Abstract
Introduction
Verruciform xanthoma is a wart-like benign lesion. The classic histologic appearance consists of foamy histiocytes within elongated dermal papillae and epithelial acanthosis. The lesion most commonly occurs in the oral cavity, but has been reported in extra-oral sites such as the penis, scrotum, and vulva. The clinical and histologic characteristics of verruciform genital-associated (Vegas) xanthomas of the penis, scrotum, and vulva are reviewed.
Methods
PubMed was used to search the following term: verruciform xanthoma. The relevant papers were obtained and reviewed.
Results
There have been 193 cases of genital-associated verruciform xanthomas. There were 164 in men and 29 in women. Similar to verruciform xanthomas of the oral mucosa, they presented as asymptomatic lesions, demonstrated foam cells in the dermal papillae, and were typically managed successfully with surgical excision.
Conclusion
Verruciform xanthoma is a benign lesion characterized by a wart-like growth that is most commonly seen in the oral mucosa. Verruciform xanthomas of the genital region have been coined Vegas xanthomas. Vegas xanthomas have been reported in association with a variety of diseases, as well as in healthy individuals. Biopsy is required for diagnosis, and complete surgical excision is typically curative.
Keywords: VEGAS xanthoma, Verruciform xanthoma, Verruciform xanthoma of the penis, Verruciform xanthoma of the scrotum, Verruciform xanthoma of the vulva
Introduction
Verruciform xanthoma is a benign tumor that typically occurs in the oral mucosa [1–86]. Extraoral lesions have been most commonly described on the penis (Table 1), scrotum (Table 2), and vulva (Table 3). Tumors in genital locations have recently been referred to as Vegas (Verruciform Genital-Associated) xanthomas [63]. The characteristics of verruciform xanthomas of the genitalia are reviewed. This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Table 1.
Verruciform xanthomas of the penis
| Case | AO (year) | Duration | Race | Location | Morphology | Color | Sizea | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1 | 8 | 25 years | I | R prepuce | V, dry growth | Pinkish | NA | [39] |
| 2 | 16 | NA | W | Penis | Ps forming v plaque | E Y | 10–20 mm | [8] |
| 3 | 22 | 3 months | NA | Prepuce | Ind plaque | R-orange | 2.5 × 1.75 cm | [11] |
| 4 | 23 | 5 years | NA | Glans penis | Firm, v, ib | Pink | 1.5 cm | [15] |
| 5b | 25 | NA | NA | NA | NA | NA | NA | [37] |
| 6 | 28 | 2 weeks | B | Left penile shaft | Pn, ker | Y-brown | 15 × 5 mm | [5] |
| 7 | 29 | NA | W | Coronal sulcus | v | NA | 2.4 × 1.7 × 0.7 cm | [10] |
| 8 | 38 | 2.5 months | W | Penile shaft perineum | Pn, p | E | 8 × 5 mm | [3] |
| 9 | 39 | 6 months | W | Glans penis | V, caul, soft | E with Y | 1.5 × 1.5 × 0.6 cm | [40] |
| 10 | 40 | 12 years | C | L glans penis | Caul, v, ker | Y-brown | 4 × 3.2 cm | [17] |
| 11 | 41 | NA | W | Glans penis | NA | NA | 2 cm | [13] |
| 57 | Whole penile shaft | Caul, foc ulc | Y | 7 × 3 cm | ||||
| 12 | 43 | 1 year | NA | Ventral shaft | Wl p | Pale brown | 0.8 cm | [45] |
| 13 | 45 | NA | I | Inner prepuce | Flat, wl, p | NA | NA | [2] |
| 14 | 52 | 1 year | W | Glans penis | NI, V plaque | W | 1.5 × 0.5 cm | [6] |
| 15 | 57 | 1.5 years | W | Glans penis | Irreg surf, not wl | R | 10 mm | [16] |
| 16 | 56 | 5 years | NA | NA | V, p | NA | 0.3 cm | [18] |
| 17 | 61 | NA | J | Inner prepuce | Ind, v plaque | Y-red | NA | [20] |
| 67 | Coronal sulcus and glans penis | Ind, eroded tumorc | ||||||
| 18 | 62 | 2 years | W | Sulcus | P, well-def, wl | E-brownish | 1.5 × 2 cm | [14] |
| 19 | 64 | 2 years | Prepuce | V lesion | NA | NA | [45] | |
| 20 | 64 | NA | W | Near coronal sulcus | NI, V plaque | R | 1.5 × 2 cm | [7] |
| 21 | 71 | NA | W | Foreskin | Firm, swollen | NA | NA | [9] |
| 22 | 72 | 2 years | W | Glans penis | G & V | R to Y | NA | [1] |
| 23 | 73 | NA | W | Inferior foreskin | P | Pink to brown | 6 × 5 × 2 mm | [4] |
| 24 | 77 | NA | NA | Glans penis | Sessile, wl | NA | 1 × 0.5 cm | [38] |
| 25 | 77 | 10 months | W | Glans penis | V nodule | Y | 15 × 12 mm | [12] |
| 26 | 85 | 7 months | W | Distal foreskin | V plaque | Skin color | 1 × 1.5 cm | [19] |
| 27 | NA | NA | I | Coronal sulcus | Flat, wl, p | NA | NA | [2] |
| 28 | NA | NA | NA | Glans penis | NA | NA | NA | [72] |
| 29d | NA | NA | NA | NA | NA | NA | NA | [77] |
AO age of onset, B black, C Chinese, caul cauliflower-like, def defined, E erythematous, F filiform, foc ulc focally ulcerated, ib irregular boundaries, irreg irregular, I Indian, ind indurated, G & V globules and small-dotted vessels, ker keratotic, m months, NA not available, NI non-indurated, p(s) papule(s), pn pedunculated, R red, Ref reference, sev several, surf surface, v verrucous, w white, wks weeks, wl wart-like, Y yellow, y year
aSize is reported as given in the case reports. This is measured either in diameter, length × width, or length × width × height
bKukreja et al. discuss a case of a 25-year-old male who was circumcised for a penile lesion. The clinical features were unavailable. The lesion was initially misdiagnosed as a squamous cell carcinoma, but due to the histological features of the lesion, their department determined it was actually a verruciform xanthoma [37]
cThe patient’s original lesion was treated with circumcision; however, its removal from the coronary sulcus was suspected to be incomplete because of severe adhesion present between the prepuce and the glans penis. A yellowish-red papule was noted at the coronary sulcus 4 months following surgery. The patient decided not to have surgery because the lesion was reported to be benign. Six years later, the patient reported with an eroded tumor covering the entire coronary sulcus and much of the glans penis. This lesion was found to be a squamous cell carcinoma. The patient received a partial penectomy
dPellice et al. reported a verruciform xanthoma of the penis. No other information was obtained [77]
Table 2.
