Abstract
Heart rate variability is a physiological measure associated with autonomic nervous system activity. This study hypothesized that lower pre-deployment HRV would be associated with higher post-deployment post-traumatic stress disorder (PTSD) symptoms. Three-hundred-forty-three Army National Guard soldiers enrolled in the Warriors Achieving Resilience (WAR) study were analyzed. The primary outcome was PTSD symptom severity using the PTSD Checklist – Military version (PCL) measured at baseline, 3- and 12-month post-deployment. Heart rate variability predictor variables included: high frequency power (HF) and standard deviation of the normal cardiac inter-beat interval (SDNN). Generalized linear mixed models revealed that the pre-deployment PCL*ln(HF) interaction term was significant (p < 0.0001). Pre-deployment SDNN was not a significant predictor of post-deployment PCL. Covariates included age, pre-deployment PCL, race/ethnicity, marital status, tobacco use, childhood abuse, pre-deployment traumatic brain injury, and previous combat zone deployment. Pre-deployment heart rate variability predicts post-deployment PTSD symptoms in the context of higher pre-deployment PCL scores.
Keywords: Post-traumatic stress disorder (PTSD), military, risk factors, combat stress, prediction, longitudinal, heart rate variability
1. Introduction
A variety of risk factors have been identified that contribute to the development of post-deployment combat-related post-traumatic stress disorder (PTSD) (U.S. Department of Defense Task Force on Mental Health, 2007). The majority of PTSD risk factors are based on self-report. Self-report risk factors include: pre-trauma factors (e.g., family or personal history of mental disorders, age at trauma, socioeconomic status, personality traits, previous or early traumatization, negative parenting experiences, education, intelligence), peri-trauma factors (e.g., magnitude of stressor, perceived life threat, traumatic brain injury (TBI), emotional responses, dissociation), and post-trauma factors (e.g., social support, emerging symptoms, subsequent life stress) (Brewin, Andrews, & Valentine, 2000; Hoge, Austin, & Pollack, 2007; King, King, Keane, Fairbank, & Adams, 1998; Ozer, Best, Lipsey, & Weiss, 2003; Ehlers, Mayou, & Bryant, 1998; Marmar et al., 2006; Shalev, Peri, Canetti, & Schreiber, 1996). Pre-deployment self-report risk factors for PTSD in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) Veterans also include: positive pre-deployment mental health screen, previous combat exposure, number of deployments, enlisted pay grade, and pre-military violence exposure (Koffel, Polusny, Arbisi, & Erbes, 2013; Phillips, Leardmann, Gumbs, & Smith, 2010; Sandweiss et al., 2011; Yurgil et al., 2013).
Historically, studies identified post-deployment associations between biological factors and PTSD symptoms. For example, in World Wars I and II, elevated post-deployment physiological reactivity to auditory stimuli was associated with poor mental health outcomes (Kardiner, 1941; Meakins & Wilson, 1918). More recent studies have found that physiological reactivity (increased heart rate, cardiac acceleration, skin conductance, and motor eye-blink response) to audiovisual combat cues and individually-tailored imagery scripts of stressful combat experiences discriminated veterans with PTSD from veterans without PTSD, veterans with other psychiatric disorders, and non-veterans (Blanchard, Kolb, & Prins, 1991; Pitman, Orr, Forgue, de Jong, & Claiborn, 1987; Wolfe et al., 2000; Forneris, Butterfield, & Bosworth, 2004). Even 20 years after combat exposure, physiological measures (heart rate, skin conductance, and eye blink startle) collected while viewing combat-related still pictures and listening to combat-related stimuli correctly classified two-thirds of veterans with and without PTSD (Keane et al., 1998). A limitation of these prior studies is that they were typically cross-sectional and therefore it was not possible to ascertain if these physiological measures represented a higher vulnerability for developing PTSD.
More recently, there are an increasing number of longitudinal studies evaluating physiological pre-trauma predictors of post-trauma PTSD. For example, in firefighters and police officers pre-trauma physiological responses to acoustic startle predicted post-trauma PTSD symptoms (Guthrie & Bryant, 2005; Orr et al., 2012; Pole et al., 2009). In military personnel, pre-deployment physiological predictors of post-deployment PTSD include attention bias, eye gaze tracking, various glucocorticoid receptor pathway components, and DNA methylation (Wald et al., 2013; Beevers, Lee, Wells, Ellis, & Telch, 2011; Rusiecki et al., 2012; van Zuiden et al., 2012). The recent Marine Resiliency Study (MRS) also evaluated pre-deployment heart rate variability (HRV) as a predictor of post-deployment PTSD and found that lower pre-deployment HRV (measured by increased low-frequency (LF) to high-frequency (HF) ratio) was associated with a higher risk of post-deployment PTSD diagnosis in a sample of active duty Marines (Minassian et al., 2015).
The Warriors Achieving Resilience or WAR study reported here examined pre-deployment HRV (measured by HF) as a physiological predictor of post-deployment PTSD in Army National Guard soldiers. HRV was chosen because of its theoretical and empirical association with the autonomic and central nervous systems (Porges, 2007; Thayer, Hansen, Saus-Rose, & Johnsen, 2009). We chose HF for the main analysis because compared to other HRV measures; the interpretation of HF may be the least ambiguous (Billman, 2013; Eckberg, 1997). Reduced HRV has been reported in patients with PTSD, depression, and other anxiety disorders (Agelink, Boz, Ullrich, & Andrich, 2002; Cohen and Benjamin, 2006; Ginsberg, Berry, & Powell, 2010). It has been suggested that higher HRV is associated with psychological resiliency and autonomic flexibility, reflecting the individual's capacity to adapt effectively to changing social or environmental demands and perform cognitive tasks requiring the use of executive functions (McCraty and Zayas, 2014; Thayer et al., 2009).
Physiological pre-trauma predictors of PTSD (such as HRV) remain understudied (Brewin et al., 2000; Ozer et al., 2003). Identifying physiological predictors of post-deployment PTSD is consistent with current National Institute of Mental Health Research Domain Criteria (RDoC) efforts to develop neurobiological measures of psychopathology. (National Institute of Mental Health, 2011) Applying the RDoC Matrix, the domain of functioning for this study is the Arousal and Regulatory Systems and the units of analysis would be Physiology (HRV) and Self-Report (PTSD symptom severity).
