Abstract
Background
Thyroid incidentalomas (TI) are highly prevalent asymptomatic thyroid nodules with ultrasound as the best imaging modality for their detection and characterization. Although they are mostly benign, potential for malignancy is up to 10–15%.
In sub-Saharan Africa little data exists on the prevalence and risk categorization of TI. The aim of this study was to determine the prevalence and ultrasound characteristics of non-palpable thyroid incidentalomas among adults in sub-Saharan setting.
Methods
A cross sectional study was carried out between March and August 2015, at two university teaching hospitals. Sampling was consecutive and included all adults aged ≥ 16 years, presenting for any ultrasound other than for the thyroid, with no history or clinical signs of thyroid disease, and no palpable thyroid lesion. Ultrasound was done using 4 to 11 MHz linear probes. Subjects with diffuse thyroid abnormalities were excluded. Variables studied were age, gender, thyroid volume, ultrasound characteristics of thyroid nodules, TIRADS scores. Differences were considered statistically significant for p-value < 0.05.
Results
The prevalence of TI was 28.3% (126 persons with TI /446 examined). This prevalence was 46.2% in population ≥ 61-year-old; 6.3% in population ≤ 20-year-old; 33.3% for females and 18.4% for males (p < 0.001). Of the 241 TI found, 49.4% were cysts, 33.6% solid, 17.0% mixed; 37.8% <5 mm and 22% >10 mm. Solid TI were mainly hyperechoic (42.0%), 3/81 were markedly hypoechoic. Sixty-nine out of 126 persons with TI (54.8%) had at least two nodules. Solitary nodules were predominant in the age group ≤20 years. Of 241 TI, 129 (53.5%) were classified TIRADS 2, 81 (33.6%) TIRADS 3, 25 (10.4%) TIRADS 4A, 6 (2.5%) TIRADS 4B, and none TIRADS 5. Characteristics associated with increased risk of malignancy where mostly founded on solid nodules (p < 0.000) and nodules larger than 15 mm (p < 0.001).
Conclusion
Thyroid incidentalomas were very frequent with a prevalence of 28.3% and potential risk of malignancy in 12.9%. Prevalence had a tendency to increase with age and in female. Cystic nodules were the most prevalent. Potential for malignancy would be increased for larger and solid nodules.
Keywords: Thyroid incidentaloma, Thyroid nodule, TIRADS, Prevalence, Sub-Saharan country
Background
Thyroid incidentalomas (TIs) are asymptomatic nodules discovered accidentally during imaging studies indicated for other reasons [1]. Ultrasound is the best imaging modality for the detection and characterization of these nodules [2, 3]. Various studies have reported a prevalence between 50 and 67% [2, 4–7]. They are mostly benign. However, there is a potential for malignancy in less than 10–15% [1, 2, 8], depending on the method of sampling and the characteristics of nodules.
TIs therefore represent a clinical challenge and a source of anxiety to patients. The clinician needs to correctly access the risk of each nodule, in order to correctly determine if and what further investigation is necessary. The TIRADS (Thyroid Imaging Reporting and Data System) permits this classification with recommendations on the need for cytologic verification or ultrasound surveillance [6, 7, 9, 10].
In sub-Saharan Africa little data exists on the prevalence and risk categorization of TI [11]. The aim of this study was therefore, to determine their prevalence in the adult population, and describe their ultrasound characteristics based on TIRADS.
Methods
A cross-sectional study was carried out in two university teaching hospitals from March to August 2015.
Study population
Persons aged ≥ 16 years, referred to the diagnostic imaging department for ultrasound scans other than that of the thyroid, who accepted freely to participate in the study were included. They had no history, palpable or other clinical signs of thyroid disease. A consecutive non-probabilistic sample was taken. Patients with diffuse thyroid disease were excluded. Verbal informed consent from participants was required.
