Abstract
Purpose
This paper evaluated the impact of cleft-related surgery on the oral health-related quality of life (OHRQoL) of youth with cleft over time.
Methods
Data were derived from a 5-year, multi-center, prospective, longitudinal study of 1196 youth with cleft lip and/or palate and their caregivers. Eligible youth were between 7.5 and 18.5 years old, spoke English or Spanish, and were non-syndromic. During each observational period, which included baseline, and 1- and 2-year post-baseline follow-up visits, youths and their caregivers completed the Child Oral Health Impact Profile, a validated measure of OHRQoL. Multilevel mixed-effects models were used to analyze the effects of receipt of craniofacial surgery on OHRQoL over time.
Results
During the course of this study a total of 516 patients (43 %) received at least one surgery. Youth in the surgery recommendation group had lower self- (β = −2.18, p < 0.05) and proxy-rated (β = −2.92, p < 0.02) OHRQoL when compared to non-surgical self- and proxy-rated OHRQoL at baseline. Both surgical and non-surgical youth (β = 3.73, p < 0.001) and caregiver (β = 1.91, p < 0.05) ratings of OHRQoL improved over time. There was significant incremental improvement (time × surgery interaction) in self-reported OHRQoL for youth postsurgery (β = 1.04, p < 0.05), but this postsurgery increment was not seen in the caregiver proxy ratings.
Conclusions
Surgical intervention impacts OHRQoL among youth with cleft. Youth who were surgical candidates had lower baseline self- and caregiver-rated OHRQoL when compared to non-surgical youth. Youth who underwent cleft-related surgery had significant incremental improvements in self-rated but not caregiver (proxy)-rated OHRQoL after surgery.
Keywords: Oral health-related quality of life, Cleft lip/palate, Longitudinal, Patient-reported outcomes, Caregiver (proxy) ratings
Introduction
Cleft lip and/or palate (CLP), one of the most common birth defects in the USA [1], affects speech and language development, dental development, and facial appearance. Cleft habilitation involves care from a team of multidisciplinary specialists that starts in infancy and often lasts into young adulthood. Although the primary surgical interventions are usually completed during the first few years of life, a complex myriad of evaluations and interventions that address functional (e.g., tooth development and speech) and esthetic (e.g., facial appearance) issues often occur during the school-age years until the habilitation process is complete. Given the lengthy and complex nature of cleft treatment, CLP is considered a chronic condition that can affect quality of life (QoL) [2, 3].
QoL refers to an individual’s perceptions of his/her position in life in the context of culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns [4]. Health- and oral health-related quality of life are aspects of QoL that refer to the effect of (oral) disease/condition and its treatment on various facets of life (e.g., physical functioning, mental health, and social interaction) [5, 6]. QoL has been used in patient-oriented research to evaluate treatment outcomes at the individual level [7]. Yet, little is known about the impact of cleft treatment over time on the QoL and oral health-related quality of life (OHRQoL) of youth with CLP. A core rationale for such procedures is to improve the well-being of those with cleft.
While many studies find children and adolescents with CLP appear to have good psychosocial functioning, resilience [8–10], and overall self-concept [11], evidence also suggests that individuals with CLP are at risk of lower OHRQoL and psychosocial well-being [7, 12]. Indeed, differences in QoL emerge when specific aspects of well-being are examined, such as personal and social self-concept [13], academic achievement [14], body image (particularly for girls) [15], and depression [16]. Like many chronic conditions, vulnerable populations (e.g., lower SES, people of color) with CLP may have limited access to care and low oral healthcare utilization [17]. Health disparities have also been found as adolescents with cleft who are without health insurance, ethnic minorities, and those having unmet clinical needs (e.g., surgical recommendations) have lower OHRQoL than their privately insured, white counterparts without a surgical recommendation [18, 20]. This existing research, however, is often cross-sectional, has small samples, fails to control for confounders, deals with different age groupings, and/or often lacks a conceptual framework [7, 11]. Further, these reports often focus on the negative psychological status and fail to incorporate positive aspects of psychosocial functioning and QoL.
While the effect of surgery on QoL has been examined for many chronic conditions, including scoliosis [20, 21], obesity [22], and congenital heart disease [23], scant data exist on the effect of cleft surgery on QoL. Therefore, this paper examines QoL among youth with cleft, their caregivers’ perceptions of the youths’ OHRQoL, and the change in these groups over time for surgical and non-surgical patients [24–27]. Demographic characteristics, clinical variables (e.g., cleft diagnosis), and OHRQoL are included as part of our model. Further, environmental or contextual factors related to caregiver characteristics (e.g., payer, sociocultural factors, caregivers’ education) are included in the model as they may influence youth OHRQoL (more information on the basis for this model can be found elsewhere [28]).
The purpose of this study was to analyze the effects of surgery for cleft lip and/or palate on self- and caregiver-rated OHRQoL among school-aged youth. Mixed-effects multilevel models were used to analyze OHRQoL as the outcome variable. Primary hypotheses included: (1) youth who anticipate a surgical intervention will have lower OHRQoL than those who do not and caregiver ratings of OHRQoL will be lower for those youth expected to undergo cleft surgery compared to youth who do not; (2) those who receive cleft surgery will have higher OHRQoL following receipt of surgery; and (3) total prior surgical procedures received will be negatively associated with OHRQoL.
