Abstract
The purpose of this study was to investigate possible rapid effects of light therapy on depressed mood in patients with seasonal affective disorder. Participants received 1 hour of bright light therapy and 1 hour of placebo dim red light in a randomized order crossover design. Depressed mood was measured at baseline and after each hour of light treatment using two self-report depression scales (Profile of Mood States–Depression-Dejection [POMS-D] subscale and the Beck Depression Inventory II [BDI-II]). When light effects were grouped for the two sessions, there was significantly greater reduction in self-report depression scores by −1.3 (p = 0.02) on the BDI-II and −1.2 (p = 0.02) on the POMS-D. A significant but modest improvement was detected after a single active light session. This is the first study, to our knowledge, to document an immediate improvement with light treatment using a placebo-controlled design with a clinical sample of depressed individuals.
Keywords: Light therapy, seasonal affective disorder, depression
Seasonal affective disorder (SAD), winter type, is a condition in which individuals experience recurrent depression during the fall/winter months and spontaneous remission in the spring/summer months (Rosenthal et al., 1984). Common presenting symptoms are increased appetite with carbohydrate cravings, increased sleep, decreased energy, and marked decrease in activity. Light therapy is an effective treatment of SAD (Eastman et al., 1998; Lewy et al., 1998; Rosenthal et al., 1984; Terman et al., 1998), with effect sizes similar to those of antidepressant therapy (Golden et al., 2005).
Light therapy clinical research has largely focused on antidepressant effects after a course of daily light treatment. Growing evidence, however, suggests that immediate improvement in depressed mood may be detectable after a single light session. For instance, Sher et al. (2001) reported significant improvement of SAD scores on a semistructured interview after 1-hour light therapy in SAD patients; however, this study was conducted in an artificial setting (positron emission tomography scanner) and did not have a control condition. A follow-up study on the same data from Sher et al. (2001) identified immediate mood improvement after 20 minutes of light that plateaued after 40 minutes of light (Virk et al., 2009). Having a control intervention is essential because this immediate mood improvement may be the consequence of a placebo effect. To our knowledge, the only controlled study of immediate light treatment effects used a negative ion-generator placebo and reported mood improvement after 30 minutes of light therapy but was conducted in a nonclinical sample of mildly depressed and nondepressed adults (Goel and Etwaroo, 2006).
Early response to light treatment has important implications for both clinical care and understanding the pathophysiology models of SAD. Clinically, mood improvement in the very early phase of depression treatment may support treatment adherence and provide some relief during the time that patients are typically the most symptomatic (Nakajima et al., 2010).
Rapid response to light therapy may also provide insights about the etiology of SAD and mediators of treatment response. Prevailing chronobiology theories of SAD focus on photoperiod and circadian phase shift (Sohn and Lam, 2005). Wehr et al. (2001) demonstrated that patients with SAD, compared with healthy controls, have longer periods of nocturnal melatonin secretion during winter than during summer, similar to photoperiodic mammals. Within a photoperiodic framework, light therapy treatment may improve SAD symptoms by increasing the artificial photoperiod and compressing the nocturnal duration of melatonin secretion. The Circadian Shift model by Lewy et al. (1987) postulates that SAD symptoms are at least partly caused by a phase delay in internal circadian systems; seasonal changes in time of daylight cause a dysynchrony with the SAD individual’s sleep/wake cycle. Morning light therapy may treat SAD symptoms by providing a corrective phase advance of the sleep/wake cycle (Terman et al., 2001). This model is consistent with reports (Burgess et al., 2004; Lam, 1994) on observed effects of light. In summary, chronobiological models of light treatment involve corrective changes that occur over a sleep/wake cycle or course of treatment. Immediate mood improvement with light treatment would support an immediate “brain stimulating” effect of light therapy.
In this study, we obtained a self-report of mood before and after an initial light therapy session. All participants received 1 hour of light plus 1 hour of placebo dim red light in a randomized crossover design. Therefore, we assessed for rapid mood changes after a single controlled light session. Implications of possible rapid mood improvement on theories of SAD etiology are discussed.
