Abstract
Objective:
The aim of this study was to assess the efficacy and feasibility of an enhanced heart failure (HF) education with a 6-month telephone follow- up program in post-discharge ambulatory HF patients.
Methods:
The Hit-Point trial was a multicenter, randomized, controlled trial of enhanced HF education with a 6-month telephone follow-up program (EHFP) vs routine care (RC) in patients with HF and reduced ejection fraction. A total of 248 patients from 10 centers in various geographical areas were randomized: 125 to EHFP and 123 to RC. Education included information on adherence to treatment, symptom recognition, diet and fluid intake, weight monitoring, activity and exercise training. Patients were contacted by telephone after 1, 3, and 6 months. The primary study endpoint was cardiovascular death.
Results:
Although all-cause mortality didn’t differ between the EHFP and RC groups (p=NS), the percentage of cardiovascular deaths in the EHFP group was significantly lower than in the RC group at the 6-month follow up (5.6% vs. 8.9%, p=0.04). The median number of emergency room visits was one and the median number of all cause hospitalizations and heart failure hospitalizations were zero. Twenty-tree percent of the EHFP group and 35% of the RC group had more than a median number of emergency room visits (p=0.05). There was no significant difference regarding the median number of all–cause or heart failure hospitalizations. At baseline, 60% of patients in EHFP and 61% in RC were in NYHA Class III or IV, while at the 6-month follow up only 12% in EHFP and 32% in RC were in NYHA Class III or IV (p=0.001).
Conclusion:
These results demonstrate the potential clinical benefits of an enhanced HF education and follow up program led by a cardiologist in reducing cardiovascular deaths and number of emergency room visits with an improvement in functional capacity at 6 months in post-discharge ambulatory HF patients.
Keywords: heart failure, disease management, cardiovascular, health education, outcomes
Introduction
Heart failure (HF) is a common clinical syndrome associated with impaired quality of life, high morbidity, mortality, and frequent hospitalization that affects millions of people from all around the world. Indeed, the rate of HF is expected to increase overtime due to the growing age of the population. Although the prevalence of HF is reported to be 1%–3% in the general population, it increases dramatically from 10% to 15% after 65 years of age, and incidence approaches 20 people per 1000 in the population per year in >75 year-old people (1). Data demonstrate that almost 15 million people have HF in European countries while 6 million have this condition in the United States (1, 2). The HAPPY study showed that the prevalence of HF is 2.9% in Turkey and that almost 1.5 million people suffer from this condition in this country (3).
HF is a progressive disease with a poor prognosis. Despite improvements in therapy, mortality and morbidity remain very high. After HF hospitalization, mortality is reported to be 10% after 30 days and 22% after 1 year (4). The recently published EURObservational Research Programme Heart Failure Pilot Survey demonstrated that the rate of 1-year mortality or rehospitalization was 36% in hospitalized HF patients and 18% in chronic HF patients (5). These large numbers, and repeated prolonged hospitalizations for HF, also create a substantial economic burden on the health care system (6). Therefore, HF requires special management strategies to overcome its worst clinical outcomes.
Disease management programs for the treatment of patients with HF have been advocated in order to optimize therapy, improve patient compliance, and decrease hospitalizations. Over the last two decades, the efficacy of many different HF management programs on clinical outcomes and quality of life have been evaluated (7–15). However, most are costly and unfeasible for use in various geographic areas. The post-discharge Heart Failure Monitoring Program in Turkey (Hit-PoinT) trial was designed to assess the efficacy and feasibility of cardiologist-led enhanced HF education at the time of hospital discharge with a 6-month telephone follow-up program in post-discharge ambulatory HF patients compared with routine care.
Methods
Study population
Inclusion criteria included: 1) >18 years of age, 2) discharged from hospital with a diagnosis of HF within 6 months of randomization, 3) current symptoms of HF despite optimal medical therapy consistent with recent guidelines (angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, beta blocker, mineralocorticoid receptor antagonist, and diuretics), 4) New York Heart Association (NYHA) functional class II–IV and left ventricular ejection fraction (LVEF) <40% as measured by transthoracic echocardiography.