Methods
Data for analysis were derived from a multi-center, prospective, longitudinal study of youth with cleft. Youths and their caregivers participating in this study were followed at one of six major cleft treatment centers in the USA: New York University Langone Medical Center, Children’s Hospital of Philadelphia, Lancaster Cleft Palate Center, Children’s Healthcare of Atlanta, University of Illinois-Chicago, and University of North Carolina-Chapel Hill. The study obtained and maintained IRB approval from the respective institutions throughout the study period. Caregiver consent and youth assent were accomplished as per IRB requirements in accordance with study protocol. The study was conducted from 2009 to 2015 with an enrollment rate across centers of 90 %. Participants included any youth having a cleft lip and palate or cleft palate only 7.5–18.5 years of age who spoke English or Spanish. Youth who were unable to read at a second grade level or had a diagnosis of an incomplete cleft lip without cleft of the alveolus, craniofacial syndrome, or other complex medical conditions were excluded from the study. Caregivers were likewise empaneled if able to speak either English or Spanish. Gift cards in the amount of $40 were provided to compensate for the participants’ time and effort. Participants were assessed at baseline and observed over two or three subsequent follow-up visits. The average length of time observed in the study for participants was 414 days, and the length of time between follow-ups ranged from 6 months to 2 years. During the course of the study, some patients received a surgical intervention and some did not. Details of the study design, including study sample and surgical procedure descriptions, are available elsewhere [18, 29, 30].
Measures
All participants in the study completed a brief demographic questionnaire including items capturing age, gender, cleft center, prior history of surgical intervention (used to create a count of number of prior surgeries), academic grade of the participating youth, ethnicity, and payer status (e.g., private insurance, Medicaid, etc.). In addition to demographic measures, participants were classified as having either a visible facial difference or a non-visible functional difference. The treating surgeon performed clinical evaluations in accordance with American Cleft Palate-Cranio-facial Association standards [31] and then completed a clinical rating form indicating surgical recommendation and procedure, if any, to be performed within 1 year (Surgery Recommendation Group). Invisible (functional) surgery recommendations included those needing secondary palatal surgery, alveolar bone graft surgery, or fistula repair that largely addresses speech dysfunction. Visible recommendations included lip/nose revision or orthognathic surgery that addresses facial appearance; those with invisible and visible recommendations (both) are grouped with visible.
The outcomes in the present analysis were measured using the Child Oral Health Impact Profile (COHIP). The COHIP assesses self-reported (youth) and proxy-reported (caregiver) OHRQoL with five discrete domains and an overall score: Oral Health (specific oral symptoms; ten items; range of 0–40); Functional Well-being (ability to carry out specific everyday tasks; six items; range of 0–24); Emotional Well-being (peer interactions and mood states; eight items; range of 0–32); School (tasks associated with the school environment; four items; range of 0–16); and Self-esteem (positive feelings about self; six items; range of 0–136). The COHIP uses a 5-point Likert scale (‘never’ = 1, ‘almost never’ = 2, ‘sometimes’ = 3, ‘fairly often’ = 4, and ‘almost all the time’ = 5); higher scores indicate better QoL. This instrument has demonstrated excellent psychometric properties [32].
Data and procedures
Summary scores for the COHIP were calculated by averaging individual item responses (for individual subscales and all items for the overall COHIP score) with adjustment for missing data following the established methods [32]. First, missing data were <2 %; participants with missing data on more than two-thirds of the items on a subscale were not included in the analysis. Second, at each observational period, participants with fewer than five total items missing had missing data imputed using the raw mean score of the specified within-visit sample scores.
Youth were classified as being <12 or ≥12 years old. Race/ethnicity was categorized as White, Hispanic, Black, Asian, and other. Payment type for surgical procedures was dichotomized as either private or non-private insurance. Type of cleft (cleft palate or cleft lip/palate) and invisible/visible surgery recommendations were determined using clinical records. Any participant with both a visible and invisible surgical recommendation was classified as visible.
Receipt of surgery was included as a time-varying predictor. Participants received surgery for facial differences (for example, facial asymmetry or jaw discrepancies) in between observational periods throughout the duration of the study. All observations, including receipt of surgery, were temporally ordered in the dataset. Surgery was not included as a time point in longitudinal analyses, but was used to indicate when a participant transitioned from the non-surgical group to the surgery received group (time-varying surgery variable =0 before and =1 after surgery during the course of the study). Youth transitioned into the received surgery group if they received an actual surgery prior to the final observational period.
To explore possible temporal delays in change in OHRQoL outcomes associated with surgery, models included lagged predictors and multiple measures of time. First, a predictor for lag from first surgery received during the course of this study was calculated indicating the total time in days that had passed since the date of first recorded surgery. Second, a lag of one observational period was used to reflect delayed response to receipt of surgery. For example, if a study participant received surgery between baseline and the first follow-up observation, then the one-period lag would reflect surgery at the second follow-up. Finally, a variable for the amount of time occurring between observed measurement occasions was included (as this varied between participants). Each lag was used in separate models in the analysis.
Statistical analysis
Baseline descriptive statistics by visit were first calculated for cleft palate/cleft lip and palate status, surgical group (visible or invisible), payer type, gender, race/ethnicity, number of prior surgeries, and age group, as well as means and standard deviations for COHIP subscales and overall COHIP (outcomes). Descriptive statistics were further stratified by treatment group (surgery received/not received) for post-baseline visits.