Army National Guard soldiers were chosen for the WAR study because National Guard service members may be at increased risk for post-deployment PTSD compared to active duty service members (U.S. Department of Defense Task Force on Mental Health, 2007). Similar to the MRS, the WAR study hypothesized that lower pre-deployment HRV would be associated with greater post-deployment PTSD symptoms. Differences between these studies include sample (MRS active duty Marines, WAR study Army National Guard), longer post-deployment follow-up (MRS 4–6 months post-deployment, WAR study 12-months post-deployment), inclusion of relevant covariates (WAR study includes history of childhood abuse, current tobacco use, and respiratory rate), and outcome measure (MRS Clinician-Administered PTSD Scale, WAR study PTSD Checklist).
OEF/OIF post-deployment rates of PTSD range from 5.5 to 13.2% suggesting that most military service members are resilient to this post-deployment outcome (Kok, Herrell, Thomas, & Hoge, 2012). However, there is an urgent need to identify physiological and modifiable risk factors for post-deployment mental health problems.
2. Methods and materials
2.1. Design
The results reported here are part of a larger longitudinal study that included a pre-deployment assessment and two post-deployment assessments at 3- and 12-months post-deployment. There were two aspects to this study, one was examining pre-deployment predictors of post-deployment PTSD symptoms (reported here) and the other was testing pre-deployment resilience trainings (will be reported elsewhere). There were three resilience training study arms: control arm (no additional training), HRV biofeedback, and cognitive bias feedback. The active study arms each received one hour of classroom training which occurred after pre-deployment data collection. The results reported here examined the relationship between pre-deployment HRV and 3- and 12-month post-deployment PTSD symptom severity. This study was approved by the Army Human Research Protection Office and the Central Arkansas Veterans Healthcare System Institutional Review Board.
2.2. Participants
Virginia Army National Guard soldiers assigned to either an Aviation or Infantry battalions scheduled to deploy to Iraq in 2011 were recruited to participate. Commanders of both units approved the study for their assigned soldiers. The Aviation battalion deployed in May 2011 and returned in December 2011 and the Infantry battalion deployed in July 2011 and returned December 2011. The withdrawal of American military forces from Iraq was completed by December 2011.
2.3. Inclusion/exclusion criteria
Army National Guard soldiers were eligible for the study if they were scheduled to deploy for OIF/OEF operations within the next 12 months, age 18–60, willing to provide the name and phone number of at least one person to help locate the member for the follow-up assessments, and were not taking beta-blockers or daytime benzodiazepines. Soldiers were not excluded for taking the following medications: antidepressant (N = 2), stimulant (N = 3), antihypertensive (mostly angiotensin-converting enzyme inhibitor, N = 16). No soldiers reported taking prazosin.
2.4. Recruitment and data collection procedures
The study was presented to large groups of soldiers during a pre-deployment Soldier Readiness Processing (SRP) drill weekend. Each soldier met privately with a member of the research team who explained the study. Those who were interested in participating in the study completed a written informed consent process and eligibility screening at that time. Commanders were not informed about whether or not a soldier was participating in the study. A similar recruitment procedure was used successfully in a previous study of active duty Army soldiers (Vasterling et al., 2006). The 3- and 12-month post-deployment follow-up assessments were similarly voluntary and completed in-person during drill weekend (except for 29.8% (70/235) of 12-month assessments that were completed by phone or mail). Approximately one and two years passed between pre-deployment data collection and 3- and 12-month post-deployment assessments, respectively.
A total of 600 soldiers completed the written consent process resulting in a 54% (600/1112) participation rate. Pre-deployment data were collected during a subsequent 2-week pre-deployment training. Four-hundred twenty-six soldiers completed the pre-deployment assessment during pre-deployment training. Fifteen of these soldiers did not deploy and were excluded from further analyses. Of the 411 remaining participating soldiers (N = 114 Aviation, N = 297 Infantry), 83.5% (343/411) completed one or both of the post-deployment research assessments. Three-hundred and seven soldiers completed the 3-month and 235 completed the 12-month follow-ups. Sixty (17.5%) participants had at least one missing data point including 30 soldiers whose HRV measures were considered to be unusable (defined below). Missing data were imputed into five data sets using a Markov chain Monte Carlo method. (Schafer, 1997) Soldiers who completed follow-up assessments were older, more likely Caucasian, more likely to have some formal education beyond high school, higher military rank, and more likely to have previously deployed overseas compared to those who did not complete follow-up assessments.
2.5. Measures
Pre-and post-deployment data collection included: sociodemographics, military demographics, current tobacco use, mental health symptoms, and heart rate variability. Sociodemographic variables included age, gender, race/ethnicity, education, and marital status. Race/ethnicity was self-reported according to the following categories: American Indian or Alaskan Native; Asian/Oriental or Pacific Islander; Black/African American; White/Caucasian, not of Hispanic origin; Hispanic, or Other. Childhood abuse was defined as childhood physical or sexual abuse using the Pre-Deployment Life Events scale from the Deployment Risk and Resilience Inventory (DRRI) (Vogt, Proctor, King, King, & Vasterling, 2008). Military variables included rank (dichotomized to Staff Sergeant or E6 and below), years of active service, years of total service, number of deployments, deployment to combat zone, pre-deployment traumatic brain injury (TBI), and combat experiences during the most recent deployment. Pre-deployment TBI was assessed using the DoD Post-Deployment Health Assessment TBI screen. Combat experiences were assessed using the 15-item Combat Experiences Survey adapted for OEF/OIF veterans (Hoge et al., 2004). Resilience was measured using the 25-item Connor and Davidson Resilience scale (Connor & Davidson, 2003). PTSD symptom severity was measured using the 17-item PTSD Checklist − Military version (PCL) (Keen, Kutter, Niles, & Krinsley, 2008; Weathers, Litz, Herman, Huska, & Keane, 1993). A PCL cut-off score of 50 or greater was used in logistic models consistent with post-deployment surveillance studies (Hoge et al., 2004; Terhakopian, Sinaii, Engel, Schnurr, & Hoge, 2008). A post-hoc cut-off score of PCL > 34 consistent with clinical screening for PTSD (Bliese et al., 2008) was also used for the 3- and 12-month post-deployment logistic regression because too few soldiers reported 12-month PCL > 50.