METHODS
Participants were recruited through local advertisement. We included participants aged 18 to 65 years who had a diagnosis of current major depressive disorder with seasonal specifier. We excluded individuals with a psychotic or bipolar I disorder; current suicidality; vision problems not correctable by glasses; somatic conditions that had increased sensitivity to light; overnight shift work schedule; illicit substance use or alcohol abuse in the past year; and treatment with an antidepressant, mood stabilizer, or antipsychotic medication in the past 30 days. This study was conducted with institutional review board approval at University of Maryland.
Clinical Diagnosis
Diagnosis of SAD was confirmed by a) diagnosis of major depressive episode with seasonal specifier based on the Structured Clinical Interview for DSM-IV-TR Axis I Disorders Patient Edition with Psychotic Screen SCID–I/P; First et al., 2002) and b) a Seasonal Affective Disorder Version of the Hamilton Depression Rating Scale (SIGH SAD; Williams et al., 1992) score of 21 or greater. Interviews were conducted by trained nurse and physician research staff.
Eligibility for study participation was assessed at four time points. First, potential participants were screened by telephone using the Seasonal Pattern Assessment Questionnaire (SPAQ). This questionnaire has been widely used in epidemiological studies to assess the prevalence of SAD. Its SAD criterion has good test-retest reliability between 2 consecutive years (Christensen et al., 2003). Participants who had a “global seasonality score” higher than 11 and endorsed that seasonal changes were at least a “moderate problem” on the SPAQ were invited for a face-to-face interview. At this interview (screen 2), the diagnostic assessments for SAD were completed. Eligible participants had the SIGH SAD repeated by telephone interview 24 hours before the first scheduled light session (screen 3) and on the morning of the first light session (screen 4). The participants needed to maintain a SIGH SAD score of 21 or greater to be eligible for participation. The SIGH SAD was repeated three times over this screening period to verify that the participant had persistent symptoms consistent with a SAD episode and not a brief 1- to 2-day fluctuation in mood. This screening process was typically completed over a 1- to 2-week period of time.
Light Session
The initial light treatment session was administered under observation at the General Clinical Research Center of the University of Maryland, starting not earlier than 11 a.m. Each participant received 2 hours of light on this first session. The 2 hours of light included 1 hour of bright white light and 1 hour of dim red placebo light administered in randomized crossover order. We used a standard light therapy unit Brite LITE 6 light box (Apollo, Salt Lake City, UT; dimensions, 7.1 × 11 × 17.4 inches/18 × 28 × 44 cm) that emits 10,000 of lux light to the eye when the user is within 24 inches of the box. The placebo light consisted of an identical structure with a red screen that will produce a dim red luminance of 50 lux at the level of the eye. The dim red light placebo has an identical appearance except for a red screen on top of the diffuser, which delivers a red light with maximum 50 lux at 24 inches. A light meter was used to confirm luminosity at the level of the eye for each participant. A photometric analysis of the two light boxes confirmed that the bright light had a total illuminance of 10,050 lux at 24 inches and a peak wavelength of 545 nm (but with several peaks across the spectrum). The placebo red light total illuminance was 42 lux, with a peak wavelength of 612 nm. A treatment expectation survey was completed at 5 minutes during each light condition. This survey asked individuals to rate on a scale of 1 to 10 how effective they believed this light would be for their symptoms of seasonal depression.
Self-report of depression was assessed using the Beck Depression Inventory II (BDI-II; Beck et al., 1996b) and the Profile of Mood States–Depression-Dejection subscale (POMS-D; McNair et al., 1971) at three time points: at baseline, after light session #1, and after light session #2. Each patient received 1 hour of bright light and 1 hour of dim red light (placebo) in randomized order.