Thyroid ultrasound procedure and image interpretation
The ultrasound was done free of charge using the routine procedure [12], with linear probes of 4–11 MHz frequency. The machines used were Prosound alpha 6 (Hitachi Medical Europe, France) 2015 and SSI-8000 (Sonoscape Co Ltd, China) 2013. Images were stored in the hard drive of each machine. An initial interpretation was done by the operator during the course of the scan. A second reading was done later by the operator and two radiologists with at least five years’ experience in thyroid sonography. Nodules were classified by consensus according to TIRADS (Table 1), as proposed by Russ and al [9, 13].
Table 1.
| TIRADS | Signification | Ultrasonographic characteristics | Malignancy risk (%) |
|---|---|---|---|
| TIRADS 1 | Normal thyroid | ▪ Normal thyroid US | - |
| TIRADS 2 | Benign aspects | ▪ Simple cyst ▪ Spongiform nodule ▪ ‘White knight’ aspect ▪ Isolated macrocalcification ▪ Typical sub-acute thyroiditis |
0.0 |
| TIRADS 3 | Probably benign aspects | ▪ None of the high suspicious aspect ▪ Isoechogenic ▪ Hyperechogenic |
0.25 |
| TIRADS 4A | Low suspicious aspect | ▪ None of the high suspicious aspect ▪ Moderately hypoechogenic |
6.0 |
| TIRADS 4B | High suspicious aspects with 1 or 2 signs and no adenopathy | ▪ Taller-than-wide shape ▪ Irregular or microlobulated margins ▪ Microcalcifications ▪ Marked hypoechogenicity |
69.0 |
| TIRADS 5 | High suspicious aspects with ≥ 3 signs and/or adenopathy | ▪ Taller-than-wide shape ▪ Irregular or microlobulated margins ▪ Microcalcifications ▪ Marked hypoechogenicity |
100 |
A preconceived data collection form was filled out for each subject. Variables studied included: age, gender, thyroid volume, ultrasound characteristics of any nodules found (echogenicity, calcifications, borders, height/breadth in transverse plane), and TIRADS score for each TI. The CSPro 5.1 software was used to create the data entry mask anonymously. Stata version 11 and SPSS version 18 software enabled the analysis of the data. The chi square test assessed the association between the TIRADS score and various socio-demographic and sonographic characteristics. The comparison of the prevalences were performed using the Fisher exact test. Results were expressed in numbers and percentages for categorical variables. Differences were considered statistically significant for p < 0.05.
Results
Four hundred and forty six subjects aged 16 to 89 were included, with 294 females (65.9%; sex ratio F/H = 1.9). The most frequent age groups was 21–40 years with 48.7% (Table 2).
Table 2.
Prevalence of thyroid incidentalomas (TIs) with respect to age and gender
| TIs | Female | Male | Total | |||
|---|---|---|---|---|---|---|
| Age (years) | Population | n (%) | Population | n (%) | Population | n (%) |
| ≤20 | 13 | 1 (7.7) | 3 | 0 (0.0) | 16 | 1 (6.3) |
| 21–40 | 163 | 35 (21.5) | 54 | 2 (3.7) | 217 | 37 (17.1) |
| 41–60 | 90 | 43 (47.8) | 71 | 21 (29.6) | 161 | 64 (39.8) |
| ≥ 61 | 28 | 19 (67.9) | 24 | 5 (20.8) | 52 | 24 (46.2) |
| Total | 294 | 98 (33.3) | 152 | 28 (18.4) | 446 | 126 (28.3) |
(p < 0.001)
Of the 446 individuals included, 126 had thyroid incidentalomas giving a prevalence of TIs of 28.3%. This prevalence was 33.3% among women (p < 0.001) and 46.6% in individuals aged more than 60 years (Table 2).
Characteristics of incidentalomas
The 126 subjects with TI cumulated a total of 241 TIs with 69 individuals (54.8%) having two or more TI (Fig. 1). Multiple TI was found in 57.2% of females and 42.2% of males.
Fig. 1.
