal. Wkly Rep. 2014;63:29–34. [PMC free article] [PubMed] [Google Scholar]
- Quinn V.P., Stevens V.J., Hollis J.F. Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. Am. J. Prev. Med. 2005;29:77–84. doi: 10.1016/j.amepre.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Schnoll R.A., Rukstalis M., Wileyto E.P., Shields A.E. Smoking cessation treatment by primary care physicians: an update and call for training. Am. J. Prev. Med. 2006;31:233–239. doi: 10.1016/j.amepre.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Schroeder S.A., Morris C.D. Confronting a neglected epidemic: tobacco cessation for persons with mental illnesses and substance abuse problems. Annu. Rev. Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. [DOI] [PubMed] [Google Scholar]
- Shirley D.K., Kesari R.K., Glesby M.J. Factors associated with smoking in HIV-infected patients and potential barriers to cessation. AIDS Patient Care STDs. 2013;27:604–612. doi: 10.1089/apc.2013.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silfen S.L., Cha J., Wang J.J., Land T.G., Shih S.C. Patient characteristics associated with smoking cessation interventions and quit attempt rates across 10 community health centers with electronic health records. Am. J. Public Health. 2015;105:2143–2149. doi: 10.2105/AJPH.2014.302444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleterry J., Jump Z., DiGiulio A. State Medicaid coverage for tobacco cessation treatments and barriers to coverage - United States, 2014–2015. MMWR Morb. Mortal. Wkly Rep. 2015;64:1194–1199. doi: 10.15585/mmwr.mm6442a3. [DOI] [PubMed] [Google Scholar]
- Stead L.F., Bergson G., Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2008 doi: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- Studts J.L., Ghate S.R., Gill J.L. Validity of self-reported smoking status among participants in a lung cancer screening trial. Cancer Epidemiol. Biomark. Prev. 2006;15:1825–1828. doi: 10.1158/1055-9965.EPI-06-0393. [DOI] [PubMed] [Google Scholar]
- Thorndike A.N., Regan S., Rigotti N.A. The treatment of smoking by US physicians during ambulatory visits: 1994 2003. Am. J. Public Health. 2007;97:1878–1883. doi: 10.2105/AJPH.2006.092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General; pp. 659–660. [Google Scholar]
- Vijayaraghavan M., Penko J., Vittinghoff E., Bangsberg D.R., Miaskowski C., Kushel M.B. Smoking behaviors in a community-based cohort of HIV-infected indigent adults. AIDS Behav. 2014;18:535–543. doi: 10.1007/s10461-013-0576-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods S.S., Jaen C.R. Increasing consumer demand for tobacco treatments: ten design recommendations for clinicians and healthcare systems. Am. J. Prev. Med. 2010;38:S385–S392. doi: 10.1016/j.amepre.2009.12.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Receipt of 5As by demographic, clinic site, and tobacco use characteristics.
Unadjusted odds ratio of receipt of 5As by demographic, clinic site, and tobacco use characteristics (N = 462).
Multivariable analysis of factors associated with self-reported receipt of 5As among patient and clinician clusters (N = 214).