Abstract
Nonalcoholic fatty liver disease (NAFLD) describes a spectrum of liver abnormalities from benign steatosis to nonalcoholic steatohepatitis (NASH). NASH is characterized by chronic and progressive liver pathology and can cause advanced fibrosis, cirrhosis, hepatocellular carcinoma, end-stage liver disease, and liver-related death. Unlike other forms of chronic liver disease, NAFLD is usually associated with insulin resistance and often at least one feature of the metabolic syndrome (obesity, impaired fasting glucose, hypertriglyceridemia, low high-density lipoprotein cholesterol, and hypertension). Although its progression rate may be slower than that of other types of liver disease, the incidence of both NAFLD and its sequelae is increasing throughout the world in parallel with the obesity epidemic. One of the important and unresolved problems is the pathogenesis of hepatocyte injury in NASH. The natural history of NAFLD remains unclear because of the paucity of histologic follow-up studies. Although there have been recent attempts to identify treatments for NAFLD, currently there is no well-established and approved therapy. Lifestyle modifications that include increased exercise and weight reduction address the underlying insulin resistance and may be the best advice for patients.
Keywords: Nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, obesity, insulin resistance, ballooning of hepatocytes
Nonalcoholic fatty liver disease (NAFLD) is a term used to describe a spectrum of histologic abnormalities, from benign steatosis to nonalcoholic steatohepatitis (NASH), in a person consuming little or no alcohol (Table 1). Although the natural history of NAFLD is not fully understood, currently available data indicate that NAFLD has the potential to progress to cirrhosis, hepatocellular carcinoma (HCC), end-stage liver disease, liver-related death, and recurrence after transplantation.1-9 A different spectrum of the disease, namely NAFLD-associated subacute liver failure, has also been reported.10
Table 1.
Terminology
| Benign steatosis: the generally nonprogressive form of NAFLD |
| HCC: hepatocellular carcinoma |
| NAFLD: nonalcoholic fatty liver disease; is characterized by predominantly macrovesicular steatosis in which hepatocytes contain vacuoles of triglycerides |
| NASH: nonalcoholic steatohepatitis; the progressive form of NAFLD that includes steatosis, necroinflammation, and variable degrees of fibrosis |
| NASH-associated cirrhosis: may lose the histologic features of NASH |
| NASH-associated HCC: HCC arising in the setting of cirrhosis caused by NASH |
| NASH-associated subacute liver failure: unexplained rapid and severe decompensation of liver function in the setting of NASH |
As the prevalence and severity of both obesity and diabetes continue to increase throughout the world, the incidence of NAFLD and its sequelae will also likely increase,11-13 though perhaps not as quickly as some other chronic liver diseases.9,14-17 Thus, NAFLD could develop into a large disease and health budget burden throughout the world.
Although recent studies support the hypothesis that NAFLD is a part of the metabolic syndrome, this remains an area of active investigation.18-25 For example, although insulin resistance seems to play an important role in the pathogenesis of NAFLD, not all patients with insulin resistance develop NAFLD and not all patients with NAFLD have insulin resistance.
An important unresolved problem is determination of the pathogenesis of hepatocyte injury in NASH. The natural history of NAFLD also remains unclear because there have been few histologic follow-up studies.9,16,26,27 The aim of this article is to provide a brief overview of the current knowledge about NAFLD and to raise awareness about this growing problem.
Definition and Prevalence of NAFLD
NAFLD is defined by the presence of excessive fat in the liver, detected either by imaging or liver biopsy.28 NAFLD used to be a diagnosis of exclusion in patients without other ongoing liver disease; however, as histologic criteria have evolved, the presence of NAFLD and NASH coexisting with other forms of liver disease has been described.29 To establish the diagnosis, patients must abstain from alcohol or drink infrequently. Recent studies suggested that the maximal safe level of ethanol consumption may be 30 g/day,30 although more stringent criteria such as 20 g/day for men and 10 g/day for women are often used in studies of patients with NAFLD.
It is estimated that approximately 10–40% of the adult population in the United States has some degree of NAFLD, and about 2–5% has NASH.31,32 Investigators from other developed nations report similarly high figures.33-37 NASH is the third most common liver disease in North America and the most common liver disease in both Australia and New Zealand.38 The prevalence of advanced disease varies somewhat with the population studied; for example, hispanic patients with NAFLD seem to progress to both NASH and cirrhosis more frequently than either blacks or whites.39,40 NAFLD is the most common histologic abnormality in patients with unexplained elevated liver enzymes in industrialized countries (4.5% of the US population is reported to have unexplained elevated alanine aminotransferase [ALT] levels).12,13,41-44 Obesity and diabetes are also important risk factors for advanced disease. An early autopsy study found NASH in 18.5% and 2.7% of markedly obese and lean subjects, respectively.45
NAFLD as Part of the Metabolic Syndrome
NAFLD is considered to be the hepatic manifestation of the metabolic syndrome (Table 2).18,19,25,46,47 Marchesini and colleagues reported that of 120 NASH patients, 88% met at least three criteria of the metabolic syndrome.23 The prevalence and severity of liver disease progressively increased with the number and severity of features of the metabolic syndrome. The prevalence of obesity, type-2 diabetes, and hyperlipidemia was 30–100%, 10–75%, and 20–92%, respectively, in different NAFLD case series.48
Table 2.
Criteria for Metabolic Syndrome*
|
The metabolic syndrome is present when three or more of the five criteria are met.
Adapted from Reaven.25
HDL = high-density lipoprotein.