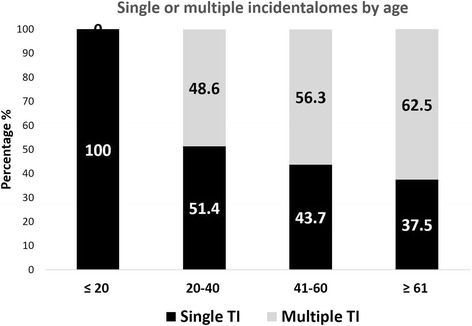
Distribution of multiple incidentalomas according to age
The location of TI was 54.0% (130/241) in the right lobe and 3.7% in the isthmus (9 cases). Most were inferiorly (base) located 38.2% (92/241), followed by location within the corpus (31.1%).
Of the 241 TIs, cystic nodules accounted for 49.4%; solid nodules for 33.6%; mixed (cystic and solid) for 17.0%. According to size 37.8% TIs were <5 mm and 22% >10 mm (Table 3).
Table 3.
Distribution of incidentalomas with respect to size and tissue structure
| Thyroid incidentalomas | Cystic | Solid | Mixed | Total |
|---|---|---|---|---|
| Largest diameter | n (%) | n (%) | n (%) | n (%) |
| < 5 mm | 67 (73.6) | 11 (12.1) | 13 (14.3) | 91 (37.8) |
| 5–9 | 41 (42.3) | 36 (37.1) | 20 (20.6) | 97 (40.3) |
| 10–14 | 8 (22.9) | 23 (65.7) | 4 (11.4) | 35 (14.5) |
| ≥ 15 | 3 (16.7) | 11 (61.1) | 4 (22.2) | 18 (7.5) |
| Total | 119 (49.4) | 81 (33.6) | 41 (17.0) | 241 (100) |
In regard to solid nodules (81/241), 42.0% were hyperechoic, 29.6% isoechoic, 24.7% with moderate hypoechogenicity and 3.7% were markedly hypoechoic. 39 solid TIs had a peripheral hypoechoic ring.
Solid and mixed incidentalomas had well defined borders in 91.0% of cases; ten nodules (8.2%) had indistinct borders. Eight nodules had macrocalcifications, two had microcalcifications. Half of them did not show any form of vascularization on Doppler examination (pulse and power). Peripheral vascularization was seen in 39.3% of cases (48/122). Only one nodule presented predominantly central vascularization.
TIRADS classification of TIs
Of 241 TIs, 129 (53.5%) were classified TIRADS 2 (Fig. 2), 81 (33.6%) TIRADS 3 (Fig. 3), 25 (10.4%) TIRADS 4A, 6 (2.5%) TIRADS 4B (Fig. 4), and none TIRADS 5.
Fig. 2.
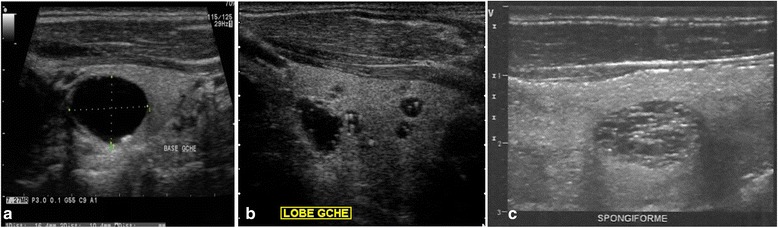
TIRADS 2 thyroid incidentalomas. Anechoic cyst with small parietal calcification (a). Colloid cysts of the left lobe (b) cystic formations containing hyperechoic pits with comet tail artefacts characteristic of colloid granulations (b). Spongiform nodule of the right lobe (c)
Fig. 3.
