Abstract
Objective:
A reliable and easy-to-perform method for measuring right ventricular (RV) afterload is desirable when scheduling patients with systolic heart failure to undergo heart transplantation. The present study aimed to investigate the accuracy of echocardiographically-derived pulmonary arterial elastance as a measurement of pulmonary vascular resistance by comparing it with invasive measures.
Methods:
Thirty-one patients with moderate to severe systolic heart failure, including 22 (71%) male patients, with a mean age of 41.16±15.9 years were enrolled in the study. Right heart catheterization and comprehensive echocardiography during the first hour after completion of cardiac catheterization were performed in all the patients. The pulmonary artery elastance was estimated using the ratio of end-systolic pressure (Pes) over the stroke volume (SV) by both cardiac catheterization [Ea (PV)-C] and echocardiography [Ea (PV)-E].
Results:
The mean Ea (PV)-C and Ea (PV)-E were estimated to be 0.73±0.49 mm Hg/mL and 0.67±0.44 mm Hg/mL, respectively. There was a significant relation between Ea (PV)-E and Ea (PV)-C (r=0.897, p<0.001). Agreement between echocardiography and catheterization methods for estimating Ea (PV), investigated by the Bland-Altman method, showed a mean bias of -0.06, with 95% limits of agreement from -0.36 mm Hg/mL to 0.48 mm Hg/mL.
Conclusion:
Doppler echocardiography is an easy, non-invasive, and inexpensive method for measuring pulmonary arterial elastance, which provides accurate and reliable estimation of RV afterload in patients with systolic heart failure.
Keywords: Key words: arterial elastance, Doppler echocardiography, pulmonary artery, right ventricular function
Introduction
Because of the current evidence regarding the increasing number of hospitalizations for pulmonary arterial elastance and death rate secondary to the heart failure and also the cost expended annually for taking care of these patients, this issue is transforming into a global epidemic (1). The function of the right ventricle in congestive heart failure is one of the strong outcome predictors (2, 3), and the most prevalent cause of the right heart failure is indeed the left ventricular failure. In these conditions, the increase of right ventricular (RV) afterload will lead to a decrease of right ventricular ejection fraction (RVEF), stroke volume, and cardiac output and eventually lead to progressive RV failure (4-6). Thus, RV afterload evaluation in patients suffering from systolic heart failure will help to predict the RV function in future. Moreover, in advanced heart failure patients who are candidates for heart transplantation, the RV afterload has an essential role in making a decision regarding placing them on the transplant list and to predict the prognosis after transplantation (7). At the present time, the standard method for examining the RV afterload in these patients is measuring pulmonary vascular resistance by right-sided catheterization, which is the average of pressure drop in the pulmonary arterial tree over the average of pulmonary flow. This method is based on the assumption of steady hemodynamics, suggesting that it is a fixed and stable hemodynamic (8). However, because RV afterload and pulmonary artery hemodynamics are induced through the acute and chronic changes created in compliance and pressure waves return in proximal pulmonary artery, it is important and vital to use other methods which seem to be more useful in a thorough and complete estimation of RV afterload (9, 10). The examination of pulmonary artery impedance is a much more precise method in the estimation of pulmonary arterial hypertension (11); on the other hand, it is very difficult to use it for the treatment of patients, considering the complexity of this method. Effective arterial elastance (Ea), which includes the systolic pressure gradient curve over the stroke volume (SV), is one of the indices used to overcome the abovementioned problems in the afterload estimation (12-15).
All of the above indices are calculated invasively through right heart catheterization. However, the use of other non-invasive methods such as echocardiography and magnetic resonance imaging (MRI) to calculate the hemodynamic indices has always been considered, particularly, Doppler echocardiography, which is able to determine the cardiac hemodynamics in a non-invasive manner, has significantly impacted clinical medicine. Because it is possible to find the pressure and flow variables through the Doppler, we have assumed that we may be able to precisely estimate the pulmonary arterial elastance through the Doppler obtained variables in the present study.
Methods
In this study, 31 patients with moderate to severe systolic heart failure (left ventricular ejection fraction <35%) have been examined. All of the patients were referred to the heart failure clinic of Rajaei Cardiovascular, Medical and Research Center, Tehran, Iran (a tertiary health care center for cardiovascular disease) between May 2009 and January 2010 to undergo right heart catheterization.
