Abstract
Mechanical index (MI) is a measure of acoustic power. It is generally omitted during routine echocardiographic imaging. By adjusting the MI, an echocardiographer can perform various contrast-specific imaging modalities during the same session.
Keywords: mechanical index, echocardiography, bioeffect
Introduction
Ultrasound is a type of energy created by pressure waves, and its effects on living tissues are named bioeffects. Heating (thermal) and mechanical (non-thermal) effects are two main bioeffects observed in an ultrasonographic examination. Two indices are derived from these bioeffects in modern ultrasonographic machines, i.e., thermal index (TI) and mechanical index (MI). All ultrasonography machines manufactured after 1992 have to add the two safety indices of MI and TI on their screen.
In this review, we tried to mention about the brief definition and clinical usage of the MI.
Mechanical index
Acoustic power is the amount of acoustic energy per time unit. Acoustic power shows the amplitude of the pulse pressure of the ultrasound beam. The MI gives the operator information about the magnitude of energy administered to a patient during an echocardiographic examination.
The MI is a measure of the power of an ultrasound beam. It is derived from the need for an indicator for the possible non-thermal bioeffects of the acoustic field, such as cavitation and streaming.
Cavitation is the expansion and contraction or collapse of bubbles because of the acoustic pressure of the ultrasound beam. Streaming is the movement of complex fluids because of radiation force pressures. The most important non-thermal bioeffect is cavitation. Therefore, before we introduce the MI, cavitation should be mentioned first.
Microbubbles are small and spherical gas-filled bubbles in the size range of 1-10 microns. When a fluid with a microbubble was exposed to an acoustic field, gas-filled bubbles undergo changes in volume in response to acoustic pressure and gets bigger. This phenomenon is known as cavitation (1). The possibility for cavitation is determined by the frequency of the system (2). Shorter the interval between pressure waveform, higher is the frequency, and lower is the growth of gas-filled bubbles.
In 1989, Holland et al. (3) showed that the initial size of the cavitation nucleus determined the minimum acoustic pressure waveform amplitude required for significant bubble growth. The initial smaller size of nucleus needs a higher acoustic pressure amplitude to overcome the stronger surface tension. It means that the higher frequencies require a very specific and small bubble radius for cavitation.
The most cavitation sensitive tissues are gas-filled organs such as the lung and intestine.
The MI can be defined as peak negative pressure divided by the square root of the frequency of the ultrasound wave.
It is calculated from a formula: P- /√ ƒ
MI: P-:peak negative pressure (MPascal) ƒ-frequency (Mhz)
Display of the MI on clinical ultrasonographic machines is mandatory in USA to provide information about the ultrasonographic exposure of the myocardial tissue and to put a limit to the output of the device. However, it is not possible to compare the MI directly from one machine to another; it is one of the most important setting in a contrast echocardiographic study. At a lower MI, microbubbles start to oscillate and vibrate, thereby giving rise to a signal in ultrasound imaging. In contrast, these microbubbles rupture at a higher MI (4). This microbubble rupture is responsible for the non-thermal bioeffect of ultrasonography (5). The MI displayed on clinical ultrasound scanners is intended to estimate these mechanical bioeffects.
The ideal value of the MI should be <1.9 to avoid the bioeffect. The FDA approved MI value of 1.9 is the maximum threshold for diagnostic imaging. Apfel and Holland (6) showed that bubble growth does not exist below the value of 0.5 for MI. However, cavitation clearly exists for values that are two to three points above this index (6). In the literature, authors reported capillary leakage and extravasations for ultrasound exposures above a MI of 0.4 in vivo tests (7, 8). In a meta-analysis performed by the World Health Organization, ultrasonography did not have adverse fetal effects in routine clinical practice (9). A randomized follow- up trial showed that repeated prenatal ultrasonography had no harmful effects on the fetus (10).
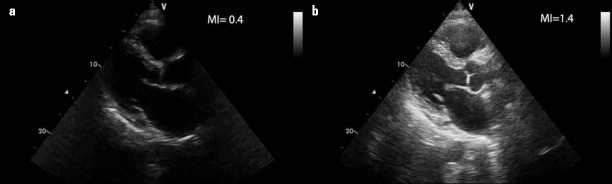
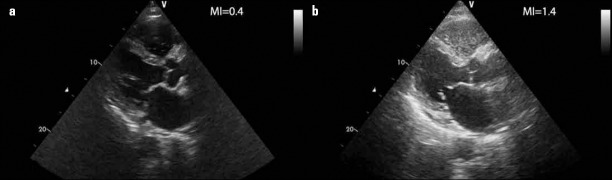
Figure 1 shows parasternal long-axis images at two different acoustic power energies. Echogenicity of the myocardial tissue is brighter at a high MI (1.4) value than a low MI value (0.4). After contrast injection, the scattering of the contrast agent becomes higher as the MI index increases. At high MI values, the contrast agent is destroyed, which causes brighter images. At low MI values, brightness of the contrast agent is low because it is not destroyed rapidly, which results in a longer lasting less brighter contrast effect (Fig. 2).