Beck Depression Inventory-Second Edition
BDI-II is an updated version of the amended BDI I. It is a 21-item self-report measure. Participants rate items on a scale of 0 to 3 based on how they have been feeling in the last 2 weeks, and the score is the total of these items. The BDI-II has high level of internal consistency (coefficient α = 0.91; Beck et al., 1996a). The BDI-II has been demonstrated to yield reliable, internally consistent, and valid scores in a primary care setting (Arnau et al., 2001). Although the BDI-II was administered three times in a single day, the participants were instructed every time to report on “the past two weeks, including today.”
Profile of Mood States–Depression-Dejection Subscale
The POMS was developed to detect transient mood states. The POMS-D subscale is a self-report measure in which participants rate how much they are feeling the following 15 emotions at this moment: unhappy, sorry for things done, sad, blue, hopeless, unworthy, discouraged, lonely, miserable, gloomy, desperate, helpless, worthless, terrified, and guilty. Participants rate their response of on a scale of 0 to 4, where 0 is “not at all like me” and 4 is “exactly like me.”
Statistical Methods
After the inspection of distributions of the mood score for outliers and approximate normality, descriptive methods for comparisons of demographic characteristics and baseline scores used chi-square tests for categorical variables and t-tests for continuous variables. t-tests were also used to compare bright and red light groups on mean changes in mood scores across each of the 1-hour light sessions. Mood score trajectories were plotted by order of light exposures. A mixed-model crossover analysis was used to control for within-subject correlation and to assess whether the light effect differed by order of light exposure. This was accomplished by including an interaction of light group by order of light administration. If the interaction was not significant, the interaction was removed, and only the light group and order were included in the model, along with any important covariates. All analyses were conducted using SAS version 9.1.
RESULTS
There were 925 participants screened by telephone, and 233 participants attended a face-to-face diagnostic evaluation. A total of 79 participants were eligible after all four screening assessments, and all of these participants received the 2-hour light session. There were 41 participants randomized to receive bright light first, and the remaining 38 received bright light during the second hour. Table 1 summarizes the baseline characteristics of the participants. No significant differences were observed between groups for age, sex, or race distributions. Baseline mood scores differed only for POMS-D, where those randomized to bright light first had significantly lower scores than those randomized to dim red light first (p = 0.04). Figure 1 presents BDI-II mood score trajectories by order of light exposure. Both plots display somewhat similar patterns where after the first hour, mood scores decreased significantly, with bright light decreasing somewhat more than red light (Table 2). Differences within the first hour were not significant.
TABLE 1.
Demographic and Baseline Characteristics of the Participants
| Variable | Bright First (n = 41) |
Red First (n = 38) |
pa | ||
|---|---|---|---|---|---|
| Age, mean (SD), yrs | 44.0 | (10.6) | 45.2 | (10.0) | 0.59 |
| Sex: male, n (%) | 24 | (58.5) | 22 | (57.9) | 0.95 |
| Race, n (%) | |||||
| White | 13 | (31.7) | 14 | (36.8) | 0.27 |
| African-American | 28 | (68.3) | 22 | (57.9) | |
| Other | 0 | (0) | 2 | (5.3) | |
| Baseline measures, mean (SD) | |||||
| BDI | 23.1 | (9.0) | 26.2 | (11.0) | 0.18 |
| POMS-D | 15.4 | (13.2) | 22.0 | (14.8) | 0.04 |
BDI indicates Beck Depression Inventory; POMS-D, Profile of Mood States–Depression-Dejection subscale.
p values from t-test or chi-square analyses.
FIGURE 1.