Verruciform xanthomas of the scrotum
| Case | AO (year) | Duration | Race | Location | Morphology | Color | Sizea | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1 | 19 | 20 years | NA | L | Lob, ML | Pinkish | 32 mm | [24] |
| 2 | 19 | NA | NA | NA | NA | NA | 15 × 11 mm | [36] |
| 3 | 35 | NA | N | NA | Cyst, crateriform | NA | 0.8 cm | [18] |
| 4 | 40 | W | R | Ped, v | NA | 9 × 5 mm | [28] | |
| 5 | 40 | 7 years | NA | NA | Ped, flat, g surf, caul | Pink | 1 cm | [41] |
| 6 | 40 | 20 years | NA | NA | 3 nod, pebbly surf | Y–R | 7, 9, and 12 mm | [33] |
| 7 | 44 | 3 years | NA | NA | Ped, spherical, g surf, caul | Pink | 3 cm | [41] |
| 8 | 49 | 2–3 years | J | L | Elastic soft, ped, g surfb | R w Y | 10 mm | [34] |
| 9 | 50 | Few months | B | L | V, fil p | Pink | 4 × 2 mm | [27] |
| 10 | 50 | 2 years | B | NA | Sessile plaque | NA | 1.2 cm | [32] |
| 11 | 53 | >1 year | NA | NA | Wl, polypoid | NA | 0.5 cm | [18] |
| 12 | 59 | 4 years | NA | NA | Mult p | Pink | 1–1.5 cm | [22] |
| 13 | 59 | 3 years | NA | NA | Polyp v nod, pebbly surf | Y–R | 6 mm | [33] |
| 14 | 59 | 3 week | NA | L | Fil p | R | 5 × 4 × 4 mm | [63] |
| 15 | 63 | 4 years | J | R | Ped, v, occ bleeding | R-pink | 2.5 × 2.5 cm | [30] |
| 16 | 63 | NA | NA | NA | V nodc | Whitish | 4 mm | [31] |
| 17 | 64 | 3.5 years | NA | NA | polypoid | NA | 1.8 cm | [18] |
| 18 | 66 | 1 year | J | NA | 2 ker pap | Y | 4 mm | [25] |
| 19 | 68 | 2 years | NA | R | ML nods | E | 20 mm | [21] |
| 20 | 68 | 12 years | J | R | Ped, v tumor | Pink | 10 mm | [42] |
| 21 | 70 | 3 years | NA | L | SL ped nods | E | 30 mm | [21] |
| 22 | 71 | 5 years | J | R | Ped, elastic, soft nod, ML, erosive surf | R | 7 × 10 mm | [35] |
| 23 | 72 | 2 years | NA | L | Nods | Pink | 6 mm | [21] |
| 24 | 74 | 1 year | J | L | Well-def | Pinkish | 13 mm | [23] |
| 25 | 75 | 10 months | J | R | Soft, ped, gran | Y | 3 cm | [29] |
| 26 | 75 | 1 year | Polyp v nod, pebbly surfd | Y–R | 7 mm | [33] | ||
| 27 | 78 | 1 year | J | L | Firm p surround ped node | Y–R | 2–5 mm | [25] |
| 28 | 78 | NA | NA | WL, p | Pink | NA | [26] | |
| 29 | 80 | 3 years | W | L | p | R | 8 × 5 mm | CR |
| 30 | 82 | 6 months | W | L | Ped, soft, ML | Pinkish | 15 mm | [24] |
| 31 | 83 | 5 years | NA | NA | Ped, soft, ML | Pink | 25 mm | [24] |
| 32–135 | e–j | V, WL | [2, 26, 34, 46, 56] |
AO age onset, B Black, C case, caul cauliflower-like, CR current report, fil filiform, g granular, J Japanese, L location, m months, ML mulberry-like, mult multiple, NA not available, nod(s) nodule(s), occ occasional, p papules, ped pedunculated, poly polypoid, R red, Ref reference, SL strawberry-like, surf surface, v verrucous, w with, wk weeks, WL wart like, Y yellow, y year(s)
aSize is reported as given in the case reports. This is measured in either in diameter, length × width, or length × width × height
bThree red papules about 1 mm in diameter were scattered in the surrounding area of the lesion. The patient noticed a nodule on the nonpsoriatic part of his scrotum while receiving systemic and topical PUVA therapy. The nodule appeared when the cumulative UVA dosage reached 27.6 J/cm2
cThis patient had four 2–3-mm diameter red papules adjacent to his 7 mm verrucous nodule
dThe patient also had a pulsating subcutaneous induration covered by lightly purplish skin under his scrotal nodule
eJoshi and Ovhal [2] documented a case of a single scrotal lesion that was diagnosed as a verruciform xanthoma in their report. There was no other information available on the patient
fMehra et al. stated that one patient in their study had 2 scrotal lesions appearing at different times in the same year [46]. No other information about the lesions was given
gFukuda H and Saito R performed a review of the Japanese dermatological literature in 2005 and found 100 scrotal cases that were not cited in this review. 36.3% of the lesions were on the left of the scrotum, 31.4% were on the right of the scrotum, 6.9% were bilateral, and 25.4% did not specify [34]
hFurue et al. conducted a study using a sample from a scrotal verruciform xanthoma from a 69-year-old man. No other information about the patient was reported [56]
iHelm et al. reported an additional scrotal case with no other information [26]
Table 3.
Verruciform xanthomas of the female genitalia
| Case | AOa (year) | Duration | Race | Loc | Morphology | Color | Sizeb | A.C. | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| 1c | 15 days | 17 years | NA | R ing fold | Wd, v plaque | E | NA | CHILD | [59] |
| 2d | 1 | 1 year | NA | L lab min | V plaque | Y | 7 × 5 cm | NR | [51] |
| 3 | 5 | 6 years | C | Vulva | V lesion | E, Y | 6 × 6 cm | CHILD | [47] |
| 4e | 8a | NA | Col | R lab maj | Thick v lesion | Brown | NA | CHILD | [60] |
| 5 | 12 | 17 years | B | Vulva | Mult v, inv lesions | NA | NA | NR | [54] |
| 6 | 15a | Childhood | NA | L groin, ext gen | Soft, exudating | Pink | NA | CHILD | [49] |
| 7 | 16 | 9–12 m | NA | L lab maj | Gran, v | W-tan | 1.5 cm | NA | [75] |
| 8 | 16a | Lifelong | NA | L inguinal area | V lesion w small nod | Y-tan | 6 × 3 cm | CHILD | [52] |
| 9f | 30 | NA | NA | L lab min | Poly | R | 2.5 cm | NR | [76] |
| 38 | Wl | 5.0 cm | |||||||
| 10g | 22 | 20 years | W | Genital mucosa | Mult v ind | R | 0.3–2.5 cm | NR | [48] |
| 11 | 27a | Since childhood | W | L vulva and per | Ver hyperker | R | NA | CHILD | [44] |
| 12 | 43a | NA | W | Clitoris | Hyperker, caul, v, wl lesion | Grayish white | 13 mm | LS | [54] |
| 13 | 44 | 8 months | NA | NA | NA | NA | 13 × 10 mm | NA | [36] |
| 14h | 44 | 1 month | NA | L lab maj | Scaly plaque | Pink | 3–4 mm | NR | [53] |
