Abstract
Objective:
Combined sedation with propofol and benzodiazepines, known as balanced propofol sedation (BPS), was developed to increase patient comfort during endoscopy. However, the effects of BPS on P-wave dispersion (Pwd), QT interval, and corrected QT (QTc) interval after endoscopy have not been investigated.
Methods:
The study population consisted of 40 patients with BPS and 42 without sedation who were scheduled to undergo upper endoscopy in this cross-sectional prospective study. Patients with hypertension, diabetes mellitus, renal failure, chronic obstructive pulmonary disease, coronary artery disease, or valvular heart disease and those on medications that interfere with cardiac conduction times were excluded. Electrocardiograms (ECGs) was recorded in all patients pre-endoscopy and 10 min post-endoscopy. QT, QT dispersion (QTd), and Pwd were defined from 12-lead ECG. The QTc interval was calculated using Bazett’s formula. All analyses were performed using SPSS 15.0.
Results:
Post-endoscopy P max duration and Pwd were prolonged compared with baseline values (86±13 ms vs. 92±10 ms and 29±12 ms vs. 33±12 ms, respectively; p<0.05). Post-endoscopy QTc and QTd were decreased compared with baseline values, but these decreases were not statistically significant (431±25 ms vs. 416±30 ms and 62±28 ms vs. 43±22 ms, respectively; p>0.05).
Conclusion:
The present study showed that P-wave duration and Pwd values increased after endoscopy with a combination of midazolam and propofol sedation. Physicians should be made aware of the potential effects of BPS in terms on P-wave duration and Pwd values.
Keywords: propofol, midazolam, electrocardiography, P-wave dispersion, QT interval, corrected QT
Introduction
Sedation during endoscopy is preferred for accuracy and patient comfort without distress. Propofol usage for endoscopy has increased over the last decade. Balanced propofol sedation (BPS), which combines propofol with small doses of a benzodiazepine, was developed to reduce the total dose of propofol administered (1). Compared with the use of propofol alone, propofol sedation combined with a benzodiazepine provides superior patient satisfaction and more rapid recovery after endoscopy (2).
Anesthetic agents may show arrhythmogenic properties because of their effects on cardiac electrical activity. The effects of anesthetic agents can be determined on 12-lead electrocardiograms (ECGs) by measuring P-wave dispersion (Pwd) and QT and corrected QT (QTc) intervals (3, 4). Pwd is an electrocardiographic marker associated with inhomogeneous and discontinuous propagation of sinus impulses (5). Prolonged P-wave duration and increased Pwd have been reported to carry an increased risk of atrial fibrillation (AF) (6). QT dispersion (QTd) can be used to assess the homogeneity of cardiac repolarization (7). Increased heterogeneity of repolarization is associated with increased risk of ventricular tachyarrhythmia (8, 9).
In patients with prolonged Pwd and QTc intervals, the choice of anesthetic is important. The effects of anesthesia induction during surgical procedures on Pwd and QTc intervals have been studied; however, there have been no studies of these effects on upper endoscopy. The present study was performed to examine the influence of BPS on atrial and ventricular electrocardiographic indices after diagnostic upper endoscopy.
Methods
Study population
The study population consisted of patients with the American Society of Anesthesiologists (ASA) physical status classification I and II (2) who were scheduled to undergo upper endoscopy between June 1, 2013 and August 30, 2014 at Bozok University Hospital, Yozgat, Turkey. The study consist of 82 consecutive patients (49 females and 33 males) who provided informed consent and underwent upper endoscopy. Patients with hypertension, diabetes mellitus, renal failure, chronic obstructive pulmonary disease, coronary artery disease, or valvular heart disease and those on medications that interfere with cardiac conduction times were excluded. The present study was approved by the local Ethics Committee. Electrocardiography was performed in all patients before and at the end of the procedure. All patients included in the study had sinus rhythm. None of the patients had atrioventricular or bundle branch block, atrial or ventricular premature beat, tachyarrhythmia, or bradyarrhythmia. The monitoring consisted of continuous measurement of oxygen saturation and heart rate and of measurement of blood pressure automatically in 2-minute-intervals.