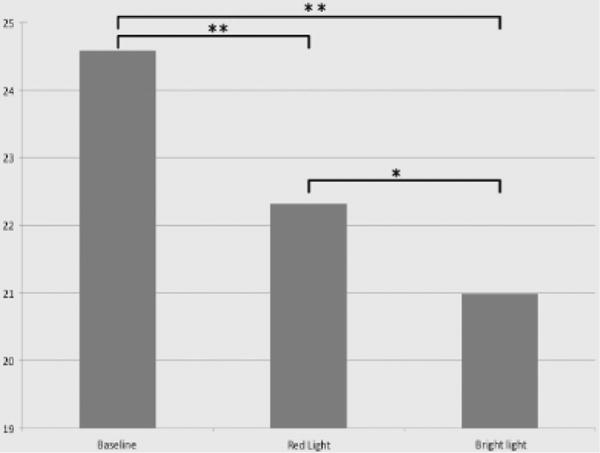
*BDI-II scores were significantly lower after treatment with bright light compared with red light (p ≤ 0.05).;
**BDI-II scores were significantly lower after 1 hour of treatment with both red and bright lights (p ≤ 0.01). BDI-II indicates Beck Depression Inventory-II.
TABLE 2.
Comparisons of Bright and Red Lights on Mean Changes Across 1 Hour by Period of Exposure
| Mean Changes Over 1 Hr
|
||||
|---|---|---|---|---|
| First Period
|
Second Period
|
|||
| Mean (SE) | pa | Mean (SE) | pa | |
| BDI | ||||
| Bright light | −2.78 (0.80) | 0.54 | −2.40 (1.05) | 0.02 |
| Red light | −2.08 (0.82) | 0.34 (0.46) | ||
| POMS-D | ||||
| Bright light | −2.68 (1.05) | 0.95 | −3.37 (1.04) | 0.02 |
| Red light | −2.58 (1.26) | −0.37 (0.78) | ||
BDI indicates Beck Depression Inventory; POMS-D, Profile of Mood States–Depression-Dejection subscale.
p values from t-tests.
For the BDI-II scale, the crossover analysis revealed a borderline interaction effect (p = 0.07); during the first hour, the difference between bright and red light exposure groups was not significant (p = 0.66); however, during the second hour, bright light has a significantly greater decline with a difference of −2.4 (p = 0.004). The patients’ expectations of effects, age, sex, and race were all nonsignificant and were not included in models; all models were adjusted for baseline score. When the interaction effect was removed from the model and the light effects were pooled over the two periods, bright light showed significantly greater decline than red light with a difference of −1.3 (p = 0.02).
For POMS-D, the interaction of order with light type was highly significant (p = 0.005), such that there was no significant difference between bright and red lights during the first period, but a highly significant difference in decline in score of −3.4 (p = 0.0005) during the second hour.
DISCUSSION
This study investigated whether rapid depression improvement can be detected after light treatment in SAD patients. Patients received 1 hour of bright light and 1 hour of placebo red light in randomized order. For both the first and second light sessions, the improvement of depression scores was greater for bright light than placebo but these differences were only significant for the second hour; in the second session, bright light outperformed the placebo in terms of improvement in both BDI-II and POMS-D. For participants who received bright light first, BDI-II scores did not continue to improve after the subsequent placebo light session. The interaction of order with light type, which was significant for the POMS-D assessment and borderline significant for BDI-II suggests a limitation of the placebo design. One possible explanation is that the participants had greater improvement after placebo light if they had not yet been exposed to active treatment. Participants who received the placebo light first continued to have significant improvement of depression scores after receiving the active treatment, with the greatest improvement detected by the POMS-D (−3.37; p = 0.02).
When light effects were grouped for the two sessions, there was significantly greater reduction in self-report depression scores by −1.3 (p = 0.02) on the BDI-II and −1.2 (p = 0.02) on the POMS-D. Therefore, a modest but rapid mood improvement was detected after a single active light session. Recent literature on antidepressant medication treatment indicates that early antidepressant effect is not solely caused by a short-lived placebo response. Uher et al. (2010) reported that rapid improvement trajectories persisted after 12 weeks of antidepressant treatment. Accordingly, some depression treatment guidelines have designated early symptom reduction thresholds to classify adequate treatment response after just 2 to 4 weeks (Lam, 2010).