Obesity and NAFLD
Obesity can be considered a low-grade chronic inflammatory condition and obesity-related cytokines such as interleukin-6 (IL-6), adiponectin, leptin, and tumor necrosis factor (TNF)α may play important roles in the development of NAFLD. The World Health Organization estimated that there were 200 million obese people in the world in 1995 and 300 million in 2002.49 Epidemiologically, the prevalence of elevated aminotransferases increases with increasing body mass index and a correlation between degree of obesity and the prevalence and severity of NAFLD has been found in several studies.50-52 For a given patient, the degree of ALT elevation does not predict the severity of disease and the full spectrum of NAFLD has been found in morbidly obese patients undergoing bariatric surgery.53-55 The prevalence of NASH is 3% and 20% in nonobese and obese subjects, respectively. Obesity is increasely common in children, and both fibrosis and cirrhosis have been seen in obese children with NAFLD. There is currently, however, no reliable estimate of the prevalence of NAFLD or its consequences in children.56-58
Type-2 Diabetes, Hyperlipidemia, and NAFLD
The prevalence of NASH associated with both cirrhosis and HCC was reported to be high among patients with type-2 diabetes with or without obesity.2,3,7,59 One study found that half of the hyperlipidemic patients had evidence of NAFLD by both ultrasound and abnormal liver enzymes.60 Even in the absence of obesity, hypertriglyceridemia is associated with insulin resistance.61
Pathogenesis of NAFLD
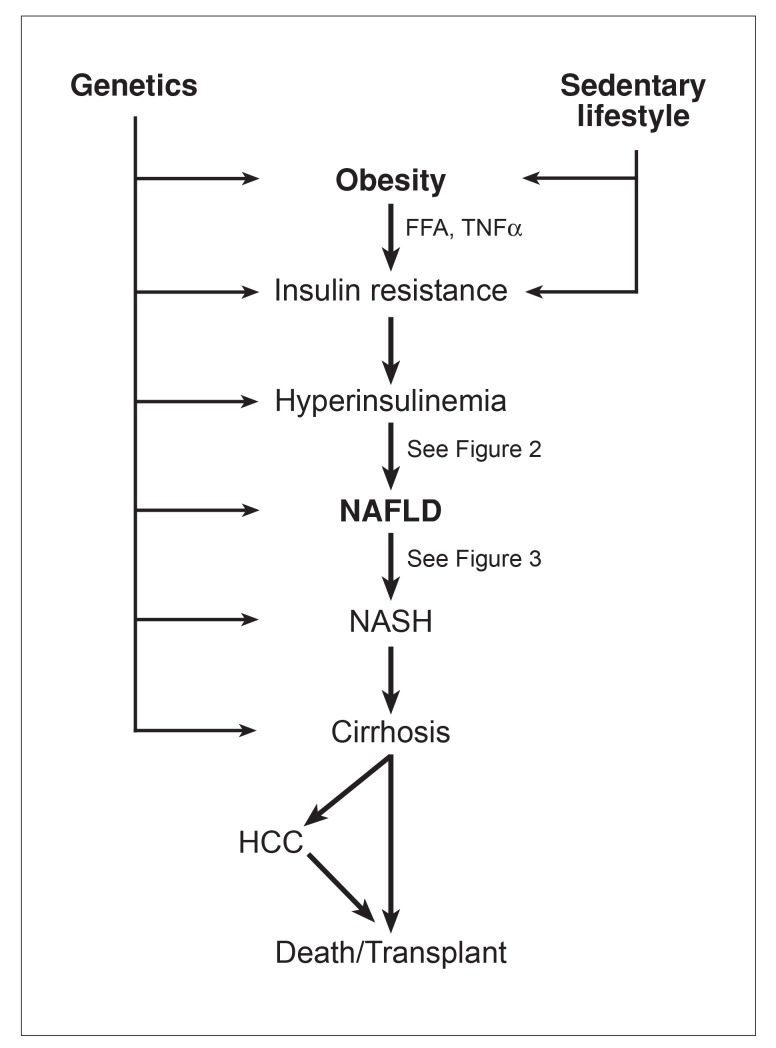
One hypothesis for the pathogenesis of NAFLD is the “two-hit” hypothesis proposed by Day and James in 1998.62 According to this paradigm, the primary abnormality is a metabolic disturbance—most frequently insulin resistance—which causes NAFLD, then a second hit induces injury and inflammation, or NASH and its sequelae (Figure 1).
Figure 1.
Genetics and obesity contribute to the development of insulin resistance and these three factors together lead to the development of nonalcoholic fatty liver disease (NAFLD). The presence of NAFLD puts certain individuals at risk for developing nonalcoholic steatohepatitis (NASH), cirrhosis, hepatocellular carcinoma (HCC), and death from end-stage liver disease or liver transplantation.
FFA = free fatty acids; TNF = tumor necrosis factor.
First Hit
The presence of excess fat is a prerequisite for the subsequent events of NASH. The main characteristic of NAFLD is the accumulation of triglycerides (TG) as fat droplets within the cytoplasm of hepatocytes. It is defined practically as more than 10% of hepatocytes having fat droplets evident on liver biopsy.63 Increased delivery of both free fatty acids (FFA) and TG to the liver, diminished hepatic utilization of FFA, diminished export of TG from the liver, and impaired beta-oxidation of FFA within hepatocytes cause TG accumulation within the cytoplasm of hepatocytes.64-66 Excess carbohydrates, either from dietary sources or de novo gluconeogenesis in the liver, is also a major stimulus for de novo fatty acid synthesis in the liver. Paradoxically, direct uptake of dietary fat as chylomicron remnants or FFA constitutes a relatively minor contribution to liver fat accumulation.67
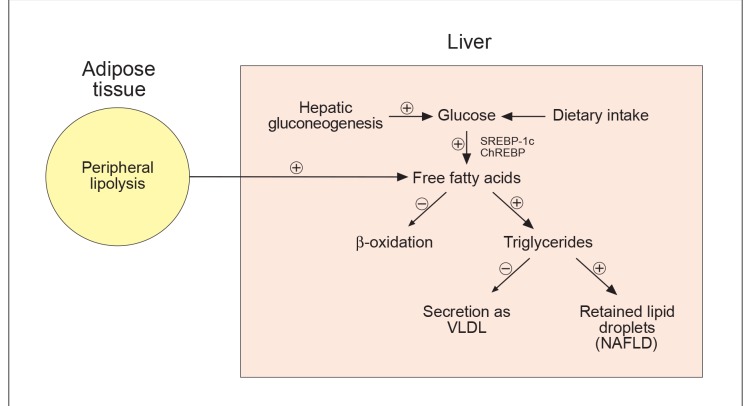
Insulin resistance is a common cause of fat accumulation in the liver. However, we also know that a small subgroup of NAFLD patients do not exhibit detectable features of impaired insulin sensitivity. This suggests that possibilities other than insulin resistance are important in a subset of patients. Furthermore, a growing body of evidence suggests that insulin resistance does not act only as a first hit, but also may play an important role in the inflammation and hepatocellular injury that characterize NASH (Figure 2).63,66,68
Figure 2.
Metabolic pathways altered by insulin resistance and hyperinsulinemia. Pathways marked by “+” signs are increased and those marked by “-” signs are inhibited. Hyperinsulinemia and insulin resistance increase both hepatic glucose production and adipose tissue free fatty acid (FFA) release, respectively, and circulating FFA are taken up by the liver. In adipocytes, insulin resistance impairs glucose uptake, further contributing to the need for increased insulin levels. In the liver, hyperinsulinemia induces sterol regulatory element—binding protein-1c (SREBP-1c) expression while hyperglycemia activates carbohydrate response element—binding protein (ChREBP). The activation of both SREBP-1c and ChREBP induces lipogenic enzymes that convert excess glucose to fatty acids in the liver. Excess fatty acids undergo mitochondrial β-oxidation or are esterified to produce triglycerides. Excess triglycerides that are not secreted as very-low-density lipoproteins (VLDL) are stored as fat droplets within the cytoplasm of hepatocytes to cause nonalcoholic fatty liver disease (NAFLD).