| 15 | 46 | Several years | J | L lab maj | Soft, ped nod w new gran lesion | Brown w Y | 35 × 24 × 22 mm | FEP | [57] |
| 16 | 48 | 2 years | J | Vulva | V surf, wd | O–R | NA | SL, LC | [50] |
| 17 | 51 | NA | NA | Lab min | V lesion, ind | Y–O | NA | LP | [43] |
| 18 | 51 | NA | NA | Clitoris | Ind plaque | Y–O | 4 mm | LS | [43] |
| 19 | 57 | NA | NA | Lab min | Mult ind plaques | Y–O | 20 mm | LS | [43] |
| 20 | 63 | NA | NA | Lab min | Ind plaque | Y–O | 5 mm | LS | [43] |
| 21 | 65a | NA | NA | Vulva | Plaque | NA | 1.5 cm | LMM | [55] |
| 22 | 73 | NA | NA | Lab maj | Leucoplasia | Y–O | 4 mm | LS | [43] |
| 23 | 75 | NA | NA | Fourchette | Ind plaque | Y–O | 10 mm | LS | [43] |
| 24i | 77 | NA | NA | Clitoris | Ind plaque | Y–O | 2 mm | LS | [43] |
| 25 | 77 | NA | NA | Lab maj | Ind plaque | Y–O | 15 mm | LP | [43] |
| 26 | 79 | NA | NA | Fourchette | Ind plaque | Y–O | 3 mm | RD | [43] |
| 27 | 80 | NA | NA | Lab maj | Ker p | Y–O | 2 mm | VPD | [43] |
| 28 | 84 | NA | NA | L vulva | V lesion | NA | NA | NR | [58] |
| 29j | NA | NA | NA | NA | NA | NA | NA | NA | [62] |
AC associated condition, AO age of onset, B black, C Chinese, caul cauliflower-like, CHILD congenital hemidysplasia with ichthyosiform nevus and limb defects, Col Columbian, demac demarcated, Dur duration, ENS epidermal nevus syndrome, ext gen external genitalia, FEP fibroepithelial polyp, gran granular, ind indurated, ing inguinal, inv inverted, J Japanese, ker keratotic, L left, Loc location, lab maj labia majora, lab min labia minora, LC lymphangioma circumscriptum, LMM leiomyomatosis of uterine corpus, LP lichen planus, LS lichen sclerosus, m months, mult multiple, NA not available, nod nodule, NR none reported, O orange, p papule, ped pedunculated, per perineum, poly polypoid, R red, RD radiodermatitis, Ref reference, SL severe lymphedema, v verrucous, VPD Vulvar Paget Disease, w with, wd well-demarcated, wl wart-like, y years
aThe age of onset was not given
bSize is reported as given in the case reports. This is measured in either in diameter, length × width, or length × width × height
cThis young girl developed multiple skin lesions 15 days after birth involving the right inguinal fold, gluteal fold, and leg. She also had lesions on her finger and toe nails and interdigital spaces [59]
dThis young girl had multiple small papules around the anus and on her left thigh. She had no other associated conditions, and was diagnosed with verruciform xanthoma. She was treated with topical imiquimod cream 5%, and the lesions almost entirely cleared 4 months after initiating treatment [50]
eThis Columbian girl was born with skin lesions. By the age of 19 months she had non-verrucous hypopigmented bands and streaks on her right arm. At 3 years old the lesion extended to her hand and fingers. At age 8 she had linear patches and plaques on the right side of her body from her neck to inguinal areas, along with hyperkeratotic and discolored fingernails and a linear band on her left middle finger extending to her nail [60]
fThe vulvar lesion was initially removed by CO2 laser ablasion, but it recurred 8 years later and was successfully treated with wide local excision [75]. This is a case of disseminated verruciform xanthoma. This woman had lesions on her plantar creases, lateral feet, dorsal surface of toes, palmar creases, dorsal aspect of third and fourth right fingers, a scaly plaque on her posterior right ear, multiple genital lesions, and a large plaque on the left inguinal fold [48]
gThis woman had disseminated verruciform xanthoma. She had a 20-year history of multiple 0.5–1 cm discrete hyperkeratotic plaques on the dorsal left food, medial calf, and medial and lateral left knee. She also developed lesions on the plantar left food, buccal mucosa, hard palate, left axilla, and left labia majora [53]
hThis woman had laser ablation of her lesion, but the lesion recurred 16 months following treatment. She then had surgical removal, but the removal was incomplete, and the verruciform xanthoma recurred 2 years later [43]
iDaimaru et al. described a case of verruciform xanthoma of the vulva. No other information was obtained [62]
History
Verruciform xanthoma is a wart-like lesion that most commonly occurs in the oral mucosa. It was first described as a xanthoma-like nevus by Sachs in 1903 [78]. In 1971, Shafer coined the term “verruciform xanthoma” while describing 15 cases in the oral cavity [64]. These lesions were reported as asymptomatic, pale or hyperkeratotic, with a pebbly surface and verrucous appearance. The most common extraoral verruciform xanthomas are reported in the genital region; however, other reported extra-oral locations include the anal region, ear, forearm, foot, hand, leg, nose, and sacrum [65–71, 74].
In 2003, Philipsen et al. did a profile of 282 oral verruciform xanthomas [79]. They found a slight male predominance below the age of 50, with a male:female ratio of 1.6:1, and a slight female predominance above the age of 50, with a male:female ratio of 0.8:1; 73.4% of the oral verruciform xanthomas were on the masticatory mucosa. The majority of cases were reported in Caucasians (139 patients) and Japanese (109 patients), but there were also reports of African Americans, Asians, and South Americans [79].
Differential Diagnosis
Clinically, verruciform xanthomas have a similar appearance to bowenoid papulosis, condyloma acuminatum, erythroplasia of Queyrat, granular cell tumor, giant molluscum contagiosum, seborrheic keratosis, squamous cell carcinoma, verruca vulgaris, verrucous carcinoma, and vulvar intraepithelial neoplasia (Fig. 1) [11, 27, 40, 75, 76]. A biopsy is necessary to confirm the diagnosis of verruciform xanthoma.
Fig. 1.