Resting state HRV was measured for 10 min at the start of data collection using a J&J Engineering I-330-C2 Plus multichannel bioamplifier instrument with 3 M Red Dot ECG electrodes (Ag/AgCl reusable gel free sensors) just below each collarbone. Respiration rate was measured simultaneously using one respiration-monitoring belt with a magnetic strain gauge sensor placed around the upper abdomen. All participants were in a standardized seated position. The maximum sampling rate per channel was 1024 samples per second. ECG data were used to determine the inter-beat-intervals (IBI) measured in milliseconds and calculate the standard deviation of R–R intervals (SDNN), low frequency (LF, 0.04–0.15 Hz) power and high frequency (HF, 0.15–0.4 Hz) power (ms2). There are non-autonomic contributions to HRV, however, HF tends to be associated with efferent parasympathetic activity and SDNN with both sympathetic and parasympathetic activity (Task Force of the European Society of Cardiology & the North American Society of Pacing & Electrophysiology, 1996). Low frequency (LF, 0.04-0.15 Hz) power results were similar to those found for SDNN and are not reported here but are available from first author upon request. The first 9 min of resting ECG data was divided into consecutive three minute segments. HRV analysis was performed separately on each 3-min segment and averaged together. Each segment was de-trended (least squares method) and a Hanning window applied prior to power spectral density calculation. HF power was natural log transformed before analysis because of the wide range and highly skewed distribution of raw HF values. All aberrant data were removed by a trained human technician prior to analysis. Usable pre-deployment HRV data was defined as less than 10% ectopic or aberrant beats (due to participant movement or equipment malfunction) and usable HRV data were available for 91.3% (313/343) of the sample. Heart rate was measured in beats per minute for an additional analysis using heart rate as the predictor of interest.
2.6. Statistical analysis
Statistical analyses were conducted using SAS 9.3. Sociodemo-graphic and clinical comparisons between soldiers who completed the 3- and 12-month post-deployment assessments and those who did not, were conducted using chi-square test for categorical data and t-tests for continuous data. Dependent variables were PTSD symptom severity based on PCL and independent variables of interest were HRV. Multiple imputations (Rubin, 1976) were performed for the sample using SAS MI procedure because 17.5% (60/343) of soldiers were missing a combination of pre-deployment combat zone exposure, TBI, childhood abuse, most recent deployment combat exposure, and baseline HRV data. Five imputed data sets were generated to account for the uncertain nature of missingness. Analyses were repeated for each of five imputed datasets and then combined using the SAS MIANALYZE procedure.
Due to the repeated measures for each participant, generalized linear mixed (SAS GLIMMIX) models were fit with a random intercept to account for within participant correlation. Continuous PCL scores were not normally distributed. Typically a gamma distribution with log link would be specified for the model; however, these results were similar to those using normal distribution and identity link. Therefore, normal distribution and identity link results are reported here for ease of interpretation. Standardized coefficients were also included as a proxy for effect size in Table 3. A GLM logit model was used to examine the effect of pre-deployment HRV on post-deployment dichotomous measures of PTSD symptom severity (PCL > 34 and PCL > 50).
Table 3.
Pre-deployment High Frequency Domain (HF) Heart Rate Variability Generalized Linear Mixed Model Predicting Post-deployment PCL.
| Variable | Estimate (SE) | Standardized Estimate (SE) | p-value |
|---|---|---|---|
| Age | 0.01 (0.08) | 1.36 (15.07) | 0.928 |
| Race (1 = Caucasian, 0 = non-Caucasian) | −3.33 (1.12) | −35.27 (11.86) | 0.003 |
| Marital (1 = Married/Cohabitating, 0 = Other) | −0.61 (1.14) | −7.15 (13.25) | 0.590 |
| Tobacco use (1 = Yes) | 0.64 (1.04) | 7.46 (12.09) | 0.538 |
| Childhood abuse (1 = Yes) | 2.34 (1.36) | 20.21 (11.75) | 0.087 |
| Previous combat zone exposure (1 = Yes) | −0.05 (1.18) | −0.63 (13.58) | 0.963 |
| Pre-deployment Traumatic Brain Injury (1 = Yes) | 8.39 (2.70) | 35.51 (11.29) | 0.002 |
| Time (3-month PCL versus 12-month) | 2.31 (0.57) | 26.63 (6.56) | <0.0001 |
| Pre-deployment Respiration Rate | 0.06 (0.14) | 5.44 (12.75) | 0.670 |
| Pre-deployment PCL | 1.28 (0.22) | 234.47 (39.65) | <0.0001 |
| Pre-deployment ln(HF) | 3.16 (1.16) | 92.60 (34.30) | 0.008 |
| Pre-deployment PCL* Pre-deployment ln(HF) | −0.17 (0.04) | −189.29 (49.88) | 0.0002 |
A purposeful selection method was used to identify candidate pre-deployment covariates based on a literature review and were included in the multivariate analysis based on bivariate association with post-deployment PTSD symptom severity (p < 0.2) (Hosmer & Lemeshow, 2000). In addition, although the pre-deployment correlations between PCL and HRV variables were not significant in our study (p-values > 0.8), others have reported significant cross-sectional correlations (e.g., Marine Resilience Study). Therefore, we tested for this interaction term and found it was significant indicating that PCL moderated the effect of HRV on future PCL outcomes. The primary aim of this study was to evaluate pre-deployment predictors of post-deployment PTSD symptom severity. Deployment related predictors were added post-hoc to the pre-deployment model.
3. Results
3.1. Descriptive and bivariate correlations with PCL
Soldiers in this study cohort were generally young, Caucasian enlisted males, who had low levels of pre-deployment PTSD symptoms (Table 1). If they had deployed previously, nearly all had deployed to an Internal Revenue Service recognized combat zone. The following variables met criteria (bivariate correlation with 3-month post-deployment PTSD symptom severity p < 0.20) to be included as covariates in the models: age, race, tobacco use, history of childhood abuse, previous deployment to a combat zone, number of previous deployments, pre-deployment TBI, and pre-deployment PCL (Table 2). Previous deployment to a combat zone and number of previous deployments both met criterion to be included as covariates. Previous deployment to a combat zone was included in the main analysis because it had the strongest correlation with 3-month post-deployment PCL and the multivariate results reported below were unchanged when number of previous deployments was used instead. Fewer covariates met inclusion criterion for the logistic regression model but for ease of presentation we used the same covariates for the linear and logistic models.