An interesting finding is that the clinical self-report depression measure (BDI-II), which is designed to detect mood changes for 2 weeks, had similar results to the POMS-D, a self-report measure that detects transient mood changes. During the 2-hour light session, the participants were asked three times (baseline, hour 1, and hour 2) to report on their depression symptoms during the past 2 weeks. Whereas the POMS-D only assesses feeling states, the BDI-II has items that would not be able to change in a 2-hour time frame (e.g., “I sleep somewhat more than usual,” and “I am too tired or fatigued to do most of the things I used to do.”). The change in BDI-II scores during a 2-hour period suggest that the current mood state may effect how we perceive the past 2 weeks, even if there has not been a long enough time for there to be a change in functioning. The similar pattern of responses for the BDI-II and the POMS-D is promising in that the BDI-II is commonly used in both primary care and mental health settings, so it would be easy to adopt in clinical settings to assess early mood changes.
The model of assessing mood symptoms at baseline and after one monitored light session is adaptable and useful in an outpatient clinical setting. Patients who perceive some improvement may be more likely to adhere to ongoing treatment. Nonadherence to depression treatment is a major public health concern. A study of antidepressant medication adherence reported that 42% of patients discontinued their antidepressant treatment within the first 30 days, the time frame during which full remission has not usually been achieved (Olfson et al., 2006). Furthermore, an estimated 25% of patients do not inform their prescriber that they have stopped the medication (Demyttenaere, 2003). A pilot study on light therapy adherence reported a similar nonadherence rate to antidepressant medication studies (Michalak et al., 2007).
More importantly, any immediate mood improvement can help alleviate hopelessness in patients dealing with depression. Even if modest, this early improvement may also impact patient views of light treatment. Bultman and Svarstad (2000) report that positive client initial beliefs about antidepressant medication predicts client satisfaction with medication at 2 months. Furthermore, client satisfaction and physician communication style explained more than 20% of variation in medication omissions. In one survey of individuals prescribed antidepressant medication, 12% of those who discontinued their medication within the first 3 months reported “no improvement” as the reason for discontinuation (Bull et al., 2002). Although a very small change in depression score rating after a single session may not be perceived by the patient as significant, it is possible that this feedback may positively influence initial views of light therapy, which in turn have potential to influence adherence.
The evidence of mood improvement after an initial light therapy treatment raises considerations about underlying the psychopathology of SAD. Early phase of mood changes may be mediated by neurotransmitter changes. Serotonin has been implicated in the pathophysiology of both seasonal and nonseasonal depression. Healthy women with a positive family history of depression and a presence of a specific serotonin transporter gene polymorphism were more likely to experience mood worsening during acute tryptophan depletion than were women without these characteristics (Neumeister et al., 2002). Serotonin levels may also be affected by light exposure. Lambert et al. (2002) reported that invasively measured serotonin turnover in healthy adults was lowest in the winter and that brain production of serotonin increased rapidly as luminosity increased. Serotonin turnover corresponded greater with luminosity that day, rather than with averaged luminosity over recent days.
There has also been growing attention on the possible role of dopamine in seasonal depression and early antidepressant effects of depression treatment. Levitan et al. (2004) has reported an association between the dopamine-4 receptor and binge eating and weight gain in women with seasonal depression. Catecholamine depletion in patients who have achieved remission of SAD with light therapy has also been demonstrated to induce significant worsening of depression symptoms comparable with tryptophan depletion and worse than a sham depletion procedure (Neumeister et al., 1998). The possible role of dopamine in rapid mood improvement is supported by pharmacological research on the antidepressant effects of stimulant medication. Stimulant medications are thought to exert therapeutic effects at least in part by blocking the reuptake of dopamine into the presynaptic neuron (Wilens, 2006). These medications are used in treatment refractory depression to augment antidepressant medications and have also been used in the depression treatment of medically frail patients where there may be advantage over traditional antidepressant medications of less drug interactions and no physical withdrawal if stopped abruptly. A review by Orr and Taylor (2007) on stimulant treatment of depression reported more rapid improvement than traditional antidepressants, with some open label studies reporting approximately one third of patients experiencing moderated to marked depression improvement on the first day of treatment. Furthermore, one study of an intravenous administered stimulant reported mood improvement after 60 minutes. Dopamine agents have been theorized to also impact quality of life by the effects of inhibiting dopamine reuptake on pleasure responsivity (IsHak et al., 2009).