Multilevel mixed-effects models (developed for youth and caregivers, respectively) were used to examine (Aim 1) the initial status (compare baseline OHRQoL) and rate of change in OHRQoL as a function of surgical status recommendation (recommended for surgery within 1 year versus not recommended for surgery within 1 year) as well as (Aim 2) receipt of actual surgery. These longitudinal models were used to account for the nesting of observations within participant and for participants within treatment center. As the sample size for the final wave of data collected was dramatically smaller than previous waves, we exclude these observations from the models. Intraclass correlation coefficients (ICCs) were calculated to estimate the proportion of variance explained at the participant level, and within-participant unconditional models were used to estimate the average change over time. Primary predictors of interest included receipt of surgery (treatment), time, and their interaction. Adjusted models included additional covariates for gender, race/ethnicity, CPO/CLP status, age group, payer status, and prior surgical history. Random intercepts were included for participant and center. Following primary analyses, results were compared to models using lagged predictors for surgical receipt and observational period. Sensitivity analyses included incorporating alternative measures of time and randomly varying slopes for receipt of surgery. Statistical significance was determined at the p = 0.05 level; the analysis was conducted using SAS 9.4 [33].
Results
There were 1196 participants in the study at baseline (Table 1); 77.5 % had cleft lip and palate, and 22.5 % had cleft palate only. At study enrollment, the average number of prior surgeries was 4.97 (SD = 3.1); 191 (16 %) participants presented with either a visible or visible/invisible surgical recommendation, 159 (13.3 %) participants had an invisible surgical recommendation only, and 798 participants (66.7 %) had no surgical recommendation. There were 580 participants (48.5 %) under 12 years of age and 616 participants (51.5 %) aged 12 years or older. For race/ethnicity, 731 participants were White (61.1 %) followed by 189 Hispanic/Latino (15.8 %), 126 Asian (10.5 %), 99 Black (8.3 %), and 39 ‘other’ race (3.3 %). Finally, there were 671 males (56.1 %) and 525 females (43.9 %). Mean youth and caregiver COHIP scores (presented in Table 2) at baseline were within expected levels as described in instrument validation reports [26, 32, 34]. There were 937 participants who presented at first follow-up. Between baseline and the first follow-up period, 258 participants (27.5 %) received a surgical intervention (Tables 3, 4), which were for visible/invisible (54 %) as well as invisible (46 %) needs.
Table 1.
Sample demographics by visit
| Baseline |
First follow-up |
Second follow-up |
||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Overall | 1196 | 937 | 715 | |||
| CPO/CLP | ||||||
| CLP | 927 | 77.5 | 753 | 80.4 | 580 | 81.2 |
| CPO | 269 | 22.5 | 184 | 19.6 | 135 | 18.9 |
| Payor | ||||||
| Private | 613 | 51.3 | 486 | 51.9 | 381 | 53.3 |
| Non-private | 531 | 44.4 | 402 | 42.9 | 286 | 40 |
| Missing | 52 | 4.4 | 49 | 5.2 | 48 | 6.7 |
| Surgery group | ||||||
| Yes | 258 | 27.5 | 259 | 36.2 | ||
| No (comparator) | 679 | 72.5 | 456 | 63.8 | ||
| Gender | ||||||
| Female | 525 | 43.9 | 412 | 44.0 | 319 | 44.6 |
| Male | 671 | 56.1 | 525 | 56.0 | 396 | 55.4 |
| Race/ethnicity | ||||||
| White | 731 | 61.1 | 551 | 58.8 | 423 | 59.2 |
| Hispanic/latino | 189 | 15.8 | 162 | 17.3 | 124 | 17.3 |
| Black | 99 | 8.3 | 77 | 8.2 | 53 | 7.4 |
| Asian | 126 | 10.5 | 108 | 11.5 | 84 | 11.8 |
| Other | 39 | 3.26 | 29 | 3.09 | 22 | 3.08 |
| Age (categorized) | ||||||
| <12 | 580 | 48.49 | ||||
| 12 and older | 616 | 51.51 | ||||
Table 2.
COHIP subscale and overall scores by visit
| Baseline |
First follow-up |
Second follow-up |
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Child Oral Symptoms | 25.3 | 6.5 | 26.1 | 6.3 | 26.3 | 6.4 |
| Child Functional Well-being | 17.7 | 4.5 | 18.3 | 4.3 | 18.8 | 4.1 |
| Child Socio-emotional Well-being | 23.5 | 7.3 | 24.8 | 7.1 | 25.7 | 6.3 |
| Child School/Environmental | 13.3 | 2.9 | 13.7 | 2.6 | 13.8 | 2.4 |
| Child Self-Esteem | 16.9 | 4.5 | 17.4 | 4.4 | 17.7 | 3.9 |
| Child Total Quality of Life Score | 96.9 | 18.7 | 100.3 | 18.4 | 102.4 | 17.2 |
| Caregiver Oral Symptoms | 25.8 | 6.3 | 25.9 | 6.4 | 26.3 | 6.2 |
| Caregiver Functional Well-being | 16.4 | 4.6 | 16.7 | 4.5 | 17.0 | 4.4 |
| Caregiver Socio-emotional Well-being | 22.0 | 7.7 | 22.7 | 7.5 | 23.4 | 7.0 |
| Caregiver School/Environmental | 13.3 | 2.8 | 13.5 | 2.7 | 13.6 | 2.5 |
| Caregiver Self-Esteem | 16.4 | 4.3 | 16.8 | 4.2 | 16.8 | 4.2 |
| Caregiver Total Quality of Life Score | 93.8 | 19.7 | 95.6 | 19.9 | 97.1 | 18.7 |
Table 3.