Patients were excluded from this study if they met the following criteria: severe renal failure requiring dialysis, serum creatinine >2.5 mg/dL, severe chronic obstructive pulmonary disease, chronic or intermittent inotropic support, acute coronary syndromes defined by progressive angina or chest pain at rest or new ECG changes and/or serial increase in cardiac troponin levels, recent percutaneous coronary interventions (PCI), cardiogenic shock, hypertrophic cardiomyopathy, acute myocarditis, severe primary valvular heart disease, dysfunction of a prosthetic heart valve, pericardial disease, pregnancy, uncontrolled thyroid disease, currently enrolled in another HF study, or life expectancy less than 6 months.
Trial design and protocol
The Hit-PoinT trial was a randomized, multicenter, controlled study designed to assess cardiologist lead enhanced HF education followed by a 6-month telephone follow-up program (EHFP) with routine care (RC) in post-discharge ambulatory HF patients at 10 centers including university and state hospitals in various geographical areas in Turkey (16). The study protocol was approved by the ethics committee and the study was performed in accordance with the guidelines of the Declaration of Helsinki. All patients gave written informed consent before enrollment.
Patients were recruited between March 2010 and April 2013. In total, 248 eligible patients with chronic HF at 10 cardiology clinics in various geographical areas were randomly assigned in a 1:1 ratio to receive either EHFP or RC at the time of hospital discharge (Fig. 1). In Turkey, there are currently no set standard discharge instructions utilized across the country for patients with HF, therefore, in the RC group, patients were discharged from hospital without receiving any education or follow-up instructions. Prescriptions were given along with the suggestion of a follow-up office visit.
Figure 1.
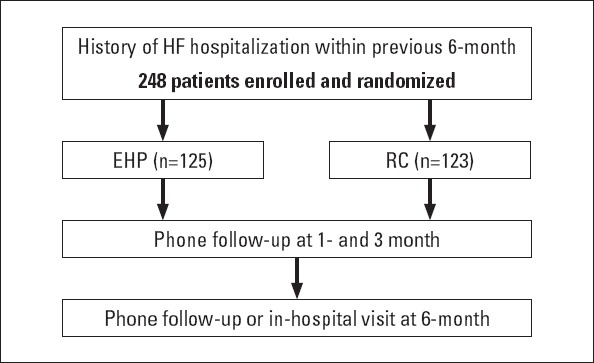
Study design and follow-up plan
EHFP - enhanced heart failure education program; HF - heart failure; RC - routine care
In the EHFP group, patients were educated by a cardiologist and a nurse on HF management during discharge and a HF education booklet was provided. Patients were followed for 6 months after randomization and were contacted by telephone at 1- and 3-month and by telephone and/or an in-hospital visit after 6 months by a study cardiologist or study nurse to collect clinical data and to go over the HF education material. During the telephone follow up, correction of doses or regimen of medication were made by a cardiologist or a nurse under the supervision of a cardiologist. Patients were invited to come to the hospital if needed.
Cardiologists/nurses training and patient’ education
Before beginning the study, two cardiologists and two nurses from each center participated in a one-day training course regarding HF patient education and the study protocol. A printed HF education booklet was prepared in order to unify the education content between centers. In accordance with the study protocol, one session of HF education was implemented by a cardiologist together with a nurse at randomization, in which the primary educator was the cardiologist. Patient education took almost one hour (30 min by the cardiologist and 30 min by the nurse), or more if needed.
The contents of the baseline education included the description, causes, symptoms, prognosis and treatment of HF. In this context, patients in the EHFP group were informed about life style changes, salt intake, fluid and alcohol intake, the importance of weight monitoring, managing weight gain, daily measurement of blood pressure, adherence to medications, participation in daily routine activities, exercise training, recognition of worsening HF symptoms, and when to contact the cardiologist. Also, digital home scales with a HF education booklet were provided to patients in the EHFP group. During telephone follow-up, in addition to study endpoints, adoption of life style changes and adherence to medications were assessed and patients were reminded about salt and fluid intake, weight monitoring, daily routine activities, and exercise training.
Outcome measures
The primary endpoint of this study was cardiovascular mortality. Secondary endpoints were all-cause hospitalization and emergency room visits, all-cause mortality and the rate of hospitalization for HF after 6 months as well as NYHA functional classification adjusted for baseline results.