Right heart catheterization was performed for all of the patients, and comprehensive echocardiography was performed during the first hour after completion of cardiac catheterization. The patients with a shunt in the heart and atrial fibrillation with rapid ventricular response were excluded from the study.
The present study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki. Institutional Review Boards at Iran University of Medical Science approved the study protocol, and written informed consent was obtained from all patients.
Right heart catheterization
Standard right heart catheterization was performed using Edwards Life Sciences Swan Ganz catheters (Irvine, CA) via the right jugular vein. The right side pressures, including pulmonary arterial and pulmonary capillary wedge pressures, for estimating the left atrium pressure were obtained using the fluid-filled system. All of the pressures were obtained at the end of the expiration, and the zero point in the mid-chest level and also the average of 10 wave burst was considered for the calculation.
Measuring cardiac output
The cardiac output was measured with both the thermodilution technique and direct Fick method.
Thermodilution technique
A 10 mL sterile, ice-cold isotonic (0.9%) saline was injected through the proximal (right atrial) lumen of the catheter and its temperature was measured by a thermistor that was placed directly behind the right atrial inlet of the catheter. The drop in temperature at the distal thermistor was subsequently recorded.
Cardiac output was calculated using an analog computer system (REF-1, ejection fraction cardiac output computer; Baxter Healthcare Corp. Santa Ana, CA).
Direct Fick method
PO2, PCO2, pH, base excess, and (calculated) SaO2 were determined from arterial and mixed venous blood samples, which were simultaneously obtained via the arterial line and the distal (pulmonary arterial) opening of the Swan-Ganz catheter, respectively (ABL 520; Radiometer, Copenhagen, Denmark). The arterial and mixed venous oxygen contents (CaO2 and CvO2) were calculated as the product of hemoglobin (g/L), the hemoglobin-binding constant for oxygen (1.34 g/L), and oxygen saturation.
Oxygen content of blood=[hemoglobin] (g/dL)×1.34 (mL O2/g of hemoglobin)×saturation of blood (percent)
Oxygen consumption (VO2) was measured while the blood samples were obtained using a commercially available system (Oxycon Champion 3.0; Jaeger, Würzburg, Germany).
The cardiac output was subsequently calculated according to the formula:
Pulmonary arterial elastance measured by catheterization [Ea (PV)-C]
The catheterization-derived effective arterial elastance of the pulmonary artery [Ea (PV)-C] was calculated using the following formula (14):
where Pes is the pulmonary artery systolic pressure (the pressure is considered as the arterial end-systolic pressure at the dicrotic notch) and SV is the stroke volume.
Doppler echocardiography
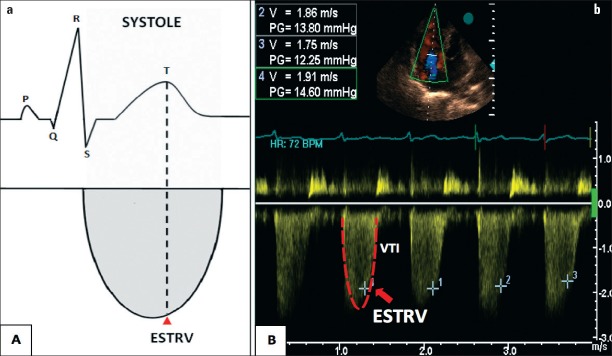
The Doppler echocardiography was performed using the GE Vivid 3 ultrasound. By locating a 1-2 mm pulsed wave sample volume in parasternal short axis, the velocity-time integral of right ventricular outflow tract flow (RVOT VTI) was obtained in the proximity of the RVOT, just within the pulmonary valve. The sample volume was located as the sound of the closing and not the opening click of the valve would be clear. The continuous wave Doppler was used to determine the tricuspid regurgitation (TR) velocity in peak and also the end of systole (at the peak of the T wave in electrocardiogram). The TR waves were chosen from the specific fields where it had the best velocity and the best signal, and the agitated saline was used when there was a sub-optimal signal in some cases (16).
Generally, we have used the average of five signals for the calculation and the average of 10 signals for the patients with atrial fibrillation. The echocardiographic physician was blind to the result of the patients’ catheterization.