Second Hit
A liver with excess fat may be more vulnerable to stressors such as reactive oxygen species (ROS), adipokines, and cytokines than a normal liver. The regenerative capacity of a fatty liver is also impaired. Yang and colleagues demonstrated that obese mice with fatty livers clear endotoxins less than nonobese controls.69 Nonetheless, the factors that play key roles in the development of NASH from NAFLD remain uncertain. Some possibilities include the duration of fatty infiltration of the liver and the duration and severity of hyperinsulinemia. Other possible second hits are oxidative stress (increased ROS and decreased antioxidants), lipid peroxidation and reactive metabolites such as malondialdehyde and 4-hydroxynonenal, adipose tissue products, transforming growth factor-β,1 Fas ligand, mitochondrial dysfunction and respiratory chain deficiency, and small intestinal bacterial overgrowth (endotoxins and TNF-α) (Figure 3).63,66,70
Figure 3.
Multiple mechanisms may play a role in causing hepatocellular injury in the setting of nonalcoholic fatty liver disease, many of which generate reactive oxygen species (ROS). For example, peroxisomal fatty acid oxidation generates hydrogen peroxide, “electron leak” from the mitochondrial respiratory chain produces superoxide, sinusoidal Kupffer cells release superoxide when stimulated by endotoxin, cytochrome P450 metabolism of fatty acids leads to electron leak from downstream redox factors to release superoxide and gut-derived ethanol may cause ROS production during its hepatocellular metabolism. Mechanisms of injury not requiring ROS may also be important and include adenosine triphosphate (ATP) depletion and disrupted organelle membranes. Hepatocytes respond with morphological changes such as ballooning, cytoskeletal protein aggregation, apoptosis, and necrosis. Individually or in sum, these processes stimulate inflammation and fibrogenesis, the latter leading to cirrhosis in some patients.
Adipose tissue is now recognized as a source of important metabolic and inflammatory mediators. These adipokines have both proinflammatory (leptin, TNF-α, and IL-6) and anti-inflammatory (adiponectin) effects.68,71-75 Adiponectin also has antilipogenic effects. Adipokines regulate both hepatic and peripheral glucose and lipid metabolism. Although these cytokines and hormones normally work in a balance, this homeostasis may be disturbed in NASH patients and studies are now focusing on these changes. NASH patients have reduced adiponectin levels and increased TNF-α levels.75,76
Hepatocyte Injury and NASH Pathology
Hepatocyte ballooning is one of the features of injury observed on NASH liver biopsies.28 Whether ballooning of hepatocytes is an adaptive (physiologic) or degenerative (pathologic) change of hepatocytes is unknown. The initial response of hepatocytes to a stressor is to increase in volume,77-82 and mild volume changes (up to 5–10%) without biochemical evidence of free radicals may be physiologic or adaptive. However, greater swelling of hepatocytes (≥30% volume increase) is usually degenerative and can cause stress protein expression, macromolecular overcrowding, disturbed cellular architecture, Mallory hyaline formation, hepatocyte apoptosis, necrosis, and cell death.
Clinical Features, Biochemical Abnormalities, and Radiological Evidence of NAFLD
NAFLD occurs at equal rates among males and females.63 The majority of cases are found within the fourth or fifth decade of life, although the full spectrum has also been described in children. Patients with NAFLD are often obese and may have hypertension. The most frequent symptoms are fatigue and right upper quadrant pain or dullness, although many patients have no symptoms. Mild or moderate hepatomegaly is one of the most common physical examination findings. Biochemically, patients with NAFLD may have hyperlipidemia, hyperglycemia, hyperinsulinemia, and reduced insulin sensitivity.63
Aminotransferases are often mildly or moderately increased, with an aspartate aminotransferase (AST)/ALT ratio less than 1, although the prevalence of NAFLD in patients with normal aminotransferases is difficult to estimate. Inversion of the AST/ALT ratio to greater than 1 suggests progression to cirrhosis83 or covert alcohol consumption; however, serum aminotransferase values fluctuate during the course of the disease.63 Moreover, NAFLD patients with normal aminotransferases can exhibit the full spectrum of histopathologic abnormalities from benign steatosis to cirrhosis.84 Gamma-glutamyltranspeptidase can also be elevated in patients with NAFLD but is not a reliable test for the presence of NASH. Unfortunately, there is also no good correlation between serum liver tests and necroinflammatory activity or stages.63 Ferritin is usually elevated and may indicate increased steatosis and inflammation or the severity of fibrosis.85,86 Abdominal ultrasonography, computed tomography, and magnetic resonance imaging (MRI) all can identify NAFLD, but cannot separate benign steatosis from NASH.87-90 MRI, particularly localized proton magnetic resonance spectroscopy, has the capability of accurately measuring hepatic TG content but is costly.32,91,92
Histopathologic Features of NAFLD
Grading, Staging, and Individual Histopathologic Features of NAFLD
Liver biopsy is the gold standard diagnostic tool not only to reach a correct diagnosis and to document grading of necroinflammation and staging of fibrosis, but also to predict prognosis in patients with clinical or radiologic evidence of NAFLD. A commonly used method for the pathologic evaluation of NASH is the system established by Brunt and colleagues93 and its recent revision.94 The newly revised system includes grading of necroinflammatory activity and staging of fibrosis (Table 3). This system requires only routine histochemical stains and includes 14 histologic features. A NALFD activity score was proposed based on the unweighted sum of the steatosis, lobular inflammation, and ballooning scores. Scores of 0–2 were usually not considered to be NASH, 3–4 possibly NASH, and 5–8 usually indicative of NASH. Although the scoring system covers the range of histologic features of pediatric NAFLD, some difficulties remain in the application of this system to pediatric subjects.
Table 3.