Table 1.
Pre-deployment Socio-demographic and Clinical Variables (N = 343)a.
| Variable | Mean (SD) or N (%)b |
|---|---|
| Age (SD) | 28.67 (8.41) |
| Male (%) | 315 (91.84) |
| Caucasian (%) | 241 (70.26) |
| Married or Cohabitating (%) | 160 (46.65) |
| Education beyond High School (%) | 268 (78.13) |
| Tobacco Use (%) | 160 (46.65) |
| Childhood Abuse (%) | 52 (15.16) |
| Rank E6 or below (%) | 293 (85.42) |
| Years in Military (SD) | 7.87 (7.94) |
| Previous Overseas Deployment (%) | 155 (45.19) |
| Number of Previous Deployments (SD) | 0.78 (1.18) |
| Previous Combat Zone Deployment (%) | 148 (43.15) |
| Number of Most Recent Combat Experiences (SD) | 2.30 (1.85) |
| Infantry battalion (%) | 248 (72.30) |
| Conner Davidson Resilience Scale (SD) | 83.90 (10.34) |
| Pre-deployment TBI (%) | 14 (4.08) |
| Pre-deployment PCL(SD) | 23.27 (8.47) |
| Pre-deployment PCL ≥ 34 (%) | 37 (10.79) |
| Pre-deployment PCL ≥50 (%) | 5 (1.46) |
| Pre-deployment Respiration Ratec | 15.01 (3.89) |
| Pre-deployment ln(HF) (SD) | 4.64 (1.23) |
| Pre-deployment SDNN (SD) | 47.25 (21.29) |
Abbreviations: TBl = traumatic brain injury, PHQ–9 = 9-item Patient Health Questionnaire for depression, PCL-M = military version of Post-traumatic Stress Disorder Checklist, SDNN = standard deviation of normal beat to beat or R–R interval, ln(HF) = natural log of high frequency heart rate variability band.
Results displayed as mean with (SD) and N with (%). 343 subject completed either the 3-month or 12-month follow-up.
Respiratory rate in breaths per minute.
Table 2.
Correlation Matrix of Pre-Deployment Variables with 3-month Post-Deployment PCL (n = 307).
| Variable | Correlation Coefficient | p-value |
|---|---|---|
| Age | 0.103 | 0.070 |
| Male | 0.032 | 0.574 |
| Caucasian | −0.106 | 0.062 |
| Married or Cohabitating | 0.067 | 0.238 |
| Education beyond High School | −0.038 | 0.512 |
| Tobacco Use | 0.101 | 0.078 |
| Childhood Abuse | 0.190 | 0.0008 |
| Rank E6 or below | 0.025 | 0.666 |
| Conner Davidson Resilience Scale | 0.004 | 0.943 |
| Number of Previous Deployments | 0.165 | 0.004 |
| Previous Combat Zone Deployment | 0.175 | 0.002 |
| Pre-deployment TBl | 0.211 | 0.0002 |
| Pre-deployment PCL-M | 0.465 | <0.0001 |
| Pre-deployment Respiration Rate | 0.041 | 0.489 |
| Pre-deployment SDNN | −0.129 | 0.026 |
| Pre-deployment ln(HF) | −0.148 | 0.015 |
3.2. Multivariate HF model predicting continuous PCL
Table 3 presents the generalized linear mixed model where HF is the predictor of interest. The pre-deployment PCL*ln(HF) interaction term was significant (p < 0.0001). Significant covariates included race and pre-deployment TBI. A similar pattern was noted when using SDNN as the predictor of interest except that the pre-deployment PCL*SDNN interaction term was not significant (p = 0.069). The main effect of SDNN in the model without the pre-deployment PCL*SDNN interaction term was also not significant (p = 0.091).
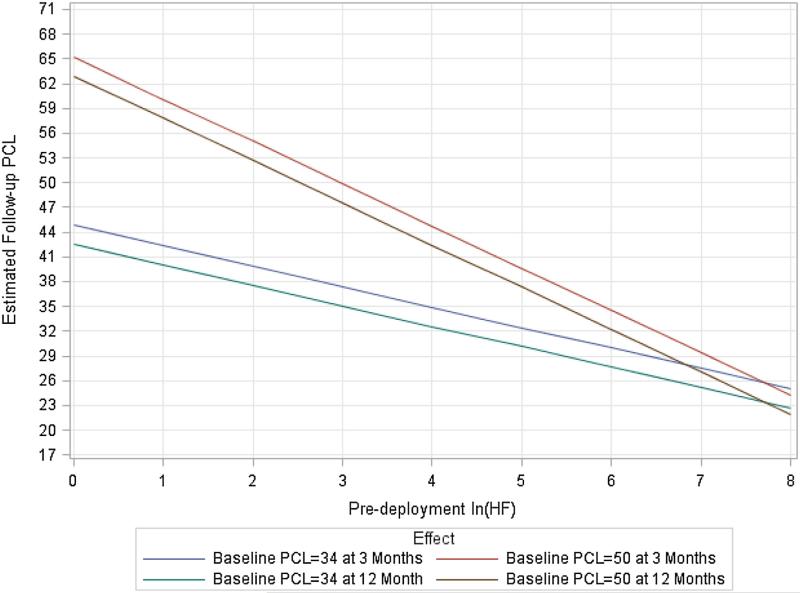
The Figure provides a visualization of the pre-deployment PCL*ln(HF) interaction effect, at 3- and 12-month post-deployment by pre-deployment HF for soldiers with pre-deployment PCL scores of 34 and 50. The Figure demonstrates the moderating effect of pre-deployment PCL on HF in predicting both 3- and 12-month post-deployment PCL scores. In this sample, the effect of HF became significant (p < 0.05) when pre-deployment PCL was 24 and higher when predicting follow-up PCL (Fig. 1).
Fig. 1.