SV was obtained using the following formula (17):
where SV is the Stroke Volume, D is the RVOT diameter and VTI is velocity-time integral of the RVOT. The RVOT diameter was calculated in the parasternal short axis, right before the pulmonary valve and the average of three times was used.
The pulmonary artery systolic pressure (Pes)
Pes was obtained by this formula:

where ESTRV stands for velocity wave of TR in end-systole (velocity wave in the peak of the T wave in the simultaneous electrocardiogram) (Fig. 1), and RAP is the right arterial pressure, which was estimated using the inferior vena cava diameter and its collapsibility during breathing (18).
Figure 1.
a, b. Diagram showing the tricuspid regurgitation flow across the tricuspid valve and the simultaneous echocardiography (ECG) recording (a); Continuous-wave Doppler ECG tracing at the level of tricuspid valve in a study patient (with systolic heart failure) (b). End-systolic tricuspid regurgitation velocity (ESTRV) is considered as the peak of the T wave in the simultaneous ECG (arrow head) VTI - velocity time integral
Pulmonary arterial elastance estimated by echocardiography [Ea (PV)-E]
All echocardiographic measurements were performed using a commercially available ultrasound system (Vivid 7, GE Medical Systems, Inc., Horten, Norway). Pulmonary arterial elastance [Ea (PV)-E] was estimated using the ratio of end-systolic pressure over the stroke volume obtained from the echocardiography.
Statistical analysis
Data were described as mean±standard deviation (SD) for interval and count (percentage) for categorical variables. Fitness of interval variables to Gaussian distribution was examined by one-sample Kolmogorov-Smirnov test. Linear correlations between the indices were estimated by Pearson’s r (for normally distributed data) and Spearman’s rho (for non-normally distributed data) correlation coefficients. The level of agreement between the two measurement methods {effective pulmonary elastance measured by catheterization [Ea (PV)-C] and calculated pulmonary elastance estimated by echocardiography [Ea (PV)-E]} was assessed using the Bland-Altman method. A p value <.05 was considered statistically significant. Statistical analysis was performed by SPSS 15 for Windows (SPSS Inc, Chicago, IL, USA).
Results
Thirty-one out of 42 patients were included in this study; 11 of them did not have an appropriate TR flow and were excluded from the study. The majority of patients were males (22 patients, 71%). The mean age was 41.16±15.90 years, and the mean body surface area was 1.71±0.19 m2. The most common etiology was non-ischemic dilated cardiomyopathy (19 patients, 61%), and the second most common etiology was ischemic cardiomyopathy (9 patients, 26%). The basic clinical features of patients are summarized in Table 1.
Table 1.
Baseline characteristics of patients
| Gender, M/F | 22 (71)/9 (29) |
| Age, years | 41.16±15.90 |
| Height, cm | 163.20±31.23 |
| Weight, kg | 66.13±12.91 |
| BSA, m2 | 1.71±0.19 |
| Diagnosis | |
| DCM | 19 (61) |
| ICMP | 8 (26) |
| HCM | 1 (3) |
| VHD | 2 (7) |
| PPCMP | (3) |
Data are presented as numbers (percentage) and mean±standard deviation. BSA - body surface area; DCM - dilated cardiomyopathy; HCM - hypertrophic cardiomyopathy; ICMP - ischemic cardiomyopathy; PPCMP - postpartum cardiomyopathy; VHD - valvular heart disease (other than aortic stenosis)
Pulmonary hemodynamic variables
Pulmonary hemodynamic variable features of the study patients are summarized in Table 2.
Table 2.
Pulmonary hemodynamic variables
| Hemodynamic data | Mean±SD |
|---|---|
| Right atrial pressure, mm Hg | 9.83±6.24 |
| PA pressure (systolic/diastolic), mm Hg | 45.83/23.60±28.54/14.11 |
| Mean PA pressure, mm Hg | 31.43±18.47 |
| Pulmonary capillary wedge pressure, mm Hg | 18.91±10.44 |
| Pulmonary vascular resistance, dyn.s/cm5 | 181.46±128.79 |
| Cardiac output, L/min | |
| Fick | 4.50±1.22 |
| Thermodilution | 4.31±0.95 |
| Cardiac index Thermodilution, L/min/m2 | 2.52±0.54 |
| Stroke volume, mL | 56.31±18.73 |
| Ea (PV)-C, mm Hg/mL† | 0.73±0.49 |
| Ea (PV)-E, mm Hg/mL‡ | 0.67±0.44 |
Ea (PV) - arterial elastance of pulmonary vasculature; PA - pulmonary artery.