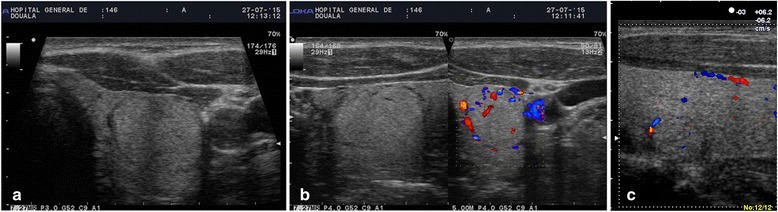
TIRADS 3 thyroid incidentalomas. Hyperechoic nodule with sharp margins, peripheral hypoechoic halo and peripheral vascularization on the left lobe (a, b). Isoechogenic nodule with peripheral hypoechoic halo and peripheral vascularization (c)
Fig. 4.
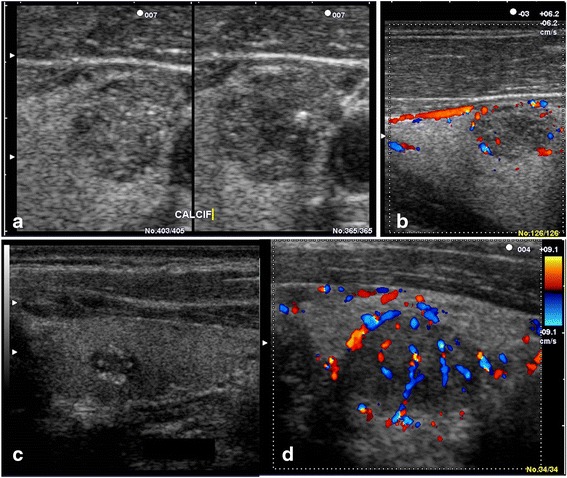
TIRADS 4 incidentalomas. TIRADS 4A: a moderately hypoechoic solid nodule of sharp margins (a) with peripheral vascularization (b). TIRADS 4B: hypoechoic nodule with microcalcifications (c) and marked hypoechoic nodule with mixed vascularization (d)
Of the 31 TIRADS 4 thyroid incidentalomas, 77.4% were solid and 22.6% mixed (p < 0.000). None was cystic (Table 4); 14.3% of TIRADS 4 nodules were 10–15 mm, 22% were > 15 mm.
Table 4.
TIRADS classification of thyroid incidentalomas with respect to tissue structure
| Thyroid incidentalomas | Cystic | Solid | Mixed | Total |
|---|---|---|---|---|
| Classification | n (%) | n (%) | n (%) | n (%) |
| TIRADS 2 | 116 (48.1) | 1 (0.4) | 12 (5.0) | 129 (53.5) |
| TIRADS 3 | 3 (1.3) | 56 (23.2) | 22 (9.1) | 81 (33.6) |
| TIRADS 4A | 0 (0.0) | 20 (8.3) | 5 (2.1) | 25 (10.4) |
| TIRADS 4B | 0 (0.0) | 4 (1.7) | 2 (0.8) | 6 (2.5) |
| Total | 119 (49.4) | 81 (33.6) | 41 (17.0) | 241 (100.0) |
(p < 0.001)
There was no significantly strong association between age, gender and TIRADS score. Prevalence of potentially malignant nodules (TIRADS 4) increased with size (p < 0.001): Table 5.
Table 5.
Prevalence of TIRADS 4 thyroid incidentalomas with respect to size
| Size | < 5 mm | 5–9 mm | 10–15 mm | >15 mm | Total |
|---|---|---|---|---|---|
| n (TIRADS 2, 3 and 4) | 91 | 97 | 35 | 18 | 241 |
| TIRADS 4A | 8 | 11 | 3 | 3 | 25 |
| TIRADS 4B | 1 | 2 | 2 | 1 | 6 |
| Malignant potential (4A + 4B) | 9.9% | 13.4% | 14.3% | 22.2% | 12.9% |
(P < 0.001)
Discussion
The aim of this study was to determine the prevalence and ultrasound characteristics of thyroid incidentalomas, amongst adult in a hospital based setting. The prevalence of TIs was 28.3% with 49.4% being cysts, and 87.1% classified TIRADS 2 or 3.
Population
Our population is comparable to those studied by Papini and al in Italy [2] and by Kim and al in Seoul [14], with female predominance. In our study women represented more than 2/3 of the population. This could be explained by the higher proportion of women referred to the imaging department, as well as in the general population in our setting.