Statistical analysis
The statistical analysis was performed using the Statistical Package for Social Sciences software 20.0 (IBM SPSS 20, SPSS Inc, Chicago, US). The variables were expressed as mean±standard deviation and median (25.–75. percentiles). We assumed an underlying 30% event rate for the primary end point in the control group and 10% in the intervention group within 6 months of enrollment with a power of 90% and a two-sided alpha level of 0.05, so a total sample size of 248 patients was required to detect such a difference. Data analysis was performed according to the intention-to-treat principle by assigned study groups. Continuous data were analyzed using an independent sample t-test or a paired sample t-test for the analysis of normally distributed variables, or Mood’s Median test was used for the analysis of non-normally distributed variables. Categorical data were presented as frequencies and percentages, and analyzed using a chi-square test and Fisher’s exact test; p values <0.05 were considered statistically significant. To test for significant differences between two percentages, the T-Test of proportions was used.
Results
A total of 248 patients with HF were enrolled into the Hit-PoinT study, of which 125 were randomly assigned to the EHFP group and 123 to the RC group. The mean age of all patients was 60.8±13.8 years. Patients were predominantly men (73%) with NYHA class II–IV HF symptoms who had a mean ejection fraction of 26.8%±7.3%. There were no significant differences in baseline characteristics between the EHFP and the RC groups, except for rate of hyperlipidemia that was more prevalent in the former (p<0.008). Use of pharmacologic therapy at baseline in patients demonstrated compliance with guideline-recommended therapy, and baseline clinical characteristics, laboratory measures, and the use of cardiovascular medication are shown in Table 1.
Table 1.
Baseline clinical and laboratory characteristics and medications
| RC (n=123) | EHFP (n=125) | P | |
|---|---|---|---|
| Mean age, years | 61.1±13.2 | 60.6±14.3 | 0.763 |
| Male gender, % | 70 | 76 | 0.281 |
| Mean weight, kg | 75.2±15.3 | 79.1±19.1 | 0.078 |
| Systolic BP, mm Hg | 110.6±15.5 | 111.2±16.9 | 0.809 |
| Diastolic BP, mm Hg | 68.8±8.8 | 70.3±11.1 | 0.249 |
| Heart rate, bpm | 78.4±13.8 | 77.7±13.8 | 0.706 |
| Diabetes, % | 37 | 35 | 0.718 |
| Hyperlipidemia, % | 25 | 40 | 0.008 |
| Ischemic HF, % | 65 | 67 | 0.817 |
| NYHA III-IV, % | 61 | 60 | 0.630 |
| LVEF, % | 26.2±7.1 | 27.4±7.1 | 0.193 |
| Atrial fibrillation, % | 32 | 29 | 0.515 |
| Sodium, mg/dL | 135.7±12.4 | 135.7±12.2 | 0.991 |
| Potassium, mg/dL | 4.4 +0.7 | 4.5+0.6 | 0.417 |
| BUN, mg/dL | 38.1±24.5 | 35.9±24.4 | 0.486 |
| Creatinine, mg/dL | 1.18+0.9 | 1.21+0.9 | 0.825 |
| Medication | |||
| ACEI, % | 79 | 71 | 0.152 |
| ARB, % | 22 | 27 | 0.280 |
| Beta blocker, % | 95 | 96 | 0.737 |
| Diuretic, % | 98 | 97 | 0.420 |
| Digoxin, % | 49 | 40 | 0.161 |
| Nitrate, % | 31 | 28 | 0.614 |
| Ca blocker, % | 3 | 8 | 0.109 |
| Antiarrhythmic, % | 13 | 15 | 0.731 |
ACE - angiotensin-converting enzyme inhibitor; ARB - angiotensin receptor blocker; BP - blood pressure; BUN - blood urea nitrogen; Ca - calcium; EHFP - enhanced heart failure education program; HF - heart failure; LVEF - left ventricular ejection fraction; NYHA - New York Heart Association; RC - routine care
In total, there were 28 deaths (18 due to cardiovascular causes) after the 6-month follow up. Of those who died due to cardiovascular cause, the number of cardiovascular deaths in the EHFP group was significantly lower than the number of cardiovascular deaths reported in the RC group (46.7% vs 84.6%, p=0.04). Although all-cause mortality did not differ between the two groups (p=NS), the percentage of cardiovascular deaths in the EHFP group was significantly lower than in the RC group at the 6-month follow up (5.6% vs. 8.9%, p=0.04) (Table 2).
Table 2.