Ea (PV) - with catheterization;
Ea (PV) - with echocardiography
A strong and significant correlation was observed between Ea (PV)-E and Ea (PV)-C (r=0.897 and p<0.001).
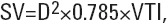
Moreover, for assessing the agreement between Ea (PV)-C and Ea (PV)-E, we applied the Bland-Altman method to obtain the agreement plot (Fig. 2). The mean difference (bias) of the measurements between echocardiography and catheterization methods is -0.06 (p=0.10). The SD of the difference is 0.21 and the 95% limits of agreement (mean±1.96 SD) range from -0.36 mm Hg/mL to 0.48 mm Hg/mL. To ensure the absence of a proportional error, a linear regression analysis was performed between the difference and mean of the two measurements (Table 3).
Figure 2.

Bland-Altman plot. The difference between echocardiography and catheterization-derived pulmonary arterial elastance is drawn against the mean of the two measurements
Table 3.
Linear regression between mean and difference of two measurement methods of Ea (PV) (Dependent variable: Difference of two measurement methods)
| Constant | Coefficient±SE | P |
|---|---|---|
| Mean of two | 0.054±.074 | 0.699 |
| measurement methods† | 1.018±0.093 | 0.132 |
Abbreviation: Ea (PV), arterial elastance of pulmonary vasculature.
[Ea (PV)-C+Ea (PV)-E]/2
Discussion
In the present study, we used echocardiography to assess the pulmonary arterial elastance as a factor of RV afterload. There was a significant increase of the pulmonary vascular resistance in congestive heart failure (CHF); however, this factor shows us a stable flow and does not explain the pulsatile flow completely, which is seen in a vascular bed with low pressure and high compliance (19). On the other hand, because of the low resistance and high compliance in the pulmonary blood flow, the pulsatile hydraulic load components are highly important and it has to be considered (20). Several studies have shown that the pulsatile load increases in chronic pulmonary hypertension, which can be determined by the rise in impedance characteristics and wave reflection. This type of unusual pulsatile load may have unsuitable effects on the ventricular-vascular coupling because of the increase in pulsatile ventricular power and consequently inappropriate loading on the ejecting RV (9, 21, 22). As it was mentioned before, pulmonary arterial impedance evaluation is a much more precise and complete method for estimating the pulmonary arterial load (11); however, because of the complexity of this method, it is totally difficult to use it for the patients. Sunagawa et al. (12) has thought up the concept of effective arterial elastance, which is a parameter including the basic elements of the Windkessel model in the vascular bed (12, 23). Sunagawa et al. (23) have demonstrated that Ea (PV) is a useful factor in the evaluation of arterial load and its interference with ventricular function. These researchers have also suggested that this factor is considered as a strong and long-lasting index in the evaluation of pulsatile load repercussions with an increase in age and hypertension. These studies have shown that the average intensity in arteries often underestimates the real load effect on the heart function (13). Morimont et al. (14) have also studied this factor for pulmonary arteries in different loading conditions. One alternative for the calculation of Ea is using the ratio of Pes over SV. Many scientists have used artery pressure in the dicrotic notch to estimate Pes and some have used peak pressure (24-28). However, in this study, we have used Pes in the dicrotic notch.