Study design
Patients who did not want to receive sedation were accepted as the control group. The main group consisted of 40 patients with BPS, cross-sectional prospective study and the control group consists 42 without sedation. According to the ASA criteria, moderate sedation was targeted to maintain patients in a responsive state to slight touch. A 12-lead ECG at a signal size of 10 mm/mV and paper speeds of 25 and 50 mm/s were recorded in all patients within 10 min pre-endoscopy and 10 min post-endoscopy or recovery from anesthesia (Fig. 1).
Figure 1.
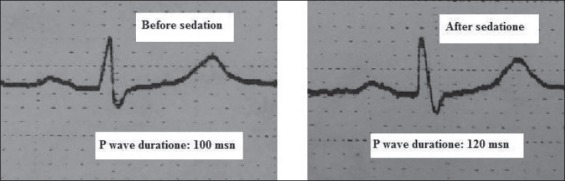
ECG example before and after balanced propofol sedation
Procedure and sedation
All upper endoscopies were performed using the standard technique with the patients initially on their left side. In every upper endoscopy, an emergency set for mask ventilation including emergency drugs was kept ready. The endoscopies were performed by one gastroenterologist (M.C.), and sedations were performed by an anesthesiologist (E.B.). All patients were given supplemental oxygen (2 L/min) through a nasal cannula and were monitored by checking ECG, pulse oximetry, heart rate, and blood pressure. All patients had an intravenous line with a continuously running normal saline infusion. The sedation group received an initial bolus of 2 mg of midazolam and an initial bolus of 30 mg of propofol intravenously. A period of 30 s was allowed to evaluate the effects of propofol before administering additional boluses of 10 mg. For elderly adults, the initial bolus was reduced to 20 mg at the discretion of the anesthesiologist administering the drug. During sedation, a Richmond Agitation-Sedation Scale (RASS) score of 3 and at the measurement after endoscopy, a RASS score of 1 were achieved (10).
Electrocardiography
The P-wave duration was measured from the onset to the offset of P wave. The maximum P-wave duration (P max), defined as the longest P-wave duration in the 12-lead surface ECG, was determined. The minimum P-wave duration (P min), defined as the shortest P-wave duration in the 12-lead surface ECG, was also determined. All recordings were performed in the same quiet room under spontaneous breathing, following 10 min of adjustment in the supine position. P-wave duration measurements were manually obtained by two of the investigators (S.S. and Y.K.Y.) using calipers and a magnifying lens for the accurate definition of the ECG deflection. Pwd was calculated from the difference between maximum and minimum P-wave durations (3). If the amplitude of P waves was indistinguishable from the baseline (either isoelectric or non-isoelectric because of electronic noise), it was considered non measurable. Four patients were excluded from the study because of unmeasurable P waves.
The QT interval was measured from the beginning of the QRS complex to where the T waves descend onto the isoelectric baseline (11, 12). When a U wave interrupted the T wave before returning to baseline, the QT interval was measured to the nadir of the curve between the T and U waves. If the end of the T wave was not clear in a particular lead, it considered non measurable and was excluded from the analysis. Bazett’s formula was used to calculate the QTc interval as QTc (ms)=QT measured/√RR (where RR is the RR interval measured in seconds). During the measurement period, the mean QTc interval was calculated from three consecutive beats. The QTd value was considered as the difference between the longest and shortest QT intervals observed for the 12 ECG leads.
Intra- and inter-observer coefficients of variation (standard deviation of differences between two observations divided by mean value and expressed as percent) were found to be 3.7% and 4.3% for P max and 4.5% and 4.9% for Pd. The interobserver variability for QT dispersion was 9.7±3.6 ms. The intraobserver variability (based on 15 randomly selected ECGs reviewed by the same observer twice) was 7.9±2.9 ms for the QT dispersion.