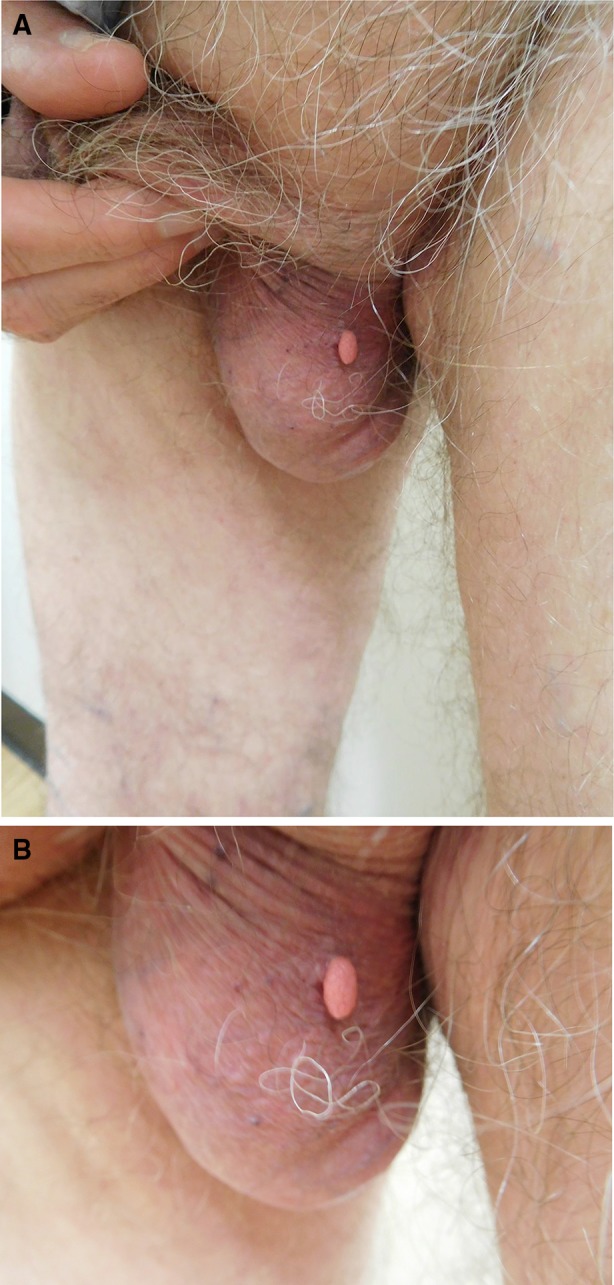
Distant (a) and closer (b) views showing a pedunculated papule protruding from the patient’s left side of the scrotum of an 83-year-old heterosexual monogamous man who had no history of sexually transmitted diseases and no reported HIV risk factors. He presented with an asymptomatic lesion of 3-year duration. Cutaneous examination revealed a flesh-colored 8 × 5 mm wart-like elongated papule localized to the left side of his scrotum. A snip excision was performed for biopsy and removal of the lesion
The histologic differential diagnosis of verruciform xanthoma includes condyloma accuminatum, granular cell epulis, granular cell tumor, verruca vulgaris, and verrucous carcinoma [30]. The characteristic pathologic features of verruciform xanthoma allow it to be distinguished. These features include acanthotic epidermis with parakeratosis that extends deep into the epithelium, uniformly elongated rete ridges, neutrophilic infiltrate in the dermis, and foamy histiocytes throughout the dermal papillae (Fig. 2) [64]. The foam cells stain Periodic Acid Schiff-positive and express CD68 antigen, indicating the presence of glycogen granules in monocyte-macrophage lineage cells [12, 13, 17, 52, 55].
Fig. 2.
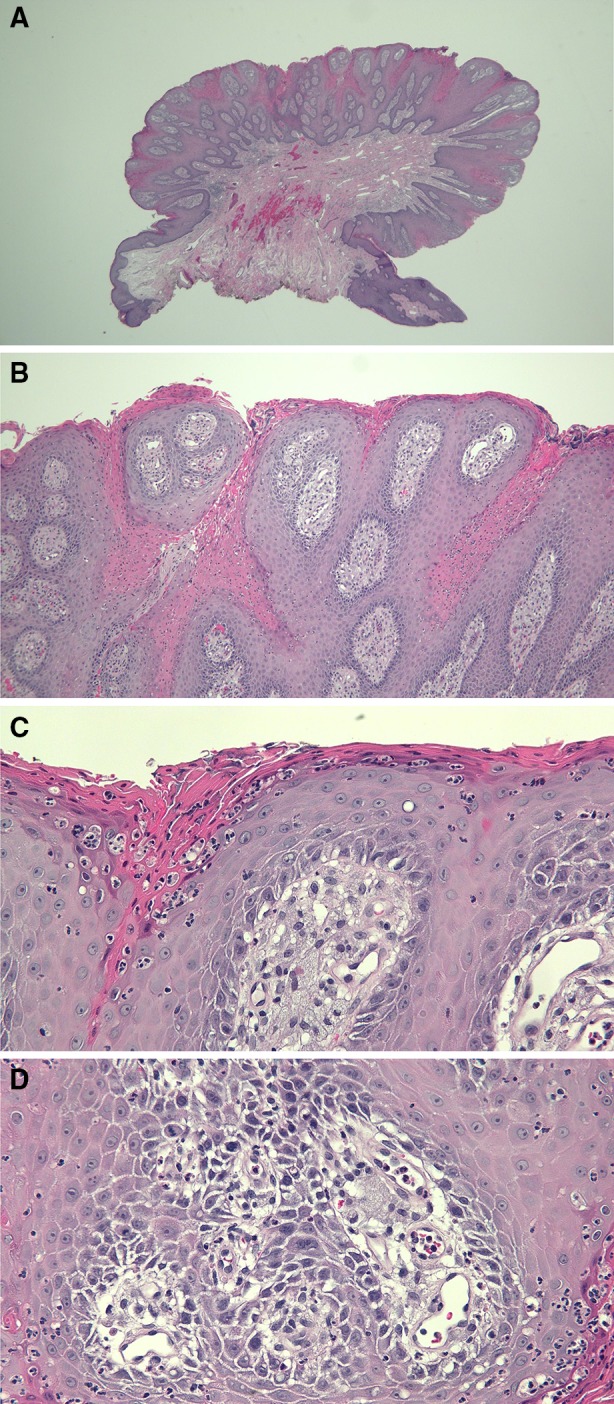
Microscopic examination of the lesion from the 83-year-old man was performed. Low magnification (a) shows a pedunculated tumor with acanthosis, papillomatosis, and elongation of the rete ridges. Intermediate magnification (b, c) reveals parakeratosis and neutrophilic inflammation in the dermis. High magnification (d) reveals numerous foamy histiocytes in the widened dermal papillae. Correlation of the clinical features and the pathologic changes establish a diagnosis of verruciform xanthoma. The lesion was completely removed at the time of biopsy, and the patient applied mupirocin 2% ointment to the site. The excision site has since completely healed without recurrence. (Hematoxylin and Eosin: a = ×2, b = ×10, c = ×20, d = ×40)
Pathogenesis
The pathogenesis of verruciform xanthoma is unknown. The majority of patients with verruciform xanthomas do not have any systemic lipid abnormalities. It has been hypothesized that the lesions are associated with human papilloma virus [30], but multiple studies have found this association to be unlikely [9, 18, 82, 83].
Zegarelli et al. postulated that a local irritant leads to epithelial degradation that initiates an inflammatory response [81]. He states that the inflammatory response damages keratinocytes, which release lipids that are then engulfed by macrophages, leading to the accumulation of foam cells. Mohsin et al. found that damaged keratinocytes release cytokines that attract neutrophils and stimulate rapid growth of the epidermis, supporting Zegarelli et al.’s hypothesis [18].
Other investigators have speculated that verruciform xanthomas may be due to an immunologic reaction [28, 84, 86]. Oliveira et al. proposed that verruciform xanthomas are formed by an autoimmune reaction inducing apoptosis of epithelial cells, similarly to lichen planus [84]. This is supported by multiple cases of verruciform xanthomas reported in association with lichen planus [43, 85].
However, there is not sufficient evidence to conclude a clear mechanism of pathogenesis associated with verruciform xanthomas.
Verruciform Xanthomas of the Penis (Table 1)
The first verruciform xanthoma of the penis was reported in 1981 by Kraemer et al. [11]. To date, there are 31 cases of penile verruciform xanthomas in the literature that have been described in 29 men. The age of onset of the lesions ranged from 8 to 85 years, with a mean of 54.5 years. Most of the lesions occurred in Caucasians.
The duration of the penile verruciform xanthomas prior to establishing the diagnosis ranged from 2 weeks to 25 years, with a mean duration of 3.7 years. The locations (of the 27 lesions for which the site was specified) include the coronal sulcus (18.5%, n = 5), glans (37.0%, n = 10), prepuce (29.6%, n = 8), and shaft (14.8%, n = 4). The colors varied; including brown, erythematous, pink, and yellow.