Proposed Grading and Staging System of NASH94
| Histologic Feature | Definition | Score |
|---|---|---|
| Steatosis | ||
| Grade | The evaluation of parenchymal involvement by steatosis | |
| <5% | 0 | |
| 5–33% | 1 | |
| >33–66% | 2 | |
| >66% | 3 | |
| Location/predominant distribution pattern | Zone 3 | 0 |
| Zone 1 | 1 | |
| Azonal | 2 | |
| Panacinar | 3 | |
| Microvesicular steatosis | Presence of contiguous patches | 1 |
| Fibrosis | ||
| Stage | None | 0 |
| Perisinusoidal or periportal | 1 | |
| Mild, zone 3, perisinusoidal | 1A | |
| Moderate, zone 3, perisinusoidal | 1B | |
| Portal/periportal | 1C | |
| Perisinusoidal and portal/periportal | 2 | |
| Bridging fibrosis | 3 | |
| Cirrhosis | 4 | |
| Inflammation | ||
| Lobular inflammation | Overall assessment of all inflammatory foci | |
| No foci | 0 | |
| <2 foci per 200X field | 1 | |
| 2–4 foci per 200X field | 2 | |
| >4 foci per 200X field | 3 | |
| Microgranulomas | Presence of small aggregates of macrophages | 1 |
| Large lipogranulomas | Present, usually in portal areas or adjacent to central veins | 1 |
| Portal inflammation | Greater than minimal when assessed from low magnification | 1 |
| Liver Cell Injury | ||
| Ballooning | None | 0 |
| Few balloon cells | 1 | |
| Many cells/prominent ballooning | 2 | |
| Acidophil bodies | Many | 1 |
| Pigmented macrophages | Many | 1 |
| Megamitochondria | Many | 1 |
| Other findings | ||
| Mallory hyaline | Many visible on routine stains | 1 |
| Glycogenated nuclei | Many contiguous patches | 1 |
Both steatosis and necroinflammation predominantly involve zone 3. The staging of NASH using this system begins with perisinusoidal fibrosis and progresses to portal fibrosis, bridging fibrosis, and cirrhosis. Ballooning of hepatocytes and Mallory hyaline are the two hallmarks of ongoing injury and inflammation and have been associated with hepatic fibrosis (Table 4).95 A pathologic typing system of NAFLD has also been described as a predictor of outcomes (Table 5).1
Table 4.
Histopathologic Abnormalities in NASH
|
Table 5.
Matteoni Typing System for NAFLD Associated with Outcomes1
| Type 1: Fatty liver alone |
| Type 2: Fat and inflammation |
| Type 3: Fat and ballooned hepatocytes |
| Type 4: Fat and ballooned hepatocytes and either Mallory bodies or fibrosis |
NASH-associated Cirrhosis
Initial studies defined NAFLD-associated cirrhosis on the basis of a history of metabolic abnormalities. Powell and colleagues reported that the features of steatohepatitis may disappear with fibrosis progression96 and Caldwell and coauthors reported that some cryptogenic cirrhosis cases do not show any characteristic pathologic features of NAFLD (burned-out NASH).2 However, these patients typically had NAFLD-associated metabolic abnormalities and subsequent studies have shown that most of the cryptogenic cirrhosis cases had prior NASH, particularly within obese and diabetic groups.3-5,39,40,97,98 Recently, Hui and colleagues proposed a definition for NAFLD-associated cirrhosis using strict clinicopathologic criteria.98 Their case definition requires clinical risk factors for more than 5 years such as obesity, diabetes, and hyperlipidemia and a pathologic description (Table 6). HCC may also be a late complication of the metabolic syndrome and NASH, typically in the setting of cirrhosis.6-8
Table 6.
Histopathologic Criteria of the Proposed Typing System for NASH-Associated Cirrhosis98
| 1. Definite: Steatosis plus intralobular mixed inflammatory foci |
| 2. Probable: Steatosis plus intralobular mononuclear inflammation |
| 3a. Possible: Intralobular mixed inflammation without steatosis |
| 3b. Possible: Steatosis without any inflammation |
| 4. Cryptogenic cirrhosis (burned-out NASH): No steatosis and no inflammation |
When to perform a liver biopsy in a patient with imaging evidence of NAFLD or risk factors for NASH remains an unresolved issue. A biopsy is generally warranted to further evaluate persistently elevated aminotransferases even when NAFLD is suspected on clinical grounds because a biopsy can identify another diagnosis or lead to changes in therapy up to a third of the time.99 Data from several series of patients undergoing bariatric surgery that show a high prevalence of advanced liver disease despite normal aminotransferases suggest that a liver biopsy should be considered in patients with risk factors for advanced disease such as extreme obesity, diabetes, or an elevated AST/ALT ratio despite normal enzymes.53,54,100 By comparison, deferring a liver biopsy while lifestyle modifications are pursued in earnest may be a reasonable alternative in a young person found to have elevated aminotransferases after weight gain if imaging demonstrates NAFLD and other causes of chronic liver disease are excluded. The inherent risk of this approach is the possibility of missing significant treatable liver diseases such as Wilson disease and autoimmune hepatitis.
Natural History of NAFLD
Knowledge about the natural course of NAFLD is still limited to relatively few small studies. Cross-sectional studies reported 30–40% of NASH patients had advanced fibrosis and 10–15% had cirrhosis at the time of biopsy.63
Natural History of NAFLD in Longitudinal Studies
An early follow-up study of 26 patients with NAFLD for a median of 11 years showed that steatosis alone is usually a benign, nonprogressive condition and its prognosis is favorable,101 although a study of 59 patients with benign steatosis reported that 2 patients (3.4%) did progress to cirrhosis.1 A recently published study investigating patients with fatty livers alone in both nonalcoholic and alcoholic groups (median follow-up 19.9 years in the nonalcoholic group) showed that 1 nonalcoholic patient (0.6%) developed cirrhosis during the follow-up period,102 whereas a larger population-based study in Minnesota over 20 years found that a diagnosis of NAFLD was associated with increased mortality, especially in those with impaired glucose tolerance or cirrhosis.103
Natural History of NASH in Longitudinal Studies
Matteoni and colleagues reported that 25% of patients with fibrosis develop cirrhosis within 10–25 years.1 Four histologic follow-up studies have given some important clues about the natural history of NASH (Table 7).9,16,26,27 The reported fibrosis progression rates in these studies are slower than those of patients with alcoholic liver disease and chronic hepatitis C infection, which measure at 0.12 units of fibrosis per year.9,14-16
Table 7.