Predicted 3- and 12-month Post-deployment PTSD Severity by Pre-deployment PTSD Severity and High Frequency (HF) Power HRV.1
1Rationale for pre-deployment PCL levels: 50 = common cutoff for positive PTSD screen in surveillance studies(Hoge et al., 2004; Terhakopian et al., 2008) and 34 = recommended cutoff for clinical screening for PTSD. (Bliese et al., 2008)
When the following deployment-related predictors of PTSD were added post-hoc to the generalized linear mixed model presented in Table 3, the pre-deployment PCL*ln(HF) interaction term remained significant (p < 0.0001). The deployment-related predictors and their p-values were TBI that occurred during the current deployment (p = 0.002), the number of combat exposures experienced during current recent deployment (< 0.0001), resilience training arm (p = 0.280), and number of days to completing follow-up (.055). The mean number of days from returning home to completing the 3- and 12-month follow-up (101.1, SD = 55.0 and 434.9 SD = 48.1, respectively) was not correlated with 3- or 12-month post-deployment PCL (p = 0.87 and p = 0.08 respectively). The HRV results were also not changed when the four soldiers who completed 3-month and one soldier who completed the 12-month post-deployment follow-up and reported pre-deployment PCL > 50 were excluded from the analyses. Further, using Table 3 model, pre-deployment PCL*heart rate (replacing HRV) interaction term was not significant and pre-deployment heart rate alone was not a significant predictor of post-deployment PTSD (p = 0.434).
3.3. Multivariate HF model predicting dichotomous PCL
The proportion of soldiers with pre-deployment PCL > 50 and PCL > 34 was 1.46% (5/343) and 10.79% (37/343) at baseline, 5.21% (16/307) and 22.15% (68/307) at 3-month post-deployment, and 2.55% (6/235) and 16.17% (38/235) at 12-months post-deployment, respectively. Similarly, in the HF logit model, the pre-deployment PCL*ln(HF) interaction term was significant when predicting PCL > 34 and PCL > 50 (β = −0.04, p = 0.014 and β = −0.05, p = 0.018, respectively) (Table 4). Significant covariates included race in models predicting PCL > 34 and PCL > 50. In the SDNN logit models, the pre-deployment PCL*pre-deployment SDNN interaction term was not significant in either model (p = 0.478 and p = 0.115, respectively). After removing the interaction term the main effect of pre-deployment SDNN was also not significant (p = 0.207 and p = 0.096, respectively).
Table 4.
Pre-deployment High Frequency Domain (HF) Heart Rate Variability Generalized Linear Mixed Model Binary Distribution/Logit Link.
| Variable | PCL ≥ 34 |
PCL ≥ 50 |
||
|---|---|---|---|---|
| Estimate (SE) | p-value | Estimate (SE) | p-value | |
| Age | −0.004 (0.02) | 0.857 | −0.04 (0.05) | 0.434 |
| Race (1 = Caucasian, 0 = non-Caucasian) | −0.81 (0.32) | 0.011 | −1.11 (0.66) | 0.093 |
| Marital (1 = Married/Cohabitating, 0 = Other) | −0.31 (0.33) | 0.356 | −0.12 (0.66) | 0.861 |
| Tobacco use (1 = Yes) | 0.24 (0.30) | 0.439 | 0.17 (0.64) | 0.785 |
| Childhood abuse (1 = Yes) | 0.53 (0.36) | 0.145 | 1.30 (0.70) | 0.063 |
| Previous combat zone exposure (1 = Yes) | −0.13 (0.35) | 0.718 | −0.63 (0.78) | 0.420 |
| Pre-deployment Traumatic Brain Injury (1 = Yes) | 1.72 (0.71) | 0.016 | 1.51 (0.99) | 0.131 |
| Time (3-month PCL versus 12-month) | 0.35 (0.26) | 0.177 | 0.88 (0.63) | 0.163 |
| Pre-deployment Respiration Rate | −0.002 (0.04) | 0.965 | −0.14 (0.10) | 0.171 |
| Pre-deployment PCL | 0.26 (0.08) | 0.001 | 0.41 (0.13) | 0.002 |
| Pre-deployment ln(HF) | 0.66 (0.41) | 0.110 | 1.64 (0.80) | 0.041 |
| Pre-deployment PCL* Pre-deployment ln(HF) | −0.04 (0.02) | 0.020 | −0.07 (0.03) | 0.008 |
4. Discussion and conclusions
Pre-deployment HF was a significant predictor of continuous and dichotomous PTSD symptom severity but only for those soldiers with higher pre-deployment PCL scores. This study demonstrated a significant inverse relationship between pre-deployment HRV and post-deployment PTSD symptom severity for soldiers with a pre-deployment PCL score of 24 or more. These results were found when controlling for pre-military violence exposure, previous deployment, pre-deployment TBI, and pre-deployment PCL which are often considered the strongest predictors of post-deployment PTSD in military service members (Phillips et al., 2010; Smith et al., 2008). In addition, the results were unchanged when controlling for deployment-related variables which were not available during pre-deployment assessment (current deployment TBI, current deployment combat experiences, and number of days to follow-up completion). In addition, pre-deployment heart rate was not a significant predictor of post-deployment PTSD symptoms. Therefore, there is value added to measuring HRV compared to heart rate alone.
According to the standardized coefficients presented in Table 3, the strongest predictor was pre-deployment PCL followed by the pre-deployment PCL*pre-deployment HRV interaction term and pre-deployment HF. Pre-deployment PCL scores could possibly be modified with medications or psychotherapy (11% reported pre-deployment PCL > 34 and 1.5% reported pre-deployment PCL > 50). Based on the main effect of pre-deployment HRV and the pre-deployment PCL*pre-deployment HRV interaction term results, pre-deployment HRV had a significant effect on post-deployment PCL for soldiers reporting pre-deployment PCL > 24. Other statistically significant predictors were race and history of pre-deployment TBI and these could be used as additional risk factors. However, PCL and HRV are the only significant pre-deployment predictors that are modifiable.
Of all the HRV measures, HF is more specifically associated with parasympathetic (vagal) activity. (Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology, 1996) Reduced vagally mediated HRV has also been linked to reduced self-regulatory capacity and cognitive functions that involve the executive centers of the prefrontal cortex (Geisler, Kubiak, Siewert, & Weber, 2013; McCraty and Zayas, 2014; Thayer et al., 2009). This findings reported here from the WAR study suggest that those soldiers with higher pre-deployment PCL scores plus evidence of poor autonomic regulation may be at increased risk for post-deployment PTSD symptoms.