6-month adverse outcomes by treatment assignment
| RC (n=123) | EHFP (n=125) | P | |
|---|---|---|---|
| Primary endpoint | |||
| Cardiovascular mortality, n (%) | 11 (8.9%) | 7 (5.6 %) | 0.04 |
| Secondary endpoints | |||
| Median number of emergency room visits >1, n (%) | 40 (35%) | 26 (23%) | 0.05 |
| Median number of all-cause hospitalizations >0, n (%) | 43 (38%) | 47 (40%) | 0.80 |
| Median number of HF hospitalizations >0, n (%) | 35 (29%) | 37 (30%) | 0.95 |
| All-cause mortality, n (%) | 13 (10.5%) | 15 (12%) | 0.75 |
EHFP - enhanced heart failure education program; HF - heart failure; RC - routine care
The median number of emergency room visits was one while the median number of all cause hospitalizations and heart failure hospitalizations was zero. Twenty-tree percent of the EHFP group and 35% of the RC group had more than median number of emergency room visits (p=0.05). Forty percent of the EHFP group and 38% of the RC group had more than median number of all cause hospitalization (p=0.80) and 30% of the EHFP and 29% of the RC group had more than median number of heart failure hospitalization (p=0.95). At baseline, 60% of patients in the EHFP group and 61% of patients in the RC group were in NYHA Class III or IV, while at 6-month follow up only 12% in the EHFP group and 32% in the RC group were in NYHA Class III or IV (p=0.001) (Fig. 2).
Figure 2.
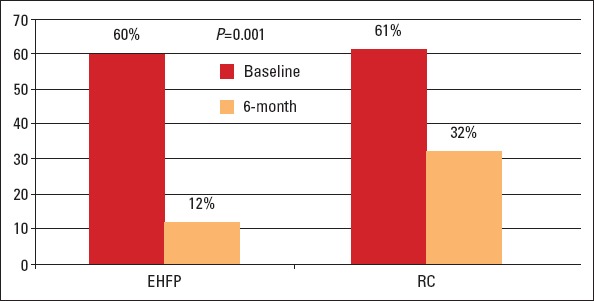
The percentage of patients with NYHA Class III or IV in RC and EHFP groups
EHFP - enhanced heart failure education program; NYHA - New York Heart Association; RC - routine care
Discussion
The results of Hit-PoinT study showed that an enhanced HF education led by a cardiologist and followed by telephone by a cardiologist and/or a nursed trained on HF reduced the cardiovascular deaths and number of emergency room visit, and also significantly improved NYHA functional capacity at 6 months in post-discharge ambulatory HF patients but provided no significant changes in the number of all-cause hospitalization, hospitalization for HF or all-cause mortality.
Although pharmacological and device therapies for the treatment of HF patients have been shown to significantly improve survival and decrease hospitalizations, uneven use of evidence-based therapies has led to the development of disease management programs. HF disease management programs have shown tremendous promise for patients not receiving comprehensive care, but that does not mean they are universally effective. These programs should be feasible and tailored according to the geographic and economic needs of different countries. The formal, controlled testing of validated methods for patient education should be encouraged. The variables should not only be knowledge but should also include a clinical outcome and functional capacity assessment (14). In this context, the Hit-PoinT study has demonstrated that simple and easily-organized enhanced HF patient education and follow-up program, in addition to routine HF care, is feasible and effective for improving clinical outcomes.
In recent years, various HF management programs have been developed to determine the effect of multidisciplinary management programs on the risk of hospital admission and mortality in patients with chronic HF (7–15). Although HF disease management programs have been shown to provide favorable clinical outcomes in terms of reducing morbidity and even mortality, findings from most studies have not been completely consistent and not all have revealed positive results (17, 18). However, recent meta-analyses evaluating HF disease management programs have reported potential improvements in quality of life and cost, in addition to reductions in mortality or re-hospitalization (19, 20).
Previously, home-based automated high-tech monitoring systems compared to enhanced patients education and follow-up have been reported to have no significant effect on cardiovascular death and readmission rate within 6 months and, therefore, enhanced patient education and follow-up was found to be as successful as the use of sophisticated home monitoring devices (21). Several studies have also examined the effects of telephone intervention. Galbreath et al. (22) showed that initial weekly and, later, monthly telephone intervention provided a borderline statistically significant reduction in all-cause mortality during an 18-month follow-up. In another study, centralized telephone interventions compared to usual care were found to be effective in reducing HF hospital admissions, but mortality was not different between the two groups (23). In another randomized controlled trial of telephone case management, no significant differences were found in HF hospitalization, HF days in the hospital, HF cost, all-cause hospitalizations, mortality, or quality of life (24). These different findings suggest that a one-size-fits-all model for disease management is not appropriate for all patients, for all health care systems, or for all countries (21).