Overall child COHIP mixed model results
| β | p value | 95 % LCL | 95 % UCL | |
|---|---|---|---|---|
| Child COHIP | ||||
| Intercept | 92.61 | <0.0001 | 79.93 | 105.28 |
| Visit | 3.73 | <0.0001 | 1.82 | 5.62 |
| Surgery | −2.18 | 0.041 | −9.16 | −1.27 |
| Visit × surgery | 1.04 | 0.029 | 0.089 | 1.87 |
| Gender | 4.21 | 0.006 | 1.27 | 7.13 |
| Race/ethnicity | ||||
| Hispanic | 1.06 | 0.390 | −1.36 | 3.49 |
| Black | −1.85 | 0.248 | −4.99 | 1.29 |
| Asian | 0.15 | 0.922 | −2.86 | 3.16 |
| Other | −1.91 | 0.211 | −4.92 | 1.09 |
| CPO/CLP | 7.05 | <0.005 | 2.12 | 11.98 |
| >12 YO | −3.14 | 0.04 | −6.16 | −0.11 |
| Payer (non-private) | −0.90 | 0.04 | −3.01 | −0.92 |
| Invisible versus visible + both | −1.34 | 0.03 | −4.14 | −0.72 |
| Surgical history | −0.51 | 0.04 | −0.99 | −0.08 |
Bold values indicate statistically significant
Table 4.
Overall caregiver COHIP mixed model results
| β | p value | 95 % LCL | 95 % UCL | |
|---|---|---|---|---|
| Caregiver COHIP | ||||
| Intercept | 97.97 | <0.001 | 84.67 | 111.27 |
| Visit | 1.91 | <0.05 | 0.11 | 3.91 |
| Surgery | −2.92 | 0.011 | −4.41 | −1.04 |
| Visit × surgery | −0.63 | 0.456 | −1.74 | 0.69 |
| Gender | 2.34 | 0.14 | −0.67 | 5.43 |
| Race/ethnicity | ||||
| Hispanic | −3.71 | 0.061 | −7.64 | 0.18 |
| Black | −1.52 | 0.545 | −6.43 | 3.40 |
| Asian | 4.17 | 0.088 | −0.62 | 8.95 |
| Other | −4.40 | 0.083 | −9.37 | 0.58 |
| CPO/CLP | 5.94 | 0.024 | 0.77 | 11.04 |
| >12 YO | −0.34 | 0.834 | −3.51 | 2.82 |
| Payer (non-private) | −1.21 | 0.353 | −3.76 | 1.34 |
| Invisible versus visible + both | 1.69 | 0.276 | −1.31 | 4.69 |
| Surgical history | −0.86 | 0.0003 | −1.33 | −0.40 |
Bold values indicate statistically significant
Of the 715 participants who presented at second follow-up, 259 (36.2 %) had received a surgical intervention, which were for visible/invisible (58 %) as well as invisible (42 %) needs.
During the course of this study, a total of 516 patients (43 %) received at least one surgery. Model results (Table 3) show that in the overall sample, youth self-ratings improved over time (visit) on the overall COHIP (β = 3.73, p < 0.001). Youth who received a surgical recommendation at baseline (N = 402, 33.3 %) showed lower average overall COHIP scores (β = −2.18, p < 0.05) as well as lower functional well-being, emotional well-being, and self-esteem scores (subscale scores not shown) when compared to youth who did not receive a surgical recommendation at baseline (N = 798, 66.7 %). Those youth who received surgery during the study period, as indicated by receipt of surgery, showed a significant incremental postsurgical improvement in the change over time of functional well-being, emotional well-being, self-esteem and overall COHIP (β = 1.04, p < 0.05) scores (visit × surgery).
Male participants had higher self-rated emotional well-being and overall COHIP scores than female participants. Compared to younger participants, youth 12 years of age and older had lower scores on emotional well-being, school, and overall COHIP. Youth with non-private insurance had lower scores on oral symptoms, functional and emotional well-being, school, and overall COHIP scores than those with private insurance. Participants with cleft palate only had higher scores on oral symptoms, emotional well-being, school, and overall COHIP than participants with cleft lip and palate. Compared to those with a visible or invisible + visible surgical recommendation, youth with invisible surgical recommendations had higher scores on functional and emotional well-being, school, and overall COHIP. A negative relationship was found between number of prior surgeries and scores on oral symptoms, functional well-being, school, and overall COHIP.
Model results (Table 4) show that for the overall sample, caregiver ratings for the overall COHIP score (β = 1.91, p < 0.05) improved over time (visit). Caregivers of youth who received a surgical recommendation at baseline showed lower average functional well-being, emotional well-being, school (subscale scores not shown), and lower average overall COHIP scores (β = −2.92, p < 0.02) when compared to caregivers of youth who did not receive a surgical recommendation at baseline. Receipt of surgery was not found to be associated with a significant incremental improvement in the change over time in caregiver-rated OHRQoL scores (β = −0.63, p > 0.05) (visit × surgery interaction). Participants with cleft palate only had higher caregiver-rated scores on emotional well-being and overall COHIP than their cleft lip and palate counterparts. A negative relationship was also found between number of prior surgeries and caregiver-rated scores on oral symptoms, functional and emotional well-being, school, and overall COHIP.