A recent meta-analysis demonstrated that anxiety disorders, including PTSD, were associated with lower HRV independent of medication use, physical health or mental health comorbidity (Chalmers, Quintana, Abbott, & Kemp, 2014). The Central Autonomic Network (Thayer et al., 2009) and Polyvagal Theory (Porges, 2007) describe anxiety symptoms being due to a deficit in the inhibitory activity of the parasympathetic nervous system. There is also evidence that HRV is associated with attentional and affect regulation, behavioral flexibility, cerebral blood flow (Thayer et al., 2009); inflammatory response (Cooper et al., 2015); cardiovascular disease (Tsuji et al., 1996); genetic markers (Newton-Cheh et al., 2007); and self-reported health status (Jarczok et al., 2015).
In the MRS study, the only significant HRV variable was the LF/HF ratio which predicted post-deployment PTSD diagnosis not PTSD symptom severity (Minassian et al., 2015). Pre-deployment HF was not a significant predictor of PTSD diagnosis or PTSD symptom severity in the MRS. In comparison, pre-deployment HF was a significant predictor of post-deployment PTSD for soldiers with higher pre-deployment PCL scores in the WAR study. As mentioned above there are many differences between the MRS and the WAR study in terms of sample, covariates, outcome measure, and follow-up duration. However, both studies found a modest association between pre-deployment HRV and post-deployment PTSD.
These results do not suggest a clear pre-deployment HRV cut-point for predicting vulnerability to post-deployment PTSD. Low HRV is most likely one of many possible risk factors for post-deployment PTSD, including genetic influences, neural pathways, and environmental factors. Even so, HRV is modifiable and the availability of personal training devices and smartphone apps that include HRV measurement is increasing rapidly.
The goal of predicting resilience to combat stress prior to deployment to a war zone has been pursued for many years (Shephard, 2003). Service members currently receive resilience training to improve stress tolerance in all branches of military service, e.g., Comprehensive Soldier and Family Fitness (CSF2) in the Army, Marine Total Fitness in the Marine Corps, Navy Operational Stress Control, and Resilience Mobile Training Teams in the Air Force. The VA/DoD Clinical Practice Guideline for Management of PTSD also lists breath training (known to increase HRV) as a strongly recommended component of PTSD psychotherapy.
Limitations to this study include controversies associated with interpretation of all measures of HRV, e.g., the association between HF and total vagal tone may not be as strong as suspected (Grossman & Kollai, 1993). Pre-deployment data was collected during a time of stressful pre-deployment training and it is not known how these results would differ if the pre-deployment data were collected during a time of less stressful training. In general, there was a low level of PTSD symptom severity and low number of soldiers with post-deployment PCL scores of 50 or more. It is not known if the HRV results would be the same for military units with higher levels of post-deployment PTSD symptoms. The relationship between pre-deployment HRV and post-deployment PCL was analyzed within the context of an HRV-based resilience training intervention. However, as reported above, controlling for study arm did not change the pre-deployment HRV prediction results. There are other predictors of combat stress vulnerability that were not included in this study, including unit cohesion and morale, trust and confidence in leadership, and training quality. The follow-up rate was relatively low, 74.7% (307/411) at 3-months and 57.2% (235/411) at 12-months, however these rates compare favorably with the 62.0% 4–6 month MRS follow-up rate (Minassian et al., 2015). There were also significant differences in the sociodemo-graphic and military experience variables between those soldiers who completed post-deployment follow-up assessments and those who did not. However, the variables that distinguished follow-up completers from non-completers appeared to be associated with age and rank and may reflect the difficulty of younger, lower ranking soldiers getting the time to complete the follow-up interviews during drill weekend. Further, there were no differences between follow-up completers and non-completers in pre-deployment PTSD or any measure of HRV. Another possible limitation is using the PCL as the outcome measure, which soldiers recognize as a PTSD screening questionnaire, and as such they may not provide honest responses (Sundin et al., 2014; Warner et al., 2011). However, controlling for secondary gain using self-report measures of over-reporting is not straight-forward (Constans et al., 2014; Brady et al., 2015).
In conclusion, pre-deployment HF in the context of higher pre-deployment PTSD symptom severity (PCL > 24) appears to be a significant physiological predictor of post-deployment PTSD symptom severity. HRV measurement has the practical advantages of being simple to measure and it can be improved with appropriate training.
Acknowledgments
Funding/Support
This work was supported by grants from the Military Operational Medical Research Program (PT074626), South Central Mental Illness and Research Educational and Clinical Center (MIRECC), and National Institutes of Health (P20 GM103425-09, UL1TR000039, KL2TR000063).
Role of Funders/Supporters
The respective funding agencies played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Author contributions
All authors above meet the following criteria for authorship:
(1) substantial contributions to conception or design of the work, or the acquisition, analysis, or interpretation of data for the work; and (2) drafting of the work or revising it critically for important intellectual content; and (3) final approval of the version to be published; and (4) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of interest
Potential conflicts of interest exist for the following co-authors: Mark and Brenda Wiederhold are the President and Executive Director of Virtual Reality Medical Centers which provide virtual reality exposure therapy with physiological monitoring. Don Chartrand is CEO of Ease Interactive Inc. which produces the Stress Resilience Training System that uses heart rate variability biofeedback. Rollin McCraty is the Director of Research for the Institute of Heart Math which produces and sells a heart rate variability device. There are no conflicts of interest for the first author or other co-authors.