Studies that assessed the impact of nurse-led disease management programs have also shown conflicting results. The REMADHE study, a long-term prospective randomized controlled study using repetitive education at 6-month intervals and monitoring for HF outpatients, found benefits of such a group program among a population of relatively young patients (25). In contrast, Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) study examining the effect of nurse-led disease management program of 2 levels of intensity (basic support and intensive support) on death and readmission reported no benefit (13). Two other studies on nurse-directed HF clinics reported favorable effects, but were conducted in experienced hospitals (26, 27). In the TEN-HMS study, Cleland et al. (28) studied the outcomes of home telemonitoring, nurse telephone support, and usual care and found an increase in HF hospitalization and no significant decrease in the number of days spent in the hospital for HF with home telemonitoring when compared to nurse telephone support and usual care during 240-day follow-up. However, in long-term follow-up of their three study groups, they reported a significant reduction in mortality in patients receiving home telemonitoring or nurse telephone support when compared to usual care (34%, 31%, and 51% respectively, p=0.032) (28). In a meta-analysis of telemonitoring and structured telephone disease management programs for HF, Clark et al. (29) reported a significant overall effect of telemonitoring on all-cause mortality compared to usual care but a non-significant effect for structured telephone monitoring programs.
The results of the Hit-Point study are generally consistent with the findings of many other studies on HF disease management programs. Our results showed a reduction in cardiovascular death and emergency room visits, and an improvement in functional capacity, although no effect on HF hospitalization, all-cause hospitalizations, or all-cause mortality were found. Currently, there are no set HF discharge instructions in place in Turkey; thus, HF patients are discharged without any specific instructions. The observed benefits to the intervention group can be explained by the education part of the program, better ambulatory care, and improved adherence to medical therapy. Readmissions to hospital for HF or other associated conditions are frequent and hospitalizations should be considered as a consequence of the clinical course of this disease. Disease management programs require close contact and follow-up with patients and this level of collaboration may lead to an increase in hospitalization or offset the positive effects of disease management programs on readmission. On the other hand, it could be speculated that close contact allows for identification of life-threatening factors and helps to overcome these problems in a timely manner, which might have a positive effect on death rates. In long-term follow-up, it can be expected to find a significant effect on all-cause mortality, as has been shown in TEN-HMS study (28).
Study limitations
Because of the design of this study, both patients and investigators could not be blinded to treatment groups, and this might have introduced some bias into the trials. The other principal limitation was the 6-month duration of the follow-up period. Indeed, because of the comprehensive list of exclusion criteria, findings are only applicable to such a cohort. Although this was a relatively small study on which to base definite conclusions, particularly with regard to reduction in cardiovascular mortality, our results showed a significant reduction in cardiovascular death and emergency room visits in the intervention group, even in short-term follow-up periods. The other important limitation of this study was that there was no assessment on changes in quality of life, adherence to treatment, and the number of ambulatory visits, which makes it difficult to evaluate the impact of intervention. Thus, addition of home visits, more frequent telephone contact, repetitive education, or more frequent hospital visits to study design would be important to determine more significant clinical outcomes.
Conclusions
The Hit-PoinT study was a randomized, multicenter, controlled clinical trial which aimed to evaluate a simple, easily-organized, and widely-applicable HF disease management model feasible for use in developing countries. The results of Hit-PoinT demonstrated the potential clinical benefits of enhanced HF education and follow up program led by a cardiologist in reducing cardiovascular deaths and number of emergency room visits, as well as an improvement in functional capacity at 6 months in post-discharge ambulatory HF patients.
Acknowledgements:
This study had been designed, supported and conducted by the Working Group on Heart Failure of the Turkish Society of Cardiology.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Previous Presentation: Presented in part at the Scientific Sessions and Resuscitation Science Symposium of the American Heart Association, 16-17 November, 2013; Dallas, Texas.