Figure 1.
a, b. Parasternal long axis images at two different mechanical indices. a. MI=0.4, b. MI=1.4
Figure 2.
a, b. After contrast injection, the scattering of the contrast agent becomes higher as the MI index increases. a. MI=0.4, b. MI=1.4
Role of mechanical index in contrast echocardiography
During contrast echocardiography, agitated saline or second generation contrast agents such as perfluorocarbon are injected intravenously, thereby creating a cloud of microbubbles. Microbubbles are intense ultrasound reflectors and forms a differential reflection compared to surrounding tissues and blood. This differential reflection enables the sonographer to clearly investigate the endocardial border, shunts, and myocardial perfusion. Maximal reflection is dependent on the frequency of the ultrasound beam and the diameter of the microbubble. Standard B mode echocardiography routinely runs at a MI between 0.9 and 1.4, leading to optimal myocardial imaging with variable bubble destruction. The ultrasound beam destroys all perfluorocarbon contrast agents above the MI of 1.3, generating a large amount of acoustic energy and this leads to an instantaneous burst signal effect. A high MI is used to achieve myocardial perfusion imaging. With ongoing destruction, the contrast effect is lost. At lower MIs, particularly <0.4, the ultrasound beam destroys less bubbles. This preserves the contrast effect and leads to homogenous and continuous imaging of the contrast agents in the blood pool. A low MI is optimal for left ventricular opacification (11).
In a study performed by Holland et al. (12), the authors reported that ultrasonographic contrast agents (UCAs) could significantly lower the threshold required for acoustic cavitation. This finding led to the development of a new idea of using a drug or gene labeled contrast agents for targeting therapeutic applications with much lower ultrasonographic energy. This work suggested that UCAs can be used to induce cavitation for therapeutic applications with much lower ultrasound energy. Many researchers have investigated this field and reported many papers (13-16).
Three methods can be used for drug delivery with UCAs. The first method is to administer microbubbles and the drug at the same time. The second method is to attach the drug on the shell of the microbubbles. The last method is to place the drug into the lumen of the microbubbles.
Drug or gene labeled microbubbles can intentionally rupture with ultrasonographic energy at the target vessel to release the drug or gene to the target site (17, 18). In addition, microbubble destruction by ultrasound wave creates micro jets, forcing drug diffusion to the target tissue (19). Under certain ultrasonographic pressure or MI, microbubbles move and collide with the vascular endothelium. This interaction between microbubbles and endothelium increases the vascular permeability (20). In a study performed by Sorace et al. (21), the authors showed that an increase in the vascular permeability is greatest at a MI of 1.0. Vascular permeability is minimal at a MI of 2.0 because destruction of microbubbles decreases the number of intact microbubbles that interact with vascular endothelium. Therefore, intact and oscillating microbubbles under certain MI are required to increase vascular permeability.
Conclusion
As a result, there are no major adverse effects of ultrasonography that have been shown in the use of ultrasonography in routine clinical practice; however, it is advised to pay attention to safety indices such as MI and TI. Therefore, an ultrasonographer or an echocardiographer should be aware of the safety indices of MI and TI. The MI is a measure of ultrasonographic power. By adjusting the power and MI, an echocardiographer can perform various contrast-specific imaging modalities during the same session. By using certain MI values, drug or gene labeled microbubbles can be specifically directed to the target tissue for therapeutic applications.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - T.Ş., O.T.; Design - T.Ş.; Supervision - T.Ş.; Resource - Y.K., O.T.; Analysis &/or interpretation - T.Ş.; Literature search - T.Ş., Y.K.; Writing - T.Ş.; Critical review - Y.K., O.T.