Summary of Longitudinal Natural History Studies
| Source | Number of Patients | Follow-up Period (mean, years) | Fibrosis Progression (% of patients) | Fibrosis Regression (% of patients) | Rate of Fibrosis Progression (stages/year) |
|---|---|---|---|---|---|
| Evans26* | 7 | 8.2 | 57% | None | 0.088† |
| Harrison27* | 22 | 5.7 | 32% | 18% | Not reported |
| Fassio16‡ | 22 | 4.3 | 32% | 18% | 0.059† |
| Adams9* | 103 | 3.2 | 37% | 29% | 0.09† |
Therapy of NAFLD
For the patient with comorbidities such as obesity, hyperlipidemia, or type-2 diabetes, lifestyle modifications that include exercise and changing dietary habits to achieve gradual and sustained weight loss are the primary recommendations. It was reported that both hepatic steatosis and inflammation respond rapidly to changed environmental conditions such as weight loss, although the response of fibrosis is slow.104 If the patient’s condition does not improve despite these interventions, medications may be considered. Goals for the pharmacologic therapy of NAFLD should target both the accumulation of fat and the consequent injury and fibrosis (Table 8).63,105,106 One pharmacologic agent, ursodiol acid, was evaluated over a 2-year period in a randomized, placebo-controlled study and showed no more benefit than placebo.107 Interventions for the treatment of NAFLD raise the important question of how these patients should be monitored for therapy effectiveness. To evaluate and compare histopathologic features of the initial and final biopsies is the best method but the decision to obtain liver biopsies must weigh the risks and benefits. In this regard, noninvasive follow-up markers would be beneficial. Potentially useful serum markers such as hyaluronic acid or the measurement of insulin sensitivity or serum cytokines levels such as adiponectin, leptin, and TNF-α may be promising for future applications.
Table 8.
|
TNF = tumor necrosis factor.
Conclusion
There has been growing concern and interest in NAFLD in the last decade, and each month approximately five new papers about NAFLD are published. With its increasing prevalence, it is estimated that NAFLD will eventually become the most frequently seen liver disease. Understanding the underlying causes of NAFLD and designing rational treatments will require continued research with collaboration among investigators in fields such as endocrinology, pathology, biochemistry, and biophysics.
References
- 1.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 2.Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–669. doi: 10.1002/hep.510290347. [DOI] [PubMed] [Google Scholar]
- 3.Poonawala A, Nair SP, Thuluvath PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology. 2000;32:689–692. doi: 10.1053/jhep.2000.17894. [DOI] [PubMed] [Google Scholar]
- 4.Ong J, Younossi ZM, Reddy V, et al. Cryptogenic cirrhosis and posttransplantation nonalcoholic fatty liver disease. Liver Transpl. 2001;7:797–801. doi: 10.1053/jlts.2001.24644. [DOI] [PubMed] [Google Scholar]
- 5.Charlton M, Kasparova P, Weston S, et al. Frequency of nonalcoholic steatohepatitis as a cause of advanced liver disease. Liver Transpl. 2001;7:608–614. doi: 10.1053/jlts.2001.25453. [DOI] [PubMed] [Google Scholar]
- 6.Ratziu V, Bonyhay L, Di Martino V, et al. Survival, liver failure, and hepatocellular carcinoma in obesity-related cryptogenic cirrhosis. Hepatology. 2002;35:1485–1493. doi: 10.1053/jhep.2002.33324. [DOI] [PubMed] [Google Scholar]
- 7.Bugianesi E, Leone N, Vanni E, et al. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology. 2002;123:134–140. doi: 10.1053/gast.2002.34168. [DOI] [PubMed] [Google Scholar]
- 8.El-Serag HB. Hepatocellular carcinoma: recent trends in the United States. Gastroenterology. 2004;127:S27–S34. doi: 10.1053/j.gastro.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol. 2005;42:132–138. doi: 10.1016/j.jhep.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 10.Caldwell SH, Hespenheide EE. Subacute liver failure in obese women. Am J Gastroenterol. 2002;97:2058–2062. doi: 10.1111/j.1572-0241.2002.05922.x. [DOI] [PubMed] [Google Scholar]
- 11.Falck-Ytter Y, Younossi ZM, Marchesini G, McCullough AJ. Clinical features and natural history of nonalcoholic steatosis syndromes. Sem Liver Dis. 2001;21:17–26. doi: 10.1055/s-2001-12926. [DOI] [PubMed] [Google Scholar]
- 12.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003;98:960–967. doi: 10.1111/j.1572-0241.2003.07486.x. [DOI] [PubMed] [Google Scholar]
- 13.Ruhl CE, Everhart JE. Determinants of the association of overweight with elevated serum alanine aminotransferase activity in the United States. Gastroenterology. 2003;124:71–79. doi: 10.1053/gast.2003.50004. [DOI] [PubMed] [Google Scholar]
- 14.Sorensen TI, Orholm M, Bentsen KD, Hoybye G, Eghoje K, Christoffersen P. Prospective evaluation of alcohol abuse and alcoholic liver injury in men as predictors of development of cirrhosis. Lancet. 1984;2:241–244. doi: 10.1016/s0140-6736(84)90295-2. [DOI] [PubMed] [Google Scholar]
- 15.Ghany MG, Kleiner DE, Alter H, et al. Progression of fibrosis in chronic hepatitis C. Gastroenterology. 2003;124:97–104. doi: 10.1053/gast.2003.50018. [DOI] [PubMed] [Google Scholar]
- 16.Fassio E, Alvarez E, Dominguez N, Landeira G, Longo C. Natural history of nonalcoholic steato hepatitis: a longitudinal study of repeat liver biopsies. Hepatology. 2004;40:820–826. doi: 10.1002/hep.20410. [DOI] [PubMed] [Google Scholar]
- 17.Clark JM, Diehl AM. Defining nonalcoholic fatty liver disease: implications for epidemiologic studies. Gastroenterology. 2003;124:248–250. doi: 10.1053/gast.2003.50032. [DOI] [PubMed] [Google Scholar]
- 18.Marchesini G, Brizi M, Morselli-Labate AM, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107:450–455. doi: 10.1016/s0002-9343(99)00271-5. [DOI] [PubMed] [Google Scholar]
- 19.Marchesini G, Brizi M, Bianchi G, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844–1850. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 20.Chitturi S, Farrell GC. Etiopathogenesis of nonalcoholic steato hepatitis. Semin Liver Dis. 2001;21:27–41. doi: 10.1055/s-2001-12927. [DOI] [PubMed] [Google Scholar]