The mean age in our study was 42 years. Papini and Kim [2, 14] had higher mean ages of 47.8 and 49.2 respectively.
Prevalence of thyroid incidentalomas on ultrasound examination
In our series, the prevalence of TIs was estimated at 28.3% compared to 27% in southern Finland [15]. This is slightly higher than the 22.4% reported by Olusola-Bello in Nigeria [11] and 21% by Kamran and al in Karachi, Pakistan [16], both in 2014. In 2009, in Germany, Guth and al [17] reported 68% prevalence with 53% < 5 mm. The prevalence therefore varies with age, sex, technology available (operator, probe frequency), the minimum size of nodules, and the presence or absence of iodine deficiency in the population. High resolution machines now permit the detection of much smaller nodules, a few millimeters in size [12].
Prevalence of TIs was significantly higher in females (33.3%; p < 0.001), than males (18.4%). This has been also reported by authors in Nigeria [11], Pakistan [16] and Iran [18]. It is generally known that the prevalence of TIs amongst females is four times that of males [10]. This prevalence increases with age, with maximum prevalence in persons > 60 years. TIs are considered as part of the physiologic aging process of the thyroid gland [10, 11, 15, 16]. This might also explain the increase in prevalence with age in our population.
Ultrasound characteristics of thyroid incidentalomas
The locations of TIs had a tendency to be in the right lobe (54%). This result was similar to the previous reports [2, 11, 16]. It might be explained by the difference of the native sizes between right and left lobes, that the right lobe was supposed to be 1.2 folds larger than the left [19–21].
Almost half of TIs were cystic in nature (49.4%) in line with other studies [7, 10, 11]. Solid nodules (33.61%) were mainly hyperechoic (42.0%). Other authors found a predominance of isoechoic or hyperechoic nodules too [2, 7, 14, 18, 22]. Characteristics to indicate malignant potentials were rare in our series (one case with lobulated margins, two cases with microcalcifications). Liebeskind and al [23] had similar findings. Different studies showed marked variability in the size of nodules. We found 22% of nodules ≥ 10 mm in our series, compared to 43% by Kamran and al [16] and 66.5% by Kim and al [14]. Fine needle aspiration is usually recommended for nodules ≥ 10 mm; those < 5 mm are usually transitory, difficult to characterize and to aspirate.
TIRADS classification (Table 1) of thyroid incidentalomas
We had similar prevalence of TIRADS 2 nodules (54.5%) as Olusola-Bello and al (54.0%) in Nigeria [11]; these two populations share similar characteristics. The risk of malignancy in our series was 12.9%, which falls within the range of 7–15% described in existing literature [2, 3, 9, 14]. There was a significant association between risk of malignancy and solidity of nodules (p < 0.000): of the 31 nodules classified TIRADS 4, 77.4% were solid and 22.6% of mixed echogenicity. Solidity of nodules is considered suspicious of malignancy in the TIRADS classification, as opposed to purely cystic and spongiform nodules. There is also an association between size and risk of malignancy (p < 0.001), the prevalence of potentially malignant nodules increases with size (14.3% of TIRADS 4 nodules were 10–15 mm, 22% were > 15 mm). This reiterates the need for cytological examination of nodules > 10 mm whereas those < 5 mm do not need this [10, 14].
We did not find an association between the TIRADS score and age or sex. Capelli and al did not find a significant difference in the prevalence of malignant nodules among the two sexes [22]. Kim and al [14] reported a significantly higher prevalence among females who however represented 4/5 of their study population.
There were some limitations in this study: first this study was conducted in a hospital-based setting; and second no cytological analysis of nodules was performed because participants were either reticent to do so, or lost to follow up. A community based study may better determine the true prevalence of thyroid incidentalomas in the general population.