Statistical analysis
Continuous variables were expressed as means±SD and categorical variables were expressed as percentages. The comparison of variables between the two groups was performed using the c2 test and Student’s t-test. Two levels of the same group were tested by paired-samples t test for parametric variables. Pearson’s correlation analysis was conducted to determine if there was a relationship between the combination dose and ECG parameters and also age and sex. In all analyses, p<0.05 was taken to indicate statistical significance. All analyses were performed using SPSS 15.0 (SPSS Inc., Chicago, IL, USA).
Results
The characteristics of the patients are summarized in Table 1. The mean age of patients in the control and sedation groups were 53.82±13.10 and 44.38±12.39 years, respectively. The control and sedation groups consisted of 59.5% and 60% females, respectively. A combination of 2 mg of midazolam and an average of 59.50±28.09 mg of propofol was administered to the sedation group. The electrocardiographic features of the patients are shown in Table 2. Four patients were excluded from the study because of unmeasurable P waves. In the sedation group, post-endoscopy P-max duration and Pwd were prolonged compared with baseline values (86±13 vs. 92±10 and 29±12 vs. 33±12, respectively; p<0.05). The comparison of the pre- and post-endoscopy values revealed no prolongation of P min duration in the sedation group (p>0.05). Post-endoscopy QTc and QTd were decreased compared with baseline values, but these decreases were not statistically significant in the sedation group (431±25 vs. 416±30; p>0.05 and 62±28 vs. 43±22, respectively; p>0.05). Electrocardiographic features were not different in the control group. There were no significant ventricular or supraventricular arrhythmias during the study, and no mortality or morbidity was observed.
Table 1.
Characteristics of study population
| Sedation group n=40 | Control group n=42 | |
|---|---|---|
| Age, years | 44.38±12.39 | 53.82±13.10 |
| Sex, f/m, % | 60%/40% | 59.5%/40.5% |
| Propofol, mg | 59.50±28.09 | - |
| Midazolam, mg | 2 | - |
| RASS score | - | |
| • Pre-endoscopy | 0 | |
| • During endoscopy | -3 | |
| • Post-endoscopy | -1 | |
| Complication, n | ||
| Oxygen saturation <90 % | 1 | 0 |
| Heart rate <50 bpm | 0 | 0 |
| Systolic blood pressure | 0 | 0 |
| <90 mm Hg | ||
Values are expressed as mean±SD, percentage (%). RASS - Richmond Agitation-Sedation Scale
Table 2.
Electrocardiographic features of both groups of pre- and post-endoscopy
| Pre-endoscopy | Post-endoscopy | P | |
|---|---|---|---|
| Control group | |||
| P Max, ms | 95±11 | 96±11 | 0.514 |
| P Min, ms | 57±14 | 57±12 | 0.707 |
| Pwd, ms | 37±14 | 39±12 | 0.347 |
| QTc, ms | 431±35 | 422±69 | 0.33 |
| QTd, ms | 57±16 | 56±15 | 0.392 |
| Sedation group | |||
| P Max, ms | 86±13 | 92±10 | 0.01 |
| P Min, ms | 58.0±13 | 58.3±11 | 0.786 |
| Pwd, ms | 29±12 | 33±12 | 0.014 |
| QTc, ms | 431±25 | 416±30 | 0.133 |
| QTd, ms | 62±28 | 43±22 | 0.606 |
Values are expressed as mean±SD. P max - maximum P-wave duration; P min - minimum P-wave duration; Pwd - P-wave dispersion; QTc - corrected QT; QTd - QT dispersion
Discussion
The present study showed that P-wave duration and Pwd values increased after upper endoscopy with a combination of midazolam and propofol sedation.
To our knowledge, atrial and ventricular electromechanical delays have not been evaluated in patients undergoing endoscopy. This is the first study to examine P-wave duration, Pwd, QTc, and QTd after upper endoscopy with BPS. The results of the present study showed that P max and Pwd values were significantly increased immediately after upper endoscopy. This study did not determine any significant differences with regard to QT indices before or after endoscopic sedation. The increased P-wave duration and Pwd observed in the present study likely indicated conduction system involvement and subsequent prolongation of inter-atrial and intra-atrial conduction times and the inhomogeneous propagation of sinus impulses, which may promote atrial electrical remodeling. These findings suggest that patients with combination sedation in endoscopy may be at risk of atrial arrhythmia. The patients in our study group were asymptomatic and had no cardiac arrhythmia.