References
- Agelink MW, Boz C, Ullrich H, Andrich J. Relationship between major depression and heart rate variability: Clinical consequences and implications for antidepressive treatment. Psychiatry Research. 2002;113:139–149. doi: 10.1016/s0165-1781(02)00225-1. [DOI] [PubMed] [Google Scholar]
- Beevers CG, Lee HJ, Wells TT, Ellis AJ, Telch MJ. Association of predeployment gaze bias for emotion stimuli with later symptoms of PTSD and depression in soldiers deployed in Iraq. American Journal of Psychiatry. 2011;168:735–741. doi: 10.1176/appi.ajp.2011.10091309. [DOI] [PubMed] [Google Scholar]
- Billman GE. The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Frontiers in Physiology. 2013;4:26. doi: 10.3389/fphys.2013.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Kolb LC, Prins A. Psychophysiological responses in the diagnosis of posttraumatic stress disorder in Vietnam veterans. Journal of Nervous & Mental Disease. 1991;179(2):97–101. doi: 10.1097/00005053-199102000-00006. [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology. 2008;76:272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- Brady RE, Constans JI, Marx BP, Spira JL, Gevirtz R, Kimbrell TA, et al. Effect of symptom over-Reporting on heart rate variability in veterans with posttraumatic stress disorder. Journal of Trauma and Dissociation. 2015;16(5):551–562. doi: 10.1080/15299732.2015.1021505. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: A meta-analysis. Frontiers in Psychiatry. 2014;5:80. doi: 10.3389/fpsyt.2014.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen H, Benjamin J. Power spectrum analysis and cardiovascular morbidity in anxiety disorders. Autonomic Neuroscience. 2006;128:1–8. doi: 10.1016/j.autneu.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Constans JI, Kimbrell TA, Nanney JT, Marx BP, Jegley S, Pyne JM. Over-reporting bias and the modified Stroop effect in Operation Enduring and Iraqi Freedom veterans with and without PTSD. Journal of Abnormal Psychology. 2014;123:81–90. doi: 10.1037/a0035100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper TM, McKinley PS, Seeman TE, Choo TH, Lee S, Sloan RP. Heart rate variability predicts levels of inflammatory markers: Evidence for the vagal anti-inflammatory pathway. Brain, Behavior, and Immunity. 2015;49:94–100. doi: 10.1016/j.bbi.2014.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckberg DL. Sympathovagal balance: A critical appraisal. Circulation. 1997;96(9):3224–3232. doi: 10.1161/01.cir.96.9.3224. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Mayou RA, Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology. 1998;107:508–519. doi: 10.1037//0021-843x.107.3.508. [DOI] [PubMed] [Google Scholar]
- Forneris CA, Butterfield MI, Bosworth HB. Physiological arousal among women veterans with and without posttraumatic stress disorder. Military Medicine. 2004;169(4):307–312. doi: 10.7205/milmed.169.4.307. [DOI] [PubMed] [Google Scholar]
- Geisler FC, Kubiak T, Siewert K, Weber H. Cardiac vagal tone is associated with social engagement and self-regulation. Biological Psychology. 2013;93(2):279–286. doi: 10.1016/j.biopsycho.2013.02.013. [DOI] [PubMed] [Google Scholar]
- Ginsberg JP, Berry ME, Powell DA. Cardiac coherence and posttraumatic stress disorder in combat veterans. Alternative Therapies in Health and Medicine. 2010;16:52–60. [PubMed] [Google Scholar]
- Grossman P, Kollai M. Respiratory sinus arrhythmia, cardiac vagal tone, and respiration: Within- and between-individual relations. Psychophysiology. 1993;30:486–495. doi: 10.1111/j.1469-8986.1993.tb02072.x. [DOI] [PubMed] [Google Scholar]
- Guthrie RM, Bryant RA. Auditory startle response in firefighters before and after trauma exposure. American Journal of Psychiatry. 2005;162:283–290. doi: 10.1176/appi.ajp.162.2.283. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge EA, Austin ED, Pollack MH. Resilience: Research evidence and conceptual considerations for posttraumatic stress disorder. Depression and Anxiety. 2007;24:139–152. doi: 10.1002/da.20175. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression analysis. 2nd ed. John Wiley & Sons; New York, NY: 2000. [Google Scholar]
- Jarczok MN, Kleber ME, Koenig J, Loerbroks A, Herr RM, Hoffmann K, et al. Investigating the associations of self-rated health: Heart rate variability is more strongly associated than inflammatory and other frequently used biomarkers in a cross sectional occupational sample. PUBLIC LIBRARY OF SCIENCE. 2015;10(2):e0117196. doi: 10.1371/journal.pone.0117196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kardiner A. The traumatic neuroses of war. National Research Council; Washington, D.C: 1941. [Google Scholar]
- Keane TM, Kolb LC, Kaloupek DG, Orr SP, Blanchard EB, Thomas RG, et al. Utility of psychophysiological measurement in the diagnosis of posttraumatic stress disorder: Results from a Department of Veterans Affairs Cooperative Study. Journal of Consulting and Clinical Psychology. 1998;66(6):914–923. doi: 10.1037//0022-006x.66.6.914. [DOI] [PubMed] [Google Scholar]
- Keen SM, Kutter CJ, Niles BL, Krinsley KE. Psychometric properties of PTSD Checklist in sample of male veterans. Journal of Rehabilitation Research and Development. 2008;45:465–474. doi: 10.1682/jrrd.2007.09.0138. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Keane TM, Fairbank JA, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, postwar social support, and additional stressful life events. Journal of Personality & Social Psychology. 1998;74(2):420–434. doi: 10.1037//0022-3514.74.2.420. [DOI] [PubMed] [Google Scholar]
- Koffel E, Polusny MA, Arbisi PA, Erbes CR. Pre-deployment daytime and nighttime sleep complaints as predictors of post-deployment PTSD and depression in National Guard troops. Journal of Anxiety Disorders. 2013;27:512–519. doi: 10.1016/j.janxdis.2013.07.003. [DOI] [PubMed] [Google Scholar]
- Kok BC, Herrell RK, Thomas JL, Hoge CW. Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan Reconciling Prevalence differences between studies. Journal of Nervous & Mental Disease. 2012;200(5):444–450. doi: 10.1097/NMD.0b013e3182532312. [DOI] [PubMed] [Google Scholar]
- Marmar CR, McCaslin SE, Metzler TJ, Best S, Weiss DS, Fagan J, et al. Predictors of posttraumatic stress in police and other first responders. Annals of New York Academy of Sciences. 2006;1071:1–18. doi: 10.1196/annals.1364.001. [DOI] [PubMed] [Google Scholar]
- McCraty R, Zayas MA. Cardiac coherence, self-regulation, autonomic stability, and psychosocial well-being. Frontiers in Psychology. 2014;5:1090. doi: 10.3389/fpsyg.2014.01090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meakins JC, Wilson RM. The effect of certain sensory stimulations on respiratory and heart rate in cases of so-called irritable heart. Heart: A Journal for the Study of the Circulation. 1918;7:17–22. [Google Scholar]