Verruciform xanthomas of the penis have been reported following necrotizing fasciitis of the anogenital region [3], radical removal of initial verruciform xanthoma with grafting of the foreskin [13], and transurethral prostate resection [4].
Verruciform Xanthomas of the Scrotum (Table 2)
The first scrotal verruciform xanthoma was described in 1984 by Al-Nafussi et al. [32]. Fukuda and Saito carried out a review of the Japanese literature and found that 81% of verruciform xanthomas in the pubic area were located on the scrotum [34]. Including the 102 cases reviewed by Fukuda and Saito, there have been 135 reported cases of scrotal verruciform xanthomas.
Kono suggested that the verruciform xanthomas may be related to irritation of the scrotum by the Japanese custom of sitting on the floor [80]. This is an interesting hypothesis since there is a significant number of scrotal verruciform xanthomas reported in the Japanese literature [34, 35, 42]. These findings support Zegarreli et al.’s proposal that verruciform xanthoma formation may be linked to epithelial degeneration due to irritation [81].
The age of onset was given for 26 of the scrotal lesions, and ranged from ages 19 to 83 years, with a mean age of 59.5 years. The duration of the tumors, prior to establishing the diagnosis, varied from 3 weeks to 20 years. The color of the tumor was most commonly pink.
Scrotal lesions have been associated with arteriovenous haemangioma [29], epidermolytic acanthoma [25, 34], graft versus host disease following bone marrow transplant for acute lymphoblastic leukemia [83], human papillomavirus [30], and psoriasis in a patient undergoing psoralen and ultraviolet A (PUVA) therapy [31]. One scrotal lesion was reported following a kidney transplant [28].
Verruciform Xanthomas of the Inguinal Fold
In addition to the scrotal and penile tumors, verruciform xanthoma of the genitalia has been reported on the inguinal folds. The man had a 7 × 5 cm well-demarcated plaque on his left inguinal fold that extended over the thigh and onto the scrotum. He also had a 1 × 2 cm plaque in the right inguinal fold [69].
Verruciform Xanthomas of the Female Genitalia (Table 3)
The first reported extraoral lesions were two cases of verruciform xanthoma of the vulva, described by Santa Cruz and Martin in 1979 [54]. A total of 28 additional vulvar verruciform xanthomas have since been reported in 27 women. Vulvar verruciform xanthomas have been described in a variety of patients, including African American, Chinese, Caucasian, Columbian, and Japanese women.
The age of onset of the female genital lesions ranges from shortly after birth [in association with congenital hemidysplasia with ichthyosiform erythroderma and limb defects (CHILD syndrome)] to age 85 years, with a mean age of 43.2 years. A total of 27 locations have been reported, which included the clitoris (11.1%, n = 3), external genitalia and groin (3.7%, n = 1), fourchette (7.4%, n = 2), genital mucosa (3.7%, n = 1), inguinal fold (7.4%, n = 2), labia majora (25.9%, n = 7), labia minora (18.5%, n = 5), and vulva not otherwise specified (22.2%, n = 6). The color of the lesion was most commonly yellowish orange.
Vulvar lesions have been found in association with CHILD syndrome [44, 47, 49, 52, 59, 60], fibroepithelial polyp [57], leiomyomatosis of uterus [55], lichen planus [43], lichen sclerosus [43, 54], lymphangioma circumscriptum with severe lymphedema [50], radiodermatitis [43], and vulvar Paget’s disease [43].
Treatment
The verruciform xanthomas are cured by complete excision; however, cases of recurrence have been described [13, 43, 76]. One case of recurrence occurred when the lesion was not completely excised [43]. CO2 laser ablation resulted in the recurrence in two cases of vulvar lesions [43, 76]. However, Joo et al. successfully removed a scrotal xanthoma with shave debulking and fractionated CO2 laser ablation [22]. Guo et al. successfully treated a large (7 × 5 mm) lesion of the labia minora with imiquiod cream 5% [51].
Conclusion
Verruciform xanthomas are benign, asymptomatic wart-like lesions most commonly found in the oral cavity. Although they appear similarly to skin lesions caused by tumors or viral infections, they can be distinguished based on histologic evaluation. The defining pathologic features include hyperkeratosis with parakeratosis, acanthosis, elongated rete ridges, neutrophilic inflammation in the dermis, and foam cells in the dermal papillae.
There have been 194 cases of verruciform genital-associated (Vegas) xanthomas reported in the literature. Patients may seek treatment because of concern of a sexually transmitted disease or the lesion may be discovered as an incidental finding during complete cutaneous skin examination. Verruciform xanthomas of the genitalia share similar histologic characteristics with verruciform xanthomas of the oral cavity. The lesions have been reported in association with a variety of cutaneous diseases and systemic conditions.
Verruciform xanthomas are usually asymptomatic and may be present for many years before being treated. Complete surgical excision is the standard method of treatment, and is typically curative. Fractionated CO2 laser therapy and imiquimoid cream have also been used to successfully remove the lesions. Verruciform xanthoma should be considered in the differential diagnosis of an acquired genital tumor.
Acknowledgements
This work was supported by the National Institute on Aging, Grant T35 AG26757 (PI: Dilip V. Jeste, MD), and the Stein Institute for Research on Aging and the Center for Healthy Aging at the University of California, San Diego. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Katherine M. Stiff and Philip R. Cohen have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/9517F0603C08B0DA.