The mechanism underlying the observed Pwd prolongation of BPS may be related to the action of the anesthetic agents on myocardial cell ion channels, or it may be due to an indirect mechanism that influences cardiac repolarization, such as modification of autonomic nervous system tone (13, 14). In animal studies, some anesthetic agents have inhibitory and blocking effects on the ion channels of cardiac myocytes (13). The expected blood concentration was 6 µg/mL, and the effect-site concentration was 3 µg/mL at the measurement time calculated by the Marsh model to achieve this effect (15). Propofol induces parasympathetic dominance (16). During endoscopy, propofol administration decreases blood pressure, and vagal responses may contribute to bradycardia and hypotension (14). Midazolam induces sympathetic dominance and also causes a reduction in arterial blood pressure and an increase in heart rate (16, 17). An increase in vagus nerve activity results in bradycardia, decreases cardiac contractility, and shortens the atrial refractory period inhomogeneously (18). We speculate that propofol predominates vagal tones despite the action of midazolam, resulting in the prolongation of the P wave.
Midazolam is used in endoscopic sedation and is known to not affect the QTc interval (19). In one study, Owczuk et al. (20) reported that propofol infusion decreased Pwd after 3 and 5 min of anesthesia. Kazancı et al. (4) found no significant effects of anesthesia induction with propofol on Pwd and QTc interval. There have been conflicting reports regarding whether propofol sedation lengthens, shortens, or does not affect QT intervals. Kim et al. (21) reported lengthening of the QTc intervals by propofol administration, whereas Oji et al. (22) reported shortening of the QTc interval. Whyte et al. (13) found no effect of propofol on QTc interval. In this study, the P max and Pwd values were significantly increased immediately after endoscopy with propofol and midazolam administration. These conflicting results indicate that large, randomized, and prospective studies are needed to define the effects of propofol on atrial and ventricular electrical activity and that there is a need to develop other noninvasive indicators that better reflect changes in atrial indices and ventricular repolarization.
The data reported in literature indicate that BPS can be safely applied in patients undergoing outpatient endoscopy (2, 23). Combination therapy during endoscopy results in greater patient satisfaction than sedation with opiates and benzodiazepines. Combination therapy also results in lower doses of propofol and shorter recovery periods (2).
Although combination therapy makes endoscopic sedation safer, the revealed arrhythmia potential should also be taken into consideration.
Study limitations
The present study had several limitations. First, the sample size was small because of the exclusion of patients with hypertension, diabetes mellitus, coronary artery disease, or valvular heart disease and those on medications that interfere with cardiac conduction times. Second, a comparison between P-wave duration values could not be conducted because of the lack of a propofol-alone group. Third, this was a cross-sectional study; therefore, we could not prospectively follow-up the patients for future arrhythmic events. Fourth, atrial and ventricular conduction times were not examined by invasive electrophysiological techniques, which are the gold standard for such evaluations. Fifth, all measurements were manually taken that may add some inaccurancy to the results. To overcome some of these restrictions, averaging techniques used in advanced recording devices and magnified graticules on standard computer screens have proven useful in the accurate evaluation of common P-wave descriptors (24).
Finally, because of the short half-life profile, the effects of propofol may be diminished after endoscopy. However, the duration of action may continue for up to 10 min, and a full recovery may occur within 10–20 min after the discontinuation of propofol.
Conclusion
Although BPS makes endoscopic sedation safer, the effects of these sedatives on atrial conduction time and revealed arrhythmia should also be taken into consideration.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - E.B., M.C.; Design - E.B., S.S., S.D.; Supervision - E.B., M.C., Y.K.Y.; Materials - M.C.; Data collection &/or processing - E.B., S.S., M.C.; Analysis &/or interpretation - S.D., M.C.; Literature search - E.B., M.C., Y.K.Y.; Writing - E.B., M.C.; Critical review - Ö.Ö.