- Minassian A, Maihofer AX, Baker DG, Nievergelt CM, Geyer MA, Risbrough VB. Association of predeployment heart rate variability with risk of postdeployment posttraumatic stress disorder in active-duty marines. JAMA Psychiatry. 2015;72(10):979–986. doi: 10.1001/jamapsychiatry.2015.0922. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health [08.17.16];NIMH research domain criteria (RDoC) 2011 doi: 10.1037/abn0000768. [Available at: http://www.nimh.nih.gov/research-priorities/rdoc/nimh-research-domain-criteria-rdoc.shtml] [DOI] [PubMed]
- Newton-Cheh C, Guo CY, Wang TJ, O'Donnell CJ, Levy D, Larson MG. Genome-wide association study of electrocardiographic and heart rate variability traits: The Framingham Heart Study. BMC Medical Genetics. 2007;8(1):S7. doi: 10.1186/1471-2350-8-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr SP, Lasko NB, Macklin ML, Pineles SL, Chang Y, Pitman RK. Predicting post-trauma stress symptoms from pre-trauma psychophysiologic reactivity, personality traits and measures of psychopathology. Biology of Mood and Anxiety Disorder. 2012;2:8. doi: 10.1186/2045-5380-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychology Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Phillips CJ, Leardmann CA, Gumbs GR, Smith B. Risk factors for posttraumatic stress disorder among deployed US male Marines. BMC Psychiatry. 2010;10:52. doi: 10.1186/1471-244X-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Forgue DF, de Jong JB, Claiborn JM. Psychophysiologic assessment of posttraumatic stress disorder imagery in Vietnam combat veterans. Archives of General Psychiatry. 1987;44(11):970–975. doi: 10.1001/archpsyc.1987.01800230050009. [DOI] [PubMed] [Google Scholar]
- Pole N, Neylan TC, Otte C, Henn-Hasse C, Metzler TJ, Marmar CR. Prospective prediction of posttraumatic stress disorder symptoms using fear potentiated auditory startle responses. Biological Psychiatry. 2009;65:235–240. doi: 10.1016/j.biopsych.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porges SW. The polyvagal perspective. Biological Psychology. 2007;74:116–143. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- Rusiecki JA, Chen L, Srikantan V, Zhang L, Yan L, Polin ML, et al. DNA methylation in repetitive elements and post-traumatic stress disorder: A case-control study of US military service members. Epigenomics. 2012;4:29–40. doi: 10.2217/epi.11.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandweiss DA, Slymen DJ, Leardmann CA, Smith B, White MR, Boyko EJ, et al. Preinjury psychiatric status, injury severity, and postdeployment posttraumatic stress disorder. Archives of General Psychiatry. 2011;68:496–504. doi: 10.1001/archgenpsychiatry.2011.44. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. Chapman & Hall; London: 1997. [Google Scholar]
- Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: A prospective study. American Journal of Psychiatry. 1996;153:219–225. doi: 10.1176/ajp.153.2.219. [DOI] [PubMed] [Google Scholar]
- Shephard B. A war of nerves: Soldiers and psychiatrists in the twentieth century. Harvard University Press; 2003. [Google Scholar]
- Smith TC, Ryan MA, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D, et al. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: Prospective population based US military cohort study. British Medical Journal. 2008;336:366–371. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundin J, Herrell RK, Hoge CW, Fear NT, Adler AB, Greenberg N, et al. Mental health outcomes in US and UK military personnel returning from Iraq. The British Journal of Psychiatry. 2014;204(3):200–207. doi: 10.1192/bjp.bp.113.129569. [DOI] [PubMed] [Google Scholar]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. European Heart Journal. 1996;17:354–381. [PubMed] [Google Scholar]
- Terhakopian A, Sinaii N, Engel CC, Schnurr PP, Hoge CW. Estimating population prevalence of posttraumatic stress disorder: An example using the PTSD checklist. Journal of Traumatic Stress. 2008;21:290–300. doi: 10.1002/jts.20341. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH. Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Annals of Behavioral Medicine. 2009;37:141–153. doi: 10.1007/s12160-009-9101-z. [DOI] [PubMed] [Google Scholar]
- Tsuji H, Larson MG, Venditti FJ, Jr., Manders ES, Evans JC, Feldman CL, et al. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation. 1996;94:2850–2855. doi: 10.1161/01.cir.94.11.2850. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Defense Task Force on Mental Health . An achievable vision: Report of the Department of Defense Task Force on mental health. Defense Health Board; Falls Church, VA: 2007. [Google Scholar]
- Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment to the Iraq war. Journal of the American Medical Association. 2006;296(5):519–529. doi: 10.1001/jama.296.5.519. [DOI] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15(4):391–403. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]
- Wald I, Degnan KA, Gorodetsky E, Charney DS, Fox NA, Fruchter E, et al. Attention to threats and combat-related posttraumatic stress symptoms: Prospective associations and moderation by the serotonin transporter gene. JAMA Psychiatry. 2013;70:401–408. doi: 10.1001/2013.jamapsychiatry.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner CH, Appenzeller GN, Grieger T, Belenkiy S, Breitbach J, Parker J, et al. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Archives of General Psychiatry. 2011;68(10):1065–1071. doi: 10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman JA, Huska JA, Keane TM. The PTSD checklist (PCL): reliability, validity and diagnostic utility. Paper presented at the 9th annual conference of the ISTSS. 1993 [Google Scholar]
- Wolfe J, Chrestman KR, Ouimette PC, Kaloupek D, Harley RM, Bucsela M. Trauma-related psychophysiological reactivity in women exposed to war-zone stress. Journal of Clinical Psychology. 2000;56(10):1371–1379. doi: 10.1002/1097-4679(200010)56:10<1371::AID-JCLP8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Yurgil KA, Barkauskas DA, Vasterling JJ, Nievergelt CM, Larson GE, Schork NJ, et al. Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty marines. JAMA Psychiatry. 2013;71:149–157. doi: 10.1001/jamapsychiatry.2013.3080. [DOI] [PubMed] [Google Scholar]
- van Zuiden M, Geuze E, Willemen HL, Vermetten E, Maas M, Amarouchi K, et al. Glucocorticoid receptor pathway components predict posttraumatic stress disorder symptom development: A prospective study. Biological Psychiatry. 2012;71:309–316. doi: 10.1016/j.biopsych.2011.10.026. [DOI] [PubMed] [Google Scholar]