Introduction
Inappropriate sinus tachycardia (IST) during pregnancy may be asymptomatic until maternal heart failure (HF) develops (1). There is no information on the safety of the use of ivabradine in pregnant patients.
Case Report
A 32-year-old patient, in the 17th week of her first pregnancy, was admitted to the local hospital with complaints of palpitations and shortness of breath, which progressed over a month. The patient had no prior history of any cardiac disease. At the time of admission, the electrocardiogram (ECG) of the patient revealed that she had supraventricular tachycardia. When the patient did not respond to adenosine and electrical cardioversion, she was transferred to our hospital. ECG revealed IST with a heart rate (HR) of 152 bpm (Fig. 1a). She was continuously monitored, and intravenous esmolol infusion and oral metoprolol were started. Due to the high HR, verapamil (240 mg/day) and digoxin (0.25 mg/day) were added, and HR decreased to 120 bpm (Fig. 1b). Echocardiography showed normal left ventricular (LV) dimensions, LV ejection fraction (LVEF) at 45%, and mild mitral regurgitation (MR). On the 7th day of hospitalization, LVEF decreased to 40%, followed by a decrease to 30% at the end of the 2nd week. The patient developed severe MR. Furosemide was added to the treatment, but the patient did not experience clinical relief. After receiving the patient’s consent, we began ivabradine treatment (2x5 mg), and the patient’s HR dropped to 90 bpm (Fig. 1c) and remained normal until discharge (Fig. 1d). Prior to ivabradine treatment, fetal echocardiography showed the fetal HR to be 156 bpm (Fig. 2a). After the 1st day of ivabradine treatment, the fetal HR was 150 bpm (Fig. 2b), and on the 7th day, it was 148 bpm (Fig. 2c). However, it did not decline further until delivery. When the patient’s HR returned to normal, LVEF improved each day and reached 50% and MR reduced. Maternal tachycardia and fetal bradycardia were not detected during the monthly follow-ups. A healthy baby boy was delivered. The baby was only fed with breast milk, and on 15th day, ECG showed sinus rhythm with an HR of 180 bpm (Fig. 2d).
Figure 1.
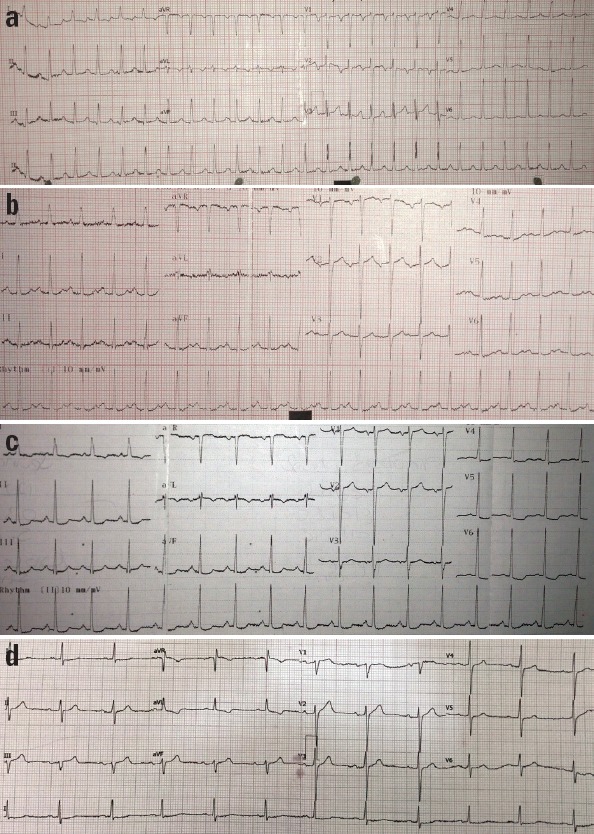
The electrocardiogram (ECG) taken at the time of admission showed that the patient had sinus tachycardia with a heart rate of 152 bpm (a). Following a maximum treatment regimen (200 mg/day of metoprolol, 0.25 mg/day of digoxin, and 240 mg/day of verapamil), the ECG showed sinus tachycardia with the heart rate of 120 bpm (b). After ivabradine treatment, the ECG showed sinus rhythm with the heart rate reduced to 90 bpm (c), and the ECG at discharge showed sinus rhythm within the normal range (d)
Figure 2.
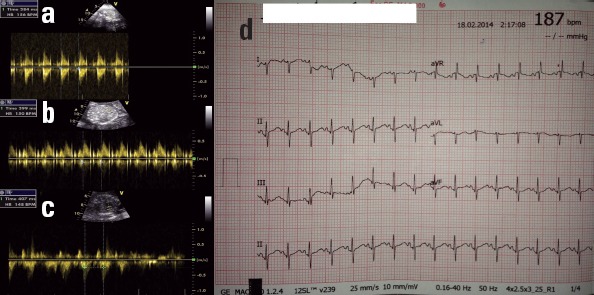
Prior to starting treatment with ivabradine, fetal echocardio-graphy showed a heart rate of 156 bpm (a). On the 1st day of ivabradine treatment, the fetal ECG showed that the fetal heart rate was 150 bpm (b). On the 1st week of ivabradine treatment, the fetal heart rate reduced to 148 bpm (c). After delivery, the mother continued her ivabradine treatment, and the ECG of the baby, who was fed only breast milk, showed sinus rhythm with a heart rate of 180 bpm (d)
Discussion
Persistent IST is a rare atrial tachycardia characterized by an exaggerated increase in HR (usually ≥100 bpm at rest) with “normal” P waves on ECG. P-wave morphology is usually similar or identical to sinus rhythm. In general, IST is a diagnosis made by exclusion. The treatment for IST has been limited to calcium channel blockers, beta-blockers, antiarrhythmic drugs, and sometimes, radiofrequency ablation. Although metoprolol, verapamil, and digoxin were used in maximum doses in our patient, the control of HR was not achieved and LVEF deteriorated each day, which led to the development of symptomatic HF.