Conclusion
Thyroid incidentalomas were very frequent with a prevalence of 28.3% and a potential risk of malignancy in 12.9%. Prevalence had a tendency to be increased with age and female sex. Purely cystic nodules are the most frequent. Risks of malignancy would be increased for a larger size and would be higher for TIs of solid components.
Acknowledgements
The authors wish to thank Dr Martine TCHUEM TCHUENTE for helping with the patients’ selection and records.
Funding
None. The authors have no funding source to disclose.
Availability of data and materials
Data of this study are available and can be shared on request.
Authors' contributions
BM conceived the study and participated in its design, data collection, statistical analysis and drafting of the manuscript. JRMT participated in the study design, review of the images and statistical analysis. SDF participated in data collection, the review of the images, statistical analysis and the drafting of the manuscript. FD participated in data collection and proof-reading of the manuscript. EMW participated in data collection and proof-reading of the manuscript. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Our study received clearance from the Ethics Committee of the Faculty and the research authorization from the hospital. Each subject was given details on the study, after which they gave free consent to participate. The consent from participants was verbal. Confidentiality and anonymity were respected.
Abbreviations
- TI
Thyroid incidentalomas
- TIRADS
Thyroid imaging reporting and data system
Contributor Information
Boniface Moifo, Email: bmoifo@yahoo.fr.
Jean Roger Moulion Tapouh, Email: tapouh@yahoo.fr.
Sylviane Dongmo Fomekong, Email: dongfosyl@yahoo.fr.
François Djomou, Email: frandjom@yahoo.fr.
Emmanuella Manka’a Wankie, Email: manuellew@yahoo.co.uk.
References
- 1.Wilhelm S. Evaluation of thyroid incidentaloma. Surg Clin North Am. 2014;94(3):485–97. doi: 10.1016/j.suc.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002;87(5):1941–6. doi: 10.1210/jcem.87.5.8504. [DOI] [PubMed] [Google Scholar]
- 3.Kang HW, No JH, Chung JH, Min Y-K, Lee M-S, Lee M-K, et al. Prevalence, clinical and ultrasonographic characteristics of thyroid incidentalomas. Thyroid Off J Am Thyroid Assoc. 2004;14(1):29–33. doi: 10.1089/105072504322783812. [DOI] [PubMed] [Google Scholar]
- 4.Hoang JK, Lee WK, Lee M, Johnson D, Farrell S. US Features of Thyroid Malignancy: Pearls and Pitfalls. RadioGraphics. 2007;27(3):847–60. doi: 10.1148/rg.273065038. [DOI] [PubMed] [Google Scholar]
- 5.Kim KM, Park JB, Kang SJ, Bae KS. Ultrasonographic guideline for thyroid nodules cytology: single institute experience. J Korean Surg Soc. 2013;84(2):73–9. doi: 10.4174/jkss.2013.84.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwak JY, Han KH, Yoon JH, Moon HJ, Son EJ, Park SH, et al. Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology. 2011;260(3):892–899. doi: 10.1148/radiol.11110206. [DOI] [PubMed] [Google Scholar]
- 7.Russ G, Leboulleux S, Leenhardt L, Hegedüs L. Thyroid Incidentalomas: Epidemiology, Risk Stratification with Ultrasound and Workup. Eur Thyroid J. 2014;3(3):154–63. doi: 10.1159/000365289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koike E, Noguchi S, Yamashita H, et al. Ultrasonographic characteristics of thyroid nodules: Prediction of malignancy. Arch Surg. 2001;136(3):334–7. doi: 10.1001/archsurg.136.3.334. [DOI] [PubMed] [Google Scholar]
- 9.Moifo B, Takoeta EO, Tambe J, Blanc F, Fotsin JG. Reliability of Thyroid Imaging Reporting and Data System (TIRADS) Classification in Differentiating Benign from Malignant Thyroid Nodules. Open J Radiol. 2013;3(3):103–7. doi: 10.4236/ojrad.2013.33016. [DOI] [Google Scholar]
- 10.Tramalloni J, Wémeau JL. Consensus français sur la prise en charge du nodule thyroïdien : ce que le radiologue doit connaître. EMC Radiol Imag Médicale Cardiovasc Thorac Cervicale. 2012;7(4):1–18. doi: 10.1016/S1879-8535(12)60946-5. [DOI] [Google Scholar]
- 11.Olusola-Bello MA, Agunloye AM, Adeyinka AO. Ultrasound prevalence and characteristics of incidental thyroid lesions in Nigerian adults. Afr J Med Med Sci. 2013;42(2):125–30. [PubMed] [Google Scholar]
- 12.Tramalloni J, Monpeyssen H. Échographie de la thyroïde. 01/2013 (2ème édition). ELSEVIER / MASSON; 2013. 191 p.