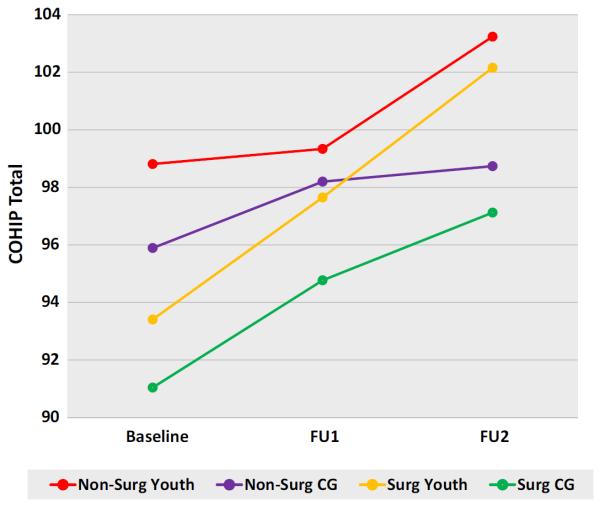
Figure 1 shows trends in overall OHRQoL over time by group. At baseline and at the second follow-up visit, youth not receiving surgery had the highest reported OHRQoL, followed by non-surgical caregivers, surgical youth, and finally caregivers of youth who received surgery reporting the lowest COHIP scores. However, all groups reported an increase in OHRQoL over time. Surgical youth experienced the greatest increase in OHRQoL between baseline and the second follow-up visit.
Fig. 1.
COHIP summary by group
A treatment lag of one observational period was unrelated to QoL outcomes, and the effect of receiving surgery did not change as a function of lag time between observations (results not shown). Alternate models specifying random effects for slope of receipt of surgery were comparable to those from mixed models.
Discussion
This paper examined the relationship between OHRQoL and receipt of surgery among school-aged youth with cleft using data from the largest multicenter, prospective, observational study on patient-reported outcomes. The results largely support the study hypotheses. Those youth with a surgical recommendation at baseline had lower self- and caregiver-rated OHRQoL than youth without a surgical recommendation at baseline. All youth in the sample had improvements on average in self-reported and caregiver-reported OHRQoL during the course of the study. Youth with a surgical event had incrementally improved self-rated OHRQoL scores postsurgery (significant time × surgery interaction). However, this incremental postsurgery increase was not detected in the caregiver’s ratings (no significant time × surgery interaction). It should be noted that those youth without a surgical recommendation within the year may have completed treatment prior to the study and/or additional surgery is expected to be scheduled at a later date (i.e., when facial growth is complete).
In other research conducted with a subsample of the present participants, MID (minimally important difference) estimates using an anchor-based approach indicated that the minimally important difference for the overall COHIP was 2.95 [35]. Framing the present finding in this manner suggests that the surgical candidates initially rated their OHRQoL as lower than peers without a surgical recommendation and that the improvements over time were modest.
A novel result was that a higher number of previous surgeries were associated with lower self- and caregiver-rated OHRQoL scores. This finding may indicate that participants with a greater number of previous surgeries had more severe cleft-related defects and/or unrealistic expectations associated with surgery treatment. An alternative explanation could be that surgery may have a point of diminishing returns. While the timing of surgery and number of procedures may be important to individuals’ OHRQoL, these results suggest that adjunct psychological counseling could provide support to patients and their families undergoing the stress and expectations associated with surgery [36, 37].
Female participants had lower self-rated emotional well-being and overall COHIP scores than the male participants. This finding supports prior research related to gender differences in appearance and attractiveness norms [38, 39]. Girls often internalize these norms [40], which place them at higher risk of appearance-related body image concerns associated with their facial difference [41–43]. Adolescent females with CLP may be particularly vulnerable to reduced QoL, and this negative self-report suggests that caregivers and clinicians should be vigilant regarding the well-being of these young females.
Participants with cleft palate only (an invisible facial difference) had higher self- and caregiver-rated OHRQoL than participants with cleft lip and palate (a visible facial difference). Since cleft lip and palate is a more severe and visible condition, it is important to identify risk and protective factors for OHRQoL and psychosocial well-being. With our cultural emphasis on appearance, exploring ways to foster resilience in this patient population is vital [10, 44, 45].
These findings underscore that patient-reported outcomes, in this case the COHIP, have evaluative properties that are responsive to change and clearly capture a different perspective than ratings by surgeons regarding their patients’ facial appearances and/or functional status. Despite the costs of care and associated expenses in time and effort, the results suggest a positive impact of surgical interventions on OHRQoL across age groups, ethnicities, and family payer status. Notably, those without private insurance had consistently lower scores on average than their privately insured counterparts. This finding supports a consistent issue in public health across chronic conditions and the general population whereby not having private insurance and being a racial/ethnic minority (i.e., Hispanic or Black) is associated with less positive health outcomes and barriers to care [46–48].