The results of this study are interpreted with awareness of limitation of crossover study design. There are possible carryover effects of the individual treatments. In addition, significant differences between the groups were observed at baseline in POMS-D, one of the outcome measures. However, these differences were adjusted and not paralleled by BDI-II scores. In addition, our sample differs from what is known about the SAD population with regard to an increased male proportion, probably, in response to our recruitment methodology. Participants were largely recruited from print advertisements rather than from clinical treatment programs. There were no differences in sex distribution between the two light-sequence groups. A strength of the study is that it confirms the previous reports of a rapid mood improving effect of bright light, using for the first time a controlled paradigm in a clinical setting, with unmedicated patients who were not treated with bright light before.
CONCLUSIONS
Traditional depression outcomes have focused on assessment of remission over a course of treatment, that is, delayed response to intervention. However, an assessment of rapid mood changes is important for both clinical care and understanding the underlying psychobiology of depression. In this study, we have demonstrated a modest improvement of SAD depression symptoms after a single light session. Rapid mood improvement with bright light suggests complex efficacy, probably by immediately stimulating major neurotransmitter systems involved in mood regulation, in addition to longer term chronobiological effects.
Acknowledgments
The authors thank the individuals who participated in this study. They also thank Dr. Leonardo Tonelli for logistical support; Ms. Christine Ballwanz, Mr. Neal Gallico, and Mr. Francis Iyoriobhe for administrative support; and Dr. Alvaro Guzman, Ms. Mei Kwan, and Ms. Natasha Dzhanashvili for their assistance with study visits. Finally, they thank Dr. Farooq Mohyuddin for his support of trainee involvement in clinical research.
This work was supported by the University of Maryland General Clinical Research Center Grant M01 RR016500, General Clinical Research Centers Program, National Center for Research Resources (NCRR) NIH. Dr. Reeves received support from NIH 1K12RR023250-01. Drs. Postolache, Snitker, Langenberg, and Johnson received support from NIMH 1R34MH073797-01A2. Seed funds for Dr. Postolache/Mood and Anxiety Program (MAP) were from the University of Maryland School of Medicine/Department of Psychiatry and the St. Elizabeths Hospital Psychiatry Residency Training. The results were presented at the Annual Meeting of the Society for Biological Psychiatry, New Orleans, 2010.
Footnotes
DISCLOSURE
The authors have nothing to disclose.
References
- Arnau RC, Meagher MW, Norris MP, Bramson R. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 2001;20:112–119. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996a;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory II (BDI-II) San Antonio, TX: The Psychological Corporation; 1996b. [Google Scholar]
- Bull SA, Hunkeler EM, Lee JY, Rowland CR, Williamson TE, Schwab JR, Hurt SW. Discontinuing or switching selective serotonin-reuptake inhibitors. Ann Pharmacother. 2002;36:578–584. doi: 10.1345/aph.1A254. [DOI] [PubMed] [Google Scholar]
- Bultman DC, Svarstad BL. Effects of physician communication style on client medication beliefs and adherence with antidepressant treatment. Patient Educ Couns. 2000;40:173–185. doi: 10.1016/s0738-3991(99)00083-x. [DOI] [PubMed] [Google Scholar]
- Burgess HJ, Fogg LF, Young MA, Eastman CI. Bright light therapy for winter depression–is phase advancing beneficial? Chronobiol Int. 2004;21:759–775. doi: 10.1081/cbi-200025979. [DOI] [PubMed] [Google Scholar]