The most popular choice for patients with drug-refractory IST is sinus node modification using radiofrequency ablation (2, 3). However, our patient did not agree to undergo the procedure because of risks such as ionizing radiation, phrenic nerve injury, requirement for permanent pacing, and pericarditis.
A specific HR reducing agent (through the inhibition of pacemaker If current), ivabradine has been documented to be effective for treating angina pectoris and HF (4, 5). The benefit of ivabradine in patients with drug-refractory IST has been des-cribed (3–6). There is no information regarding the safety of ivabradine use during pregnancy. In the literature, there is only one study by Babic et al. (7) that demonstrates the administration of ivabradine to a first-trimester pregnant patient presenting with myocardial infarction.
The success of ivabradine treatment for IST-associated cardiomyopathy has been reported in 2 patients in the literature (8, 9). With the improvement of tachycardia, the patients’ clinical symptoms and LVEF also improved, and reduction in MR was observed.
In rats, ivabradine has been shown to pass to the breast milk, but its effect is unknown (10). In our patient, the baby was only fed breast milk and neither bradycardia nor cardiac dysfunction was observed. Therefore, we concluded that ivabradine did not pass to breast milk in amounts that affect the baby’s HR.
Conclusion
We have shown that ivabradine treatment improved tachycardia and HF in a pregnant patient with IST-induced cardiomyopathy. In addition, no maternal and fetal side effects were observed. However, further studies are still needed to evaluate the use of ivabradine treatment during pregnancy and breastfeeding.
References
- 1.Szumowski L, Szufladowicz E, Orczykowski M, Bodalski R, Derejko P, Przybylski A, et al. Ablation of severe drug-resistant tachy-arrhythmia during pregnancy. J Cardiovasc Electrophysiol. 2010;21:877–82. doi: 10.1111/j.1540-8167.2010.01727.x. [DOI] [PubMed] [Google Scholar]
- 2.Gianni C, Di Biase L, Mohanty S, Gökoğlan Y, Güneş MF, Horton R, et al. Catheter ablation of inappropriate sinus tachycardia. J Interv Card Electrophysiol. 2015 Aug 27; doi: 10.1007/s10840-015-0040-2. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 3.Salazar Adum JP, Arora R. Treatment for inappropriate sinus tachycardia. Am J Ther. 2015 Sep 16; doi: 10.1097/MJT.0000000000000335. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Fox K, Ford I, Steg PG, Tendera M, Ferrari R. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL):a randomized, double- blind, placebo-controlled trial. Lancet. 2008;372:807–16. doi: 10.1016/S0140-6736(08)61170-8. [DOI] [PubMed] [Google Scholar]
- 5.Mason PK, Di Marco JP. New pharmacological agents for arrhythmias. Circ Arrhythm Electrophysiol. 2009;2:588–97. doi: 10.1161/CIRCEP.109.884429. [DOI] [PubMed] [Google Scholar]
- 6.Rakovec P. Treatment of inappropriate sinus tachycardia with iva-bradine. Wien Klin Wochensch. 2009;121:716–8. doi: 10.1007/s00508-009-1265-9. [DOI] [PubMed] [Google Scholar]
- 7.Babic Z, Gabric ID, Pintaric H. Successful primary percutaneous coronary intervention in the first trimester of pregnancy. Catheter Cardiovasc Interv. 2011;77:522–5. doi: 10.1002/ccd.22813. [DOI] [PubMed] [Google Scholar]
- 8.Winum PF, Cayla G, Rubini M, Beck L, Messner-Pellenc P. A case of cardiomyopathy induced by inappropriate sinus tachycardia and cured by ivabradine. Pacing Clin Electrophysiol. 2009;32:942–4. doi: 10.1111/j.1540-8159.2009.02414.x. [DOI] [PubMed] [Google Scholar]
- 9.Bohora S, Lokhandwala Y, Parekh P, Vasavda A. Reversal of tachycardiomyopathy due to left atrial tachycardia by ivabradine. J Cardiovasc Electrophysiol. 2011;22:340–2. doi: 10.1111/j.1540-8167.2010.01860.x. [DOI] [PubMed] [Google Scholar]
- 10.Kockova R, Svatunkova J, Novotny J, Hejnova L, Ostadal B, Sedmera D. Heart rate changes mediate the embryotoxic effect of antiarrhythmic drugs in the chick embryo. Am J Physiol Heart Circ Physiol. 2013;304:895–902. doi: 10.1152/ajpheart.00679.2012. [DOI] [PubMed] [Google Scholar]