- 21.Seppälä-Lindroos A, Vehkavaara S, Häkkinen A-M, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endo Metab. 2002;87:3023–3028. doi: 10.1210/jcem.87.7.8638. [DOI] [PubMed] [Google Scholar]
- 22.Pagano G, Pacini G, Musso G, et al. Nonalcoholic steatohepatitis, insulin resistance, and metabolic syndrome: further evidence for an etiologic association. Hepatology. 2002;35:367–372. doi: 10.1053/jhep.2002.30690. [DOI] [PubMed] [Google Scholar]
- 23.Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–923. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 24.Bugianesi E, Zannoni C, Vanni E, Marzocchi R, Marchesini G. Non-alcoholic fatty liver and insulin resistance: a cause-effect relationship? Dig Liver Dis. 2004;36:165–173. doi: 10.1016/j.dld.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 25.Reaven G. The metabolic syndrome or the insulin resistance syndrome? Different names, different concepts, and different goals. Endocrinol Metab Clin North Am. 2004;33:283–303. doi: 10.1016/j.ecl.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Evans CDJ, Oien KA, MacSween RNM, Mills PR. Non-alcoholic steatohepatitis: a common cause of progressive chronic liver injury? J Clin Pathol. 2002;55:689–692. doi: 10.1136/jcp.55.9.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrison SA, Torgerson S, Hayashi PH. The natural history of nonalcoholic fatty liver disease: a clinical histopathological study. Am J Gastroenterol. 2003;98:2042–2047. doi: 10.1111/j.1572-0241.2003.07659.x. [DOI] [PubMed] [Google Scholar]
- 28.Brunt EM. Nonalcoholic steatohepatitis: definition and pathology. Semin Liver Dis. 2001;21:3–16. doi: 10.1055/s-2001-12925. [DOI] [PubMed] [Google Scholar]
- 29.Brunt EM, Ramrahkiani S, Cordes BG, et al. Concurrence of histologic features of steatohepatitis with other forms of chronic liver disease. Mod Pathol. 2003;16:49–56. doi: 10.1097/01.MP.0000042420.21088.C7. [DOI] [PubMed] [Google Scholar]
- 30.Bellentani S, Saccoccio G, Costa G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage: the Dionysos Study Group. Gut. 1997;41:845–850. doi: 10.1136/gut.41.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim WR, Brown RS, Jr., Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227–242. doi: 10.1053/jhep.2002.34734. [DOI] [PubMed] [Google Scholar]
- 32.Szczepaniak LS, Nurenberg P, Leonard D, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol. 2005;288:E462–468. doi: 10.1152/ajpendo.00064.2004. [DOI] [PubMed] [Google Scholar]
- 33.Nomura H, Kashiwagi S, Hayashi J, Kajiyama W, Tani S, Goto M. Prevalence of fatty liver in a general population of Okinawa, Japan. Jpn J Med. 1988;27:142–149. doi: 10.2169/internalmedicine1962.27.142. [DOI] [PubMed] [Google Scholar]
- 34.Bellentani S, Tiribelli C, Saccoccio G, et al. Prevalence of chronic liver disease in the general population of northern Italy: the Dionysos Study. Hepatology. 1994;20:1442–1449. doi: 10.1002/hep.1840200611. [DOI] [PubMed] [Google Scholar]
- 35.Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137:1–9. doi: 10.7326/0003-4819-137-1-200207020-00006. [DOI] [PubMed] [Google Scholar]
- 36.Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005;42:44–52. doi: 10.1002/hep.20734. [DOI] [PubMed] [Google Scholar]
- 37.Fan J-G, Zhu J, Li X-J, et al. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol. 2005;43:508–514. doi: 10.1016/j.jhep.2005.02.042. [DOI] [PubMed] [Google Scholar]
- 38.McGlynn KA, London WT. Epidemiology and natural history of hepatocellular carcinoma. Baillieres Best Pract Res Clin Gastroenterol. 2005;19:3–23. doi: 10.1016/j.bpg.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 39.Caldwell SH, Harris DM, Patrie JT, Hespenheide EE. Is NASH underdiagnosed among African Americans? Am J Gastroenterol. 2002;97:1496–1500. doi: 10.1111/j.1572-0241.2002.05795.x. [DOI] [PubMed] [Google Scholar]
- 40.Browning JD, Kumar KS, Saboorian MH, Thiele DL. Ethnic differences in the prevalence of cryptogenic cirrhosis. Am J Gastroenterol. 2004;99:292–298. doi: 10.1111/j.1572-0241.2004.04059.x. [DOI] [PubMed] [Google Scholar]
- 41.Daniel S, Ben-Menachem T, Vasudevan G, Ma CK, Blumenkehl M. Prospective evaluation of unexplained chronic liver transaminase abnormalities in asymptomatic and symptomatic patients. Am J Gastroenterol. 1999;94:3010–3014. doi: 10.1111/j.1572-0241.1999.01451.x. [DOI] [PubMed] [Google Scholar]
- 42.Ratziu V, Giral P, Charlotte F, et al. Liver fibrosis in overweight patients. Gastroenterology. 2000;118:1117–1123. doi: 10.1016/s0016-5085(00)70364-7. [DOI] [PubMed] [Google Scholar]
- 43.Skelly MM, James PD, Ryder SD. Findings on liver biopsy to investigate abnormal liver function tests in the absence of diagnostic serology. J Hepatol. 2001;35:195–199. doi: 10.1016/s0168-8278(01)00094-0. [DOI] [PubMed] [Google Scholar]
- 44.Liangpunsakul S, Chalasani N. Unexplained elevations in alanine aminotransferase in individuals with the metabolic syndrome: results from the third National Health and Nutrition Survey (NHANES III) Am J Med Sci. 2005;329:111–116. doi: 10.1097/00000441-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 45.Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–1110. doi: 10.1002/hep.1840120505. [DOI] [PubMed] [Google Scholar]
- 46.Sanyal AJ, Campbell-Sargent C, Mirshani F, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–1192. doi: 10.1053/gast.2001.23256. [DOI] [PubMed] [Google Scholar]
- 47.Chitturi S, Abeygunasekera S, Farrell GC, et al. NASH and insulin resistance: insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002;35:373–379. doi: 10.1053/jhep.2002.30692. [DOI] [PubMed] [Google Scholar]
- 48.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 49.Formiguera X, Cantón A. Obesity: epidemiology and clinical aspects. Baillieres Best Pract Res Clin Gastroenterol. 2004;18:1125–1146. doi: 10.1016/j.bpg.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 50.Andersen T, Christoffersen P, Gluud C. The liver in consecutive patients with morbid obesity: a clinical, morphological, and biochemical study. Int J Obes. 1984;8:107–115. [PubMed] [Google Scholar]