- Christensen EM, Larsen JK, Gjerris A. The stability of the seasonal pattern assessment questionnaire score index over time and the validity compared to classification according to DSM IIIR. J Affect Disord. 2003;74:167–172. doi: 10.1016/s0165-0327(02)00009-5. [DOI] [PubMed] [Google Scholar]
- Demyttenaere K. Risk factors and predictors of compliance in depression. Eur Neuropsychopharmacol. 2003;13:S69–S75. doi: 10.1016/s0924-977x(03)00095-6. [DOI] [PubMed] [Google Scholar]
- Eastman CI, Young MA, Fogg LF, Liu L, Meaden PM. Bright light treatment of winter depression: a placebo controlled trial. Arch Gen Psychiatry. 1998;55:883–889. doi: 10.1001/archpsyc.55.10.883. [DOI] [PubMed] [Google Scholar]
- First MD, Spitzer RL, Miriam G, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Patient Edition with Psychotic Screen-Revised. New York: Biometrics Research, New York State Psychiatric Institute; 2007. [Google Scholar]
- Goel N, Etwaroo GR. Bright light, negative ions, and auditory stimuli produce rapid mood changes in a student population: a placebo-controlled study. Psychol Med. 2006;36:1253–1263. doi: 10.1017/S0033291706008002. [DOI] [PubMed] [Google Scholar]
- Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, Wisner KL, Nemeroff CB. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162:656–662. doi: 10.1176/appi.ajp.162.4.656. [DOI] [PubMed] [Google Scholar]
- IsHak WW, Davis M, Jeffrey J, Balayan K, Pechnick RN, Bagot K, Rapaport MH. The role of dopaminergic agents in improving quality of life in major depressive disorder. Curr Psychiatry Rep. 2009;11:503–508. doi: 10.1007/s11920-009-0076-z. [DOI] [PubMed] [Google Scholar]
- Lam RW. Morning light therapy for winter depression: predictors of response. Acta Psychiatr Scand. 1994;89:97–101. doi: 10.1111/j.1600-0447.1994.tb01494.x. [DOI] [PubMed] [Google Scholar]
- Lam RW. The importance of early symptom relief in antidepressant treatment: focus on agomelatine. J Psychopharmacol. 2010;24:27–30. doi: 10.1177/1359786810372979. [DOI] [PubMed] [Google Scholar]
- Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD. Effect of sunlight and season on serotonin turnover in the brain. Lancet. 2002;360:1840–1842. doi: 10.1016/s0140-6736(02)11737-5. [DOI] [PubMed] [Google Scholar]
- Levitan RD, Masellis M, Basile VS, Lam RW, Kaplan AS, Davis C, Muglia P, Mackenzie B, Tharmalingam S, Kennedy SH, Macciardi F, Kennedy JL. The dopamine-4 receptor gene associated with binge eating and weight gain in women with seasonal affective disorder: an evolutionary perspective. Biol Psychiatry. 2004;56:665–669. doi: 10.1016/j.biopsych.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Lewy AJ, Bauer VK, Cutler NL, Sack RL, Ahmed S, Thomas KH, Blood ML, Jackson JM. Morning vs evening light treatment of patients with winter depression. Arch Gen Psychiatry. 1998;55:890–896. doi: 10.1001/archpsyc.55.10.890. [DOI] [PubMed] [Google Scholar]
- Lewy AJ, Sack RL, Miller LS, Hoban TM. Antidepressant and circadian phase-shifting effects of light. Science. 1987;235:352–354. doi: 10.1126/science.3798117. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Manual for the Profile of mood states. San Diego, CA: Educ Industr Testing Serv; 1971. [Google Scholar]
- Michalak EE, Murray G, Wilkinson C, Dowrick C, Lam RW. A pilot study of adherence with light treatment for seasonal affective disorder. Psychiatry Res. 2007;149:315–320. doi: 10.1016/j.psychres.2006.05.005. [DOI] [PubMed] [Google Scholar]