Contributor Information
Katherine M. Stiff, Email: katherinestiff@gmail.com
Philip R. Cohen, Email: mitehead@gmail.com
References
- 1.Arzberger E, Oliveira A, Hofmann-Wellenhof R, Zalaudek I, Cerroni L, Komericki P. Dermoscopy and reflectance confocal microscopy in verruciform xanthoma of the glans penis. J Am Acad Dermatol. 2015;72:e147–e149. doi: 10.1016/j.jaad.2015.02.1094. [DOI] [PubMed] [Google Scholar]
- 2.Joshi R, OVhal A. Verruciform xanthoma: report of five cases. Indian J Dermatol. 2012;57:479–482. doi: 10.4103/0019-5154.103069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cumberland L, Dana A, Resh B, Fitzpatrick J, Goldenberg G. Verruciform xanthoma in the setting of cutaneous trauma and chronic inflammation: report of a patient and brief review of literature. J Cutan Pathol. 2010;37:895–900. doi: 10.1111/j.1600-0560.2009.01470.x. [DOI] [PubMed] [Google Scholar]
- 4.Sinnya S, Wheller L, Carroll M, Williamson R, De’Ambrosis B. Verruciform xanthoma of the penis: a rare Australian case. Australas J Dermatol. 2015;56:e99–e101. doi: 10.1111/ajd.12161. [DOI] [PubMed] [Google Scholar]
- 5.Cuozzo DW, Vachher P, Sau P, Frishberg DP, James WD. Verruciform xanthoma: a benign penile growth. J Urol. 1995;153:1625–1627. doi: 10.1016/S0022-5347(01)67481-0. [DOI] [PubMed] [Google Scholar]
- 6.Requena L, Sarasa JL, Martin L, Pique E, Farina MC, Olivares M, Escalonilla P. Verruciform xanthoma of the penis with acantholytic cells. Clin Exp Dermatol. 1995;20:504–508. doi: 10.1111/j.1365-2230.1995.tb01390.x. [DOI] [PubMed] [Google Scholar]
- 7.Balus S, Breathnach AS, O’Grady AJ. Ultrastructural observations on ‘foam cells’ and the source of their lipid in verruciform xanthoma. J Am Acad Dermatol. 1991;24:760–764. doi: 10.1016/0190-9622(91)70117-K. [DOI] [PubMed] [Google Scholar]
- 8.Sette CS, Wachholz PA, Brandão LS, Marques GF, Casafus FS, Soares CT. Verruciform xanthoma on the penis: an unusual location. Clin Exp Dermatol. 2015;40:807–808. doi: 10.1111/ced.12579. [DOI] [PubMed] [Google Scholar]
- 9.Ersahin C, Szpaderska AM, Foreman K, Yong S. Verruciform xanthoma of the penis not associated with human papillomavirus infection. Arch Pathol Lab Med. 2005;129:e62–e64. doi: 10.5858/2005-129-e62-VXOTPN. [DOI] [PubMed] [Google Scholar]
- 10.Ronan SG, Bolano J, Manaligod JR. Verruciform xanthoma of penis. Light and electron-microscopic study. Urology. 1984;23:600–603. doi: 10.1016/0090-4295(84)90082-7. [DOI] [PubMed] [Google Scholar]
- 11.Kraemer BB, Schmidt WA, Foucar E, Rosen T. Verruciform xanthoma of the penis. Arch Dermatol. 1981;117:516–518. doi: 10.1001/archderm.1981.01650080070034. [DOI] [PubMed] [Google Scholar]
- 12.Miake S, Nakahara T, Kurihara Y, Hachisuka J, Moroi Y, Furue M. Verruciform xanthoma of the glans penis mimicking squamous cell carcinoma—role of scavenger receptor positive macrophages. Eur J Dermatol. 2012;22:391–392. doi: 10.1684/ejd.2012.1675. [DOI] [PubMed] [Google Scholar]
- 13.Lora V, Kanitakis J, Bertozzi E, Amantea A, Cota C. Recurrent verruciform xanthoma on a skin autograft of the penis. Eur J Dermatol. 2013;23:905–907. doi: 10.1684/ejd.2013.2165. [DOI] [PubMed] [Google Scholar]
- 14.Amantea A, Gaudio E, Catricalà C, Donati P, Balus L. Xantoma verruciforme del pene. G Ital Dermatol Venereol. 1989;124:37–40. [PubMed] [Google Scholar]
- 15.Laguna Urraca G, Concha López A, Tudela Patón MP. Xantoma verruciforme de pene. Actas Urol Esp. 1990;14:210–213. [PubMed] [Google Scholar]
- 16.Canillot S, Stamm C, Balme B, Perrot H. Xanthome verruciforme du gland. Ann Dermatol Venereol. 1994;121:404–407. [PubMed] [Google Scholar]
- 17.Xia TL, Li GZ, Na YQ, Guo YL. Verruciform xanthoma of the penis: report of a case. Chin Med J (Engl) 2004;117:150–152. [PubMed] [Google Scholar]
- 18.Mohsin SK, Lee MW, Amin MB, Stoler MH, Eyzaguirre E, Ma CK, Zarbo RJ. Cutaneous verruciform xanthoma: a report of five cases investigating the etiology and nature of xanthomatous cells. Am J Surg Pathol. 1998;22:479–487. doi: 10.1097/00000478-199804000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Teixeira V, Reis JP, Tellechea Ó, Vieira R, Figueiredo A. Verruciform xanthoma: report of two cases. Dermatol Online J. 2012;18:10. [PubMed] [Google Scholar]
- 20.Takiwaki H, Yokota M, Ahsan K, Yokota K, Kurokawa Y, Ogawa I. Squamous cell carcinoma associated with verruciform xanthoma of the penis. Am J Dermatopathol. 1996;18:551–554. doi: 10.1097/00000372-199610000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Ogata D, Tsuchida T. Characteristic dermoscopic features of verruciform xanthoma: report of three cases. J Dermatol. 2015;42:1103–1104. doi: 10.1111/1346-8138.13034. [DOI] [PubMed] [Google Scholar]
- 22.Joo J, Fung MA, Jagdeo J. Successful treatment of scrotal verruciform xanthoma with shave debulking and fractionated carbon dioxide laser therapy. Dermatol Surg. 2014;40:214–217. doi: 10.1111/dsu.12382. [DOI] [PubMed] [Google Scholar]
- 23.Ito C, Kitazawac R, Makita K, Watanabe T, Toda A, Haraguchi R, Tanaka S, Kitazawa S. Scrotal cutaneous verruciform xanthoma with monocyte chemoattractant protein-1 immunohistochemical study: a case report. J Med Case Rep. 2012;6:260. doi: 10.1186/1752-1947-6-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ohnishi T, Shiraishi H, Fukaya S, Tanaka T, Watanabe S. Verruciform xanthoma: report of three patients with comparative dermoscopic study. Clin Exp Dermatol. 2015;40:156–159. doi: 10.1111/ced.12503. [DOI] [PubMed] [Google Scholar]
- 25.Fujimoto N, Asano C, Ono K, Tajima S. Verruciform xanthoma results from epidermal apoptosis with galectin-7 overexpression. Eur Acad Dermatol Venereol. 2013;27:922–923. doi: 10.1111/j.1468-3083.2012.04664.x. [DOI] [PubMed] [Google Scholar]
- 26.Helm TN, Richards P, Lin L, Helm KF. Verruciform xanthoma with porokeratosis-like features but no clinically apparent lymphedema. J Cutan Pathol. 2012;39:887–888. doi: 10.1111/j.1600-0560.2012.01942.x. [DOI] [PubMed] [Google Scholar]
- 27.Gill BJ, Chan AJ, Hsu S. Verruciform xanthoma. Dermatol Online J. 2014;20:12. [PubMed] [Google Scholar]