- 51.Tominaga K, Kurata JH, Chen YK, et al. Prevalence of fatty liver in Japanese children and relationship to obesity. An epidemiological ultrasonographic survey. Dig Dis Sci. 1995;40:2002–2009. doi: 10.1007/BF02208670. [DOI] [PubMed] [Google Scholar]
- 52.Sanyal A. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;1213:1705–1725. doi: 10.1053/gast.2002.36572. [DOI] [PubMed] [Google Scholar]
- 53.Luyckx FH, Desaive C, Thiry A, et al. Liver abnormalities in severely obese subjects: effect of drastic weight loss after gastroplasty. Int J Obes Related Metab Disord. 1998;22:222–226. doi: 10.1038/sj.ijo.0800571. [DOI] [PubMed] [Google Scholar]
- 54.García-Monzón C, Martín-Pérez E, Iacono OL, et al. Characterization of pathogenic and prognostic factors of nonalcoholic steatohepatitis associated with obesity. J Hepatol. 2000;33:716–724. doi: 10.1016/s0168-8278(00)80301-3. [DOI] [PubMed] [Google Scholar]
- 55.Ong JP, Elariny H, Collantes R, et al. Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Obes Surg. 2005;15:310–315. doi: 10.1381/0960892053576820. [DOI] [PubMed] [Google Scholar]
- 56.Baldridge AD, Perez-Atayde AR, Graeme-Cook F, Higgins L, Lavine JE. Idiopathic steatohepatitis in childhood: a multicenter retrospective study. J Pediatr. 1995;127:700–704. doi: 10.1016/s0022-3476(95)70156-7. [DOI] [PubMed] [Google Scholar]
- 57.Noguchi H, Tazawa Y, Nishinomiya F, Takada G. The relationship between serum transaminase activities and fatty liver in children with simple obesity. Acta Paediatrica Japonica. 1995;37:621–625. doi: 10.1111/j.1442-200x.1995.tb03389.x. [DOI] [PubMed] [Google Scholar]
- 58.Rashid M, Roberts EA. Nonalcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr. 2000;30:48–53. doi: 10.1097/00005176-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 59.Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107:1103–1109. doi: 10.1016/0016-5085(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 60.Assy N, Kaita K, Mymin D, Levy C, Rosser B, Minuk G. Fatty infiltration of liver in hyperlipidemic patients. Dig Dis Sci. 2000;45:1929–1934. doi: 10.1023/a:1005661516165. [DOI] [PubMed] [Google Scholar]
- 61.Steiner G. Hyperinsulinaemia and hypertriglyceridaemia. J Intern Med Supplement. 1994;736:23–26. [PubMed] [Google Scholar]
- 62.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 63.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 64.Lewis GF, Carpentier A, Adeli K, Giacca A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr Rev. 2002;23:201–229. doi: 10.1210/edrv.23.2.0461. [DOI] [PubMed] [Google Scholar]
- 65.Haque M, Sanyal AJ. The metabolic abnormalities associated with non-alcoholic fatty liver disease. Baillieres Best Pract Res Clin Gastroenterol. 2002;16:709–731. doi: 10.1053/bega.2002.0325. [DOI] [PubMed] [Google Scholar]
- 66.Browning JD, Horton JD. Molecular mediators of hepatic steatosis and liver injury. J Clin Invest. 2004;114:147–152. doi: 10.1172/JCI22422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bugianesi E, Gastaldelli A, Vanni E, et al. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia. 2005;48:634–642. doi: 10.1007/s00125-005-1682-x. [DOI] [PubMed] [Google Scholar]
- 69.Yang SQ, Lin HZ, Lane MD, Clemens M, Diehl AM. Obesity increases sensitivity to endotoxin liver injury: implications for the pathogenesis of steatohepatitis. Proc Natl Acad Sci. 1997;94:2557–2562. doi: 10.1073/pnas.94.6.2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pessayre D, Fromenty B. NASH: a mitochondrial disease. J Hepatol. 2005;42:928–940. doi: 10.1016/j.jhep.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 71.Crespo J, Cayón A, Fernández-Gil P, et al. Gene expression of tumor necrosis factor α and TNF-receptors, p55 and p75, in nonalcoholic steatohepatitis patients. Hepatology. 2001;34:1158–1163. doi: 10.1053/jhep.2001.29628. [DOI] [PubMed] [Google Scholar]
- 72.Chitturi S, Farrell G, Frost L, et al. Serum leptin in NASH correlates with hepatic steatosis but not fibrosis: a manifestation of lipotoxicity? Hepatology. 2002;36:403–409. doi: 10.1053/jhep.2002.34738. [DOI] [PubMed] [Google Scholar]
- 73.Maeda N, Shimomura I, Kishida K, et al. Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med. 2002;8:731–737. doi: 10.1038/nm724. [DOI] [PubMed] [Google Scholar]
- 74.Xu A, Wang Y, Keshaw H, Xu LY, Lam KS, Cooper GJ. The fat-derived hormone adiponectin alleviates alcoholic and nonalcoholic fatty liver diseases in mice. J Clin Invest. 2003;112:91–100. doi: 10.1172/JCI17797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hui JM, Hodge A, Farrell GC, Kench JG, Kriketos A, George J. Beyond insulin resistance in NASH: TNF-α or adiponectin? Hepatology. 2004;40:46–54. doi: 10.1002/hep.20280. [DOI] [PubMed] [Google Scholar]
- 76.Bugianesi E, Pagotto U, Manini R, et al. Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity. J Clin Endo Metab. 2005;90:3498–3504. doi: 10.1210/jc.2004-2240. [DOI] [PubMed] [Google Scholar]
- 77.Haussinger D, Lang F. Cell volume in the regulation of hepatic function: a mechanism for metabolic control. Biochem Biophys Acta. 1991;1071:331–350. doi: 10.1016/0304-4157(91)90001-d. [DOI] [PubMed] [Google Scholar]
- 78.McManus ML, Churchwell KB, Strange K. Regulation of cell volume in health and disease. N Engl J Med. 1995;333:1260–1266. doi: 10.1056/NEJM199511093331906. [DOI] [PubMed] [Google Scholar]
- 79.Lang F, Lepple-Wienhues A, Paulmichl M, Szabo I, Siemen D, Gulbins E. Ion channels, cell volume, and apoptotic cell death. Cell Physiol Biochem. 1998;8:285–292. doi: 10.1159/000016290. [DOI] [PubMed] [Google Scholar]
- 80.Dunkelberg JC, Feranchak AP, Fitz JG. Liver cell volume regulation: size matters. Hepatology. 2001;33:1349–1352. doi: 10.1053/jhep.2001.24750. [DOI] [PubMed] [Google Scholar]