While the findings contribute to the existing cleft literature, study results should be interpreted with care. Ultimate OHRQoL outcomes cannot be fully understood as half of the sample was 12 years old or younger and 27.8 % (N = 344) received an additional surgical recommendation at the most recent follow-up study evaluation. Of those 344 participants, 48 rejected their surgical recommendations. Our findings suggest that longer term follow-up of a cohort such as the present sample would reveal additional insights about quality of life, health utilization, and satisfaction with care. Relatedly, the enactment of the Affordable Care Act ensures that young adults can remain on their parents’ insurance and continue to have their treatment covered until age 26. This change in coverage coupled with the recent reported dissatisfaction among young adults with cleft [49] might result in an increased demand for ongoing cleft care. Indeed, new evidence advises that young adults often seek additional care for a range of reasons (e.g., dental implants, hearing concerns, other perceived esthetic needs) as indicated by CLEFTLINE officials, a call-in service of the American Cleft Palate Educational Foundation [50]. Therefore, continuing to follow this cohort will be critical to ascertain the trajectory of OHRQoL until treatment is no longer sought and/or recommended.
Other study limitations include the possibility that the effects of surgery may be related to youth or caregiver perceptions of facial and speech differences, respectively. Further research should investigate the interrelationships among OHRQoL and patient/caregiver/professional ratings of extent of difference. Additionally, a majority of individuals receiving surgery either did not complete the study protocol or present for all follow-up visits, in part due to the additional interventions throughout the study period. As a result, participant attrition may bias results. The use of mixed models allowed the analysis to draw from all available data, though future studies incorporating multiple imputation for multilevel data may be useful. Furthermore, current analyses used tests of statistical significance, which may not capture the true effect of treatment on OHRQoL [51]. Additional reporting of the minimally important difference and clinically meaningful change will be undertaken but is beyond the scope of this paper [27, 35, 52]. Finally, since there was no control group in this study, incorporating population-based assessments like items from the National Survey on Children with Special Health and N-HANES queries as well as generic quality of life surveys would provide worthwhile comparisons [53–55] regarding employment, educational attainment, health care utilization, barriers to care and QoL that facilitate group comparisons and elucidate long-term treatment outcomes in this population. Currently, scant data exist on adults with cleft and only continued use of multicenter studies can provide vital data and increase generalizability regarding this population compared to normative and other patient groups. Empaneling a youth sample for long-term follow-up could afford a means of capturing distal outcomes.
In conclusion, the COHIP appears to be a sensitive outcome measure that suggests while those youth recommended for surgery initially have lower OHRQoL than youth without a surgical recommendation, having cleft-related surgery improves youth OHRQoL. Additionally, youth with a high number of previous surgical interventions are at risk of decreased OHRQoL. Caregiver proxy ratings appear to provide similar findings with the exception of incrementally improved OHRQoL following surgery.
Acknowledgments
The authors recognize and thank the National Institutes of Health/National Institute for Dental and Craniofacial Research for supporting this research project, Quality of Life in Children with Cleft—DE018729 (H.L. Broder, PI). We appreciate the participation of the patients and their caregivers at the research sites. Lastly, we thank our research and clinical collaborators at New York University Langone Medical Center (R. Flores, PI), Children’s Hospital of Philadelphia (C. Crerand, D. Sarwer, PIs), Children’s Healthcare of Atlanta (J. Riski, PI), University of North Carolina, (M. Stein, PI); and University of Illinois at Chicago, (J. Rosenberg, PI).
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Compliance with ethical standards
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent/assent was obtained from all individual participants included in the study.
References
- 1.Canfield MA, Ramadhani TA, Yuskiv N, Davidoff MJ, Petrini JR, Hobbs CA, et al. Improved national prevalence estimates for 18 selected major birth defects—United States, 1999–2001 (Reprinted from MMWR, vol 54, pg 1301–1305, 2006) Jama-Journal of the American Medical Association. 2006;295(6):618–620. [Google Scholar]
- 2.Patrick DL, Topolski TD, Edwards TC, Aspinall CL, Kapp-Simon KA, Rumsey NJ, et al. Measuring the quality of life of youth with facial differences. Cleft Palate-Craniofacial Journal. 2007;44(5):538–547. doi: 10.1597/06-072.1. [DOI] [PubMed] [Google Scholar]
- 3.Broder HL. Children’s oral health-related quality of life. Community Dentistry and Oral Epidemiology. 2007;35(Suppl 1):5–7. doi: 10.1111/j.1600-0528.2007.00400.x. [DOI] [PubMed] [Google Scholar]
- 4.WHOQOL Group The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science and Medicine. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 5.Wehby GL, Ohsfeldt RL, Murray JC. Health professionals’ assessment of health-related quality of life values for oral clefting by age using a visual analogue scale method. The Cleft Palate-Craniofacial Journal. 2006;43(4):383–391. doi: 10.1597/05-066.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure? Community Dentistry and Oral Epidemiology. 2007;35(6):401–411. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 7.Queiroz Herkrath APCD, Herkrath FJ, Rebelo MAB, Vettore MV. Measurement of health-related and oral health-related quality of life among individuals with nonsyndromic orofacial clefts: A systematic review and meta-analysis. Cleft Palate-Craniofacial Journal. 2015;52(2):157–172. doi: 10.1597/13-104. [DOI] [PubMed] [Google Scholar]