- 28.Kanitakis J, Euvrard S, Butnaru AC, Claudy A. Verruciform xanthoma of the scrotum in a renal transplant patient. Br J Dermatol. 2004;150:161–163. doi: 10.1111/j.1365-2133.2004.05752.x. [DOI] [PubMed] [Google Scholar]
- 29.Kishimoto S, Takenaka H, Shibagaki R, Nagata M, Katoh N, Yasuno H. Verruciform xanthoma arising in an arteriovenous haemangioma. Br J Dermatol. 1998;139:546–548. doi: 10.1046/j.1365-2133.1998.02434.x. [DOI] [PubMed] [Google Scholar]
- 30.Khaskhely NM, Uezato H, Kamiyama T, Maruno M, Kariya KI, Oshiro M, Nonaka S. Association of human papillomavirus type 6 with a verruciform xanthoma. Am J Dermatopathol. 2000;22:447–452. doi: 10.1097/00000372-200010000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Yamamoto T, Katayama I, Nishioka K. Verruciform xanthoma in a psoriatic patient under PUVA therapy. Dermatology. 1995;191:254–256. doi: 10.1159/000246557. [DOI] [PubMed] [Google Scholar]
- 32.Al-Nafussi AI, Azzopardi JG, Salm R. Verruciform xanthoma of the skin. Histopathology. 1985;9:245–52. doi: 10.1111/j.1365-2559.1985.tb02439.x. [DOI] [PubMed] [Google Scholar]
- 33.Kimura S. Verruciform xanthoma of the scrotum. Arch Dermatol. 1984;120:1378–1379. doi: 10.1001/archderm.1984.01650460118032. [DOI] [PubMed] [Google Scholar]
- 34.Fukuda H, Saito R. Verruciform xanthoma in close association with isolated epidermolytic acanthoma: a case report and review of the Japanese dermatological literature. J Dermatol. 2005;32:464–468. doi: 10.1111/j.1346-8138.2005.tb00781.x. [DOI] [PubMed] [Google Scholar]
- 35.Takizawa H, Ohnishi T, Watanabe S. Verruciform xanthoma. Report of a case with molecular biological analysis of HPV and immunohistochemical analysis of cytokeratin expression. Clin Exp Dermatol. 2001;26:730–731. doi: 10.1046/j.1365-2230.2001.00926-5.x. [DOI] [PubMed] [Google Scholar]
- 36.Orchard GE, Wilson Jones E, Russel Jones R. Verruciform xanthoma: an immunocytochemical study. Br J Biomed Sci. 1994;51:28–34. [PubMed] [Google Scholar]
- 37.Kukreja M, Kamal M, Ray R, Mannan AA. Verruciform xanthoma of the penis in a young male masquerading as squamous cell carcinoma: case report. Gulf J Oncol. 2011;10:65–68. [Google Scholar]
- 38.Torrecilla Ortíz C, Marco Perrez LM, Dinares Prat J, Autonell J. Xantoma verruciforme de pene. Actas Urol Esp. 1997;21:797–799. [PubMed] [Google Scholar]
- 39.George WM, Azadeh B. Verruciform xanthoma of the penis. Cutis. 1989;44:167–70. [PubMed] [Google Scholar]
- 40.Geiss DF, Del Rosso JQ, Murphy J. Verruciform xanthoma of the glans penis: a benign clinical simulant of genital malignancy. Cutis. 1993;51:369–372. [PubMed] [Google Scholar]
- 41.Shindo Y, Mikoshiba H, Okamoto K, Morohashi M. Verruciform xanthoma of the scrotum. J Dermatol. 1985;12:443–448. doi: 10.1111/j.1346-8138.1985.tb02870.x. [DOI] [PubMed] [Google Scholar]
- 42.Nakamura S, Kanamori S, Nakayama K, Aoki M. Verruciform xanthoma on the scrotum. J Dermatol. 1989;16:397–401. doi: 10.1111/j.1346-8138.1989.tb01288.x. [DOI] [PubMed] [Google Scholar]
- 43.Fite C, Plantier F, Dupin N, Avril MF, Moyal-Barracco M. Vulvar verruciform xanthoma: ten cases associated with lichen sclerosus, lichen planus, or other conditions. Arch Dermatol. 2011;147:1087–1092. doi: 10.1001/archdermatol.2011.113. [DOI] [PubMed] [Google Scholar]
- 44.Gantner S, Rutten A, Requena L, Gassenmaier G, Landthaler M, Hafner C. CHILD syndrome with mild skin lesions: histopathologic clues for the diagnosis. J Cutan Pathol. 2014;41:787–790. doi: 10.1111/cup.12377. [DOI] [PubMed] [Google Scholar]
- 45.Lonsdale RN. Verruciform xanthoma of the penis. Br J Urol. 1992;70:574–575. [PubMed] [Google Scholar]
- 46.Mehra S, Li L, Fan CY, Smoller B, Morgan M, Somach S. A novel somatic mutation of the 3beta-hydroxysteroid dehydrogenase gene in sporadic cutaneous verruciform xanthoma. Arch Dermatol. 2005;141:1263–1267. doi: 10.1001/archderm.141.10.1263. [DOI] [PubMed] [Google Scholar]
- 47.Xu XL, Huang LM, Wang Q, Sun JF. Multiple verruciform xanthomas in the setting of congenital hemidysplasia with ichthyosiform Eeythroderma and limb defects syndrome. Pediatr Dermatol. 2015;32:135–137. doi: 10.1111/pde.12198. [DOI] [PubMed] [Google Scholar]
- 48.Sopena J, Gamo R, Iglesias L, Rodriguez-Peralto JL. Disseminated verruciform xanthoma. Br J Dermatol. 2004;151:717–719. doi: 10.1111/j.1365-2133.2004.06164.x. [DOI] [PubMed] [Google Scholar]
- 49.Zamora-Martinez E, Martin-Moreno L, Barat Cascante A, Castro-Torres A. Another CHILD syndrome with xanthomatous pattern. Dermatologica. 1990;180:263–266. doi: 10.1159/000248044. [DOI] [PubMed] [Google Scholar]
- 50.Ijichi A, Mitoma C, Yasukochi Y, Uchi H, Furue M. Vulvar verruciform xanthoma developing in acquired lymphangioma circumscriptum. J Dermatol. 2016. doi:10.1111/1346-8138.13490. (Epub ahead of print PMID 27334742). [DOI] [PubMed]
- 51.Guo Y, Dang Y, Toyohara JP, Geng S. Successful treatment of verruciform xanthoma with imiquimod. J Am Acad Dermatol. 2013;69:184–186. doi: 10.1016/j.jaad.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 52.Barr RJ, Plank CJ. Verruciform xanthoma of the skin. J Cutan Pathol. 1980;7:422–428. doi: 10.1111/j.1600-0560.1980.tb01216.x. [DOI] [PubMed] [Google Scholar]
- 53.Tang R, Kopp SA, Cobb C, Halpern AV. Disseminated verruciform xanthoma: a case report. Cutis. 2014;93:307–310. [PubMed] [Google Scholar]
- 54.Santa Cruz DJ, Martin SA. Verruciform xanthoma of the vulva. Report of two cases. Am J Clin Pathol. 1979;71:224–228. doi: 10.1093/ajcp/71.2.224. [DOI] [PubMed] [Google Scholar]
- 55.de Rosa G, Barra E, Gentile R, Boscaino A, Di Prisco B, Ayala F. Verruciform xanthoma of the vulva: case report. Genitourin Med. 1989;65:252–254. doi: 10.1136/sti.65.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Furue M, Suzuki H, Kodama T, Hiramoto T, Sugiyama H, Tamaki K. Colocalization of scavenger receptor in CD68 positive foam cells in verruciform xanthoma. J Dermatol Sci. 1995;10:213–219. doi: 10.1016/0923-1811(95)00406-I. [DOI] [PubMed] [Google Scholar]