References
- 1.Young FR. Cavitation. London: Imperial College Press; 1999. [CrossRef] [Google Scholar]
- 2.Anderson AL, Hampton LD. Acoustics of gas-bearing sediments: I. Background. J Acoust Soc Am. 1980;67:1865. [CrossRef] [Google Scholar]
- 3.Holland CK, Apfel RE. An improved theory for the prediction of microcavitation thresholds. IEEE Trans Ultrason Ferroelectr Freq Control. 1989;36:204–8. doi: 10.1109/58.19152. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 4.Palekar-Shaanbag P, Chogale MM, Jog SV, Gaikwad SS. Microbubbles and their applications in pharmaceutical targeting. Curr Drug Deliv. 2013;10:363–73. doi: 10.2174/1567201811310040001. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 5.American Institute of Ultrasound in Medicine. Bioeffects of diagnostic ultrasound with gas body contrast agents. Official statement. Laurel, MD: American Institute of Ultrasound in Medicine; 2002. [Google Scholar]
- 6.Apfel RE, Holland CK. Gauging the likelihood of cavitation from short pulse, low duty cycle diagnostic ultrasound. Ultrasound Med Biol. 1991;17:179. doi: 10.1016/0301-5629(91)90125-g. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Skyba DM, Price RJ, Linka AZ, Skalak TC, Kaul S. Direct in vivo visualization of intravascular destruction of microbubbles by ultrasound and its local effects on tissue. Circulation. 1998;98:290–3. doi: 10.1161/01.cir.98.4.290. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Miller DL, Quddus J. Diagnostic ultrasound activation of contrast agent gas bodies induces capillary rupture in mice. Proc Natl Acad Sci USA. 2000;97:10179–84. doi: 10.1073/pnas.180294397. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torloni MR, Vedmedovska N, Merialdi M, Betrán AF, Allen T, Gonzalez R, et al. ISUOG-WHO Fetal Growth Study Group. Safety of ultrasonography in pregnancy: WHO systematic review of the literature and meta-analysis. Ultrasound Obstet Gynecol. 2009;33:599–608. doi: 10.1002/uog.6328. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Newnham JP, Doherty DA, Kendall GE, Zubrick SR, Landau LL, Stanley FJ. Effects of repeated prenatal ultrasound examinations on childhood outcome up to 8 years of age: follow-up of a randomized controlled trial. Lancet. 2004;364:2038–44. doi: 10.1016/S0140-6736(04)17516-8. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 11.Stewart MJ. Contrast echocardiography. Heart. 2003;89:342–8. doi: 10.1136/heart.89.3.342. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holland CK, Apfel RE. Thresholds for transient cavitation produced by pulsed ultrasound in a controlled nuclei environment. J Acoust Soc Am. 1990;88:2059–69. doi: 10.1121/1.400102. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 13.Shohet RV, Chen S, Zhou YT, Wang Z, Meidell RS, Unger RH, et al. Echocardiographic destruction of albumin microbubbles directs gene delivery to the myocardium. Circulation. 2000;101:2554–6. doi: 10.1161/01.cir.101.22.2554. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.Hashiya N, Aoki M, Tachibana K, Taniyama Y, Yamasaki K, Hiraoka K, et al. Local delivery of E2F decoy oligodeoxynucleotides using ultrasound with microbubble agent (Optison) inhibits intimal hyperplasia after balloon injury in rat carotid artery model. Biochem Biophys Res Commun. 2004;317:508–14. doi: 10.1016/j.bbrc.2004.03.070. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 15.Suzuki R, Takizawa T, Negishi Y, Hagisawa K, Tanaka K, Sawamura K, et al. Gene delivery by combination of novel liposomal bubbles with perfluoropropane and ultrasound. J Control Rel. 2007;15:531–7. doi: 10.1016/j.jconrel.2006.09.008. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 16.Xie F, Tsutsui JM, Lof J, Unger EC, Johanning J, Culp WC, et al. Effectiveness of lipid microbubbles and ultrasound in declotting thrombosis. Ultrasound Med Biol. 2005;21:979–85. doi: 10.1016/j.ultrasmedbio.2005.03.008. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 17.Stride E, Saffari N. On the destruction of microbubble ultrasound contrast agents. Ultrasound Med Biol. 2003;29:563–73. doi: 10.1016/s0301-5629(02)00787-1. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 18.Marin A, Sun H, Husseini GA, Pitt WG, Christensen DA, Rapoport NY. Drug delivery in pluronic micelles: Effect of high-frequency ultrasound on drug release from micelles and intracellular uptake. J Control Release. 2002;84:39–47. doi: 10.1016/s0168-3659(02)00262-6. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 19.Liu Y, Yang H, Sakanishi A. Ultrasound: mechanical gene transfer into plant cells by sonoporation. Biotech Adv. 2006;24:1–16. doi: 10.1016/j.biotechadv.2005.04.002. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 20.Ward M, Wu J, Chiu JF. Ultrasound-induced cell lysis and sonoporation enhanced by contrast agents. J Acoust Soc Am. 1999;105:2951–7. doi: 10.1121/1.426908. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 21.Sorace AG, Warram JM, Umphrey H, Hoyt K. Microbubble- mediated ultrasonic techniques for improved chemotherapeutic delivery in cancer. J Drug Target. 2012;20:43–54. doi: 10.3109/1061186X.2011.622397. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]