- 8.Baker SR, Owens J, Stern M, Willmot D. Coping strategies and social support in the family impact of cleft lip and palate and parents’ adjustment and psychological distress. Cleft Palate-Craniofacial Journal. 2009;46(3):229–236. doi: 10.1597/08-075.1. [DOI] [PubMed] [Google Scholar]
- 9.Broder HL. Using psychological assessment and therapeutic strategies to enhance well-being. Cleft Palate-Craniofacial Journal. 2001;38(3):248–254. doi: 10.1597/1545-1569_2001_038_0248_upaats_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 10.Feragen KB, Borge AI, Rumsey N. Social experience in 10-year-old children born with a cleft: Exploring psychosocial resilience. Cleft Palate-Craniofacial Journal. 2009;46(1):65–74. doi: 10.1597/07-124.1. [DOI] [PubMed] [Google Scholar]
- 11.Hunt O, Burden D, Hepper P, Johnston C. The psychosocial effects of cleft lip and palate: A systematic review. European Journal of Orthodontics. 2005;27(3):274–285. doi: 10.1093/ejo/cji004. [DOI] [PubMed] [Google Scholar]
- 12.Topolski TD, Edwards TC, Patrick DL. Quality of life: How do adolescents with facial differences compare with other adolescents? Cleft Palate-Craniofacial Journal. 2005;42(1):25–32. doi: 10.1597/03-097.3.1. [DOI] [PubMed] [Google Scholar]
- 13.Broder H, Strauss RP. Self-concept of early primary-school age children with visible or invisible defects. Cleft Palate-Craniofacial Journal. 1989;26(2):114–118. [PubMed] [Google Scholar]
- 14.Wehby GL, Collet B, Barron S, Romitti PA, Ansley TN, Speltz M. Academic achievement of children and adolescents with oral clefts. Pediatrics. 2014;133(5):785–792. doi: 10.1542/peds.2013-3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crerand CE, Sarwer DB, Kazak AE, Clark A, Rumsey N. Body image and psychosocial functioning in adolescents with craniofacial conditions. The Cleft Palate-Craniofacial Journal. 2015 doi: 10.1597/15-167. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pinquart M, Shen Y. Depressive symptoms in children and adolescents with chronic physical illness: An updated meta-analysis. Journal of Pediatric Psychology. 2011;36(4):375–384. doi: 10.1093/jpepsy/jsq104. [DOI] [PubMed] [Google Scholar]
- 17.Al Agili DE, Roseman J, Pass MA, Thornton JB, Chavers LS. Access to dental care in Alabama for children with special needs: Parents’ perspectives. Journal of the American Dental Association. 2004;135:490–495. doi: 10.14219/jada.archive.2004.0216. [DOI] [PubMed] [Google Scholar]
- 18.Broder HL, Wilson-Genderson M, Sischo L, Norman RG. Examining factors associated with oral health-related quality of life for youth with cleft. Plastic and Reconstructive Surgery. 2014;133(6):828e–834e. doi: 10.1097/PRS.0000000000000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broder HL, Wilson-Genderson M, Sischo L. Health disparities among children with cleft. American Journal of Public Health. 2012;102(5):828–830. doi: 10.2105/AJPH.2012.300654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danielsson AJ, Wiklund I, Pehrsson K, Nachemson AL. Health-related quality of life in patients with adolescent idiopathic scoliosis: A matched follow-up at least 20 years after treatment with brace or surgery. European Spine Journal. 2001;10(4):278–288. doi: 10.1007/s005860100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard A, Donaldson S, Hedden D, Stephens D, Alman B, Wright J. Improvement in quality of life following surgery for adolescent idiopathic scoliosis. Spine. 2007;32(24):2715–2718. doi: 10.1097/BRS.0b013e31815a51cd. [DOI] [PubMed] [Google Scholar]
- 22.Karlsson J, Taft C, Rydén A, Sjöström L, Sullivan M. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: The SOS intervention study. International Journal of Obesity. 2007;31(8):1248–1261. doi: 10.1038/sj.ijo.0803573. [DOI] [PubMed] [Google Scholar]
- 23.Latal B, Helfricht S, Fischer JE, Bauersfeld U, Landolt MA. Psychological adjustment and quality of life in children and adolescents following open-heart surgery for congenital heart disease: A systematic review. BMC Pediatrics. 2009;9(1):6. doi: 10.1186/1471-2431-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. Journal of Clinical Epidemiology. 1994;47(1):81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 25.Sischo L, Broder HL. Oral health-related quality of life: What, why, how, and future implications. Journal of Dental Research. 2011;90(11):1264–1270. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Genderson MW, Sischo L, Markowitz K, Fine D, Broder HL. An overview of children’s oral health-related quality of life assessment: From scale development to measuring outcomes. Caries Research. 2013;47(Suppl 1):13–21. doi: 10.1159/000351693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Controlled Clinical Trials. 1989;10(4):407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 28.Broder HL, Wilson-Genderson M, Sischo L. Examination of a theoretical model for oral health-related quality of life among youths with cleft. American Journal of Public Health. 2014;104(5):865–871. doi: 10.2105/AJPH.2013.301686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruff RR, Sischo L, Broder HL. Resiliency and socioemotional functioning in youth receiving surgery for orofacial anomalies. Community Dentistry and Oral Epidemiology. 2016;44(4):371–380. doi: 10.1111/cdoe.12222. doi: 10.1111/cdoe.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Long RE, Jr., Wilson-Genderson M, Grayson BH, Flores RL, Broder HL. Oral health related quality of life and self-rated speech in children with existing fistulas in mid-childhood and adolescence. The Cleft Palate-Craniofacial Journal. 2015 doi: 10.1597/15-123. doi: 10.1597/15-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Cleft Palate Association Parameters for the evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies (Revised Edition–November 2009) Cleft Palate-Craniofacial Journal. 1993;30(Suppl 1) [PubMed] [Google Scholar]