- 57.Kishimoto S, Takenaka H, Shibagaki R, Nagata M, Yasuno H. Verruciform xanthoma in association with a vulval fibroepithelial polyp. Br J Dermatol. 1997;137:816–820. doi: 10.1111/j.1365-2133.1997.tb01126.x. [DOI] [PubMed] [Google Scholar]
- 58.Leong FJ, Meredith DJ. Verruciform xanthoma of the vulva. A case report. Pathol Res Pract. 1998;194:661–665. doi: 10.1016/S0344-0338(98)80106-4. [DOI] [PubMed] [Google Scholar]
- 59.Fedda F, Khattab R, Ibrahim A, Hayek S, Khalifeh I. Verruciform xanthoma: a special epidermal nevus. Cutis. 2011;88:269–272. [PubMed] [Google Scholar]
- 60.Hashimoto K, Prada S, Lopez AP, Hoyos JG, Escobar M. CHILD syndrome with linear eruptions, hypopigmented bands, and verruciform xanthoma. Pediatr Dermatol. 1998;15:360–366. doi: 10.1046/j.1525-1470.1998.1998015360.x. [DOI] [PubMed] [Google Scholar]
- 61.Minamitsuji Y, Kishi H, Saga K, Masukawa J. A female case of verruciform xanthoma. Jpn J Clin Dermatol. 1996;50:1026–1028. [Google Scholar]
- 62.Daimaru Y, Hatano C, Sato S. A case of verruciform xanthoma of the vulva. Jpn J Clin Dermatol. 1997;51:733–735. [Google Scholar]
- 63.Beutler BD, Cohen PR. Verruciform genital-associated xanthoma: report of patient with verruciform xanthoma of the scrotum and literature review. Dermatol Online J. 2015;21:1087–2108. [PubMed] [Google Scholar]
- 64.Shafer WG. Verruciform xanthoma. Oral Surg Oral Med Oral Pathol. 1971;31:784–789. doi: 10.1016/0030-4220(71)90134-4. [DOI] [PubMed] [Google Scholar]
- 65.Griffel B, Cordoba M. Verruciform xanthoma in the anal region. Am J Proctol Gastroenterol Colon Rectal Surg. 1980;31:24–25. [PubMed] [Google Scholar]
- 66.Jensen JL, Liao SY, Jeffes EW. Verruciform xanthoma of the ear with coexisting epidermal dysplasia. Am J Dermatopathol. 1992;14(5):426–430. doi: 10.1097/00000372-199210000-00009. [DOI] [PubMed] [Google Scholar]
- 67.Blankenship DW, Zech L, Mirzabeigi M, Venna S. Verruciform xanthoma of the upper-extremity in the absence of chronic skin disease or syndrome: a case report and review of the literature. J Cutan Pathol. 2013;40(8):745–752. doi: 10.1111/cup.12159. [DOI] [PubMed] [Google Scholar]
- 68.Mountcastle EA, Lupton GP. Verruciform xanthoma of the digits. J Am Acad Dermatol. 1989;20:313–317. doi: 10.1016/S0190-9622(89)70036-0. [DOI] [PubMed] [Google Scholar]
- 69.Connoly SB, Lewis EJ, Lindholm JS, Zelickson BD, Zachary CB, Tope WD. Management of cutaneous verruciform xanthoma. J Am Acad Dermatol. 2000;42:343–347. doi: 10.1016/S0190-9622(00)90108-7. [DOI] [PubMed] [Google Scholar]
- 70.Huguet P, Toran N, Tarragona J. Cutaneous verruciform xanthoma arising on a congenital lymphoedematous leg. Histopathology. 1995;26(3):277–279. doi: 10.1111/j.1365-2559.1995.tb01443.x. [DOI] [PubMed] [Google Scholar]
- 71.Than T, Birch PJ, Dawes PJ. Verruciform xanthoma of the nose. J Laryngol Otol. 1999;113(1):79–81. doi: 10.1017/S0022215100143221. [DOI] [PubMed] [Google Scholar]
- 72.Zhou H. Verruciform xanthoma of the glans penis: report of a case. Zhonghua Bing Li Xue Za Zhi. 2012;41:127. (PMID 22455893 in Chinese). [PubMed]
- 73.Allen CM, Kapoor N. Verruciform xanthomai n a bone marrow transplant recipient. Oral Surg Oral Med Oral Pathol. 1993;75:591–594. doi: 10.1016/0030-4220(93)90231-R. [DOI] [PubMed] [Google Scholar]
- 74.Cooper TW, Santa Cruz DJ, Bauer EA. Verruciform xanthoma. Occurrence in eroded skin in a patient with recessive dystrophic epidermolysis bullosa. J Am Acad Dermatol. 1983;8:463–467. doi: 10.1016/S0190-9622(83)70050-2. [DOI] [PubMed] [Google Scholar]
- 75.Frankel MA, Rhodes HE, Euscher ED. Verruciform xanthoma in an adolescent: a case report. J Low Genit Tract Dis. 2012;16:70–74. doi: 10.1097/LGT.0b013e31822fcadd. [DOI] [PubMed] [Google Scholar]
- 76.Reich O, Regauer S. Recurrent verruciform xanthoma of the vulva. Int J Gynecol Pathol. 2004;23:75–77. doi: 10.1097/01.pgp.0000101143.79462.f7. [DOI] [PubMed] [Google Scholar]
- 77.Pellice C, Jr, Sole M, Pellice C, Carretero P. Verruciform xanthoma of the penis. J Urol (Paris) 1987;93:41–42. [PubMed] [Google Scholar]
- 78.Sachs O. Beitrage zur histologie der weichen naevi. Archiv Dermatol Syphillis. 1903;66:101–26. (No PMID).
- 79.Philipsen HP, Reichart PA, Takata T, Ogawa I. Verruciform xanthoma—biological profilfe of 282 oral lesions based on a literature survey with nine new cases from Japan. Oral Oncol. 2003;39:325–336. doi: 10.1016/S1368-8375(02)00088-X. [DOI] [PubMed] [Google Scholar]
- 80.Kono Y. Verruciform xanthoma. Hifu Rinsho. 1985;27:1082–83. (No PMID).
- 81.Zegarelli DJ, Zegarelli-Schmidt EC, Zegarelli EV. Verruciform xanthoma. Further light and electron microscopic studies, with the addition of a third case. Oral Surg Oral Med Oral Pathol. 1975;40:246–256. doi: 10.1016/0030-4220(75)90156-5. [DOI] [PubMed] [Google Scholar]
- 82.Travis WD, Davis GE, Tsokos M, Lebovics R, Merrick HF, Miller SP, Gregg RE, Di Bisceglie AM, Parker RI, Ishak KG, et al. Multifocal verruciform xanthoma of the upper aerodigestive tract in a child with systemic lipid storage disease. Am J Surg Pathol. 1989;13:309–316. doi: 10.1097/00000478-198904000-00006. [DOI] [PubMed] [Google Scholar]
- 83.Helm KF, Höpfl RM, Kreider JW, Lookingbill DP. Verruciform xanthoma in an immunocompromised patient: a case report and immunohistochemical study. J Cutan Pathol. 1991;20:84–86. doi: 10.1111/j.1600-0560.1993.tb01256.x. [DOI] [PubMed] [Google Scholar]
- 84.Oliveira PT, Jaeger RG, Cabral LA, Carvalho YR, Costa AL, Jaegar MM. Verruciform xanthoma of the oral mucosa. Report of four cases and a review of the literature. Oral Oncol. 2001;37:326–331. doi: 10.1016/S1368-8375(00)00068-3. [DOI] [PubMed] [Google Scholar]
- 85.Miyamoto Y, Nagayama M, Hayashi Y. Verruciform xanthoma occurring within oral lichen planus. J Oral Pathol Med. 1996;25:188–191. doi: 10.1111/j.1600-0714.1996.tb00218.x. [DOI] [PubMed] [Google Scholar]
- 86.Mostafa KA, Takata T, Ogawa I, Ijuhin N, Nikai H. Verruciform xanthoma of the oral mucosa: a clincopathological study with immunohistochemical findings related to pathogenesis. Virchows Arch A. 1993;423:243–248. doi: 10.1007/BF01606886. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.