Assessment of RV afterload in systolic heart failure patients seems necessary because it provides both therapeutic and prognostic implications. Previous studies have demonstrated that pulmonary hypertension and resultant right heart dysfunction is increasingly common in patients with systolic heart failure, which potently affects exercise capacity and clinical outcome in these patients, regardless of left ventricular ejection fraction (29, 30). In patients with advanced heart failure, the presence of pulmonary vascular resistance and its reactivity to vasodilators such as nitric oxide donators, milrinone, the phosphodiesterase-5 inhibitor sildenafil, and the natriuretic peptide nesiritide are in extensive use to define the patients` eligibility for cardiac transplantation. [Ea (PV)] is a measure of total RV afterload, which reflects both the resistive and pulsatile components. In left heart failure patients with pulmonary hypertension, Ea (PV) has also been found to be able to discriminate survivors from non-survivors over a mean time period of 4.4 years (31). Currently, right heart catheterization is considered the gold standard method for the assessment of the pulmonary vasculature hemodynamics. However, as an invasive and expensive procedure, it has its known specific limitations and complications. Nowadays, echocardiography is highly considered as an easy and non-invasive method in patients for diagnostic and prognostic evaluation. Doppler echocardiography is quietly precise for the estimation of simple cardiac hemodynamic measures, and the TR flow is used to estimate the RV systolic pressure and pulmonary artery pressures (32). In addition, we can estimate the RV SV using the RVOT VTI and RVOT diameter using echocardiography (17). Thus, in this study, we have suggested that it is possible to estimate the pulmonary artery elastance through the use of TR flow gradient at the end of systole and the RV SV, which is obtained by the hydraulic orifice formula. As it was mentioned, there is a strong and significant relation between the calculated elastance by echocardiography and the one obtained from right heart catheterization. With the increasing importance of non-invasive methods in the evaluation of patients suffering from heart failure and also because of the absolute need to identify some necessary factors for estimating the RV afterload more precisely, the use of this factor in addition to the pulmonary arterial resistance may further help us to evaluate the patients with heart failure.
Study limitations
In the present study, we used the fluid-filled catheters to calculate the pressure. Although it is quite obvious that using a high-fidelity pressure transducer catheter is more precise for studying the hemodynamics, these catheters are expensive and complex and it is difficult to use them in clinical settings. However, we have also used the dicrotic notch to estimate Pes, while the final time of blood drainage depends on both the external loading and myocardial contractility. It is necessary to have a full profile tricuspid insufficiency Doppler curve through the systole, including end-systole, to estimate the pulmonary arterial pressure and Pes.
Conclusion
Considering the important effectiveness of RV afterload on RV ejection fraction and pulmonary artery elastance as a surrogate of RV afterload, it seems completely essential to determine Ea (PV) in patients with systolic heart failure for both therapeutic and prognostic decision making. Doppler echocardiography is an easy, non-invasive, and inexpensive way for measuring pulmonary arterial elastance, which provides accurate and reliable estimation of RV afterload in patients with systolic heart failure.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - S.T., M.E., A.A., N.N., H.B.A., M.M., M.C.; Design - S.T., M.E., A.A., N.N., H.B.A., M.M., M.C.; Supervision - S.T., M.E., A.A., N.N., H.B.A., M.M., M.C.; Materials - S.T., H.B., A.A.; Data collection &/or processing - S.T., M.E., A.A.; Analysis &/or interpretation - M.C., H.B.A.; Literature search - M.C., A.A., S.T.; Writing - S.T., M.E., A.A., N.N., H.B.A., M.M., M.C.; Critical review - S.T., M.E., A.A., N.N., H.B.A., M.M., M.C.; Other - S.T., M.E., A.A., N.N., H.B.A., M.M., M.C.