Appendix: Investigators and Nurses
Eskişehir, Turkey: Yüksel Çavuşoğlu, Erkan Gencer, Nilgün Akyol and Julide Coşkun. İzmir, Turkey: Mehdi Zoghi. İstanbul, Turkey: Mehmet Eren, Ahmet Lütfü Orhan, Songül Gençoğlu and Semra Akkaya. Urfa, Turkey: Evin Bozçalı, Veli Polat, Leyla Bilgiç and Belma Bayraklı. Kocaeli, Turkey: Güliz Kozdağ and Nursen Alkaya. Bursa, Turkey: Aysel Aydın Kaderli, Tunay Şentürk, Sevil Dede and Munise Dırık. Edirne, Turkey: Meryem Aktoz, Güray Alicik, Arzu Dereli and Serpil Menekşe. Samsun, Turkey: Halit Zengin, Korhan Soylu, Canan Gülboy and Şoray Ünyeli. Gaziantep, Turkey: Mehmet Aksoy, İbrahim Sarı, Meral Çakır and Sima Annaç. Ankara, Turkey: Ahmet Temizhan and Mehmet Timur Selçuk. İzmir, Turkey: Oktay Ergene, Rida Berilgen, Dilek Yurtsever and Gülhan Şimşek. Pittsburgh, U.S: Özlem Soran.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seferovic PM, Stoerk S, Filippatos G, Mareev V, Kavoliuniene A, Ristic AD, et al. Organization of heart failure management in European Society of Cardiology member countries: survey of the Heart Failure Association of the European Society of Cardiology in collaboration with the Heart Failure National Societies/Working Groups. Eur J Heart Fail. 2013;15:947–59. doi: 10.1093/eurjhf/hft092. [DOI] [PubMed] [Google Scholar]
- 3.Değertekin M, Erol Ç, Ergene O, Tokgözoğlu L, Aksoy M, Erol MK, et al. Heart failure prevalence and predictors in Turkey: HAPPY study. Arch Turk Soc Cardiol. 2012;40:298–308. doi: 10.5543/tkda.2012.65031. [DOI] [PubMed] [Google Scholar]
- 4.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study) Am J Cardiol. 2008;101:1016–22. doi: 10.1016/j.amjcard.2007.11.061. [DOI] [PubMed] [Google Scholar]
- 5.Maggioni AP, Dahlström U, Flippatos G, Chioncel O, Leiro MC, Drozdz J, et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot) Eur J Heart Fail. 2013;15:808–17. doi: 10.1093/eurjhf/hft050. [DOI] [PubMed] [Google Scholar]
- 6.Şahin S, Doğan U, Özdemir K, Gök H. Evaluation of clinical and demographic characteristics and their association with length of hospital stay in patients admitted to cardiac intensive care unit with the diagnosis of acute heart failure. Anatolian J Cardiol. 2012;12:123–31. doi: 10.5152/akd.2012.038. [DOI] [PubMed] [Google Scholar]
- 7.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM, et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–5. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 8.Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Ünger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162:705–12. doi: 10.1001/archinte.162.6.705. [DOI] [PubMed] [Google Scholar]
- 9.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA. 1999;281:613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 10.Berg GD, Wadhwa S, Johnson AE. A matched-cohort study of health services utilization and financial outcomes for a heart failure disease-management program in elderly patients. J Am Geriatr Soc. 2004;52:1655–61. doi: 10.1111/j.1532-5415.2004.52457.x. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg LR, Piette JD, Walsh MN, Frank TA, Jaski BE, Smith AL, et al. WHARF Investigators. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: the Weight Monitoring in Heart Failure (WHARF) trial. Am Heart J. 2003;146:705–12. doi: 10.1016/S0002-8703(03)00393-4. [DOI] [PubMed] [Google Scholar]
- 12.Bocchi EA, Cruz F, Guimaraes G, Pinho Moreira LF, Issa VS, Ayub Ferreira, et al. Long-term prospective, randomized, controlled study using repetitive education at six-month intervals and monitoring for adherence in heart failure outpatients: the REMADHE trial. Circ Heart Fail. 2008;1:115–24. doi: 10.1161/CIRCHEARTFAILURE.107.744870. [DOI] [PubMed] [Google Scholar]
- 13.Jaarsma T, van der Wal MH, Lesman-Leegte I, Luttik ML, Hogenhuis J, Veege NJ, et al. Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) Investigators. Effect of moderate or intensive disease management program on outcome in patients with heart failure: Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) Arch Intern Med. 2008;168:316–24. doi: 10.1001/archinternmed.2007.83. [DOI] [PubMed] [Google Scholar]