- 32.Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the Child Oral Health Impact Profile (COHIP Child’s version) Community Dentistry and Oral Epidemiology. 2007;35(Suppl 1):20–31. doi: 10.1111/j.1600-0528.2007.0002.x. [DOI] [PubMed] [Google Scholar]
- 33.SAS Institute . Base SAS 9.4 procedures guide: Statistical procedures. SAS Institute; Cary: 2014. [Google Scholar]
- 34.Dunlow N, Phillips C, Broder HL. Concurrent validity of the COHIP. Community Dentistry and Oral Epidemiology. 2007;35(Suppl 1):41–49. doi: 10.1111/j.1600-0528.2007.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruff RR, Broder HL, Sischo L. Minimally important difference of the child oral health impact profile for children with orofacial anomalies. Health and Quality of Life Outcomes. 2016 doi: 10.1186/s12955-016-0544-1. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sischo L, Clouston S, Phillips C, Broder HL. Caregiver responses to early cleft palate care: A mixed method approach. Health Psychology. 2015;35(5):474–482. doi: 10.1037/hea0000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broder HL, Flores RL, Clouston S, Kirschner RE, Garfinkle JS, Sischo L, et al. Surgeon’s and care-givers’ appraisal of primary cleft lip treatment with and without nasoalveolar molding: A prospective multicenter pilot study. Plastic and Reconstructive Surgery. 2015;137(3):938–945. doi: 10.1097/01.prs.0000479979.83169.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bordo S. Unbearable weight: Feminism, western culture, and the body. University of California Press; Berkeley: 2003. [Google Scholar]
- 39.Brumberg JJ. The body project: An intimate history of American girls. Knopf Doubleday Publishing Group; New York: 2010. [Google Scholar]
- 40.Lawler M, Nixon E. Body dissatisfaction among adolescent boys and girls: The effects of body mass, peer appearance culture and internalization of appearance ideals. Journal of Youth and Adolescence. 2011;40(1):59–71. doi: 10.1007/s10964-009-9500-2. [DOI] [PubMed] [Google Scholar]
- 41.Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103(2):302. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- 42.Dittmar H, Howard S. Thin-ideal internalization and social comparison tendency as moderators of media models’ impact on women’s body-focused anxiety. Journal of Social and Clinical Psychology. 2004;23(6):768–791. [Google Scholar]
- 43.Stice E, Bearman SK. Body-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: A growth curve analysis. Developmental Psychology. 2001;37(5):597. doi: 10.1037//0012-1649.37.5.597. [DOI] [PubMed] [Google Scholar]
- 44.Feragen KB, Kvalem IL, Rumsey N, Borge AIH. Adolescents with and without a facial difference: The role of friendships and social acceptance in perceptions of appearance and emotional resilience. Body Image. 2010;7(4):271–279. doi: 10.1016/j.bodyim.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 45.Strauss RP. “Only skin deep”: Health, resilience, and craniofacial care. Cleft Palate-Craniofacial Journal. 2001;38(3):226–230. doi: 10.1597/1545-1569_2001_038_0226_osdhra_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 46.Seid M. Barriers to care and primary care for vulnerable children with asthma. Pediatrics. 2008;122(5):994–1002. doi: 10.1542/peds.2007-3114. [DOI] [PubMed] [Google Scholar]
- 47.McPherson M, Weissman G, Strickland BB, van Dyck PC, Blumberg SJ, Newacheck PW. Implementing community-based systems of services for children and youths with special health care needs: How well are we doing? Pediatrics. 2004;113(5 Suppl):1538–1544. [PubMed] [Google Scholar]
- 48.US Department of Health and Human Services . Oral health in America: A report of the surgeon general. National Institute of Dental and Craniofacial Research; Rockville, MD: 2000. [Google Scholar]
- 49.Feragen KB, Stock NM, Kvalem IL. Risk and protective factors at age 16: Psychological adjustment in children with a cleft lip and/or palate. Cleft Palate-Craniofacial Journal. 2015;52(5):555–573. doi: 10.1597/14-063. [DOI] [PubMed] [Google Scholar]
- 50.Kirschner RE. President of the American Cleft Palate-Craniofacial Association. Jun, 2015. Personal communication with Dr. Broder. 2015. [DOI] [PubMed]
- 51.Masood M, Masood Y, Saub R, Newton JT. Need of minimal important difference for oral health-related quality of life measures. Journal of Public Health Dentistry. 2012;74(1):13–20. doi: 10.1111/j.1752-7325.2012.00374.x. [DOI] [PubMed] [Google Scholar]
- 52.Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Medical Care. 1999;37(5):469–478. doi: 10.1097/00005650-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 53.Strickland BB, Singh GK, Kogan MD, Mann MY, van Dyck PC, Newacheck PW. Access to the medical home: New findings from the 2005–2006 National Survey of Children with Special Health Care Needs. Pediatrics. 2009;123(6):e996–e1004. doi: 10.1542/peds.2008-2504. [DOI] [PubMed] [Google Scholar]
- 54.Wehby GL, Cassell CH. The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Diseases. 2010;16(1):3–10. doi: 10.1111/j.1601-0825.2009.01588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seid M, Opipari-Arrigan L, Gelhard LR, Varni JW, Driscoll K. Barriers to care questionnaire: Reliability, validity, and responsiveness to change among parents of children with asthma. Academic Pediatric. 2009;9(2):106–113. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]