- 13.Russ G, Bigorgne C, Royer B, Rouxel A, Bienvenu-Perrard M. Le système TIRADS en échographie thyroïdienne. J Radiol. 2011;92(7–8):701–13. doi: 10.1016/j.jradio.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 14.Kim D-L, Song K-H, Kim SK. High prevalence of carcinoma in ultrasonography-guided fine needle aspiration cytology of thyroid nodules. Endocr J. 2008;55(1):135–42. doi: 10.1507/endocrj.K07-120. [DOI] [PubMed] [Google Scholar]
- 15.Karaszewski B, Wilkowski M, Tomasiuk T, Szramkowska M, Klasa A, Obołończyk L, et al. The prevalence of incidentaloma--asymptomatic thyroid nodules in the Tricity (Gdansk, Sopot, Gdynia) population. Endokrynol Pol. 2006;57(3):196–200. [PubMed] [Google Scholar]
- 16.Kamran M, Hassan N, Ali M, Ahmad F, Shahzad S, Zehra N. Frequency of thyroid incidentalomas in Karachi population. Pak J Med Sci. 2014;30(4):793–7. doi: 10.12669/pjms.304.4808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guth S, Theune U, Aberle J, Galach A, Bamberger CM. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest. 2009;39(8):699–706. doi: 10.1111/j.1365-2362.2009.02162.x. [DOI] [PubMed] [Google Scholar]
- 18.Mohammadi A, Amirazodi E, Masudi S, Pedram A. Ultrasonographic Prevalence of Thyroid Incidentaloma in Bushehr, Southern Iran. Iran J Radiol. 2009;6(2):65–8. [Google Scholar]
- 19.Şahin E, Elboğa U, Kalender E. Regional reference values of thyroid gland volume in Turkish Adults. Srp Arh Celok Lek. 2015;143(3–4):141–5. doi: 10.2298/sarh1504141s. [DOI] [PubMed] [Google Scholar]
- 20.Müller-Leisse C, Tröger J, Khabirpour F, Pöckler C. Normal values of thyroid gland volume. Ultrasound measurements in schoolchildren 7 to 20 years of age. Dtsch Med Wochenschr 1946. 1988;113(48):1872–5. doi: 10.1055/s-2008-1067904. [DOI] [PubMed] [Google Scholar]
- 21.Moifo B, Djomou F, Dongmo Fomekong S, Tapouh M, Jr, Manka’a Wankie E, Bola A, Ndjolo A, Gonsu Fotsin J. Ultrasound biometrics of normal thyroid gland of Cameroonian adults. J Afr Imag Med. 2016;8(3):102–106. [Google Scholar]
- 22.Cappelli C, Castellano M, Pirola I, Cumetti D, Agosti B, Gandossi E, et al. The predictive value of ultrasound findings in the management of thyroid nodules. QJM. 2006;100(1):29–35. doi: 10.1093/qjmed/hcl121. [DOI] [PubMed] [Google Scholar]
- 23.Liebeskind A, Sikora AG, Komisar A, Slavit D, Fried K. Rates of malignancy in incidentally discovered thyroid nodules evaluated with sonography and fine-needle aspiration. J Ultrasound Med. 2005;24(5):629–634. doi: 10.7863/jum.2005.24.5.629. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of this study are available and can be shared on request.