- 81.Minton AP. The influence of macromolecular crowding and macromolecular confinement on biochemical reactions in physiological media. J Biol Chem. 2001;276:10577–10580. doi: 10.1074/jbc.R100005200. [DOI] [PubMed] [Google Scholar]
- 82.Del Monte U. Swelling of hepatocytes injured by oxidative stress suggests pathological changes related to macromolecular crowding. Med Hypotheses. 2005;64:818–825. doi: 10.1016/j.mehy.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 83.Sorbi D, Boynton J, Lindor KD. The ratio of aspartate aminotransferase to alanine aminotransferase: potential value in differentiating nonalcoholic steatohepatitis from alcoholic liver disease. Am J Gastroenterol. 1999;94:1018–1022. doi: 10.1111/j.1572-0241.1999.01006.x. [DOI] [PubMed] [Google Scholar]
- 84.Mofrad P, Contos MJ, Haque M, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37:1286–1292. doi: 10.1053/jhep.2003.50229. [DOI] [PubMed] [Google Scholar]
- 85.Turlin B, Mendler MH, Moirand R, Guyader D, Guillygomarc’h A, Deugnier Y. Histologic features of the liver in insulin resistance-associated iron overload: a study of 139 patients. Am J Clin Pathol. 2001;116:263–270. doi: 10.1309/WWNE-KW2C-4KTW-PTJ5. [DOI] [PubMed] [Google Scholar]
- 86.Bugianesi E, Manzini P, D’Antico S, et al. Relative contribution of iron burden, HFE mutations, and insulin resistance to fibrosis in nonalcoholic fatty liver. Hepatology. 2004;39:179–187. doi: 10.1002/hep.20023. [DOI] [PubMed] [Google Scholar]
- 87.Jacobs JE, Birnbaum BA, Shapiro MA, et al. Diagnostic criteria for fatty infiltration of the liver on contrast-enhanced helical CT. Am J Roentgenology. 1998;171:659–664. doi: 10.2214/ajr.171.3.9725292. [DOI] [PubMed] [Google Scholar]
- 88.Reid AE. Nonalcoholic steatohepatitis. Gastroenterology. 2001;121:710–723. doi: 10.1053/gast.2001.27126. [DOI] [PubMed] [Google Scholar]
- 89.Clark JM, Brancati FL, Diehl AM. Nonalcoholic fatty liver disease. Gastroenterology. 2002;122:1649–1657. doi: 10.1053/gast.2002.33573. [DOI] [PubMed] [Google Scholar]
- 90.Saadeh S, Younossi ZM, Remer EM, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123:745–750. doi: 10.1053/gast.2002.35354. [DOI] [PubMed] [Google Scholar]
- 91.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 92.Thomas EL, Hamilton G, Patel N, et al. Hepatic triglyceride content and its relation to body adiposity: a magnetic resonance imaging and proton magnetic resonance spectroscopy study. Gut. 2005;54:122–127. doi: 10.1136/gut.2003.036566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brunt EM, Janney CJ, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Non-alcoholic steatohepatitis: A proposal for grading and staging the histologic lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 94.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 95.Gramlich T, Kleiner DE, McCullough AJ, Matteoni CA, Boparai N, Younossi ZM. Pathologic features associated with fibrosis in nonalcoholic fatty liver disease. Hum Pathol. 2004;35:196–199. doi: 10.1016/j.humpath.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 96.Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW. The natural history of nonalcoholic steato hepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74–80. doi: 10.1002/hep.1840110114. [DOI] [PubMed] [Google Scholar]
- 97.Ayata G, Gordon FD, Lewis WD, et al. Cryptogenic cirrhosis: clinicopathologic findings at and after liver transplantation. Hum Pathol. 2002;33:1098–1104. doi: 10.1053/hupa.2002.129419. [DOI] [PubMed] [Google Scholar]
- 98.Hui JM, Kench J, Chitturi S, et al. Long-term outcomes of cirrhosis in nonalcoholic steato hepatitis compared with hepatitis C. Hepatology. 2003;38:420–427. doi: 10.1053/jhep.2003.50320. [DOI] [PubMed] [Google Scholar]
- 99.Chapman RW. To perform or not to perform liver biopsy-that is the question. Gut. 2002;51:9–10. doi: 10.1136/gut.51.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sorrentino P, Tarantino G, Conca P, et al. Silent non-alcoholic fatty liver disease-a clinical-histological study. J Hepatol. 2004;41:751–757. doi: 10.1016/j.jhep.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 101.Teli MR, James OF, Burt AD, Bennett MK, Day CP. The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology. 1995;22:1714–1719. [PubMed] [Google Scholar]
- 102.Dam-Larsen S, Franzmann M-B, Christoffersen P, Larsen K, Becker U, Bendtsen F. Histological characteristics and prognosis in patients with fatty liver. Scand J Gastro. 2005;40:460–467. doi: 10.1080/00365520510012217. [DOI] [PubMed] [Google Scholar]
- 103.Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 104.Palmer M, Schaffner F. Effect of weight reduction on hepatic abnormalities in overweight patients. Gastroenterology. 1990;99:1408–1413. doi: 10.1016/0016-5085(90)91169-7. [DOI] [PubMed] [Google Scholar]
- 105.Bugianesi E, Marzocchi R, Villanova N, Marchesini G. Non-alcoholic fatty liver disease/non-alcoholic steatohepatitis (NAFLD/NASH): treatment. Baillieres Best Pract Res Clin Gastroenterol. 2004;18:1105–1116. doi: 10.1016/j.bpg.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 106.Mendes FD, Lindor KD. Recent advances in the treatment of non-alcoholic fatty liver disease. Expert Opinion on Investigational Drugs. 2005;14:29–35. doi: 10.1517/13543784.14.1.29. [DOI] [PubMed] [Google Scholar]
- 107.Lindor KD, Kowdley KV, Heathcote EJ, et al. Ursodeoxycholic acid for treatment of nonalcoholic steatohepatitis: results of a randomized trial. Hepatology. 2004;39:770–778. doi: 10.1002/hep.20092. [DOI] [PubMed] [Google Scholar]
- 108.Zelman S. The liver in obesity. Arch Intern Med. 1952;90:141–156. doi: 10.1001/archinte.1952.00240080007002. [DOI] [PubMed] [Google Scholar]
- 109.Lombardi B. Considerations on the pathogenesis of fatty liver. Lab Invest. 1966;15:1–20. [PubMed] [Google Scholar]
- 110.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clinic Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 111.Harrison SA, Neuschwander-Tetri BA. Pharmacologic management of nonalcoholic fatty liver disease. Clin Liv Dis. 2004;8:715–728. doi: 10.1016/j.cld.2004.04.011. [DOI] [PubMed] [Google Scholar]