- Nakajima S, Suzuki T, Watanabe K, Kashima H, Uchida H. Accelerating response to antidepressant treatment in depression: a review and clinical suggestions. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:259–264. doi: 10.1016/j.pnpbp.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Konstantinidis A, Stastny J, Schwarz MJ, Vitouch O, Willeit M, Praschak-Rieder N, Zach J, de Zwaan M, Bondy B, Ackenheil M, Kasper S. Association between serotonin transporter gene promoter polymorphism (5HTTLPR) and behavioral responses to tryptophan depletion in healthy women with and without family history of depression. Arch Gen Psychiatry. 2002;59:613–620. doi: 10.1001/archpsyc.59.7.613. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Turner EH, Matthews JR, Postolache TT, Barnett RL, Rauh M, Vetticad RG, Kasper S, Rosenthal NE. Effects of tryptophan depletion vs catecholamine depletion in patients with seasonal affective disorder in remission with light therapy. Arch Gen Psychiatry. 1998;55:524–530. doi: 10.1001/archpsyc.55.6.524. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Tedeschi M, Wan GJ. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163:101–108. doi: 10.1176/appi.ajp.163.1.101. [DOI] [PubMed] [Google Scholar]
- Orr K, Taylor D. Psychostimulants in the treatment of depression : a review of the evidence. CNS Drugs. 2007;21:239–257. doi: 10.2165/00023210-200721030-00004. [DOI] [PubMed] [Google Scholar]
- Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y, Mueller PS, Newsome DA, Wehr TA. Seasonal Affective Disorder: A description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry. 1984;41:72–80. doi: 10.1001/archpsyc.1984.01790120076010. [DOI] [PubMed] [Google Scholar]
- Sher L, Matthews JR, Turner EH, Postolache TT, Katz KS, Rosenthal NE. Early response to light therapy partially predicts long-term antidepressant effects in patients with seasonal affective disorder. J Psychiatry Neurosci. 2001;26:336–338. [PMC free article] [PubMed] [Google Scholar]
- Sohn CH, Lam RW. Update on the biology of seasonal affective disorder. CNS Spectr. 2005;10:635–646. doi: 10.1017/s109285290001960x. [DOI] [PubMed] [Google Scholar]
- Terman JS, Terman M, Lo ES, Cooper TB. Circadian time of morning light administration and therapeutic response in winter depression. Arch Gen Psychiatry. 2001;58:69–75. doi: 10.1001/archpsyc.58.1.69. [DOI] [PubMed] [Google Scholar]
- Terman M, Terman JS, Ross DC. A controlled trial of timed bright light and negative air ionization for treatment of winter depression. Arch Gen Psychiatry. 1998;55:875–882. doi: 10.1001/archpsyc.55.10.875. [DOI] [PubMed] [Google Scholar]
- Uher R, Muthén B, Souery D, Mors O, Jaracz J, Placentino A, Petrovic A, Zobel A, Henigsberg N, Rietschel M, Aitchison KJ, Farmer A, McGuffin P. Trajectories of change in depression severity during treatment with antidepressants. Psychol Med. 2010;40:1367–1377. doi: 10.1017/S0033291709991528. [DOI] [PubMed] [Google Scholar]
- Virk G, Reeves G, Rosenthal NE, Sher L, Postolache TT. Short exposure to light treatment improves depression scores in patients with seasonal affective disorder: A brief report. Int J Disabil Hum Dev. 2009;8:283–286. doi: 10.1901/jaba.2009.8-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehr TA, Duncan WC, Jr, Sher L, Aeschbach D, Schwartz PJ, Turner EH, Postolache TT, Rosenthal NE. A circadian signal of change of season in patients with seasonal affective disorder. Arch Gen Psychiatry. 2001;58:1108–1114. doi: 10.1001/archpsyc.58.12.1108. [DOI] [PubMed] [Google Scholar]
- Wilens TE. Mechanism of action of agents used in attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67:32–38. [PubMed] [Google Scholar]
- Williams JB, Link MJ, Rosenthal NE, Amira L, Terman M. Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD) New York: New York State Psychiatric Institute; 1992. [Google Scholar]