References
- 1.Mann DL. Management of heart failure patients with reduced ejection fraction. In: Bonow RO, Mann DL, Zipes DP, et al., editors. Braunwald’s Heart Disease. 9th Edition. Elsevier; 2012. pp. 543–77. [Google Scholar]
- 2.de Groote P, Millaire A, Foucher-Hossein C, Nugue O, Marchandise X, Ducloux G, et al. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol. 1998;32:948–54. doi: 10.1016/s0735-1097(98)00337-4. [DOI] [PubMed] [Google Scholar]
- 3.Di Salvo TG, Mathier M, Semigran MJ, Dec GW. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol. 1995;25:1143–53. doi: 10.1016/0735-1097(94)00511-n. [DOI] [PubMed] [Google Scholar]
- 4.Chen EP, Craig DM, Bittner HB, Davis RD, Van Trigt P. Pharmacological strategies for improving diastolic dysfunction in the setting of chronic pulmonary hypertension. Circulation. 1998;97:1606–12. doi: 10.1161/01.cir.97.16.1606. [DOI] [PubMed] [Google Scholar]
- 5.Szabó G, Soós P, Bährle S, Radovits T, Weigang E, Kékesi V, et al. Adaptation of the right ventricle to an increased afterload in the chronically volume overloaded heart. Ann Thorac Surg. 2006;82:989–95. doi: 10.1016/j.athoracsur.2006.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Shah RV, Fifer MA. Heart Failure. In: Lilli, Leonard S, editors. Pathophysiology of heart disease. 4th ed. Lippincott Williams & Wilkins; 2007. pp. 225–52. [Google Scholar]
- 7.Mehra MR, Kobashigawa J, Starling R, Russell S, Uber PA, Parameshwar J, et al. Listing criteria for heart transplantation:International Society for Heart and Lung Transplantation Guidelines for the care of cardiac transplant candidates. J Heart Lung Transplant. 2006;25:1024–42. doi: 10.1016/j.healun.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Weinberg CE, Hertzberg JR, Ivy DD, Kirby KS, Chan KC, Valdes-Cruz L, et al. Extraction of pulmonary vascular compliance, pulmonary vascular resistance, and right ventricular work from single-pressure and Doppler flow measurements in children with pulmonary hypertension:a new method for evaluating reactivity in vitro and clinical studies. Circulation. 2004;110:2609–17. doi: 10.1161/01.CIR.0000146818.60588.40. [DOI] [PubMed] [Google Scholar]
- 9.Milnor WR, Conti R, Lewis KB, O’Rourke MF. Pulmonary arterial pulse wave velocity and impedance in man. Circ Res. 1969;25:637–49. doi: 10.1161/01.res.25.6.637. [DOI] [PubMed] [Google Scholar]
- 10.Grant BJB, Lieber BB. Clinical significance of pulmonary arterial input impedance. Eur Respir J. 1996;9:2196–9. doi: 10.1183/09031936.96.09112196. [DOI] [PubMed] [Google Scholar]
- 11.Lankhaar JW, Westerhof N, Faes TJ, Marques KM, Marcus JT, Postmus PE, et al. Quantification of right ventricular afterload in patients with and without pulmonary hypertension. Am J Physiol Heart Circ Physiol. 2006;291:H1731–7. doi: 10.1152/ajpheart.00336.2006. [DOI] [PubMed] [Google Scholar]
- 12.Sunagawa K, Maughan WL, Sagawa K. Optimal arterial resistance for the maximal stroke work studied in isolated canine left ventricle. Circ Res. 1985;56:586–95. doi: 10.1161/01.res.56.4.586. [DOI] [PubMed] [Google Scholar]
- 13.Kelly RP, Ting CT, Yang TM, Liu CP, Maughan WL, Chang MS, et al. Effective arterial elastance as index of arterial vascular load in humans. Circulation. 1992;86:513–21. doi: 10.1161/01.cir.86.2.513. [DOI] [PubMed] [Google Scholar]
- 14.Morimont P, Lambermont B, Ghuysen A, Gerard P, Kolh P, Lancellotti P, et al. Effective arterial elastance as an index of pulmonary vascular load. Am J Physiol Heart Circ Physiol. 2008;294:H2736–42. doi: 10.1152/ajpheart.00796.2007. [DOI] [PubMed] [Google Scholar]
- 15.Amin A, Taghavi S, Esmaeilzadeh M, Bakhshandeh H, Naderi N, Maleki M. pulmonary arterial elastance for estimating right ventricular afterload in systolic heart failure. Congest Heart Fail. 2011;17:288–93. doi: 10.1111/j.1751-7133.2011.00222.x. [DOI] [PubMed] [Google Scholar]
