Introduction
Left ventricular thrombus (LVT) is a frequent complication of acute myocardial infarction (MI). Late ventricular thrombus formation is a rare phenomenon, and it is associated with adverse chamber remodeling. Oral vitamin K antagonists (VKAs) are the current treatment recommendation for LVT. Herein we present a case of late LVT that successfully resolved by treatment with apixaban.
Case Report
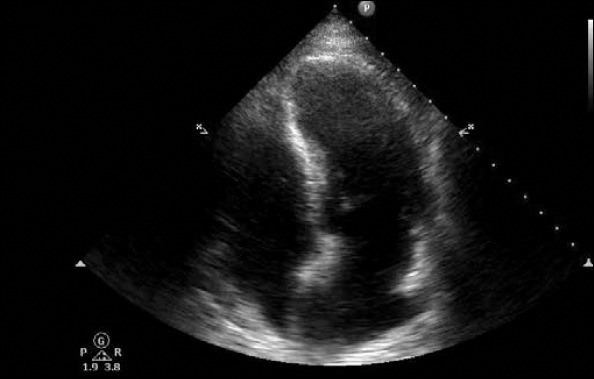
A 55-year-old male patient with a history of anterior MI was followed-up in our outpatient clinic. He did not have atrial fibrillation (AF), and the ejection fraction was 45%. MI occurred 6 years ago, and warfarin has been previously prescribed for LVT. However, he had gastric bleeding at the follow-up while he was using warfarin and acetylsalicylate. At the time of gastric bleeding, INR was 7, and it was learned that his previous visits for INR measurement were inelaborate. Because of patient noncompliance and absence of LVT on echocardiography, warfarin treatment was stopped. Clopidogrel was prescribed, and he was called for echocardiography controls. After 6 months, control echocardiography revealed a mobile apical thrombus (Fig. 1, Video 1). Warfarin treatment was planned for the patient once more. Because of safety concerns regarding non-compliant warfarin use and alternative treatment demands of the patient, we decided to give novel oral anticoagulants (NOACs). The patient was informed about the scarcity of data on the use of NOACs in his condition, and his consent was obtained. Apixaban at a dose of 5 mg twice a day was prescribed to the patient.
Figure 1.

Apical thrombus image (arrow)
After 2 weeks, control echocardiography revealed a suspicious apical thrombus image (Fig. 2, Video 2). At the end of 1 month, the apical thrombus image was not present (Fig. 3, Video 3). Because of the absence of cardiac magnetic resonance imaging at our center, we were unable to prove the definite disappearance of the apical thrombus in our case. However, the thrombus was not seen in all views at the last examination.
Figure 2.

Suspected apical thrombus image (arrow)
Figure 3.
Apical thrombus could not be detected
Discussion
Usually, LVT formation occurs 1-2 weeks after ST-segment elevation MI (STEMI); however, adverse chamber remodeling is associated with late LVT formation (1). Guidelines recommend using oral anticoagulants for at least 3 months after STEMI in case of LVT (2). Despite the fact that trials of long-term anticoagulation of these patients do not exist, late LVT reports in literature emphasize that the duration of anticoagulation may be individualized in certain conditions (3, 4). Recently, NOACs were shown to be effective in thromboembolism prevention, and their safety was shown to be superior to VKAs in AF (5). Although their efficacy and safety are not well defined in patients with LVT, the success of these agents in the treatment of LVT were shown in some reports (6, 7).
Guidelines recommend using VKAs for at least 3 months in patients with LVT or those who are at risk for LVT development. However, the duration of triple antithrombotic therapy should be minimized because of an increased bleeding risk (2, 8). We stopped warfarin treatment because of gastric bleeding with INR of 7 and patient non-compliance. Luckily, we could detect LVT on echocardiography in controls. However, the “safe anticoagulation problem” arose in this patient, and we thought that any NOAC would be better and safer than VKAs, which could not be monitored. Because the incidence of gastrointestinal bleeding is lower in AF patients, we chose apixaban as an anticoagulant in this patient (9). Despite the absence of trials in literature regarding the use of NOACs in case of LVT, some reports encourage the use of these agents (6, 7). Investigations that specifically address late LVT formation in STEMI patients are absent in literature. Regarding stroke and mortality, any superiority of warfarin over acetylsalicylate has not been shown in patients with systolic heart failure with sinus rhythm. Hence, decisions regarding the use of anticoagulants in this population should be individualized (10). Antithrombotic effectiveness and low bleeding risks of apixaban may alter our knowledge and change the practices in the future with randomized controlled trials.
Conclusion
LVT can be seen even years after acute STEMI, and long-term anticoagulation decisions must be individualized. We demonstrated the success of apixaban in the resolution of LVT. Randomized clinical trials in the future are necessary to determine the clinical benefits of apixaban in patients with LVT.
Video 1
Mobile apical thrombus located on the septal apical aneurysmal segment.
Video 2
Suspected thrombus image can be seen in the septal apical aneurysm.
Video 3
Apical thrombus could not be detected.
References
- 1.Delewi R, Nijveldt R, Hirsch A, Marcu CB, Robbers L, Hassell ME, et al. Left ventricular thrombus formation after acute myocardial infarction as assessed by cardiovascular magnetic resonance imaging. Eur J Radiol. 2012;81:3900–4. doi: 10.1016/j.ejrad.2012.06.029. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 2.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013;82:E1–27. doi: 10.1002/ccd.24776. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 3.Lacalzada J, Marí B, Izquierdo MM, Sánchez-grande A, de la Rosa A, Laynez I. Recurrent intraventricular thrombus six months after ST-elevation myocardial infarction in a diabetic man: a case report. BMC Res Notes. 2013;6:348. doi: 10.1186/1756-0500-6-348. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liou K, Lambros J. Delayed left ventricular apical thrombus formation following discontinuation of dual anti-platelet therapy. Heart Lung Circ. 2014;23:e237–9. doi: 10.1016/j.hlc.2014.06.007. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 5.Heidbuchel H, Verhamme IP, Alings M, Antz M, Hacke W, Oldgren J, et al. European Heart Rhythm Association Practical Guide on the use of new oralanticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15:625–51. doi: 10.1093/europace/eut083. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 6.Nagamoto Y, Shiomi T, Matsuura T, Okahara A, Takegami K, Mine D, et al. Resolution of a left ventricular thrombus by the thrombolytic action of dabigatran. Heart Vessels. 2014;29:560–2. doi: 10.1007/s00380-013-0403-5. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Mano Y, Koide K, Sukegawa H, Kodaira M, Ohki T. Successful resolution of a left ventricular thrombus with apixaban treatment following acute myocardial infarction. Heart Vessels. 2014 Aug 1; doi: 10.1007/s00380-014-0562-z. Epub ahead of print. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Steg PG, James SK, Atar D, Badano LR, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569619. doi: 10.1093/eurheartj/ehs215. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 9.Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation-developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14:1385–413. doi: 10.1093/europace/eus305. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Lip GY, Piotrponikowski P, Andreotti F, Anker SD, Filippatos G, Homma S, et al. Thromboembolism and antithrombotic therapy for heart failure in sinus rhythm: an executive summary of a joint consensus document from the ESC Heart Failure Association and the ESC Working Group on Thrombosis. Thromb Haemost. 2012;108:1009–22. doi: 10.1160/TH12-08-0578. [CrossRef] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