References
- 1.Molina-Infante J, Duenas-Sadornil C, Mateos-Rodriguez JM, Perez-Gallardo B, Vinagre-Rodriguez G, Hernandez-Alonso M, et al. Non-anesthesiologist-administered propofol versus midazolam and propofol, titrated to moderate sedation, for colonoscopy: a randomized controlled trial. Dig Dis Sci. 2012;57:2385–93. doi: 10.1007/s10620-012-2222-4. [DOI] [PubMed] [Google Scholar]
- 2.Levitzky BE, Lopez R, Dumot JA, Vargo JJ. Moderate sedation for elective upper endoscopy with balanced propofol versus fentanyl and midazolam alone: a randomized clinical trial. Endoscopy. 2012;44:13–20. doi: 10.1055/s-0031-1291421. [DOI] [PubMed] [Google Scholar]
- 3.Aytemir K, Özer N, Atalar E, Sade E, Aksöyek S, Övünç K, et al. P wave dispersion on 12-lead electrocardiography in patients with paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2000;23:1109–12. doi: 10.1111/j.1540-8159.2000.tb00910.x. [DOI] [PubMed] [Google Scholar]
- 4.Kazancı D, Ünver S, Karadeniz U, İyican D, Koruk S, Yılmaz MB, et al. A comparison of the effects of desflurane, sevoflurane and propofol on QT, QTc, and P dispersion on ECG. Ann Card Anaesth. 2009;12:107–12. doi: 10.4103/0971-9784.51361. [DOI] [PubMed] [Google Scholar]
- 5.Doğan U, Doğan EA, Tekinalp M, Tokgöz OS, Arıbaş A, Akıllı H, et al. P-wave dispersion for predicting paroxysmal atrial fibrillation in acute ischemic stroke. Int J Med Sci. 2012;9:108–14. doi: 10.7150/ijms.9.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caldwell J, Koppikar S, Barake W, Redfearn D, Michael K, Simpson C, et al. Prolonged P-wave duration is associated with atrial fibrillation recurrence after successful pulmonary vein isolation for paroxysmal atrial fibrillation. J Interv Card Electrophysiol. 2014;39:131–8. doi: 10.1007/s10840-013-9851-1. [DOI] [PubMed] [Google Scholar]
- 7.Eslami V, Safi M, Taherkhani M, Adibi A, Movahed MR. Evaluation of QT, QT dispersion, and T-wave peak to end time changes after primary percutaneous coronary intervention in patients presenting with acute ST-elevation myocardial infarction. J Invasive Cardiol. 2013;25:232–4. [PubMed] [Google Scholar]
- 8.Booker PD, Whyte SD, Ladusans EJ. Long QT syndrome and anaesthesia. Br J Anaesth. 2003;90:349–66. doi: 10.1093/bja/aeg061. [DOI] [PubMed] [Google Scholar]
- 9.Shah RR. Drug-induced QT dispersion: does it predict the risk of Torsade de Pointes? J Electrocardiol. 2005;38:10–8. doi: 10.1016/j.jelectrocard.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Almgren M, Lundmark M, Samuelson K. The Richmond Agitation-Sedation Scale: translation and reliability testing in a Swedish intensive care unit. Acta Anaesthesiol Scand. 2010;54:729–35. doi: 10.1111/j.1399-6576.2009.02173.x. [DOI] [PubMed] [Google Scholar]
- 11.Hancı V, Ayoğlu H, Yurtlu S, Yıldırım N, Okyay RD, Erdoğan G, et al. An evaluation of P wave dispersion, QT, corrected QT and corrected QT dispersion intervals on the electrocardiograms of malnourished adults. Anaesth Intensive Care. 2010;38:122–7. doi: 10.1177/0310057X1003800120. [DOI] [PubMed] [Google Scholar]
- 12.Szczeklik W, Sokolowska BM, Mastalerz L, Miszalski-Jamka T, Pacult K, Gorka J, et al. QT dispersion in patients with Churg-Strauss syndrome. Kardiol Pol. 2011;69:1143–9. [PubMed] [Google Scholar]