- 16.Himelman RB, Stulbarg M, Kircher B, Lee E, Kee L, Dean NC, et al. Noninvasive evaluation of pulmonary artery pressure during exercise by saline-enhanced Doppler echocardiography in chronic pulmonary disease. Circulation. 1989;79:863–71. doi: 10.1161/01.cir.79.4.863. [DOI] [PubMed] [Google Scholar]
- 17.Conolly HM, Oh JK. Echocardiography. In: Robert O, Bonow, Douglas L Mann, Douglas P Zipes, Peter Libby, editors. Braunwald’s Heart Disease. 9th Edition. Elsevier; 2012. pp. 200–76. [Google Scholar]
- 18.Forfia PR, Wiegers SE. Otto CM. In The Practice of clinical echocardiography. 3rd ed. Philadelphia: Saunders Elsevier; 2007. Echocardiographic findings in acute and chronic respiratory disease; pp. 848–76. [Google Scholar]
- 19.Kussmaul WG, 3rd, Altschuler JA, Matthai WH, Laskey WK. Right ventricular-vascular interaction in congestive heart failure. Importance of low-frequency impedance. Circulation. 1993;88:1010–5. doi: 10.1161/01.cir.88.3.1010. [DOI] [PubMed] [Google Scholar]
- 20.Bergel DH, Milnor WR. Pulmonary vascular impedance in dog. Circ Res. 1965;16:401–15. doi: 10.1161/01.res.16.5.401. [DOI] [PubMed] [Google Scholar]
- 21.Yin FC, Guzman PA, Brin KP, Maughan WL, Brinker JA, Traill TA, et al. Effects of nitroprusside on hydraulic vascular loads on the right and left ventricle in patients with heart failure. Circulation. 1983;67:1330–9. doi: 10.1161/01.cir.67.6.1330. [DOI] [PubMed] [Google Scholar]
- 22.Laskey WK, Ferrari VA, Palevsky HI, Kussmaul WG. Pulmonary artery hemodynamics in primary pulmonary hypertension. J Am Coll Cardiol. 1993;21:406–12. doi: 10.1016/0735-1097(93)90682-q. [DOI] [PubMed] [Google Scholar]
- 23.Sunagawa K, Maughan WL, Burkhoff D, Sagawa K. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol Heart Circ Physiol. 1983;245:H773–80. doi: 10.1152/ajpheart.1983.245.5.H773. [DOI] [PubMed] [Google Scholar]
- 24.Grossman W, Braunwald E, Mann T, McLaurin LP, Green LH. Contractile state of the left ventricle in man as evaluated from end-systolic pressure-volume relations. Circulation. 1977;56:845–52. doi: 10.1161/01.cir.56.5.845. [DOI] [PubMed] [Google Scholar]
- 25.Borow KM, Neumann A, Wynne J. Sensitivity of end-systolic pressure-dimension and pressure-volume relations to the inotropic state in humans. Circulation. 1982;65:988–97. doi: 10.1161/01.cir.65.5.988. [DOI] [PubMed] [Google Scholar]
- 26.Slutsky R, Watkins J, Peterson K, Karliner J. The response of left ventricular function and size to atrial pacing, volume loading and afterload stress in patients with coronary artery disease. Circulation. 1981;63:864–70. doi: 10.1161/01.cir.63.4.864. [DOI] [PubMed] [Google Scholar]
- 27.Marsh JD, Green LH, Wynne J, Cohn PF, Grossman W. Left ventricular end-systolic pressure-dimension and stress-length relation in normal human subjects. Am J Cardiol. 1979;44:1311–7. doi: 10.1016/0002-9149(79)90446-6. [DOI] [PubMed] [Google Scholar]
- 28.Mehmel HC, Stockins B, Ruffmann K, Olshausen K, Schuler G, Kubler W. The linearity of the end-systolic pressure-volume relation in man and its sensitivity for the assessment of left ventricular function. Circulation. 1981;63:1216–22. doi: 10.1161/01.cir.63.6.1216. [DOI] [PubMed] [Google Scholar]
- 29.Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II:pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117:1717–31. doi: 10.1161/CIRCULATIONAHA.107.653584. [DOI] [PubMed] [Google Scholar]
- 30.Kjaergaard J, Akkan D, Iversen KK, Kjoller E, Køber L, Torp-Pedersen C. Prognostic importance of pulmonary hypertension in patients with heart failure. Am J Cardiol. 2007;99:1146–50. doi: 10.1016/j.amjcard.2006.11.052. [DOI] [PubMed] [Google Scholar]
- 31.Tampakakis E, W Kelemen BW, Shpigel A, Rickard J, Leary PJ, Kasper EK, et al. Right ventricular effective arterial elastance is a novel predictor of mortality in pulmonary hypertension due to left heart disease. (abstr) Circulation. 2014;130:A16651. [Google Scholar]
- 32.Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984;70:657–62. doi: 10.1161/01.cir.70.4.657. [DOI] [PubMed] [Google Scholar]