- 14.Soran OZ, Piña IL, Lamas GA, Kelsey SF, Selzer F, Pilotte J, et al. A randomized clinical trial of the clinical effects of enhanced heart failure monitoring using a computer based telephonic monitoring system in older minorities and women. J Card Fail. 2008;14:711–7. doi: 10.1016/j.cardfail.2008.06.448. [DOI] [PubMed] [Google Scholar]
- 15.Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, et al. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure. The telemedical interventional monitoring in heart failure study. Circulation. 2011;123:1873–80. doi: 10.1161/CIRCULATIONAHA.111.018473. [DOI] [PubMed] [Google Scholar]
- 16.Çavuşoğlu Y, Zoghi M, Eren M, Bozçalı E, Kozdağ G, Şentürk T, et al. Does cardiologist lead enhanced heart failure education and follow-up program affect cardiovascular mortality?: Hit-Point. Circulation. 2013;128(Suppl) Meeting Abstract: 17804. [Google Scholar]
- 17.McAlister FA, Lawson FM, Teo KK, Armstrong PW. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110:378–84. doi: 10.1016/s0002-9343(00)00743-9. [DOI] [PubMed] [Google Scholar]
- 18.Göhler A, Januzzi JL, Worrell SS, Osterziel KJ, Gazelle GS, Dietz R, et al. A systematic meta-analysis of the efficacy and heterogeneity of disease management programs in congestive heart failure. J Card Fail. 2006;12:554–67. doi: 10.1016/j.cardfail.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 19.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–9. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 20.Gonseth J, Guallar-Castillon P, Banegas JR, Rodriguez-Artalejo F. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur Heart J. 2004;25:1570–95. doi: 10.1016/j.ehj.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 21.Soran OZ, Feldman AM, Piña IL, Lamas GA, Kelsey SF, Selzer F, et al. Cost of medical services in older patients with heart failure those receiving enhanced monitoring using a computer-based telephonic monitoring system compared with those in usual care: the heart failure home care trial. J Card Fail. 2010;16:859–66. doi: 10.1016/j.cardfail.2010.05.028. [DOI] [PubMed] [Google Scholar]
- 22.Galbreath AD, Krasuski RA, Smith B, Stajduhar KC, Kwan MD, Ellis R, et al. Long-term healthcare and cost outcomes of disease management in a large, randomized, community-based population with heart failure. Circulation. 2004;110:3518–26. doi: 10.1161/01.CIR.0000148957.62328.89. [DOI] [PubMed] [Google Scholar]
- 23.GESICA Investigators. Randomised trial of telephone intervention in chronic heart failure: DIAL trial. BMJ. 2005;331:425. doi: 10.1136/bmj.38516.398067.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riegel B, Carlson B, Glaser D, Romero T. Randomized controlled trial of telephone case management in Hispanics of Mexican origin with heart failure. J Cardiac Fail. 2006;12:211–9. doi: 10.1016/j.cardfail.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Bocchi EA, Cruz F, Guimaraes G, Moreira LFP, Issa VS, Ferreira SMA, et al. A long-term prospective randomized controlled study using repetitive education at 6 month intervals and monitoring for heart failure outpatients-The REMADHE Study. ACC Meeting, 56th Annual Scientific Sesssion, New Orleans, LA March 24-27. 2007:415–9. [Google Scholar]
- 26.Strömberg A, Martensson J, Fridlund B, Levin LA, Karlsson JE, Dahlström U. Nurse-led heart failure clinics improve survival and self-care behavior in patients with heart failure: results from a prospective, randomized trial. Eur Heart J. 2003;24:1014–23. doi: 10.1016/s0195-668x(03)00112-x. [DOI] [PubMed] [Google Scholar]
- 27.De la Porte PW, Lok DJ, van Veldhuisen DJ, van Wijngaarden J, Cornel JH, Zuithoff NP, et al. Added value of a physician-and-nurse-directed heart failure clinic: results from the Deventer-Alkmaar heart failure study. Heart. 2007;93:819–25. doi: 10.1136/hrt.2006.095810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cleland JG, Louis AA, Rigby AS, Janssens U, Balk AH. TEN-HMS Investigators. Non-invasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the trans-European network-home-care management system (TEN-HMS) study. J Am Coll Cardiol. 2005;45:1654–64. doi: 10.1016/j.jacc.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 29.Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ. 2007;334:942. doi: 10.1136/bmj.39156.536968.55. [DOI] [PMC free article] [PubMed] [Google Scholar]