- 13.Whyte SD, Booker PD, Buckley DG. The effects of propofol and sevoflurane on the QT interval and transmural dispersion of repolarization in children. Anesth Analg. 2005;100:71–7. doi: 10.1213/01.ANE.0000140781.18391.41. [DOI] [PubMed] [Google Scholar]
- 14.Friedrich K, Stremmel W, Sieg A. Endoscopist-administered propofol sedation is safe - a prospective evaluation of 10,000 patients in an outpatient practice. J Gastrointestin Liver Dis. 2012;21:259–63. [PubMed] [Google Scholar]
- 15.Absalom AR, Mani V, De Smet T, Struys MM. Pharmacokinetic models for propofol--defining and illuminating the devil in the detail. Br J Anaesth. 2009;103:26–37. doi: 10.1093/bja/aep143. [DOI] [PubMed] [Google Scholar]
- 16.Ogawa Y, Iwasaki K, Aoki K, Gokan D, Hirose N, Kato J, et al. The different effects of midazolam and propofol sedation on dynamic cerebral autoregulation. Anesth Analg. 2010;111:1279–84. doi: 10.1213/ANE.0b013e3181f42fc0. [DOI] [PubMed] [Google Scholar]
- 17.Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19:463–81. doi: 10.3748/wjg.v19.i4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alıcı G, Özkan B, Yazıcıoğlu MV, Şahin M, Bulut M, Acar G, et al. P-wave dispersion by 12-lead electrocardiography in carotid artery stenting. Clin Auton Res. 2013;23:81–4. doi: 10.1007/s10286-012-0186-2. [DOI] [PubMed] [Google Scholar]
- 19.Owczuk R, Twardowski P, Dylczyk-Sommer A, Wujtewicz MA, Sawicka W, Drogoszewska B, et al. Influence of promethazine on cardiac repolarisation: a double-blind, midazolam-controlled study. Anaesthesia. 2009;64:609–14. doi: 10.1111/j.1365-2044.2009.05890.x. [DOI] [PubMed] [Google Scholar]
- 20.Owczuk R, Wujtewicz MA, Sawicka W, Polak-Krzeminska A, Suszynska-Mosiewicz A, Raczynska K, et al. Effect of anaesthetic agents on p-wave dispersion on the electrocardiogram: comparison of propofol and desflurane. Clin Exp Pharmacol Physiol. 2008;35:1071–6. doi: 10.1111/j.1440-1681.2008.04963.x. [DOI] [PubMed] [Google Scholar]
- 21.Kim DH, Kweon TD, Nam SB, Han DW, Cho WY, Lee JS. Effects of target concentration infusion of propofol and tracheal intubation on QTc interval. Anaesthesia. 2008;63:1061–4. doi: 10.1111/j.1365-2044.2008.05564.x. [DOI] [PubMed] [Google Scholar]
- 22.Oji M, Terao Y, Toyoda T, Kuriyama T, Miura K, Fukusaki M, et al. Differential effects of propofol and sevoflurane on QT interval during anesthetic induction. J Clin Monit Comput. 2013;27:243–8. doi: 10.1007/s10877-012-9420-7. [DOI] [PubMed] [Google Scholar]
- 23.VanNatta ME, Rex DK. Propofol alone titrated to deep sedation versus propofol in combination with opioids and/or benzodiazepines and titrated to moderate sedation for colonoscopy. Am J Gastroenterol. 2006;101:2209–17. doi: 10.1111/j.1572-0241.2006.00760.x. [DOI] [PubMed] [Google Scholar]
- 24.Dilaveris P, Batchvarov V, Gialafos J, Malik M. Comparison of different methods for manual P wave duration measurement in 12-lead electrocardiograms. Pacing Clin Electrophysiol. 1999;22:1532–8. doi: 10.1111/j.1540-8159.1999.tb00358.x. [DOI] [PubMed] [Google Scholar]


